Abstract
Background:
The integration of regulated pharmacy technicians (RPTs) into community pharmacy practice was intended to relieve pharmacists of certain technical duties to facilitate greater provision of direct patient care services, commensurate with expanded scope of practice. There is scant data available regarding the success, value and impact of RPT integration, either in Canada or in other jurisdictions.
Methods:
Pharmacists and RPTs working in community practices were interviewed. Qualitative data were categorized using an iterative coding process to identify themes related to barriers and facilitators to integrating and optimizing the role of the RPT in community practice in Ontario.
Results:
A total of 16 RPTs and 12 pharmacists were interviewed from community sites in Ontario. Strategies for facilitating successful integration of RPTs into daily workflow were identified, based on 4 major themes: environmental factors, interpersonal factors, professional identity formation and innovative use of delegation.
Interpretation:
Integration of RPTs into community practice is complex and requires careful management, planning, training and follow-up to ensure attainment of objectives. Simply hiring RPTs and placing them into existing workflow patterns is generally not a successful implementation strategy.
Conclusions:
Implementation strategies identified through this study can provide employers, managers, pharmacists and RPTs with opportunities to enhance RPT integration and optimize the role of both pharmacists and RPTs in community practice.
Knowledge Into Practice.
Simply regulating pharmacy technicians does not ensure successful integration into the workforce.
Workplace redesign to support expanded roles for regulated technicians is essential.
Helping regulated pharmacy technicians manage interpersonal communication and conflict should be considered to enhance their confidence in this new role.
Further opportunities for appropriate delegation of pharmacists’ activities should be considered.
Mise En Pratique Des Connaissances.
Le seul fait de réglementer les techniciens en pharmacie ne suffit pas à assurer une intégration efficace de cette ressource au sein des effectifs.
Il est essentiel de procéder à une restructuration du lieu de travail afin de favoriser l’élargissement des rôles des techniciens réglementés.
Il faudrait aussi envisager des moyens d’aider les techniciens en pharmacie réglementés à gérer les communications et les conflits interpersonnels, afin de leur donner davantage confiance dans leur nouveau rôle.
D’autres possibilités devraient aussi être envisagées pour assurer une délégation appropriée des fonctions des pharmaciens.
Background
The continuing expansion of pharmacists’ roles in direct patient care requires a more effective utilization of time and resources within the community pharmacy environment.1 To support this evolution, pharmacy regulatory authorities in diverse jurisdictions have created the role of regulated pharmacy technician (RPT) as a way of optimizing and rationalizing roles and responsibilities within pharmacies to manage workload and time required for direct patient care activities.1,2 As noted in the literature and by the regulatory authorities, it was anticipated that RPTs would relieve pharmacists of technical tasks to facilitate greater time and focus on therapeutic and cognitive aspects of medication management services.3
Large numbers of RPTs now exist around the world, yet there is scant literature highlighting whether the initial expectations of their role have actually been fulfilled and what barriers and facilitators to optimizing RPTs’ roles (particularly in community practice) exist.3,4 Given the importance of RPTs to the anticipated/projected workflow in community practice (and workload reduction for pharmacists), there is a need to better understand the integration process. Few jurisdictions have undertaken systematic research to identify factors supporting successful integration of RPTs into the community pharmacy setting, and so evidence is currently lacking as to the success, value and impact of RPTs in community practice and what integration strategies facilitate optimal use of their knowledge and skills.4,5 Instead, after enabling regulatory change has occurred, it has been left substantially to employers and managers to work out integration details at the local/store level.6,7
In Ontario, the scope of practice for RPTs includes accepting telephone orders for verbal prescriptions (with the exception of narcotics, controlled drugs, benzodiazepines and targeted substances), providing prescription transfers and checking of prescriptions for dispensing accuracy (e.g., correct patient, prescriber, dosage form, route of administration and directions for use).8 Given the large amount of time these activities require, the availability of RPTs within a community setting should release time for pharmacists to perform direct patient care activities more appropriately aligned with their evolving scope of practice, provided RPTs have in fact been optimally integrated within their workplaces and can actually work to the full extent of their scope of practice.
Objective
The objective of this exploratory study was to examine strategies to facilitate integration of RPTs into community pharmacy practice in Ontario, in a manner that would support optimal scope of practice for RPTs.
Methods
This study was exploratory in nature and used a qualitative method for data collection and analysis. As little was known about this subject, particularly in the context of Ontario, one-on-one interviews with community pharmacists and RPTs were identified as the most effective way to gather data. A semistructured interview protocol was used (Appendix 1, available in the online version of the article), designed to elicit participants’ experiences with RPT integration and their beliefs regarding facilitators and barriers to optimizing scope of practice of RPTs in community pharmacy.
Inclusion criteria for this research included 1) either a pharmacist or RPT, registered in good standing with the Ontario College of Pharmacists (OCP); 2) working a minimum of 24 hours/week in community pharmacy; and 3) minimum 1 year of experience working in a community practice setting with 1 or more RPTs on staff.
A purposeful snowball sampling method was used for this research. Initially, the OCP provided a shortlist of pharmacists/pharmacies as potential key informants to begin recruitment. Further recruitment occurred by accessing the publicly available OCP website to identify pharmacies that employed RPTs, then approaching them directly with a request to participate in this research. Finally, the online social networking tool LinkedIn was used as for recruitment, by searching the Ontario database for individuals self-declaring as “regulated pharmacy technician” as their occupation. As individuals were approached to participate in this research, they were also asked to nominate other peers/individuals they knew who they thought might also be interested in participating in this work.
All interviews were audiotaped with field notes and transcriptions made subsequent to the interview. In the event the participant elected not to be recorded, real-time field notes were maintained. Iterative coding was undertaken, using a method for qualitative content analysis in case study research described by Yin.9 Preliminary coding was completed after each interview to help inform subsequent interviews and further refinement of the coding structure. Interviews continued until saturation of themes was identified. All participants completed informed consent pursuant to a research protocol approved by the research ethics board.
Findings and discussion
A total of 28 individuals participated in this research (16 RPTs and 12 pharmacists; Table 1). All of the RPTs in this study indicated that they had initially worked as unregulated or certified pharmacy assistants prior to undertaking the RPT designation; all had completed the designation through an approved bridging education program. All of the pharmacists who participated in this study indicated they had previous experiences working with both regulated technicians and unregulated assistants.
Table 1.
Demographic characteristics of participants
| Pharmacists:Regulated pharmacy technicians | 12:16 (total = 28) |
| Years of experience as regulated pharmacy technician (RPT) | 2.7 ± 1.4 years |
| Number of RPTs who were assistants prior to regulation | 16/16 (100%) |
| Number of RPTs who remained in the same store after becoming regulated | 12/16 (75%) |
| Years of experience of pharmacists | 8.1 ± 3.5 years |
| Percentage of participants who worked in environment with at least 1 RPT | 28/28 (100%) |
All participants in this study indicated that the initial promise of regulation of pharmacy technicians in Ontario remained substantially unfulfilled and that in most cases, RPTs’ day-to-day responsibilities included a large number of pharmacy assistant–level activities (Table 2). A key variable in determining the extent of RPT-vs-assistant activities appeared to be the staffing ratio in the pharmacy with respect to the prescription volume: busier pharmacies with lower staffing ratios appeared to push RPTs toward assistant-level activities more frequently. Where higher ratios existed and where workload was somewhat lower or more predictable, there appeared to be greater likelihood of RPTs performing activities commensurate with their education and training.
Table 2.
Typical activities undertaken by regulated pharmacy technicians participating in this study
| Blister pack checking | 16/16 (100%) |
| Dispensed prescription checking | 16/16 (100%) |
| Taking verbal (telephone) prescriptions | 16/16 (100%) |
| Transferring prescriptions to another pharmacy | 16/16 (100%) |
| Pharmacy assistant tasks (e.g., cash register, preparing/filling prescriptions, managing inventory, dealing with third-party payer issues, prescription order entry, etc.) | 16/16 (100%) |
| Medication reconciliation post hospital discharge | 2/16 (12.5%) |
| Providing patient education on medical/health devices | 2/16 (12.5%) |
| Screening patients for adherence issues/adherence monitoring | 2/16 (12.5%) |
| Screening suitable patients for or undertaking best possible medication history | 2/16 (12.5%) |
| Managing refill request processes (e.g., initiating faxes to MD offices for refills) | 2/16 (12.5%) |
Four key themes emerged in this study related to strategies/tactics that appeared to optimize the role of the regulated pharmacy technician in community practice:
1. Environmental strategies
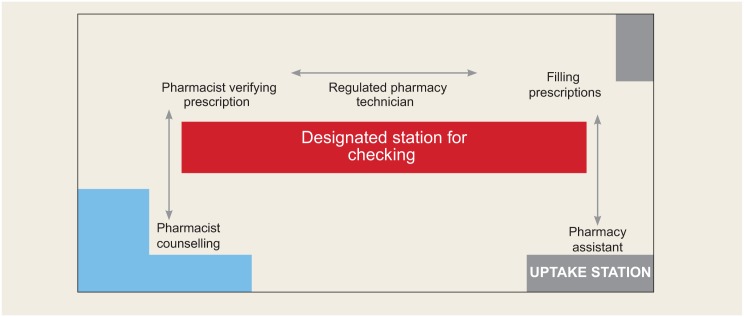
The physical environment/layout of the pharmacy was identified by all participants as a crucial predictor of successful integration. Physical layout was a particular concern: several studies had previously identified the physical layout of community pharmacies as being a potential barrier to delivery of direct patient care services, but none had focused on RPTs in particular. One important design feature highlighted by many participants involved a dedicated/designated workstation for RPTs that provided some measure of privacy or insulation from distraction/disruption:
We have a designated station and a computer for me to do the checking part of the prescriptions, along with other functions like taking doctors’ prescriptions over the phone and prescription transfer. (RPT)
The way the workflow is set up keeps the technician in reach of assistants from one way and pharmacists from the other way. (RPT)
The linear design of our pharmacy makes the workflow very smooth. (RPT)
Virtually all participants in this study highlighted the importance of physical layout and design of the pharmacy as a way to optimize workflow, enhance efficiencies and minimize disruptions. Several participants compared the workflow design to the renovation of a kitchen, noting how important placement of key “appliances” (such as a computer or a packaging machine) within the environment was to optimize workflow. Most participants agreed that a linear layout with an RPT situated in the middle—in close reach of both pharmacy assistants and pharmacists—placed the RPT in a strategic location to best perform functions smoothly and efficiently (Figures 1 and 2).
Figure 1.
Traditional dispensing layout in community pharmacy practice and the bottlenecks that may occur due to the physical design and placement of computers, dispensing stations, etc.
Figure 2.
Model for workflow in community pharmacy practice that could enhance operational efficiencies by segregating activities and personnel in a more effective way to minimize disruptions and distractions
Another environmental strategy that was identified as important to successful integration of RPTs involved staffing ratios that are appropriate for prescription volumes:
Having a pharmacy assistant is needed to allow me to practise to full scope. If the pharmacy assistant fills prescriptions, then I can check them. On the days when we don’t have an assistant, then I will be doing most of the assistant job. (RPT)
While it is difficult to accurately define an “appropriate staffing ratio,” most participants in the study suggested that a ratio of 1:1:1 (pharmacist:RPT:assistant) with a daily prescription volume of 150 to 200 seemed reasonable. Coupled with this staffing ratio is the need for careful schedule planning to incorporate technicians at times of peak volume, to allow for optimal utilization of their skills:
Scheduling is very important. The pharmacy manager needs to know when it is best to have an RPT working. I work weekdays only but not on weekends, based on the [store’s] prescription volume. (RPT)
2. Interpersonal strategies
With the introduction of RPTs, an entirely new team dynamic has been evolving in community pharmacy practice, particularly due to potential overlapping/redundant functions shared by both RPTs and pharmacists. A recent study suggested that this may produce conflict within the pharmacy team based on role ambiguity and a desire for “turf protection.”10
Participants in this study highlighted the importance of effective management practices within the pharmacy to support integration of RPTs. A key aspect of this involved clear role definitions for pharmacists, RPTs and assistants and clear boundaries around who does what:
The head office and management here planned my function very well. I have my own computer and workstation here, with specific tasks during the shift. This reduces confusion and chaos during busy hours. (RPT)
Pharmacists need to be aware of the scope of practice of RPTs in order to avoid duplication of work such as checking the technical aspects of the prescription. (RPT)
Participants in this study noted the importance of reinforcing role definition over time, as staff changes within community pharmacy are common:
We identified roles and responsibilities for each pharmacy staff early on, after having an RPT on board. This seems small but it was very significant to avoid stepping on each other’s toes and reduce friction among different players. This will need to be reinforced every time we have someone new joining the team—some pharmacists are still unfamiliar with the RPT’s scope of practice and what they are capable of doing. (Pharmacist)
Some participants in this study reported frustration with the lack of trust displayed by some pharmacists as to their competencies, particularly since there is sufficient evidence2,4,7 to confirm that accuracy rates of technicians in checking prescriptions are at least similar (if not superior) to pharmacists:
It can be frustrating when you have to reestablish this trust every time you work with a new pharmacist. (RPT)
Importantly, lack of trust was not raised as a significant, common issue for all or most participants in this study, and virtually all participants agreed that as the profession progresses through this current transition phase, this issue of trust will become even less significant.
3. Professional identity formation
All of the RPTs in this study appeared to be strong advocates for their evolving profession and were optimistic about the growth of the role now and in the future:
We are still new to this, so pharmacists don’t know how to trust me yet, but this [means we must] prove ourselves and show what we can do. At the end, I’m accountable for my work. I was fortunate to have an opportunity to train with another regulated pharmacy technician who was practising to full scope and who inspired me to push for my new role after being regulated. Training is very important because it will allow you to see what other successful regulated pharmacy technicians are doing. (RPT)
While optimism about the future of the RPT profession was strong, there were concerns expressed by many participants about the current state of professionalism:
I see other technicians struggle after getting regulated and then stay in the same store. It seems so much harder on these technicians to establish a new role. (RPT)
I know they say we are professionals—and I would like to feel like I am—but I don’t think that’s the way anyone else sees it. We are glorified assistants right now, which is frustrating because, in school, you learn so much about the potential of the role and I don’t think there are enough of us [RPTs] who feel like we are professionals yet to get others to wake up and notice us. (RPT)
If we don’t see ourselves as a worthy profession, who else will? It makes me sad that there are so many of us out there who got regulated because we had to, the employers forced us, or whatever, not because we thought we were actually real professionals who could make a difference. Until that changes, we won’t be professionals no matter what label we are given. (RPT)
The notion that incomplete professional identity formation among RPTs is a potential barrier to successful integration in the role raises important questions regarding modelling, mentoring, socialization and education and requires further examination. Several participants noted the significance of incomplete professional identity formation in day-to-day work as an RPT:
It’s a problem, right? If you don’t think you’re a professional then some of the things, the decisions you need to make as an RPT, you’re just going to bump it back to the pharmacist, then they [the pharmacists] get frustrated and wonder, what’s the point of a regulated technician? You need to be able to make decisions, be accountable, take responsibility like a professional, you know, like if you have to decide how to manage dispensing when you have limited supply in stock, or deal with changes in a patient’s insurance, stuff like that. You need to be able to handle it on your own, like a professional or what’s the point? (RPT)
4. Innovative strategies for delegation of tasks utilizing new skills
Participants in this study, particularly pharmacists, noted that there are important tasks that RPTs could potentially take responsibility for that are not currently part of their scope of practice. These participants noted that the knowledge and skills required to successfully complete RPT registration requirements translate into other areas beyond prescription checking. Some specific additional areas for expansion of RPT scope of practice discussed by participants included:
A. Adherence screening programs: The process of identifying patients at high risk for adherence issues is both important and time-consuming. It is also somewhat proceduralized, involving asking patients questions regarding their real-world experience of taking medications and carefully documenting responses. Both pharmacists and technicians indicated that a more formalized adherence screening program in community pharmacy, built on the work of RPTs, could be a significant value to patients and pharmacists if it were to become a more common part of practice. Pharmacists in particular noted that they know they should be more diligent in adherence screening activities but currently experience time pressures that make this challenging.
B. Medication reviews: The best possible medication history (BPMH) is the foundation for many important pharmacy services, including MedsCheck, medication synchronization and seamless care/transitions of care activities between hospital and home. RPTs may be in a strong position to support the work of pharmacists by taking greater responsibility for BPMH and medication review lists, leaving the pharmacists to undertake the actual assessment and problem-solving activities associated with these roles.
C. Training on devices: Increasingly, devices such as glucometers, peak flow meters, spirometers and ovulation detection kits are important in community pharmacy practice. Currently, education on use of these devices is left mainly to pharmacists, although there may be opportunities for expanded roles for RPTs in these areas.
D. Releasing refills before therapeutic double-check by pharmacist: One of the more controversial recommendations/strategies suggested by both pharmacists and technicians in this study related to the timing of release of prescriptions checked by RPTs.
The fact that we are still not able to release refills before they are therapeutically checked by the pharmacist is still a major hiccup because the refill prescriptions still pile up and can’t be released to the patient before they are reviewed by the pharmacist. In an ideal world, this could be done later on, since the patient has been taking this medication already. If the technician’s scope of practice expands to be able to release refills before they are seen by the pharmacist, then the whole pharmacy setup could be changed to have 2 lanes—one for refills that are entirely done by technicians at the moment and another lane for new prescriptions. (RPT)
Variants of this suggestion were made by both pharmacists and RPTs in this study, and most indicated that the true potential of RPTs to save time and improve efficiency in community practice will be attenuated until this change occurs. Importantly, proponents of this concept identified that it was controversial and would be deemed risky by some individuals and regulators, but in most cases, both pharmacists and RPTs indicated that in the current system, the therapeutic check provided by the pharmacist was perfunctory at best and did not warrant the logistical bottleneck it caused. This change, many participants reasoned, would truly expand the role of RPTs and revolutionize the current workflow for the ultimate benefit of patients, with minimal risks for patients:
We all know that pharmacists are supposed to be doing this therapeutic double-check on refill prescriptions, but honestly it just doesn’t happen like that. If I’m doing the therapeutic double-check, I might as well do the dispensing double-check, so it makes the [RPT’s] role kind of redundant. I know [the regulatory body] thinks it is safer or whatever if pharmacists do that therapeutic double-check, but actually it interferes with the whole efficiency of the process. If they would just let [RPTs] handle the whole refill process from start to finish—then you’d really see the whole thing take off and honestly, you wouldn’t see any greater or fewer therapeutic errors as a result. (Pharmacist)
The unique role of the pharmacist in ensuring therapeutic appropriateness of all medications used by patients is well established; ongoing monitoring of drug therapy is integral to the care provided by pharmacists. Ensuring, for example, that patients are not experiencing (or are appropriately managing) side effects of medications requires a pharmacotherapeutic knowledge base and skill set that is aligned with the education and training of pharmacists. Pharmacists have a unique opportunity during the refill process to engage in conversation with patients around therapeutic response, management of side effects, potential drug interactions and other topics of importance. While a completely independent technician-run refill pathway may have some immediate appeal in terms of operational efficiency, it must be balanced against the potential loss associated with the ongoing monitoring and follow-up roles that are an essential part of the patient care process and that are uniquely associated with pharmacists’ scope of practice.
Limitations
While this study aimed to establish factors that could enhance successful integration of RPTs in community practice, it is important to note some limitations. As a qualitative exploratory study, the data are based on a relatively small sample size, although this sample did have both pharmacists and RPTs, and the themes that emerged from the research were based on saturation of findings. The purposeful snowball sampling technique used in this study was effective at identifying interested and enthusiastic participants but means that participants in this study may not be indicative of the pharmacy population in Ontario and are not statistically representative. The face-to-face interview method without corroboration or triangulation to confirm veracity of what participants said and claimed with respect to “successful” integration may also be a limitation. Despite these potential limitations, as exploratory research, this work has potential for applicability within community pharmacy and points to future areas for research, especially related to formation of professional identity within the regulated technician community.
Conclusions
This exploratory study has identified strategies and tactics that may be useful to unleash the potential of regulated pharmacy technicians in the community pharmacy workforce. The 4 themes identified provide important information for managers, educators, pharmacists and regulators to provide supports to facilitate greater use of RPTs to the fullest scope of practice possible. Further, ongoing research into the evolution of the RPT profession is needed to support continuous enhancement of their role and potential to enhance patient care in community pharmacy.
Supplemental Material
Supplemental material, CPH765892_Appendix for Facilitating integration of regulated pharmacy technicians into community pharmacy practice in Ontario: Results of an exploratory study by Luna Salameh, Daniel Yeung, Natali Surkic, Paul Gregory and Zubin Austin in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada
Footnotes
Author Contributions:L. Salameh and D. Yeung were responsible for initial drafting of the manuscript, data collection and primary data analysis. N. Surkic was responsible for data collection and preliminary data analysis. P. Gregory revised the manuscript and was responsible for data collection and primary data analysis. Z. Austin initiated and supervised the project and was responsible for design/methodology and final drafting of the manuscript.
Declaration of Conflicting Interests:The authors have no conflict of interests to declare.
Funding:The authors gratefully acknowledge the funding and support of the Ontario College of Pharmacists for this research.
References
- 1. Jones W, Rutter PM. The introduction of a checking technician programme in community pharmacy and its impact on pharmacist activities. Int J Pharm Pract 2002;10(suppl):R90. [Google Scholar]
- 2. Adams AJ, Martin SJ, Stolpe SF. “Tech-check-tech”: a review of the evidence of its safety and benefits. Am J Health Syst Pharm 2007;68:1824–33. [DOI] [PubMed] [Google Scholar]
- 3. Beney J, Bero LA, Bond C. Expanding the roles of outpatient pharmacists: effects on health services utilization, costs and patient outcomes. Cochrane Database Syst Rev 2000;3:CD000336. [DOI] [PubMed] [Google Scholar]
- 4. Quigley and Watts Public Health Specialists. Evaluation of the pharmacy checking technician demonstration site project. Ministry of Health; Available: https://www.psnz.org.nz/Folder?Action=View%20File&Folder_id=114&File=NZ%20PACT%20Framework%20%20Version%202.0%2003%2003%2017.pdf (accessed Jun. 1, 2017). [Google Scholar]
- 5. Lester C, Chui M. Using link analysis to explore the impact of the physical environment on pharmacist tasks. Res Social Admin Pharm 2016;12(4):627–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Angelo LB, Ferreri SP. Assessment of workflow redesign in community pharmacy. J Am Pharm Assoc 2005;45(2):145–50. [DOI] [PubMed] [Google Scholar]
- 7. Klammer GA, Ensom RJ. Pharmacy technician refill checking: safe and practical. Can J Hosp Pharm 1994;47:117-9, 122–3. [PubMed] [Google Scholar]
- 8. Ontario College of Pharmacists. Understanding what a pharmacy technician can do. Available: www.ocpinfo.com/practice-education/practice-tools/support-materials/technician-role/ (accessed Jun. 1, 2017).
- 9. Yin R. Case study research, design and methods. 3rd ed. Thousand Oaks (CA): Sage; 2003. [Google Scholar]
- 10. Gregory P, Austin Z. Conflict in community pharmacy practice: the experience of pharmacists, technicians and assistants. Can Pharm J (Ott) 2016;150(1):32-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, CPH765892_Appendix for Facilitating integration of regulated pharmacy technicians into community pharmacy practice in Ontario: Results of an exploratory study by Luna Salameh, Daniel Yeung, Natali Surkic, Paul Gregory and Zubin Austin in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada