Figure 4.
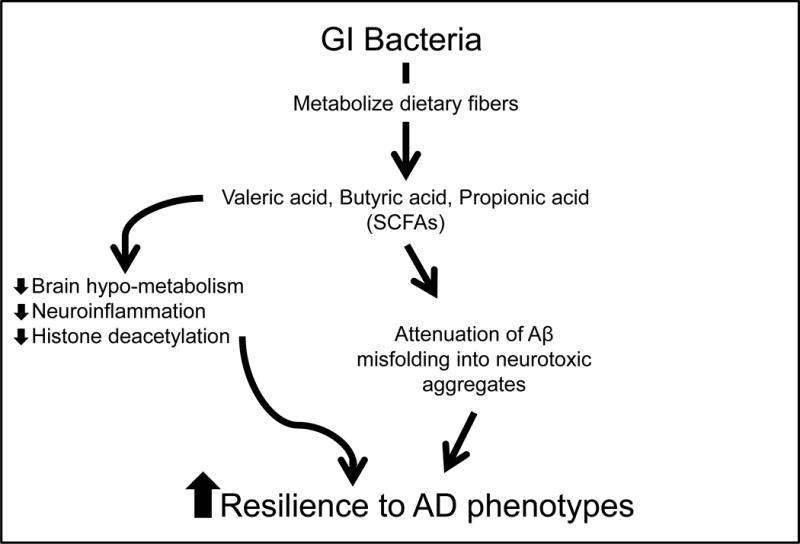
Schematics summarizing the mechanisms by which GI microbial-derived SCFAs may modulate AD. Intestinal bacteria help protect against AD by converting dietary fibers into biologically available SCFAs, which may promote resilience to AD through multiple cellular/molecular mechanisms. Previously published evidence suggests SCFAs may benefit AD by: (1) alleviating brain hypo-metabolism as SCFAs provide alternative substrates for brain energy metabolism [20], (2) attenuating neuro-inflammation by modulating the maturation and function of microglia in the brain [5], and (3) inhibiting histone deacetylases and normalize aberrant histone acetylation in the AD brain [7,14,34]. In addition, evidence from the present study suggests that certain SCFAs, particularly valeric acid, butyric acid, and propionic acid, may also benefit AD by attenuating Aβ-mediated pathologic processes by interfering with the assembly of Aβ1-40 and Aβ1-42 peptides into neurotoxic Aβ aggregates.
