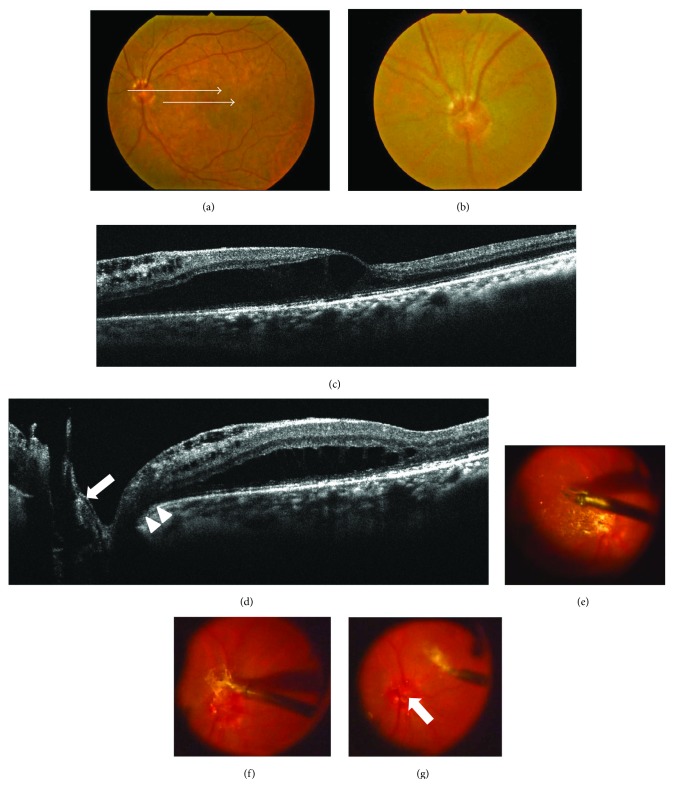
Figure 3.
Photographs of the left eye in a 70-year-old patient with maculopathy in whom an optic disc coloboma became clear after surgery with epipapillary membrane removal (case 4). (a, b) Fundus photographs before surgery showing macular elevation (a) and a shallow cavitation in the center of the optic disc (b). Upper and lower arrows indicate the spectral domain optical coherence tomography (SD-OCT) scan in Figures 3(c) and 3(d), respectively (a). (c, d) SD-OCT images before surgery showing retinal schisis extending from the optic disc to the macula (c), with membrane tissue but with no obvious pit-like deep cavitation on the disc (d, arrow), and a shallow tunnel-like hyporeflective lesion directly connecting the retinal schisis to the disc (d, arrowheads). (e–g) Findings during pars plana vitrectomy. Internal limiting membrane (ILM) at the area from the macula to the surrounding of the disc was peeled (e). ILM connected the membrane tissue on the optic disc (f). When the epipapillary membrane tissue was removed, a pit-like concavity, which was hidden behind the tissue, appeared (g, arrow).