Abstract
Foreign body ingestion is common in infants and young children and can cause numerous complications, mainly if ingested and left in place for prolonged periods. In recent years, particular dangers, specifically from ingested button batteries, have become increasingly recognized as a public health issue. Of particular note is the rapid onset of full thickness burns and oesophageal perforation which may occur within as little as 2 h following the ingestion of button batteries. The aim of this review is twofold: (1) to increase awareness of the need for rapid action from radiologists, emergency care physicians and paediatricians on identifying a button battery impacted within the oesophagus, and (2) to review the imaging appearances that can distinguish button batteries from other similar appearing foreign bodies, most notably coins.
Introduction
Foreign body ingestion is a common occurrence in young children and infants and can cause injury through several different mechanisms.1 The most common mechanism of injury, from most foreign bodies, is simply the result of prolonged pressure effects of the foreign body, which, because the original event was not witnessed, can remain in situ for weeks or months. In a 5-year retrospective review of cases referred to a tertiary paediatric gastroenterology service in Romania, the most commonly ingested foreign bodies were coins (26%), with batteries comprising 6.6% of their cohort.1 Button batteries, unlike all other ingested foreign bodies, can cause catastrophic injuries (such as a tracheal-oesophageal fistula or a fatal oesophago-aortic fistula) within hours of ingestion. Additionally, when inserted into the nose, button batteries may cause not only mucosal injuries but also have been reported to result in nasal septal perforations, nasal adhesions and saddle nose deformity.2
A study by Sharpe et al identified an annual incidence of 3300 battery-related emergency department attendances in the USA between 1990 and 2009.3 Impaction of button batteries results in formation of a local external current between the positive and negative poles of the battery, which has been shown to rapidly cause hydrolysis and hydroxide formation, leading to clinically significant burns and oesophageal perforation within as little as 2 h of ingestion. Ingestion of newly purchased (and, therefore, fully charged) batteries is of particular concern.4
Although an examination of the National Poison Data System, published in 2010 by Litovitz et al, suggested the incidence of battery ingestion over a period of 24 years, between 1985 and 2009, was steady (varying between an annual incidence of 6.3 and 15.1 cases per million population), it also demonstrated a worrying 4.4-fold increase in clinically significant events and a 6.7-fold increase in major or fatal outcomes over the final 3 years compared to the initial 3 years of their study. They identified 13 fatalities and 73 major complications. The diagnosis was initially missed in 7 of the fatal cases and 19 of the cases with major complication, most often through failure of recognition that foreign body ingestion had occurred at all. Perhaps more significantly to radiologists, 4.5% of ingested batteries in the significant harm group were initially misdiagnosed as ingested coins on radiography.4 It is, therefore, critical that general practitioners, paediatricians and emergency care physicians maintain a high level of suspicion whenever a foreign body is encountered and that radiologists are able to assist in recognizing the features that distinguish an impacted coin from a similar appearing, but much less benign, button battery that requires rapid emergency removal.
The button battery explained
Button batteries can be found in an increasing number of electronic devices, both those you might expect (watches, remote controls and car keys) and more surprising items such as musical greetings cards.5
Externally, they are composed of two metallic discs. The larger, flat surface stamped with a code is the cathode and the smaller surface the anode.6
A database of button batteries available in the UK (found at http://www.watchbattery.co.uk) contains more than 85 different types, powered by alkaline, silver oxide, mercury and lithium cores. They vary in size from 4.8 to 30 mm in diameter and 1.2 to 16 mm in height. The code stamped on the flat surface (e.g. CR2032) defines its chemistry (C = lithium), shape (R = round), diameter (20 = 20 mm) and height (32 = 3.2 mm) (Figure 1 and Table 1).
Figure 1.

A 3V CR2032 button battery compared with a 2 pence coin.
Table 1.
Battery codes from http://www.watchbattery.co.uk
| Code | Battery chemistry |
|---|---|
| BR/CR | Lithium |
| L | Alkaline |
| SR | Silver oxide |
| LR | Alkaline |
| SG | Silver oxide |
| AG | Alkaline |
The review by Litovitz et al identified 20-mm diameter button batteries as the cause of 92% of major and fatal outcomes (70% CR2032, 20% CR2025).4
Methods of injury
Numerous mechanisms of injury have been described, including leakage of alkaline battery content, heavy metal ingestion and local pressure trauma/ischaemic necrosis, but the most important mechanism is reported to be electrolytic production of alkaline fluid via formation of a local circuit by oesophageal tissue contacting both the anode and cathode.7
A practical experiment, designed as a demonstration tool for use at public health awareness events, uses a piece of thinly sliced meat (e.g. ham), folded over a button battery, as a model of a battery lodged within a child’s oesophagus. As shown in the recreation below, a black ring-shaped burn appears after only 5 min. A crackling sound can be heard from the moment the ham is folded over the battery (Figure 2).5 After 2 h, there is a hole in the meat at the point closest to the battery’s anode. This is in keeping with the findings of Tanaka et al who described the positioning of the greatest damage in button batteries lodged in the oesophagus of dogs.8 A video of this experiment and patient experiences can be found at https://youtu.be/q5ApVlDCEjc.
Figure 2.
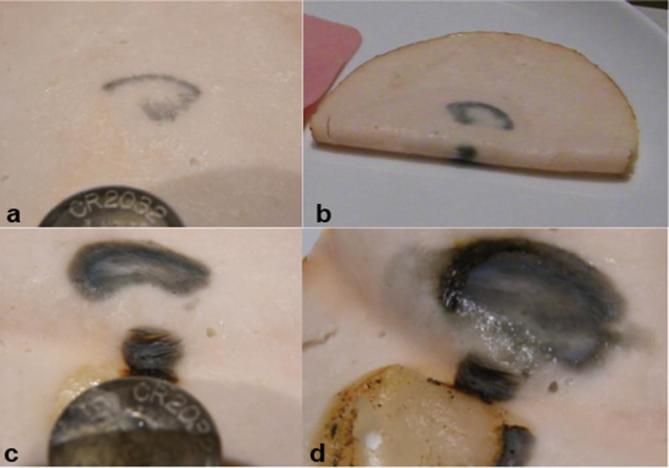
A variation of the button battery demonstration as described in Online fact sheet: Safekids Aotearoa. Button battery injuries—a demonstration plan for practitioners (Aukland: Safekids Aotearoa available at http://www.safekids.nz/Safety-Topics/Details/Type/View/ID/13957/Button-Battery#accordionFive). A button battery is placed onto a slice of cooked meat (in this case a slice of chicken approximately 2 mm in thickness), which is then folded over to simulate the battery contacting both sides of a child’s oesophagus. After just 5 min, there is discolouration of the meat extending the full thickness of the slice (a - inner surface, b - outer surface, at 5 mins) After 2 h (c), there is a defect extending through the full thickness of the slice. Note that the worst damage is at the anode and the folded portion immediately between anode and cathode (d). An audible crackling sound can be heard from the moment the meat is first folded over.
The narrowest parts of the oesophagus, and therefore the most common sites of impaction, are the thoracic inlet, the region of the aortic arch and at the gastro-oesophageal junction.9
Consistent with local electrical current formation being the major cause of morbidity, Litovitz et al describe a 3.2-fold increase in clinically significant outcomes in instances of ingestion of a new battery compared to spent batteries. All clinically significant events occurred in children who ingested 20–25 mm cells (as apposed to 15–18 mm cells) with 12.6% of children under 6 years ingesting 20–25 mm battery cells experiencing a major complication or death.4
Radiographic appearance
A frontal radiograph should demonstrate the so-called “double rim” or “halo” sign which distinguishes a button battery from a coin (the latter appearing solid) (Figure 3), although there is a case report of a false-positive halo sign following ingestion of two coins which stacked together immediately superior to the gastro-oesophageal junction.10 Where there is clinical doubt, a tangential lateral projection may demonstrate the “step-off” of the smaller diameter anode as it projects from the battery (Figure 3), although it should be noted that there are very thin batteries available where the step off is too small to be discerned via radiography (these do not generally stay lodged in the oesophagus).11 As described above, the anode is the site of the greatest damage and, as such, its position may also predict subsequent complications.12
Figure 3.
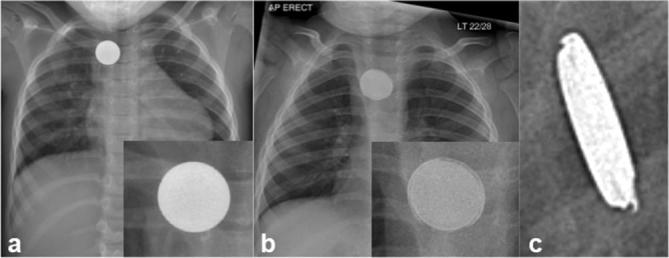
Frontal chest radiographs of two infants presenting with foreign bodies lodged in the oesophagus at the level of the aortic arch (magnified inset). (a) Round object, solid from edge to edge—2p coin. (b) Round object with peripheral “double rim” or “halo”—button battery. (c) The “step-off” of the smaller negative pole is demonstrated on a lateral projection radiograph.
Complications and management options
Reported complications from button battery impaction include fatal exsanguination via aorto-oeosophageal fistulation, formation of trachea-oesophageal fistulae (Figure 4), oesophageal and tracheal stenoses, vocal cord paralysis, empyema and spondylodiscitis.4,13,14
Figure 4.
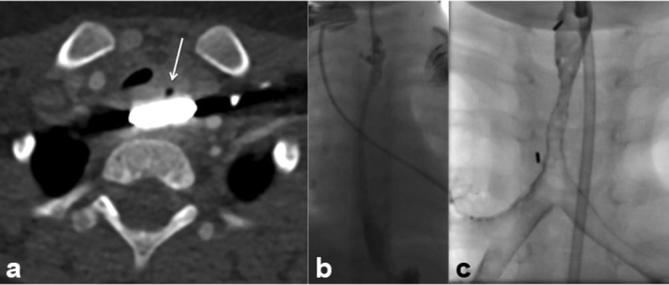
(a) CT demonstrating a button battery lodged at the level of the thoracic inlet. Note the tiny focus of gas anteriorly. (b) Subsequent to removal, upper gastrointestinal contrast study of the same patient demonstrates a small diverticulum at the level of the previously impacted button battery. The patient underwent surgical repair. (c) A different patient with previous impaction of a button battery leading to tracheo-oesophageal fistula formation. The child underwent surgical repair, but required repeated post-operative tracheal dilatations for recurrent stricture formation, as demonstrated on this bronchogram.
If button battery ingestion is thought possible, plain radiography is advised to ascertain its location. The exception to this rule is in batteries known to be under 12 mm in diameter in children over 12 years (significant complications in this situation have been found to be rare). Smaller children warrant investigation even if asymptomatic. Batteries lodged in the oesophagus must be removed as soon as possible, ideally within 2 h.4
If the battery has passed the gastro-oesophageal junction, the majority will pass spontaneously, unless they have been swallowed alongside one or more magnets.15
Recognition of a battery in the oesophagus is a paediatric emergency. Recently published guidance from the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition advises emergent removal of button batteries lodged within the oesophagus and includes a recommendation for subsequent CT angiography or MRI to assess for aortic injury if oesophageal injuryis demonstrated on endoscopy.16 If there is a risk or concern that the battery has been in situ for some time, CT may be of value in demonstrating the site of the battery in relation to the major blood vessels. The presence of mediastinal air would be worrisome for oesophageal perforation and possible trachea-oesophageal fistula. However, in line with Pugmire et al, it is our practice to consider CT and MRI on a case-by-case basis.2
Conclusion
Foreign body ingestion is common in infants. Button battery ingestions pose a major risk, with more frequent and severe associated complications than other foreign bodies. Full thickness burns, oesophageal perforation, trachea-oesophageal and even oesophago-aortic fistulation are possible, within a few hours of ingestion.
An American task force document from 2013 recommends a radiograph be obtained immediately on presentation to assess for oesophageal position of an ingested button battery. Plain radiography in frontal and orthogonal projections allows differentiation of button batteries from similarly sized coins via the “double rim” or “halo” appearance and allows ascertainment of direction of the smaller diameter anode where the most severe damage occurs. In routine practice, however, a single frontal projection is usually sufficient. Given the possible false-negative lateral step-off appearance in very thin batteries, suspicion should remain high even in the absence of this sign and prompt removal of the foreign body performed.
With the necessary knowledge, radiologists can provide valuable assistance to emergency care and paediatric physicians in distinguishing ingested button batteries from coins and in investigating possible sequelae of button battery impaction.
Acknowledgement
The families of the children whose images are contained within this review gave consent for their inclusion.
Contributor Information
Thomas Semple, Email: tsemple@doctors.org.uk.
Alistair D Calder, Email: Alistair.Calder@gosh.nhs.uk.
Madhavan Ramaswamy, Email: Madhavan.Ramaswamy@gosh.nhs.uk.
Kieran McHugh, Email: Kieran.McHugh@gosh.nhs.uk.
References
- 1.Diaconescu S, Gimiga N, Sarbu I, Stefanescu G, Olaru C, Ioniuc I, et al. Foreign bodies ingestion in children: experience of 61 cases in a pediatric gastroenterology unit from Romania. Gastroenterol Res Pract 2016; 2016: 1–6. doi: 10.1155/2016/1982567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pugmire BS, Lin TK, Pentiuk S, de Alarcon A, Hart CK, Trout AT. Imaging button battery ingestions and insertions in children: a 15-year single-center review. Pediatr Radiol 2017; 47: 178–85. doi: 10.1007/s00247-016-3751-3 [DOI] [PubMed] [Google Scholar]
- 3.Sharpe SJ, Rochette LM, Smith GA. Pediatric battery-related emergency department visits in the United States, 1990–2009. Pediatrics 2012; 129: 1111–7. doi: 10.1542/peds.2011-0012 [DOI] [PubMed] [Google Scholar]
- 4.Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. Emerging battery-ingestion hazard: clinical implications. Pediatrics 2010; 125: 1168–77. doi: 10.1542/peds.2009-3037 [DOI] [PubMed] [Google Scholar]
- 5.Aotearoa S. Online fact sheet: Safekids Aotearoa. Button battery injuries - A demonstration plan for practitioners. 2016. [cited 21 December 2016] Available from: http://www.safekids.nz/Safety-Topics/Details/Type/View/ID/13957/Button-Battery#accordionFive
- 6.Laulicht B, Traverso G, Deshpande V, Langer R, Karp JM. Simple battery armor to protect against gastrointestinal injury from accidental ingestion. Proc Natl Acad Sci U S A 2014; 111: 16490–5. doi: 10.1073/pnas.1418423111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomson M, Sharma S. The hazards of button battery ingestion. Arch Dis Child 2015; 100: 1010–1. doi: 10.1136/archdischild-2015-308313 [DOI] [PubMed] [Google Scholar]
- 8.Tanaka J, Yamashita M, Yamashita M, Kajigaya H. Esophageal electrochemical burns due to button type lithium batteries in dogs. Vet Hum Toxicol 1998; 40: 193–6. [PubMed] [Google Scholar]
- 9.Mirshemirani A, Khaleghnejad-Tabari A, Kouranloo J, Sadeghian N, Rouzrokh M, Roshanzamir F, et al. Clinical evaluation of disc battery ingestion in children. Middle East J Dig Dis 2012; 4: 107–10. [PMC free article] [PubMed] [Google Scholar]
- 10.Gan RWC, Nasher O, Jackson PB, Singh SJ. Diagnosis of button battery ingestion by ‘halo’ radiographic sign: an exception to the rule. BMJ Case Rep 2015; 2015: 2015209908. doi: 10.1136/bcr-2015-209908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jatana KR, Litovitz T, Reilly JS, Koltai PJ, Rider G, Jacobs IN. Pediatric button battery injuries: 2013 task force update. Int J Pediatr Otorhinolaryngol 2013; 77: 1392–9. doi: 10.1016/j.ijporl.2013.06.006 [DOI] [PubMed] [Google Scholar]
- 12.Shakir NT, Pollock AN. Battery ingestion. Pediatr Emerg Care 2014; 30: 72–3. doi: 10.1097/PEC.0000000000000081 [DOI] [PubMed] [Google Scholar]
- 13.Simonin M, D'Agostino I, Lebreton M, Jughon O, Hamza J, Oualha M. Bilateral vocal palsy following coin cell lithium battery ingestion: a case report and review. Eur J Pediatr 2013; 172: 991–3. doi: 10.1007/s00431-012-1899-x [DOI] [PubMed] [Google Scholar]
- 14.Kieu V, Palit S, Wilson G, Ditchfield M, Buttery J, Burgner D, et al. Cervical spondylodiscitis following button battery ingestion. J Pediatr 2014; 164: 1500–1500.e1. doi: 10.1016/j.jpeds.2014.02.016 [DOI] [PubMed] [Google Scholar]
- 15.el-Barghouty N. Management of disc battery ingestion in children. Br J Surg 1991; 78: 247–247. doi: 10.1002/bjs.1800780239 [DOI] [PubMed] [Google Scholar]
- 16.Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen TC, et al. Management of Ingested Foreign Bodies in Children. J Pediatr Gastroenterol Nutr 2015; 60: 562–74. doi: 10.1097/MPG.0000000000000729 [DOI] [PubMed] [Google Scholar]


