Abstract
INTRODUCTION
Postoperative cerebrospinal fluid (CSF) leak is a serious complication following transsphenoidal surgery for which elevated body mass index (BMI) has been implicated as a risk factor, albeit only in two recent North American studies. Given the paucity of evidence, we sought to determine if this association holds true in an Asian population, where the BMI criteria for obesity differ from the international standard.
METHODS
A retrospective study of 119 patients who underwent 123 transsphenoidal procedures for sellar lesions between May 2000 and May 2012 was conducted. Univariate and multivariate logistic regression analyses were performed to investigate the impact of elevated BMI and other risk factors on postoperative CSF leak.
RESULTS
10 (8.1%) procedures in ten patients were complicated by postoperative CSF leak. The median BMI of patients with postoperative leak following transsphenoidal procedures was significantly higher than that of patients without postoperative CSF leak (27.0 kg/m2 vs. 24.6 kg/m2; p = 0.018). Patients categorised as either moderate or high risk under the Asian BMI classification were more likely to suffer from a postoperative leak (p = 0.030). Repeat procedures were also found to be significantly associated with postoperative CSF leak (p = 0.041).
CONCLUSION
Elevated BMI is predictive of postoperative CSF leak following transsphenoidal procedures, even in an Asian population, where the definition of obesity differs from international standards. Thus, BMI should be considered in the clinical decision-making process prior to such procedures.
Keywords: Asian, body mass index, cerebrospinal fluid leak, transsphenoidal surgery
INTRODUCTION
Postoperative cerebrospinal fluid (CSF) leak is a well-known complication following transsphenoidal surgery for sellar lesions, with a reported incidence in the range of 8.6%–15.9%.(1-4) Its occurrence may result in meningitis, and prolonged treatment or reparative surgery are required in some patients.
Obesity is increasingly prevalent in the world today. This phenomenon holds true in Singapore as well. An association between elevated body mass index (BMI) and the occurrence of postoperative CSF leak has been suggested, but only recently and in just two studies,(4,5) both of which had North American populations. We sought to investigate whether this relationship held true in our local multiracial Asian population when using Asian-specific criteria for BMI that were adopted by the medical practice in Singapore.
METHODS
All 147 patients who underwent 151 transsphenoidal procedures for sellar lesions at the Department of General Surgery, Ng Teng Fong General Hospital, Singapore, between 1 May 2000 and 31 May 2012 were eligible for study. Patients with incomplete data sets, insufficient anthropometric data and those who underwent surgery for an extrasellar pathology were excluded (Fig. 1). 119 patients who underwent a total of 123 procedures were included in the final analysis.
Fig. 1.
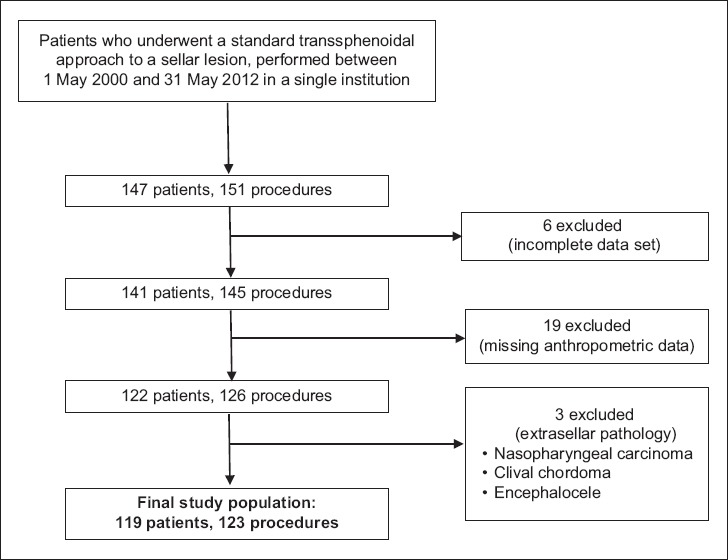
Flowchart shows the inclusion and exclusion criteria used for patient selection.
The study was approved by the hospital institutional review board. Both inpatient and outpatient medical records were retrospectively reviewed. Patient demographics and anthropometric data were recorded. Patients were categorised based on both the World Health Organization (WHO) international and Asian BMI classifications (Fig. 2). BMI data was further stratified to create three- and two-tiered classifications. In the three-tiered classification, patients who were underweight or normal (at low risk) were categorised as ‘acceptable’ and were compared with patients who were overweight and obese (at moderate risk and high risk, respectively) according to the Asian BMI criteria. In the two-tiered classification, overweight and obese patients comprised one group that was compared to the acceptable group, which included underweight and normal-weight patients.
Fig. 2.
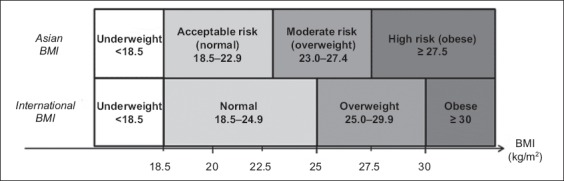
Chart shows differences in threshold between the World Health Organization’s international and Asian body mass index (BMI) classifications.
Histopathological diagnoses, methods of sellar repair or reconstruction, and data on intraoperative and postoperative CSF leaks were recorded. The occurrence of intraoperative leaks was determined by reviewing patients’ operative records. Postoperative leak was determined as the presence of CSF rhinorrhoea on clinical examination following surgery.
The surgeries were performed by eight different surgeons at our institution. Surgeons were free to choose the method of initial access toward the sphenoid sinus – either transnasal or sublabial – but all procedures were performed using a standard transsphenoidal approach (i.e. none of the procedures had expanded approaches). Various combinations of autologous and non-autologous grafts were used for the repair or reconstruction of the sellar floor. This included fascia lata, fat, remnant bone from the sellar opening and equine collagen biomatrix (TissuDura®, Baxter AG, Vienna, Austria). Fibrin sealant (Tisseel® fibrin sealant; Baxter Healthcare, Deerfield, IL, USA) was commonly used as reinforcement. For some endonasal procedures, the use of a vascularised nasoseptal mucosal flap was also an option. All except 18 procedures were performed using an operating microscope. For 18 transsphenoidal surgeries, visualisation was aided by the use of an endoscope via a transnasal approach, with assistance from an otorhinolaryngologist.
Patients were divided into two groups based on the presence or absence of postoperative CSF leak. Wilcoxon rank-sum and Fisher’s exact tests were used to compare these patient groups for continuous and dichotomous variables, respectively. Factors such as ethnicity, BMI, the use of endoscope, intraoperative CSF leak, repeat procedures and methods of sellar repair were examined in a series of univariate analyses. Multivariate regression analysis based on a stepwise approach was also performed, including univariate analyses with p < 0.20 as the cut-off for inclusion in the final adjusted model. Statistical analysis of the data was performed using IBM SPSS Statistics version 20 (IBM Corp, Armonk, NY, USA). A p-value < 0.05 was considered as statistically significant.
RESULTS
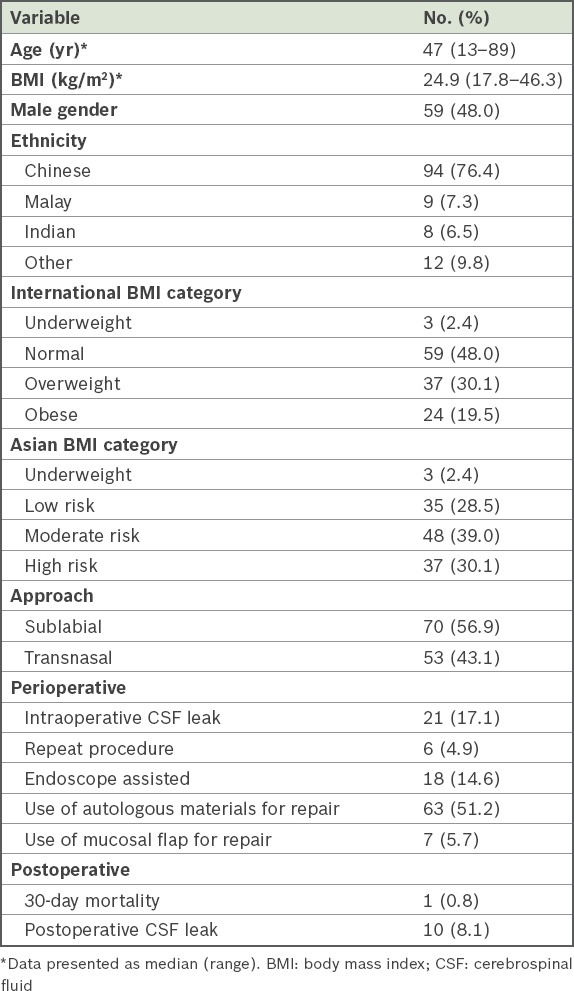
A total of 123 transsphenoidal surgeries for sellar repair were performed for 119 patients, among which 59 (48.0%) procedures were performed on men (Table I). The median age of the patients during surgery was 47 (range 13–89) years. A majority of the procedures (76.4%) were performed on patients of Chinese ethnicity, consistent with Singapore’s population, which is predominantly Chinese.
Table I.
Demographic details of patients who underwent transsphenoidal procedures (n = 123).
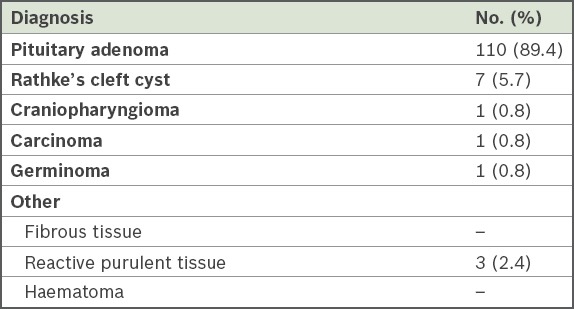
Pituitary adenoma (89.4%) was the most common histopathological diagnosis noted in our study, accounting for nearly nine in every ten procedures (Table II). Six patients underwent repeat procedures, which was defined as surgery on a patient who had undergone a previous similar procedure within any period of time, but not within the same admission and without clinical evidence of CSF leak prior to the reviewed surgical procedure.
Table II.
Histopathological diagnoses of patients who underwent transsphenoidal procedures (n = 123).
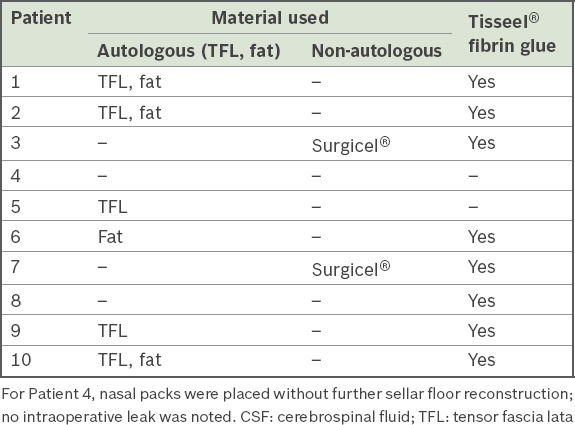
10 (8.1%) procedures in ten patients were complicated by postoperative CSF leak. The closure technique varied in this group, with different combinations of materials used for the reconstruction and repair of the sellar floor (Table III). Two of the ten patients required reparative surgery, while the remaining eight patients were successfully managed using measures such as bed rest in a flat supine position, repeated lumbar punctures or insertion of a lumbar drain.
Table III.
Types of material used for sellar floor reconstruction in patients with postoperative CSF leak (n = 10).
1 (0.8%) patient died on the 20th postoperative day due to intracranial bleeding at the operative site complicated by hydrocephalus and cerebral infarction, which did not improve despite ventriculostomy. Another patient (0.8%) developed postoperative meningitis, which occurred despite the absence of postoperative CSF leakage. She was successfully treated using intravenous antibiotics.
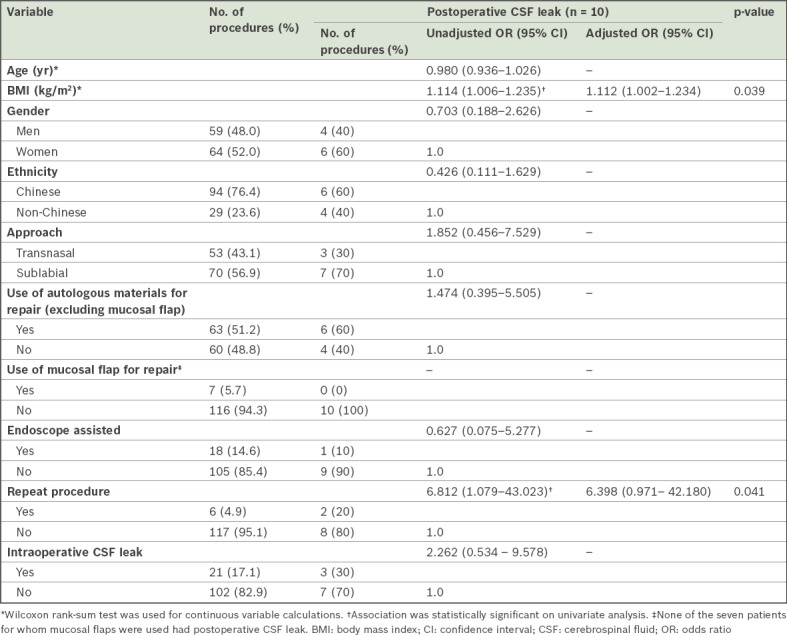
No significant difference was noted between patients with and without postoperative CSF leak with regard to gender, age and ethnicity (Table IV). The median BMI of patients with postoperative leak was significantly greater than that of patients without postoperative leak (27.0 kg/m2 vs. 24.6 kg/m2; p = 0.018). There was a trend toward increased occurrence of postoperative leak with increasing obesity, which was observed when patients were categorised using both the WHO international (p = 0.192) and Asian BMI (p = 0.176) classifications. This association was more pronounced when compared using the well-established three-tiered classification (international: p = 0.096; Asian: p = 0.084), although it did not reach statistical significance. None of the patients classified as acceptable under the Asian BMI three-tiered classification developed postoperative CSF leak (Fig. 3). When stratified using the two-tiered Asian BMI classification, we found that all patients who had postoperative CSF leak were of at least moderate risk (100.0%). Among patients who did not develop postoperative leak, this percentage was lower, with only about two-thirds (66.4%) being categorised as moderate and high risk; this difference in the proportion of moderate- and high-risk procedures among patients with and without postoperative CSF leak was found to be statistically significant (p = 0.030).
Table IV.
Demographic data of patients stratified by the presence or absence of a postoperative CSF leak.
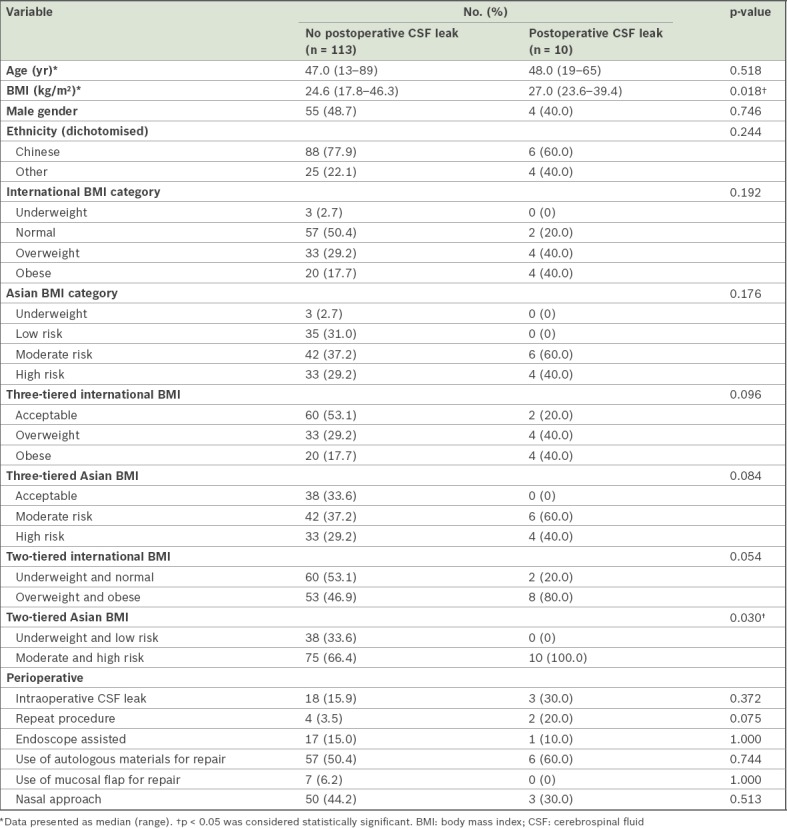
Fig. 3.
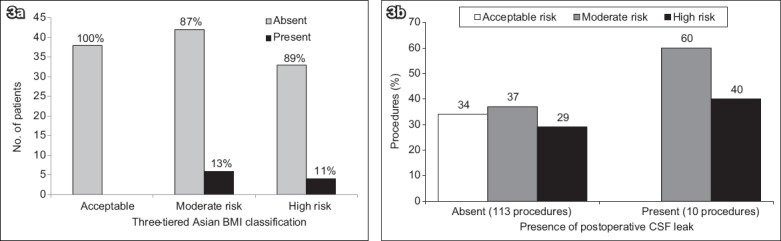
Charts show (a) the occurrence of postoperative CSF leak stratified by the three-tiered Asian BMI classification, and (b) the association between Asian BMI categories and the occurrence of postoperative CSF leak. BMI: body mass index; CSF: cerebrospinal fluid
Repeat procedures were found to be associated with increased risk of postoperative CSF leak on univariate analysis (p = 0.041; Table V). The occurrence of intraoperative leak (p = 0.268), use of endoscope (p = 0.668), transnasal approach (p = 0.389) and the use of autologous materials for repair or reconstruction of the sellar floor (p = 0.564) were all not statistically significant on univariate analysis in relation to the occurrence of postoperative CSF leak following transsphenoidal procedures (data not shown).
Table V.
Univariate and multivariate analysis of risk factors for postoperative CSF leak.
DISCUSSION
The transsphenoidal approach to lesions in the sella turcica has seen many advances throughout the last century. Hirsch and Cushing were pioneers of the technique in the early 1900s,(6) and Hardy was credited with popularising the technique again in the 1960s with the use of the operating microscope and the advent of antibiotics,(7) reducing complication rates arising from CSF leak and meningitis, which had plagued this procedure a few decades earlier. More recently, the use of endoscopes, which was popularised in the 1990s by Carrau et al,(8) is playing an increasingly important role in current practice, offering superior visualisation compared to the traditional microscope. Despite these advances, the risk of postoperative CSF leak following transsphenoidal surgeries remains a significant complication with potentially severe morbidity and mortality, particularly for infection in the form of meningitis.
Obesity is a major cause of morbidity and mortality in developed countries, including Singapore. The WHO introduced an international classification for obesity in 1995, which was termed as BMI.(9) The year 2004 saw the introduction of a specific BMI range for determining public health and clinical action in Asian populations, in recognition of the health risks posed at lower BMI values in this population.(10) Data from the latest National Health Survey revealed that 23.0% of Singaporean adults were in the high-risk group under the Asian BMI classification. Moreover, the trend of obesity in Singapore has been increasing steadily, with age-standardised prevalence rising from 6.3% in 1998 to 10.8% in 2010.(11)
Obesity is purported to be a significant risk factor for the occurrence of spontaneous CSF rhinorrhoea.(12-14) It has also been linked to raised intracranial pressure in various metabolic(15-17) and mechanical theories,(18,19) and is a recognised risk factor in the setting of idiopathic intracranial hypertension.(15,20) More recently, observations by Dlouhy et al(4) and Ivan et al(5) have suggested an association between obesity and increased risk of postoperative CSF leak following transnasal anterior skull base approaches. The exact pathophysiology is uncertain, but it is likely that the associations between elevated BMI and spontaneous CSF leak and between obesity and intracranial hypertension share a similar pathogenesis, with sustained elevated intracranial pressure eventually resulting in dehiscence of the sellar reconstruction following surgery.(4)
We found a significantly higher median BMI among patients with postoperative CSF leak following transsphenoidal procedures, compared with those without. Notably, this result, while consistent with that of Dlouhy et al, is from a multiracial Asian population. Our rate of postoperative CSF leak (8.1%) was lower than the 13.5% reported in the earlier study. This may be partly attributed to the lower median BMI observed in our Asian study population (BMI 27.0 kg/m2) as opposed to the North American population in Dlouhy et al’s study (BMI 39.2 kg/m2).(4)
Repeat procedures were found to be associated with an increased risk of postoperative CSF leak. This was not unexpected given the obvious difficulties resulting from the alterations in anatomy and surgical planes following the initial surgery, and the subsequent increased risk of intraoperative leak. Contrary to the findings by Ivan et al,(5) we did not find a significant relationship between the occurrences of intraoperative and postoperative leaks. This observation could have been due to unintentional bias when operating surgeons made greater efforts to ensure a good repair following an intraoperative leak. Given the small number of patients in the present study, however, the strength of correlations drawn between BMI and postoperative CSF leak following transsphenoidal procedures remains weak. Our study results should thus be interpreted with caution.
Various techniques have been described with regard to sellar reconstruction following a transsphenoidal approach, differing in the type of materials used and the manner in which they are utilised (e.g. tiered or combination repairs).(21,22) Reconstruction methods varied widely in our study due to the number of surgeons involved. The usage of autologous materials in the form of fascia lata or fat was analysed, given its historical importance as the earliest effective method of sellar reconstruction, as described by Dandy(23) and Collins,(24) but no significant correlation was found with respect to postoperative CSF leak.
The vascularised nasoseptal flap, first described by Hadad et al,(25) has become increasingly popular, with recent literature suggesting that its use could reduce the incidence of postoperative CSF leak when compared to mucosal-free grafts.(3,26,27) Our study included only a small proportion (5.7%) of patients who had undergone a nasoseptal flap repair. Although none of these patients developed postoperative CSF leaks, the small sample size limits us from making any firm inferences regarding its usefulness in reducing the occurrence of postoperative CSF leak subsequent to transsphenoidal procedures among patients with elevated BMI. Given what we understand from the current literature, however, it would be reasonable to consider the use of such flap repair, in conjunction with meticulous surgical technique, in order to minimise the risk of postoperative CSF leak in higher-risk patients, such as those with elevated BMI.
To the best of our knowledge, this is the largest study to consider the relationship between elevated BMI and the occurrence of postoperative CSF leak following transsphenoidal procedures – an association that has only been described in recent years and in just two previous articles. Furthermore, this is the only study that has specifically focused on an Asian population while considering region-specific criteria for BMI.
This study was not without limitations. We acknowledge the inherent bias that is associated with any retrospective method of data retrieval and analysis. Other limitations, such as the heterogeneity of the lesional pathology, surgical approach, and the technique and method of sellar reconstruction, may also dilute the strength of any potential correlation drawn between BMI and the incidence of postoperative CSF leak in these patients. Given the relatively low incidence of this complication, a larger sample size would help to increase the overall power of the study, including correlations between CSF leak and other risk factors during subgroup analysis.
In conclusion, elevated BMI has been shown to be a significant predictor for postoperative CSF leak following transsphenoidal surgery. This holds true even in an Asian population when region-specific BMI measures are applied, showing the strength of this association across diverse populations. Larger prospective studies are warranted to further validate this relationship.
ACKNOWLEDGEMENT
The authors would like to thank Ms San Moe Thu, Department of Surgery, NUS Yong Loo Lin School of Medicine, National University of Singapore, Singapore, for her role in facilitating the statistical analysis. This work was presented as a poster at the ASEAN (Association of Southeast Asian Nations) Neuroscience 2015 meeting held in Singapore in July 2015.
REFERENCES
- 1.Senior BA, Ebert CS, Bednarski KK, et al. Minimally invasive pituitary surgery. Laryngoscope. 2008;118:1842–55. doi: 10.1097/MLG.0b013e31817e2c43. [DOI] [PubMed] [Google Scholar]
- 2.Zhan R, Chen S, Xu S, Liu JK, Li X. Postoperative low-flow cerebrospinal fluid leak of endoscopic endonasal transsphenoidal surgery for pituitary adenoma--wait and see, or lumbar drain? J Craniofac Surg. 2015;26:1261–4. doi: 10.1097/SCS.0000000000001691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassam AB, Prevedello DM, Carrau RL, et al. Endoscopic endonasal skull base surgery: analysis of complications in the authors'initial 800 patients. J Neurosurg. 2011;114:1544–68. doi: 10.3171/2010.10.JNS09406. [DOI] [PubMed] [Google Scholar]
- 4.Dlouhy BJ, Madhavan K, Clinger JD, et al. Elevated body mass index and risk of postoperative CSF leak following transsphenoidal surgery. J Neurosurg. 2012;116:1311–7. doi: 10.3171/2012.2.JNS111837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ivan ME, Iorgulescu JB, El-Sayed I, et al. Risk factors for postoperative cerebrospinal fluid leak and meningitis after expanded endoscopic endonasal surgery. J Clin Neurosci. 2015;22:48–54. doi: 10.1016/j.jocn.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 6.Lanzino G, Laws ER., Jr Pioneers in the development of transsphenoidal surgery: Theodor Kocher, Oskar Hirsch, and Norman Dott. J Neurosurg. 2001;95:1097–103. doi: 10.3171/jns.2001.95.6.1097. [DOI] [PubMed] [Google Scholar]
- 7.Liu JK, Das K, Weiss MH, Laws ER, Jr, Couldwell WT. The history and evolution of transsphenoidal surgery. J Neurosurg. 2001;95:1083–96. doi: 10.3171/jns.2001.95.6.1083. [DOI] [PubMed] [Google Scholar]
- 8.Carrau RL, Jho HD, Ko Y. Transnasal-transsphenoidal endoscopic surgery of the pituitary gland. Laryngoscope. 1996;106:914–8. doi: 10.1097/00005537-199607000-00025. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva: World Health Organization; 1995. [PubMed] [Google Scholar]
- 10.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health Singapore. [Accessed January 31 2016];National Health Survey 2010. Available at: https://www.moh.gov.sg/content/moh_web/home/Publications/Reports/2011/national_health_survey2010.html . [Google Scholar]
- 12.Lindstrom DR, Toohill RJ, Loehrl TA, Smith TL. Management of cerebrospinal fluid rhinorrhea: the Medical College of Wisconsin experience. Laryngoscope. 2004;114:969–74. doi: 10.1097/00005537-200406000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Dunn CJ, Alaani A, Johnson AP. Study on spontaneous cerebrospinal fluid rhinorrhoea: its aetiology and management. J Laryngol Otol. 2005;119:12–5. doi: 10.1258/0022215053222833. [DOI] [PubMed] [Google Scholar]
- 14.Banks CA, Palmer JN, Chiu AG, et al. Endoscopic closure of CSF rhinorrhea:193 cases over 21 years. Otolaryngol Head Neck Surg. 2009;140:826–33. doi: 10.1016/j.otohns.2008.12.060. [DOI] [PubMed] [Google Scholar]
- 15.Ooi LY, Walker BR, Bodkin PA, Whittle IR. Idiopathic intracranial hypertension: can studies of obesity provide the key to understanding pathogenesis? Br J Neurosurg. 2008;22:187–94. doi: 10.1080/02688690701827340. [DOI] [PubMed] [Google Scholar]
- 16.Abdollahi M, Cushman M, Rosendaal FR. Obesity: risk of venous thrombosis and the interaction with coagulation factor levels and oral contraceptive use. Thromb Haemost. 2003;89:493–8. [PubMed] [Google Scholar]
- 17.Lampl Y, Eshel Y, Kessler A, et al. Serum leptin level in women with idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry. 2002;72:642–3. doi: 10.1136/jnnp.72.5.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sugerman HJ, DeMaria EJ, Felton WL, 3rd, Nakatsuka M, Sismanis A. Increased intra-abdominal pressure and cardiac filling pressures in obesity-associated pseudotumor cerebri. Neurology. 1997;49:507–11. doi: 10.1212/wnl.49.2.507. [DOI] [PubMed] [Google Scholar]
- 19.Sugerman HJ, Felton WL, 3rd, Sismanis A, et al. Gastric surgery for pseudotumor cerebri associated with severe obesity. Ann Surg. 1999;229:634–40. doi: 10.1097/00000658-199905000-00005. discussion 640-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sugerman HJ, Felton WL, 3rd, Salvant JB, Jr, Sismanis A, Kellum JM. Effects of surgically induced weight loss on idiopathic intracranial hypertension in morbid obesity. Neurology. 1995;45:1655–9. doi: 10.1212/wnl.45.9.1655. [DOI] [PubMed] [Google Scholar]
- 21.Cappabianca P, Cavallo LM, Esposito F, Valente V, De Divitiis E. Sellar repair in endoscopic endonasal transsphenoidal surgery: results of 170 cases. Neurosurgery. 2002;51:1365–71. discussion 1371-2. [PubMed] [Google Scholar]
- 22.Couldwell WT, Kan P, Weiss MH. Simple closure following transsphenoidal surgery. Technical note. Neurosurg Focus. 2006;20:E11. doi: 10.3171/foc.2006.20.3.12. [DOI] [PubMed] [Google Scholar]
- 23.Dandy WE. Pneumocephalus (intracranial pneumatocele or aerocele) Arch Surg. 1926;12:949–82. [Google Scholar]
- 24.Collins WF. Hypophysectomy: historical and personal perspective. Clin Neurosurg. 1974;21:68–78. doi: 10.1093/neurosurgery/21.cn_suppl_1.68. [DOI] [PubMed] [Google Scholar]
- 25.Hadad G, Bassagasteguy L, Carrau R, et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116:1882–6. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- 26.McCoul ED, Anand VK, Singh A, et al. Long-term effectiveness of a reconstructive protocol using a nasoseptal flap after endoscopic skull base surgery. World Neurosurg. 2014;81:136–43. doi: 10.1016/j.wneu.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 27.Park JH, Choi JH, Kim YI, Kim SW, Hong YK. Modified Graded Repair of Cerebrospinal Fluid Leaks in Endoscopic Endonasal Transsphenoidal Surgery. J Korean Neurosurg Soc. 2015;58:36–42. doi: 10.3340/jkns.2015.58.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]


