Abstract
Background
A growing body of research continues to elucidate health inequities experienced by transgender individuals and further underscores the need for medical providers to be appropriately trained to deliver care to this population. Medical education in transgender health can empower physicians to identify and change the systemic barriers to care that cause transgender health inequities as well as improve knowledge about transgender-specific care.
Methods
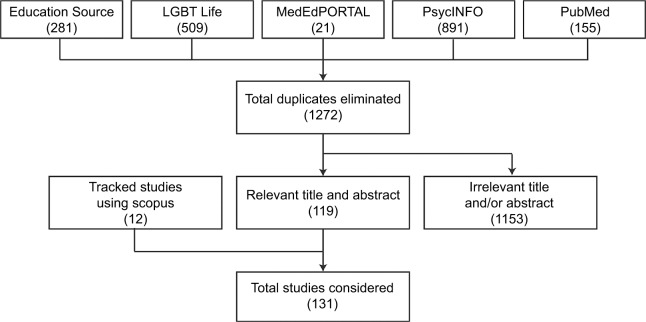
We conducted structured searches of five databases to identify literature related to medical education and transgender health. Of the 1272 papers reviewed, 119 papers were deemed relevant to predefined criteria, medical education, and transgender health topics. Citation tracking was conducted on the 119 papers using Scopus to identify an additional 12 relevant citations (a total of 131 papers). Searches were completed on October 15, 2017 and updated on December 11, 2017.
Results
Transgender health has yet to gain widespread curricular exposure, but efforts toward incorporating transgender health into both undergraduate and graduate medical educations are nascent. There is no consensus on the exact educational interventions that should be used to address transgender health. Barriers to increased transgender health exposure include limited curricular time, lack of topic-specific competency among faculty, and underwhelming institutional support. All published interventions proved effective in improving attitudes, knowledge, and/or skills necessary to achieve clinical competency with transgender patients.
Conclusion
Transgender populations experience health inequities in part due to the exclusion of transgender-specific health needs from medical school and residency curricula. Currently, transgender medical education is largely composed of one-time attitude and awareness-based interventions that show significant short-term improvements but suffer methodologically. Consensus in the existing literature supports educational efforts to shift toward pedagogical interventions that are longitudinally integrated and clinical skills based, and we include a series of recommendations to affirm and guide such an undertaking.
Keywords: medical education, transgender, LGBT health, medical training, residency
Introduction
In recent decades, the field of lesbian, gay, bisexual, transgender, and queer (LGBTQ) health has become a national priority.1,2 Transgender individuals face unique health care concerns. The term transgender, as it is used here, includes people whose gender identity differs from their sex assigned at birth as well as those whose gender identity does not confirm to conventional binary gender categories known as gender nonbinary or gender nonconforming.3 Some transgender people may undergo medical interventions, such as hormone therapy (eg, estrogen and testosterone) and gender-affirming surgeries to attain physical characteristics that better align with their gender identity. Data from national surveys estimate that ~1 million Americans’ identity as trans-gender.4 A growing body of research continues to elucidate health inequities experienced by transgender individuals1,2,5,6 and further underscores the need for medical providers to be appropriately trained to deliver care to this population. Research has shown that transgender populations experience significant health disparities such as a disproportionately higher burden of mental health illness, including increased rates of depression, anxiety, and suicide.7,8 Human immunodeficiency virus (HIV) infection is notably higher in transgender populations, especially transgender women.9–11 Poorer health outcomes are partially caused, and further compounded, by socioeconomic inequities, including higher rates of unemployment, poverty, legal discrimination, and harassment when compared with cisgender people (ie, those whose sex assigned at birth aligns with their gender identity).12,13
Notably, negative attitudes toward and lack of knowledge about transgender health have manifested in reports of transgender people being denied health care or experiencing discrimination, including verbal and physical abuse, in health care settings.14 Access to care is also affected by the lack of insurance due to poverty or unemployment and coverage denials based on categorization of medically necessary procedures such as “sex-specific”, “cosmetic”, and “experimental”.7,14–17 The Patient Protection and Affordable Care Act improved health care access for transgender Americans but did so incompletely and does not address the lack of physician training in transgender health care.18–22 Medical education that improves attitudes toward and awareness of transgender populations, provides knowledge of unique clinical concerns, and develops skills to deliver competent care is one tool for addressing transgender health inequities.23–25
A growing number of institutions have acknowledged the role of education in improving care for transgender individuals and have taken steps to address transgender health. However, they often do so under the larger umbrella of LGBTQ health inequities.26–28 An established body of research merits focusing on transgender health issues as a separate clinical skill set from lesbian, gay, and bisexual (LGB) health. Medical education in transgender health can empower physicians to identify and change the systemic barriers to care that contribute to transgender health inequities. It can also improve knowledge about transgender-specific care, such as hormone therapy, gender-affirming surgical procedures, high prevalence of gender dysphoria, and other mental health diagnoses such as depression and anxiety.14,29 Clinicians should be trained to recognize long-term health outcomes associated with gender-affirming interventions (eg, dyslipidemias associated with estrogens and erythrocytosis associated with testosterone) as well as make necessary modifications to preventive care interventions (eg, screening transgender women for breast cancer and osteoporosis).30 Transgender patients should have their sex assigned at birth and current anatomical inventory recorded within the medical record to facilitate appropriate timely delivery of preventive care interventions, as cancer screening needs to be based on existing anatomy.25
From systemic barriers to clinical competency, medical education has a foundational role in equipping physicians to address transgender health inequities. We outline various domains within the literature and describe where consensus or divergence of recommendations exists. We conclude with a discussion of previous research in this area and provide recommendations based on our findings.
Methods
We conducted structured searches of five databases (Education Source, LGBT Life, MedEdPORTAL, PsycINFO, and PubMed) to identify literature related to medical education and transgender health (Figure 1 and Supplementary material). Given the broad nature of this literature and varying methodologies of the studies included, our methodology is consistent with a scoping review.31 Search results were screened for relevancy and the following criteria: undergraduate and graduate, allopathic and osteopathic medical schools in North America published since January 1, 2000. We included publications of primary literature, reviews, opinion pieces, and policy papers to ensure a broad overview of the available literature. Of the 1272 papers reviewed, 119 papers were deemed relevant to these predefined criteria and the topics of medical education and transgender health. Citation tracking was conducted on the 119 papers using Scopus to identify an additional 12 relevant citations not retrieved in database searches (a total of 131 papers). Searches were completed on October 15, 2017 and updated on December 11, 2017.
Figure 1.
Search algorithm for articles on transgender health.
The nature of our analysis is transgender health education specific, yet many of our results captured LGBTQ-focused literature. Thus, our analysis focuses primarily on transgender- specific publications and utilizes LGBTQ health research with appropriate contextualization when needed to accurately identify existing transgender health education research.
Results
An emerging field with few best practices
Our literature search yielded letters to the editor, perspectives, response articles, assessments of curricular time allotment to transgender or LGBTQ health, and assessments of student attitudes and knowledge around transgender health. These were mostly focused on LGBTQ health as an aggregated population, with few explicit mentions of the need for educational efforts tailored to transgender topics.32–34 A considerable number of articles, even in the last few years, have called for increased inclusion of transgender health.34–38 They suggest that progress has yet to be made in including transgender health as an accepted component of health professional education. There were no explicit mentions of health topics specific to gender nonbinary populations.
These findings reveal that efforts toward incorporating transgender health into undergraduate and graduate medical educations are nascent. Such programs are sparse, with only 16% of Liaison Committee on Medical Education accredited academic practices reporting a comprehensive LGBTQ-competency training program; more than half (52%) report no LGBTQ training.39 Advocates for the inclusion of trans-gender medical education widely agreed that it should begin in medical school and continue through postgraduate training and be a part of continuing medical education, which has been endorsed by the American College of Physicians and echoed by other medical institutions.26,27,37,40,41 Advocates also agreed that innovations in transgender medical education are closely linked with advances in transgender and LGB health delivery, such as improvements in the collection of sexual orientation and gender identity data and increasing LGBTQ visibility and acceptance within medical institutions.37,42,43
Throughout these editorials, there is no consensus on the exact educational interventions that should be used to address transgender health. How to quantify curricular hours, account for the “hidden curriculum”, and advocate for increased transgender education are topics discussed without any agreement of best practices.34,35,42 As one recent discussion article said “Best practices and acceptable measures of evaluating trainings remains unknown”.34
Barriers to implementation and efficacy
Even in the setting of validated educational interventions, the authors of this body of literature agreed that problems will persist given limited curricular time, lack of topic-specific competency among faculty, and underwhelming institutional support. The educational resources that do exist are difficult to implement in the face of these formidable barriers. Authors emphasize the challenges of providing faculty competent in transgender health. Some note that having self-identified LGBTQ faculty does not equate pedagogic or clinical competency in LGB or transgender health issues.32 Ultimately, as tools to measure educational outcomes are developed, the authors agreed on the importance of parallel efforts in faculty development, competency, and support to create the human capital for transgender medical education.34,44,45
If interventions are implemented, the discrete (ie, onetime) nature of many educational interventions is a ubiquitous setback to pedagogical efficacy. A review of LGBTQ educational interventions found that the average intervention consisted of only one to two lectures and roughly half had a component involving patient interaction.46 Because these were broad LGBTQ interventions, even less time was likely devoted to transgender topics. Structural setbacks to intervention assessments included that as many as a half were optional (resulting in potential for selection bias), response bias, short-term nature of assessments, and lack of research that evaluates the comparability of scales used in different intervention assessments.46,47
Assessing the current state of transgender medical education
The actual quantification of curricular hours devoted to transgender health must be extrapolated from the small number of studies that looked at LGBTQ health as a whole. There are few studies that attempt to quantify curricular hours and those that have used varying methods and have disparate conclusions. One recent study, which is widely cited throughout the literature, found that there is considerable variation in LGBTQ health curricula between US medical schools; the mean curricular time throughout medical school was 5 hours, with 6.8% reporting zero preclinical hours and 33.3% reporting zero hours during clinical years.48 The most frequently taught topics were broadly LGBTQ relevant, such as sexual orientation, HIV, gender identity, and safer sex; transgender-specific topics, such as transitioning and gender-affirming procedures or surgeries, were among the least frequently addressed.48 Regarding transgender health specifically, 74% of medical students’ report receiving <2 hours of curricular time devoted to transgender clinical competency.49 Another study found that postgraduate year 1 and 2 trainees report a median of 22 hours of LGBTQ-related content in their undergraduate curricula, with the most time devoted to HIV, safe sex, and differences of sex development, but is unclear to what extent any of these 22 hours were transgender specific or related.50 This same study found that 93% of respondents reported delivering medical care to less than five transgender patients and 40% cared for zero transgender patients during undergraduate training.50 Despite varying study methodologies, transgender health has yet to gain widespread curricular exposure.
Lack of transgender health education is reflected by students’ lack of awareness and knowledge surrounding transgender health. Of all LGBTQ topics, transgender health is the least well understood. A survey of Boston University students’ knowledge and attitudes about LGB and transgender patients reported that compared with LGB health knowledge, comfort and knowledge about transgender patients were much lower.51 A larger, interschool survey echoed the same finding, reporting that transgender-specific knowledge topics, such as those surrounding gender-affirming surgeries, were the worst understood of all LGBTQ health topics.52 These results, contextualized alongside several studies that more robustly demonstrate lower comfort and knowledge regarding LGBTQ patients as a whole when compared with straight and cisgender patients, elucidate the current state of transgender health when disaggregated from LGBTQ health.53–56
The literature reviewed notes that transgender health competency is generally poor, but precise characterization of medical student competency in transgender health is difficult given limitations cited by the literature. Very few studies directly assessed medical student attitudes about transgender patients or knowledge about transgender health issues. Only two such studies were found, both online surveys that asked medical students to subjectively report their own attitudes and knowledge about transgender health.51,52 No objective assessments of transgender-specific attitudes, knowledge, or clinical skills could be found. One survey in 2017 assessed medical students at Boston University and another in 2015 assessed students at 170 US allopathic and osteopathic schools (4262 responses of possible 9522). However, the latter study reports on data collected in 2010, limiting conclusions that can be drawn regarding students’ current attitudes and knowledge given the notable increase in transgender-related media coverage and political attention since its publication. Therefore, characterization of medical students’ current transgender health competency largely depends on a single study of students at a single institution.
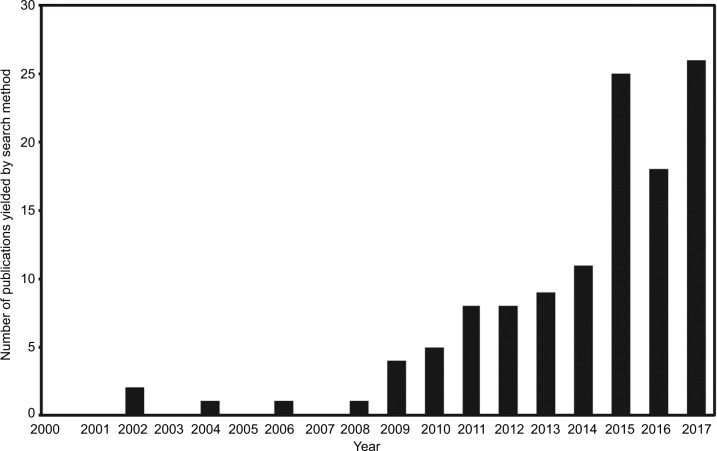
Current publication trends (eg, 5 in 2010 and 25 in 2015) (Figure 2), especially in the larger context of LGBTQ education, indicate that while remaining sparse, the publication rate of literature addressing transgender health competency and education has accelerated greatly in recent years. The literature acknowledges a motivation for change. In one survey of Canadian medical students, 95% found transgender issues important to their health care education.57 This transgender-specific trend is consistent with the overall trend in LGBTQ health education attitudes in the literature. In one large survey of 132 medical school deans, 76% rated their own LGBTQ curricula as “fair” or “poor”, with only 24% rating it as “good”.48 A smaller survey reported that medical students acknowledged a lack of LGBTQ health education and valued its inclusion in the larger health curriculum.58 A survey of clerkship and course directors at the University of Louisville expressed a desire to almost double curricular time devoted to LGBTQ health.59 Thus, while motivation for increasing transgender health education cannot currently be well-characterized given the difficulty of disaggregating transgender education from the umbrella of LGBTQ health, the literature reveals an increasing identification of interest in increasing both transgender-specific and LGBTQ health education.
Figure 2.
Publication rate on transgender medical education.
Undergraduate medical education interventions
A combination of factors limits consensus on best practices for how to structure pedagogical interventions to address transgender health education. These factors include a paucity of published studies, the heterogeneity of educational interventions and assessment metrics, and the short-term nature of outcome measurements. The general format of interventions varies widely, including their location in the curriculum, duration, and grouping within LGBTQ lectures or as discrete, transgender-specific interventions.
A salient finding of our review is the general dearth of literature regarding transgender health education, even in the setting of a rise in LGBTQ education. Although 26 studies published data on LGBTQ curriculum in some capacity, only eight (31%) studies included transgender-specific content (Table 1).58,60–66 Zero papers addressed health concerns specific for nonbinary populations. The majority of LGBTQ studies identified did not disaggregate transgender health issues from the larger LGBTQ umbrella in assessments of interventions. Given the unique social considerations and medical needs of transgender patients, the literature on transgender medical education is limited by the predominant approach that aggregates transgender and LGB populations.
Table 1.
Relevant studies on transgender-related health topics in medical school
| Authors | Year | N | Total time | Placement in curriculum | Format | Outcomes |
|---|---|---|---|---|---|---|
| Braun et al64 | 2017 | 46 | Up to 10 hours | Variable | Optional lunch-hour electives | Increased knowledge of: Transgender terminology (78–87% correct, P<0.01) SOGI data collection (50–89% correct, P<0.01) Awareness of DSM-V gender dysphoria diagnosis (15–59% correct, P<0.01) Gender-affirming medications (47–58% correct, P<0.01) Primary care for transgender people (57–81% correct, P<0.01) Federal policies (26–34% correct, P<0.01) Reduced transphobia (15.9–14.1 on a 45-point scale with higher scores indicating increased transphobia, P<0.05) |
| Dowshen et al60 | 2013 | 150 | 1 hour | Family medicine clerkship | Mandatory module | Increased knowledge of: Difference between sexuality and gender concepts (P<0.05) Poor population health outcomes in transgender communities (P<0.001) Increased comfort with sexual history, examination, and laboratory evaluation (P<0.0001) Ability to discuss hormone therapy (P<0.01) Ability to identify appropriate resources and transgender-friendly practices (P<0.0001) |
| Eriksson and Safer63 | 2016 | 121 | 1 hour | MS1 | Mandatory lecture | Increased knowledge of: Etiology of gender identity (14–80% correct, P<0.001) (N=43) Gender identity as a durable biologic phenomenon (63–93% correct, P<0.001) Gender identity, transgender medicine, and recognition of cross-sex hormone therapy as a valid treatment (20–50% correct, P<0.001) (N=56). |
| Grubb et al61 | 2013 | 29 | 2 hours | – | Mandatory module | Increased knowledge of: Presence of prostate status post-vaginoplasty (69–95% correct, P<0.05) Intersex anatomy examples (52–76% correct, P<0.05) |
| Safer and Pearce62 | 2013 | 66 | 1 hour | MS2, endocrinology | Curricular content | Decreased discomfort with treating trans male patients (38–12.5% uncomfortable, P<0.001) Decreased discomfort with treating trans female patients (38–14% uncomfortable, P = 0.0006) Decreased unwillingness to treat a trans male patient (18–3% uncomfortable, P = 0.02) Decreased unwillingness to treat a trans female patient (15–3% uncomfortable, P=0.02) Decreased belief that health care for trans males is not conventional medicine (7–0%) Decreased belief that health care for trans females is not conventional medicine (7–0%) |
| Sawning et al65 | 2017 | 39 | Variable, up to 11 hours | Variable | Optional lunch-hour electives | Increased beliefs that: Same sex behavior is normal (74–90%, P=0.019) Transgender identities are normal (77–85%, P=0.037) |
| Sequeira et al58 | 2012 | 30 | 4 hours (3×1 hour lectures, 1 hour standardized patient encounter). 2 hours lecture was trans-specific |
MS1 and MS2 | Optional course: lectures and standardized patient encounter | Free-text responses that indicated increased trans competency A total of 90% reported learning something new and applicable about hormone replacement therapy |
| Vance et al66 | 2017 | 20 | 7 hours (2 hours module, 5 hours clinical observation) | Adolescent and young adult medicine clerkship | Online modules and clinical observation | Increased perceived knowledge and awareness of all aspects of transgender care assessed (for each of 20 measures, P<0.001) |
Abbreviations: SOGI, sexual orientation and gender identity; DSM-V, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; MS1, first-year medical student; MS2, second-year medical student.
Again, publication patterns within the literature speak both to the newness of the field and to a rapid growth in transgender health education interventions. While published findings on efforts to improve transgender health education are mostly from the last 5 years, more interventions are published each year. This acceleration is likely due to an increased visibility of transgender identities and health concerns and a well-documented push from residency directors, health educators, and students to expand LGBTQ health education broadly.59
These accelerating publication patterns are due in part to discrete, transgender-specific educational interventions, as well as transgender topics within a broader LGBTQ intervention.58,61,65 Given the limited number of studies, the literature lacked consensus as to which teaching strategy (aggregated with LGBTQ or separated as transgender only) is more effective at addressing attitudes, knowledge, and skill for transgender health. Authors that support discrete interventions argue that they allow more in-depth discussion of transgender health issues. Yet, citing the limited resources and time available for modifying curricula, some authors argue that the most feasible way to include transgender topics is to aggregate them with existing LGBTQ health education interventions.
The educational interventions used various formats including optional lunchtime discussion sessions, elective or mandatory didactic lectures, clinical observations, inter-clerkship week lectures, and online educational modules (Table 1).67 Interventions were placed in preclinical basic science curricula (eg, endocrinology curricular block), in doctoring courses geared at developing interview skills and bedside manner, or in family medicine or pediatrics clinical rotations. The duration of teaching time in studies also varied considerably with format of the intervention. Mandatory lectures were usually shorter, mostly 1 or 2 hours. Two of the optional interventions, both lunchtime discussion series, were much longer, with 10 or 11 hours of curricular content in total.64,65
While no consensus has been reached as to which pedagogical design was more effective, there was commonality in that all published interventions were associated with improving attitudes, knowledge, and/or skills necessary to achieve clinical competency with transgender patients. We outline here the specific findings in these learning domains.
Three educational interventions were associated with improved attitudes about transgender patients and their health care needs. Two series of optional lunchtime electives were associated with decreased transphobia and increased acceptance of transgender identities.64,65 Another intervention was associated with a 67% decrease in the number of students who felt uncomfortable treating transgender patients, as well as increased acceptance of transgender health care as “conventional medicine”.62
Three interventions were associated with increased knowledge of trans-specific social and political concepts that are important to transgender health care. An optional lunchtime series was associated with increased knowledge about federal policies impacting transgender health.64 A family medicine clerkship module was associated with knowledge about health disparities facing transgender patients, as well as basic concepts relevant to transgender and LGB health, like the distinction between sexuality and gender.60
Four interventions were associated with increased comfort and knowledge regarding sexual history taking, diagnosis of gender dysphoria, and transition-related treatment of transgender patients. An educational module included in the family medicine clerkship was associated with increased comfort with transgender sexual history taking, examination, and laboratory evaluation.60 Both an optional lunchtime series and a mandatory module were associated with increased awareness of transgender patients’ anatomy before and after gender-affirmation procedures.61,64 The lunchtime series was also associated with increased knowledge of gender dysphoria diagnoses and hormone therapy. Several interventions reported generally increased knowledge about transgender health care.63,64,66 The family medicine clerkship module was also associated with increased clinical performance when interacting with transgender patients; students improved their ability to discuss the hormone therapy and to identify the appropriate resources and transgender-friendly practices.60
Despite some significant increase in attitudes, knowledge, and/or skills, there were limitations noted. Authors consistently observed that while interventions proved effective when assessed in the short term, it cannot be determined whether short-term improvements are sustained. Most studies that assessed postinterventional knowledge did so immediately after the intervention. Authors frequently identified the need for long-term assessments but are limited by resources to conduct them. Additionally, authors frequently acknowledged the uncertainty in how documented short-term changes in attitudes, knowledge, or skills translate into improved clinical outcomes for transgender patients. There is agreement that long-term assessments of pedagogical interventions will elucidate which educational interventions are most effective in sustaining changes in attitudes, knowledge, and skills as well as pedagogical impacts on clinical outcomes.
Graduate medical education interventions
To our knowledge, this is the first review of graduate medical education literature regarding transgender health. Screening for title and abstract yielded 15 papers, which included surveys, reports on educational interventions, and editorials. Generally, there are fewer graduate publications on transgender medical education when compared with undergraduate. Specialties found in our search include psychiatry, internal medicine and family medicine, endocrinology, emergency medicine (EM), plastic surgery, otolaryngology, and urology.22,50,68–80 The residency specialties that had published the most were plastic surgery/urology and internal medicine.
There is a consensus that transgender-specific health education in both didactic and clinical settings is lacking. At the graduate level, there is often no didactic or clinical exposure, both for LGBTQ health in general and transgender health specifically. There were no data available on nonbinary health education. Where teaching exists, it is often minimal. These deficiencies are consistent across all specialties for which data exist. A 2015 dissertation on medical resident education on sexuality showed no education to minimal education about transgender patients (average score 1.55 of the 5, 0 representing no education) and 83.1% reporting minimal or no transgender health education during residency.81 The only graduate-specific EM study found that LGBTQ topics averaged a total of 45 minutes, which was not transgender specific.76 Surveys of plastic surgery and urology residents found that only 65 and 54% of respondents, respectively, had education on or direct exposure to transgender patient care during residency.78 The literature demonstrates a consistent underexposure to transgender health in both the graduate classroom and clinic.
Despite the increasing acceptance of the importance of graduate medical education addressing transgender health, attitudinal setbacks across specialties remain but are not necessarily ubiquitous. One survey of psychiatry residents in Canada found lower than expected rates of transphobia when compared with similar studies of undergraduate students.82 One study found variation in attitudes by geographic region, with south-eastern regions having more negative attitudes held by residency program directors regarding the importance of transgender health education.77 In one EM study, 16% of EM residency program directors did not support the inclusion of LGBTQ-specific education.76 As the effort to add transgender health to undergraduate curricula changes, the attitudinal landscape at the graduate level will likely shift dramatically and further documentation is warranted.
Interventions that address shortcomings in resident approaches to transgender health are primarily didactic or policy oriented. Discrete, transgender-specific didactics for internal medicine and family medicine residents have been shown to increase knowledge around hormone replacement therapy.71 One study used an observed structured clinical encounter (OSCE) format to assess the ability of primary care residents to care for transgender patients, finding that 61% of residents did not consistently ask about gender identity.83 A limitation to discrete interventions was documented in one study on psychiatry residents, where significant short-term increases in knowledge and comfort were not sustained when assessed with long-term follow-up.69 Multiple authors expressed that skill-focused education at incremental curricular levels, ie, across the length of the residency rather than a discrete modular unit, would have the best educational impact on residents and ultimately clinical outcomes.69,75
The literature discussed interventions to both curricula and policy that would improve graduate transgender education. A curricular mandate from the Accreditation Council for Graduate Medical Education (ACGME) is discussed throughout the literature as the most pragmatic means to the integration of transgender patient care into residency curriculums.22,77–79 The ACMGE’s professional mandate would standardize expectations for resident competencies in transgender health and would move toward case log requirements for surgical fields and accreditation of fellowships for highly specialized transgender-specific procedures.22,79,84
Despite the limited number of studies found for graduate medical education and transgender health, there does appear to be momentum toward adding more transgender health education and clinical exposure to multiple specialties. While a consistent lack of transgender health education is noted, so is the belief that education should be improved. In one study of internal medicine residents, 97% believed in the value of learning comprehensive care skills for transgender patients, but only 45% had any prior education on these issues.74 In another study of endocrinology fellows, 93.8% indicated the importance of transgender health training, but only 72.2% of responding programs provided teaching on transgender health.75 In their discussion sections, authors often observed how the emerging interdisciplinary models of care for transgender patients have yet to be critically incorporated into the design of educational interventions in specialist training. These authors agree that if care delivery models change, education should change to reflect and best-serve new care models.
Discussion
Medical education has been identified as a critical means by which to address health inequities experienced by the transgender community.23,27 The transgender community is experiencing a rapid increase in visibility, through positive media portrayals of high-profile transgender individuals, through controversial legal battles taking place throughout the USA, and through increased coverage of the frequent violence experienced by the community. Recent changes in health care laws have improved health care access for trans-gender people both by allowing payment for gender-affirming interventions and by addressing discriminatory practices in health care.18 We conducted a broad literature review to assess the state of medical education to identify emerging best practices addressing transgender health education. To our knowledge, we are the first to conduct a literature review of North American medical undergraduate and graduate educations specifically on transgender health disaggregated from the LGBTQ umbrella.
Attitudes, knowledge, and skills are foundational components to establish clinical competency.26 Studies of pedagogical interventions targeting student attitudes and knowledge of transgender health consistently show significant improvements. However, these findings should be considered in light of the following: 1) transgender health is often aggregated within the larger LGB umbrella, 2) the assessments are short term with few assessing learner outcomes at long range time points, 3) metrics are often subject to priming or selection bias, especially with elective curricular content, and 4) patient-related outcomes have not been assessed. Additionally, while the general focus on teaching to change attitudes is perhaps warranted in many institutional cultural climates, it does not address the clinical skills needed to begin to alleviate health inequities.46,85 The studies that are transgender specific, with few exceptions, did not focus on developing clinical skills that could potentially impact patient outcomes.60,83 Further emphasis on clinical skill development is necessary to ensure medical students meet Association of American Medical Colleges’ clinical competency standards. New data support the efficacy of clinical exposure in improving requisite comfort and knowledge toward transgender patients.86
The literature offers solutions to the circumscribed nature of current pedagogical interventions. A truly effective pedagogical intervention has been described as one that teaches transgender health in a way that does not create a narrative of a medicalized or pathologized “other” but rather encourages evaluation of the structural and cultural causes of gender minority health inequities.47 Other structural changes in pedagogic delivery would benefit transgender medical education. The literature contains an emerging consensus that modular, ie, one time or discrete, interventions are strongly associated with short-term improvements in attitudes. However, these interventions lack long-term data on efficacy and are not proven to improve transgender patient outcomes. Authors of studies throughout this body of literature suggested incorporating transgender clinical competencies across the curriculum rather than in one or two condensed lectures. Doing so would reinforce topics in their relevant clinical context with emphasis over time. A longitudinal incorporation of transgender health topics into the standard curriculum would also support its disaggregation from the generalized topic of LGBTQ health. For example, this could include discussions of sex organs as opposed to “male and female genitalia” in anatomy, or a discussion of gender identity during lectures on puberty. Because of the issues discussed here, one-time interventions for transgender education are insufficient to create sustainable learning and clinical improvements.
Our review identified the need for an increased emphasis on clinical outcomes. In studies that looked at changes in attitudes and awareness of transgender issues as well as clinical comfort, face-to-face interactions and clinical exposure to transgender patients were the most effective in improving students’ metrics. In moving beyond attitudinal didactic interventions, there is evidence that observed simulated clinical encounters are effective tools for increasing undergraduate and graduate comfort and skill for transgender patients.60,83 Particularly at a graduate level, the need for skill-based pedagogical interventions was ubiquitous throughout the literature. Shifting program director attitudes, expanding fellowship opportunities that provide skills for transgender populations (eg, gender-affirming surgeries), and conferment of credibility of these topics through accreditation were identified as ways to build pedagogical platforms to teach transgender-relevant clinical skills. The shift to skill-based assessment for transgender health teachings will be supported by increasing patient–learner interaction and top-down acknowledgment of the topic’s importance through accreditation and training opportunities.
The literature also details many of the challenges within medical education on transgender health topics. Documented perceptions of lack of time, irrelevance, or lack of competent faculty to teach are prevalent. If the current state of transgender medical education is attitude- and awareness-based one-time interventions, then the shift to integrated and longitudinal clinical skill-based interventions requires significant human capital and institutional investment.
We include the following series of recommendations that are meant to affirm and guide this undertaking:
Accreditation boards, testing boards, deans of curriculum, and residency program directors must specifically name transgender health as a required topic and identify expectations of clinical competencies. National educational organizations and institutional leadership should encourage allotment of curricular resources and time in accordance with clear, agreed upon learning objectives. A one-time lecture, which includes all aspects of LGBTQ health, is insufficient to produce better clinical skills for learners.
Separate transgender health content from the larger LGBTQ umbrella. Gender identity is a distinct domain from sexual orientation (LBG), and the medical concerns relating to gender identity warrant specific attention. Where appropriate, the transgender population should be further individuated so that gender-based health inequities can be more thoroughly understood, such as differences in health outcomes between transmen, transwomen, and gender nonbinary individuals. Integration of important aspects of transgender health may be appropriately placed into lectures and other curricular content traditionally focused on cisgender people including topics such as breast cancer screening and fertility.
Incorporate pedagogical interventions that improve attitudes toward and awareness of transgender health inequities, which is foundational to imparting clinical skills to address such inequities. Thus, while this type of intervention has significant shortcomings when it is the only intervention, it is likely necessary and foundational for building clinical comfort and competency on transgender-specific clinical concerns.86
Pedagogical intervention around transgender health should provide insight into the social and legal barriers that produce health inequities for this community.86 Additionally, care should be taken to ensure that curricula content avoids the pathologization of transgender identities and acknowledges that not all transgender people seek gender-related care. Curricular content, in an attempt to support the transgender community, should acknowledge its documented resilience and agency over medical initiatives that impact the transgender community.87
Pedagogical interventions must focus on the improvement of students’ clinical skills and measured outcomes. Achieving this will include an increased emphasis on direct patient–learner interaction, likely through OSCEs, rotations with LGBTQ-focused community health centers, or direct care of transgender individuals during standard clinical rotations when possible. Metrics are already in place by which to assess clinical competencies for LGBTQ patients.26 It bears noting that tracking clinical outcomes from an educational intervention is impossible without clear and accurate gender identity data in medical records, which is not ubiquitous at this moment.
A standardized measure regarding what qualifies as transgender content in undergraduate medical curricula and a centralized and accurate reporting system to track progress should be developed by a national institution in order to more reliably assess curricular changes and pedagogical best practices. Graduate medical education of transgender health topics should also be standardized in this way but will likely vary by which transgender health topics are most relevant to each specialty (eg, hormone therapy for primary care and gender-affirming procedures for urology).
Our findings are not without limitations. The scope of our literature search was limited to undergraduate and graduate medical educations in North America since 2000. While we believe this to be pragmatically limited in scope, there exists many calls for novel educational or curricular changes for medical students that exist within the literature on a variety of other topics. However, we focused on the current state of transgender health education delivery and pedagogical research rather than recommended curricular content, which has been outlined elsewhere.88 Another limitation is our incorporation of dissertations, opinion pieces, and letters to the editor. While the majority of our analysis is based on peer-reviewed publications, we include these formats to more accurately capture the attitudes and opinions contributing to this emerging field of research. Additionally, it is likely that many pedagogical interventions have been implemented without publication and are thus absent from the literature. Our inclusion of the MedEdPORTAL database captured some relevant studies, but our findings only speak to published curricular changes. It merits mention that curriculum development processes, medical education programs, and staff trainings for transgender-specific clinical goals have emerged but are not reviewed here due to scope.89–91
Conclusion
Transgender populations experience health inequities in part due to the exclusion of transgender-specific health needs from medical school and residency curricula. Currently, transgender medical education is largely composed of one-time attitude and awareness-based interventions that show significant short-term improvements but suffer methodologically from the lack of long-term assessment, the lack of emphasis on clinical skills, or the evaluation of patient outcomes. Consensus in the existing literature supports educational efforts to shift toward pedagogical interventions that are longitudinally integrated and clinical skills based. We believe the integration of transgender health topics into their related medical domains, and increased emphasis on clinical skills will create a curriculum that addresses attitudes, knowledge, and skills and will ultimately alleviate the dire health inequities faced by the transgender community.
Supplementary material
Search databases and terms
Education Source (EBSCO)
(“Transgender Persons” OR “Transsexualism” OR “Health Services for Transgender Persons” OR “Disorders of Sex Development” OR “differences of sex development” OR “difference of sex development” OR “disorders of sex development” OR “disorder of sex development” OR “gender incongruence” OR “gender fluidity” OR “gender reassigned” OR “gender reassignment” OR “gender minority” OR “gender non conformity” OR “gender nonconformity” OR “gender nonconforming” OR “gender non conforming” OR “gender expression” OR “gender variance” OR “gender-variant” OR “crossgender” OR “F2M” OR “female-to-male” OR “gender change” OR “gender changes” OR “gender dysphoria” OR “gender dysphorias” OR “gender queer” OR “gender queering” OR “gender transition” OR “gender transitioning” OR “genderqueer” OR “genderqueer” OR “genderqueers” OR “M2F” OR “male-to-female” OR “sex change” OR “sex changed” OR “sex changer” OR “sex changers” OR “sex changes” OR “sex reversal” OR “sex reversals” OR “sex transition” OR “trans female” OR “trans females” OR “trans male” OR “trans males” OR “trans man” OR “trans men” OR “trans people” OR “trans woman” OR “trans-sexuality” OR “transexual” OR “transgender” OR “transgendered” OR “transgenders” OR “transsexual” OR “transsexualism” OR “transsexuality” OR “transsexuals” OR “transvestite”) AND (“medical students” OR “medical student” OR “medical education” OR “medical college” OR “medical curriculum” OR “clinical clerkship” OR “clinical clerkships” OR “clinical rotation” OR “clinical rotations” OR “clinical curriculum” OR “medical training” OR “Internship and Residency” OR “Teaching Rounds” OR “Students, Medical” OR “Schools, Medical” OR “Education, Medical” OR “Education, Medical, Undergraduate” OR “Education, Medical, Graduate” OR “Education, Medical, Continuing”) AND (“medical students” OR “medical student” OR “medical education” OR “medical college” OR “medical curriculum” OR “clinical clerkship” OR “clinical clerkships” OR “clinical rotation” OR “clinical rotations” OR “clinical curriculum” OR “medical training” OR “Internship and Residency” OR “Teaching Rounds” OR “Students, Medical” OR “Schools, Medical” OR “Education, Medical” OR “Education, Medical, Undergraduate” OR “Education, Medical, Graduate” OR “Education, Medical, Continuing”)
LGBT Life (EBSCO)
(“Transgender Persons” OR “Transsexualism” OR “Health Services for Transgender Persons” OR “Disorders of Sex Development” OR “differences of sex development” OR “difference of sex development” OR “disorders of sex development” OR “disorder of sex development” OR “gender incongruence” OR “gender fluidity” OR “gender reassigned” OR “gender reassignment” OR “gender minority” OR “gender non conformity” OR “gender nonconformity” OR “gender nonconforming” OR “gender non conforming” OR “gender expression” OR “gender variance” OR “gender-variant” OR “crossgender” OR “F2M” OR “female-to-male” OR “gender change” OR “gender changes” OR “gender dysphoria” OR “gender dysphorias” OR “gender queer” OR “gender queering” OR “gender transition” OR “gender transitioning” OR “genderqueer” OR “genderqueer” OR “genderqueers” OR “M2F” OR “male-to-female” OR “sex change” OR “sex changed” OR “sex changer” OR “sex changers” OR “sex changes” OR “sex reversal” OR “sex reversals” OR “sex transition” OR “trans female” OR “trans females” OR “trans male” OR “trans males” OR “trans man” OR “trans men” OR “trans people” OR “trans woman” OR “transsexuality” OR “transexual” OR “transgender” OR “transgendered” OR “transgenders” OR “transsexual” OR “transsexualism” OR “transsexuality” OR “transsexuals” OR “transvestite”) AND (“medical students” OR “medical student” OR “medical education” OR “medical college” OR “medical curriculum” OR “clinical clerkship” OR “clinical clerkships” OR “clinical rotation” OR “clinical rotations” OR “clinical curriculum” OR “medical training” OR “Internship and Residency” OR “Teaching Rounds” OR “Students, Medical” OR “Schools, Medical” OR “Education, Medical” OR “Education, Medical, Undergraduate” OR “Education, Medical, Graduate” OR “Education, Medical, Continuing”) AND (“medical students” OR “medical student” OR “medical education” OR “medical college” OR “medical curriculum” OR “clinical clerkship” OR “clinical clerkships” OR “clinical rotation” OR “clinical rotations” OR “clinical curriculum” OR “medical training” OR “Internship and Residency” OR “Teaching Rounds” OR “Students, Medical” OR “Schools, Medical” OR “Education, Medical” OR “Education, Medical, Undergraduate” OR “Education, Medical, Graduate” OR “Education, Medical, Continuing”)
MedEdPORTAL
(“Transgender”)
PsycINFO
(“Transgender” AND “Education”)
PubMed
(((“Medical education”[Journal] OR “Academic medicine: journal of the Association of American Medical Colleges”[Journal] OR “Advances in health sciences education: theory and practice”[Journal] OR “Medical teacher”[Journal] OR “Academic emergency medicine: official journal of the Society for Academic Emergency Medicine”[Journal] OR “Simulation in healthcare: journal of the Society for Simulation in Healthcare”[Journal] OR “Journal of surgical education”[Journal] OR “Evaluation & the health professions”[Journal] OR “BMC medical education”[Journal] OR “The Journal of continuing education in the health professions”[Journal] OR “Teaching and learning in medicine”[Journal] OR “The clinical teacher”[Journal] OR “Education for health (Abingdon, England)”[Journal] OR “Advances in physiology education”[Journal] OR “Canadian medical education journal”[Journal] OR “Journal of graduate medical education”[Journal] OR “Medical education online”[Journal] OR “Perspectives on medical education”[Journal] OR “Journal of research in interprofessional practice and education”[Journal] OR “Medical science educator”[Journal] OR “The journal of the International Association of Medical Science Educators: JIAMSE”[Journal]))) OR (“medical students”[tiab] OR “medical student”[tiab] OR “medical education”[tiab] OR “medical college”[tiab] OR “medical curriculum”[tiab] OR “clinical clerkship”[tiab] OR “clinical clerkships”[tiab] OR “clinical rotation”[tiab] OR “clinical rotations”[tiab] OR “clinical curriculum”[tiab] OR “medical training”[tiab] OR “Internship and Residency”[Mesh] OR “Teaching Rounds”[Mesh] OR “Students, Medical”[Mesh] OR “Schools, Medical”[Mesh] OR “Education, Medical”[Mesh] OR “Education, Medical, Undergraduate”[Mesh] OR “Education, Medical, Graduate”[Mesh] OR “Education, Medical, Continuing”[Mesh])
Acknowledgments
We wish to acknowledge Vania Rashidi for his assistance with making the figures. We also wish to acknowledge Dr Victoria Harnick for her early guidance in framing this article, as well as Joseph Nicholson for his input on our search strategy.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sexual and gender minorities formally designated as a health disparity population for research purposes [press release] National Institute of Minority Health and Health Disparities. 2016 [Google Scholar]
- 2.Institute of Medicine (US) Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities . The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press (US); 2011. [PubMed] [Google Scholar]
- 3.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend. 2011;13(4):165–232. [Google Scholar]
- 4.Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health. 2017;107(2):216. doi: 10.2105/AJPH.2016.303578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of trans-gender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am J Public Health. 2013;103(10):1820–1829. doi: 10.2105/AJPH.2012.300796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radix AE, Lelutiu-Weinberger C, Gamarel KE. Satisfaction and health-care utilization of transgender and gender non-conforming individuals in NYC: a community-based participatory study. LGBT Health. 2014;1(4):302–308. doi: 10.1089/lgbt.2013.0042. [DOI] [PubMed] [Google Scholar]
- 7.Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91(6):915–921. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lombardi E. Transgender health: a review and guidance for future research-proceedings from the Summer Institute at the Center for Research on Health and Sexual Orientation, University of Pittsburgh. Int J Transgend. 2010;12(4):211–229. [Google Scholar]
- 9.Operario D, Nemoto T. HIV in transgender communities: syndemic dynamics and a need for multicomponent interventions. J Acquir Immune Defic Syndr. 1999;2010(55 suppl 2):S91–S93. doi: 10.1097/QAI.0b013e3181fbc9ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radix A, Sevelius J, Deutsch MB. Transgender women, hormonal therapy and HIV treatment: a comprehensive review of the literature and recommendations for best practices. J Int AIDS Soc. 2016;19(3 suppl 2):20810. doi: 10.7448/IAS.19.3.20810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 12.Streed CG, Jr, McCarthy EP, Haas JS. Association between gender minority status and self-reported physical and mental health in the United States. JAMA Intern Med. 2017;177(8):1210–1212. doi: 10.1001/jamainternmed.2017.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reisner SL, Hughto JM, Dunham EE, et al. Legal protections in public accommodations settings: a critical public health issue for transgender and gender-nonconforming people. Milbank Q. 2015;93(3):484–515. doi: 10.1111/1468-0009.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on Health and Health Care. Washington, DC: National Center for Transgender Equality and the National Gay and Lesbian Task Force; 2010. [Google Scholar]
- 15.Ben-Asher N. The necessity of sex change: a struggle for intersex and transsex liberties. Harv J Law Gender. 2006;29:51–98. [Google Scholar]
- 16.Rush v. Parham, 625 F.2d 1150(5th Cir. 1980).
- 17.Nardi C. Comment, when health insurers deny coverage for breast reconstructive surgery: gender meets disability. Wis L Rev. 1997;1997(4):777–826. [PubMed] [Google Scholar]
- 18.Gage S. The transgender eligibility gap: how the ACA fails to cover medically necessary treatment for transgender individuals and how HHS can fix it. New Engl Law Rev. 2015;49:92. [Google Scholar]
- 19.Singh S, Durso L. Widespread Discrimination Continues to Shape LGBT People’s Lives in Both Subtle and Significant Ways. 2017. [Accessed December, 2017]. [webpage on the Internet] Available from: https://www.americanprogress.org/issues/lgbt/news/2017/05/02/429529/widespread-discrimination-continues-shape-lgbt-peoples-lives-subtle-significant-ways/
- 20.US Department of Health & Human Services [webpage on the Internet] Access to Healthcare: Nondiscrimination. 2017. [Accessed December 28, 2017]. Available from: https://www.hhs.gov/programs/topic-sites/lgbt/accesstohealthcare/nondiscrimination/index.html.
- 21.Out2Enroll Reaching and Assisting LGBT Communities. 2015. [Accessed December 28, 2017]. Available from: http://out2enroll.org/lgbthealthcare/wp-content/uploads/2015/09/Out2Enroll-Updated-Slide-Deck-091615.pdf.
- 22.Morrison SD, Wilson SC, Smith JR. Are we adequately preparing our trainees to care for transgender patients? J Grad Med Educ. 2017;9(2):258. doi: 10.4300/JGME-D-16-00712.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mayer KH, Bradford JB, Makadon HJ, Stall R, Goldhammer H, Landers S. Sexual and gender minority health: what we know and what needs to be done. Am J Public Health. 2008;98(6):989–995. doi: 10.2105/AJPH.2007.127811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The World Professional Association for Transgender Health [Accessed December 28, 2017];Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. 2011 7 Available from: https://www.wpath.org/publications/soc. [Google Scholar]
- 25.Cahill S, Makadon H. Sexual orientation and gender identity data collection in clinical settings and in electronic health records: a key to ending LGBT health disparities. LGBT Health. 2014;1(1):34–41. doi: 10.1089/lgbt.2013.0001. [DOI] [PubMed] [Google Scholar]
- 26.Hollenbach A, Eckstrand K, Dreger A. Implementing Curricular and Institutional Climate Changes to Improve Health Care for Individuals Who Are LGBT, Gender Nonconforming, or Born with DSD. 1st ed. Washington, DC: Association of American Medical Colleges; 2014. [Google Scholar]
- 27.Institute of Medicine . The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 28.Lombardi E. Public health and trans-people: barriers to care and strategies to improve treatment. In: Meyer I, Northridge ME, editors. The Health of Sexual Minorities Public Health. New York: Springer; 2007. p. 15. [Google Scholar]
- 29.Streed CG, Jr, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: a narrative review. Ann Intern Med. 2017;167(4):256–267. doi: 10.7326/M17-0577. [DOI] [PubMed] [Google Scholar]
- 30.Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(11):3869–3903. doi: 10.1210/jc.2017-01658. [DOI] [PubMed] [Google Scholar]
- 31.Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jann JT, Edmiston EK, Ehrenfeld JM. Important considerations for addressing LGBT health care competency. Am J Public Health. 2015;105(11):e8. doi: 10.2105/AJPH.2015.302864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bidell MP, Stepleman LM. An interdisciplinary approach to lesbian, gay, bisexual, and transgender clinical competence, professional training, and ethical care: introduction to the special issue. J Homosex. 2017;64(10):1305–1329. doi: 10.1080/00918369.2017.1321360. [DOI] [PubMed] [Google Scholar]
- 34.Bonvicini KA. LGBT healthcare disparities: what progress have we made? Patient Educ Couns. 2017;100(12):2357–2361. doi: 10.1016/j.pec.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 35.Arrowsmith L. Improving osteopathic medical training in providing health care to lesbian, gay, bisexual, and transgender patients. J Am Osteopath Assoc. 2015;115(1):6–7. doi: 10.7556/jaoa.2015.001. [DOI] [PubMed] [Google Scholar]
- 36.Coker TR, Austin SB, Schuster MA. Health and healthcare for lesbian, gay, bisexual, and transgender youth: reducing disparities through research, education and practice. J Adolesc Health. 2009;45(3):213–215. doi: 10.1016/j.jadohealth.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 37.Daniel H, Butkus R. Lesbian, gay, bisexual, and transgender health disparities: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;163(2):135–137. doi: 10.7326/M14-2482. [DOI] [PubMed] [Google Scholar]
- 38.Hart D. Toward better care for lesbian, gay, bisexual and transgender patients. Minn Med. 2013;96(8):42–45. [PubMed] [Google Scholar]
- 39.Khalili J, Leung LB, Diamant AL. Finding the perfect doctor: identifying lesbian, gay, bisexual, and transgender-competent physicians. Am J Public Health. 2015;105(6):1114–1119. doi: 10.2105/AJPH.2014.302448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eliminating health disparities – promoting awareness and education of lesbian, gay, bisexual, and transgender (LGBT) health issues in medical education H-295878 [press release] American Medical Association. [Accessed December 28, 2017]. Available from: https://policysearch.ama-assn.org/policyfinder/detail/transgender%20?uri=%2FAMADoc%2FHOD.xml-0-2177.xml.
- 41.Advancing Effective Communication . Cultural competence, and patient-and family centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: a field guide [press release] Oak Brook, IL: The Joint Commission; 2011. [Google Scholar]
- 42.Curry RH. Capturing curricula. JAMA. 2011;306(9):997–998. doi: 10.1001/jama.2011.1266. [DOI] [PubMed] [Google Scholar]
- 43.Lutwak N. Improving care of transgender patients. Acad Emerg Med. 2017;24(8):1034–1035. doi: 10.1111/acem.13236. [DOI] [PubMed] [Google Scholar]
- 44.Ng H. Lesbian, gay, bisexual, and transgender health and medical education. JAMA. 2011;306(21):2326. doi: 10.1001/jama.2011.1782. author reply 2326–2327. [DOI] [PubMed] [Google Scholar]
- 45.Mansh M, Garcia G, Lunn MR. From patients to providers: changing the culture in medicine toward sexual and gender minorities. Acad Med. 2015;90(5):574–580. doi: 10.1097/ACM.0000000000000656. [DOI] [PubMed] [Google Scholar]
- 46.Utamsingh PD, Kenya S, Lebron CN, Carrasquillo O. Beyond sensitivity. LGBT healthcare training in U.S. Medical Schools: a review of the literature. Am J Sex Educ. 2017;12(2):148–169. [Google Scholar]
- 47.Desrosiers J, Wilkinson T, Abel G, Pitama S. Curricular initiatives that enhance student knowledge and perceptions of sexual and gender minority groups: a critical interpretive synthesis. Can Med Educ J. 2016;7(2):e121–e138. [PMC free article] [PubMed] [Google Scholar]
- 48.Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306(9):971–977. doi: 10.1001/jama.2011.1255. [DOI] [PubMed] [Google Scholar]
- 49.Dowshen N, Meadows R, Byrnes M, Hawkins L, Eder J, Noonan K. Policy perspective: ensuring comprehensive care and support for gender nonconforming children and adolescents. Transgend Health. 2016;1(1):75–85. doi: 10.1089/trgh.2016.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Honigberg MC, Eshel N, Luskin MR, Shaykevich S, Lipsitz SR, Katz JT. Curricular time, patient exposure, and comfort caring for lesbian, gay, bisexual, and transgender patients among recent medical graduates. LGBT Health. 2017;4(3):237–239. doi: 10.1089/lgbt.2017.0029. [DOI] [PubMed] [Google Scholar]
- 51.Liang JJ, Gardner IH, Walker JA, Safer JD. Observed deficiencies in medical student knowledge of transgender and intersex health. Endocr Pract. 2017;23(8):897–906. doi: 10.4158/EP171758.OR. [DOI] [PubMed] [Google Scholar]
- 52.White W, Brenman S, Paradis E, et al. Lesbian, gay, bisexual, and transgender patient care: medical students’ preparedness and comfort. Teach Learn Med. 2015;27(3):254–263. doi: 10.1080/10401334.2015.1044656. [DOI] [PubMed] [Google Scholar]
- 53.Sanchez NF, Rabatin J, Sanchez JP, Hubbard S, Kalet A. Medical students’ ability to care for lesbian, gay, bisexual, and transgendered patients. Fam Med. 2006;38(1):21–27. [PubMed] [Google Scholar]
- 54.Lapinski J, Sexton P, Baker L. Acceptance of lesbian, gay, bisexual, and transgender patients, attitudes about their treatment, and related medical knowledge among osteopathic medical students. J Am Osteopath Assoc. 2014;114(10):788–796. doi: 10.7556/jaoa.2014.153. [DOI] [PubMed] [Google Scholar]
- 55.Burke SE, Dovidio JF, Przedworski JM, et al. Do contact and empathy mitigate bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–651. doi: 10.1097/ACM.0000000000000661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hayes V, Blondeau W, Bing-You RG. Assessment of medical student and resident/fellow knowledge, comfort, and training with sexual history taking in LGBTQ patients. Fam Med. 2015;47(5):383–387. [PubMed] [Google Scholar]
- 57.Chan B, Skocylas R, Safer JD. Gaps in transgender medicine content identified among Canadian Medical School Curricula. Transgend Health. 2016;1(1):142–150. doi: 10.1089/trgh.2016.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sequeira GM, Chakraborti C, Panunti BA. Integrating lesbian, gay, bisexual, and transgender (LGBT) content into undergraduate medical school curricula: a qualitative study. Ochsner J. 2012;12(4):379–382. [PMC free article] [PubMed] [Google Scholar]
- 59.Tamas RL, Miller KH, Martin LJ, Greenberg RB. Addressing patient sexual orientation in the undergraduate medical education curriculum. Acad Psychiatry. 2010;34(5):342–345. doi: 10.1176/appi.ap.34.5.342. [DOI] [PubMed] [Google Scholar]
- 60.Dowshen N, Gilbert K, Feiler A, Lee S. 30. Transgender health education impact on medical student knowledge, skills and attitudes. J Adolesc Health. 2013;52(2 suppl 1):S35. [Google Scholar]
- 61.Grubb HHH, Amiel J, Bogart J, Laird J. Cultural humility with lesbian, gay, bisexual, and transgender populations: a novel curriculum in LGBT health for clinical medical students. MedEdPORTAL. 2013;9:9542. [Google Scholar]
- 62.Safer JD, Pearce EN. A simple curriculum content change increased medical student comfort with transgender medicine. Endocr Pract. 2013;19(4):633–637. doi: 10.4158/EP13014.OR. [DOI] [PubMed] [Google Scholar]
- 63.Eriksson SE, Safer JD. Evidence-based curricular content improves student knowledge and changes attitudes towards transgender medicine. Endocr Pract. 2016;22(7):837–841. doi: 10.4158/EP151141.OR. [DOI] [PubMed] [Google Scholar]
- 64.Braun HM, Garcia-Grossman IR, Quiñones-Rivera A, Deutsch MB. Outcome and impact evaluation of a transgender health course for health profession students. LGBT Health. 2017;4(1):55–61. doi: 10.1089/lgbt.2016.0119. [DOI] [PubMed] [Google Scholar]
- 65.Sawning S, Steinbock S, Croley R, Combs R, Shaw A, Ganzel T. A first step in addressing medical education curriculum gaps in lesbian-, gay-, bisexual-, and transgender-related content: the University of Louisville Lesbian, Gay, Bisexual, and Transgender Health Certificate Program. Educ Health (Abingdon) 2017;30(2):108–114. doi: 10.4103/efh.EfH_78_16. [DOI] [PubMed] [Google Scholar]
- 66.Vance SR, Jr, Deutsch MB, Rosenthal SM, Buckelew SM. Enhancing pediatric trainees’ and students’ knowledge in providing care to transgender youth. J Adolesc Health. 2017;60(4):425–430. doi: 10.1016/j.jadohealth.2016.11.020. [DOI] [PubMed] [Google Scholar]
- 67.Ferrara E, Pugnaire MP, Jonassen JA, et al. Sexual health innovations in undergraduate medical education. Int J Impot Res. 2003;15(suppl 5):S46–S50. doi: 10.1038/sj.ijir.3901072. [DOI] [PubMed] [Google Scholar]
- 68.Barber ME, Dresche J, Rosari V. The GAP online LGBT mental health curriculum. J Gay Lesbian Mental Health. 2012;16(1):41–48. [Google Scholar]
- 69.Kidd JD, Bockting W, Cabaniss DL, Blumenshine P. Special-“T” training: extended follow-up results from a residency-wide professionalism workshop on transgender health. Acad Psychiatry. 2016;40(5):802–806. doi: 10.1007/s40596-016-0570-7. [DOI] [PubMed] [Google Scholar]
- 70.Mokonogho J, Mittal S, Quitangon G. Treating the transgender homeless population: experiences during residency training. J Gay Lesbian Mental Health. 2010;14(4):346–354. [Google Scholar]
- 71.Thomas DD, Safer JD. A simple intervention raised resident-physician willingness to assist transgender patients seeking hormone therapy. Endocr Pract. 2015;21(10):1134–1142. doi: 10.4158/EP15777.OR. [DOI] [PubMed] [Google Scholar]
- 72.McGarry KA, Clarke JG, Cyr MG, Landau C. Evaluating a lesbian and gay health care curriculum. Teach Learn Med. 2002;14(4):244–248. doi: 10.1207/S15328015TLM1404_8. [DOI] [PubMed] [Google Scholar]
- 73.Klein EW, Nakhai M. Caring for LGBTQ patients: methods for improving physician cultural competence. Int J Psychiatry Med. 2016;51(4):315–324. doi: 10.1177/0091217416659268. [DOI] [PubMed] [Google Scholar]
- 74.Johnston CD, Shearer LS. Internal medicine resident attitudes, prior education, comfort, and knowledge regarding delivering comprehensive primary care to transgender patients. Transgend Health. 2017;2(1):91–95. doi: 10.1089/trgh.2017.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Davidge-Pitts C, Nippoldt TB, Danoff A, Radziejewski L, Natt N. Transgender health in endocrinology: current status of endocrinology fellowship programs and practicing clinicians. J Clin Endocrinol Metab. 2017;102(4):1286–1290. doi: 10.1210/jc.2016-3007. [DOI] [PubMed] [Google Scholar]
- 76.Moll J, Krieger P, Moreno-Walton L, et al. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know? Acad Emerg Med. 2014;21(5):608–611. doi: 10.1111/acem.12368. [DOI] [PubMed] [Google Scholar]
- 77.Morrison SD, Dy GW, Chong HJ, et al. Transgender-related education in plastic surgery and urology residency programs. J Grad Med Educ. 2017;9(2):178–183. doi: 10.4300/JGME-D-16-00417.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Morrison SD, Chong HJ, Dy GW, et al. Educational exposure to transgender patient care in plastic surgery training. Plast Reconstr Surg. 2016;138(4):944–953. doi: 10.1097/PRS.0000000000002559. [DOI] [PubMed] [Google Scholar]
- 79.Dy GW, Osbun NC, Morrison SD, Grant DW, Merguerian PA. Exposure to and attitudes regarding transgender education among urology residents. J Sex Med. 2016;13(10):1466–1472. doi: 10.1016/j.jsxm.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 80.Massenburg BM, Morrison SD, Rashidi V, et al. Educational exposure to transgender patient care in otolaryngology training. J Craniofacial Surg. 2018 doi: 10.1097/SCS.0000000000004609. [DOI] [PubMed] [Google Scholar]
- 81.Criniti SM. Perspectives of Sexuality Education Among Medical Residents. Ann Arbor, MI: ProQuest Information & Learning; 2015. [Google Scholar]
- 82.Ali N, Fleisher W, Erickson J. Psychiatrists’ and psychiatry residents’ attitudes toward transgender people. Acad Psychiatry. 2016;40(2):268–273. doi: 10.1007/s40596-015-0308-y. [DOI] [PubMed] [Google Scholar]
- 83.Greene RE, Hanley K, Cook TE, Gillespie C, Zabar S. Meeting the primary care needs of transgender patients through simulation. J Grad Med Educ. 2017;9(3):380–381. doi: 10.4300/JGME-D-16-00770.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morrison SD, Smith JR, Mandell SP. Are surgical residents prepared to care for transgender patients? JAMA Surg. 2018;153(1):92–93. doi: 10.1001/jamasurg.2017.4024. [DOI] [PubMed] [Google Scholar]
- 85.Shindel AW, Baazeem A, Eardley I, Coleman E. Sexual health in undergraduate medical education: existing and future needs and platforms. J Sex Med. 2016;13(7):1013–1026. doi: 10.1016/j.jsxm.2016.04.069. [DOI] [PubMed] [Google Scholar]
- 86.Park JA, Safer JD. Clinical exposure to transgender medicine improves students’ preparedness above levels seen with didactic teaching alone: a key addition to the Boston University Model for Teaching Transgender Healthcare. Transgend Health. 2018;3(1):10–16. doi: 10.1089/trgh.2017.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Radix A, Erickson-Schroth L, Jacobs LA. In: Trauma, Resilience, and Health Promotion in LGBT Patients: What Every Healthcare Provider Should Know. 1st ed. Eckstrand K, Potter J, editors. Berlin: Springer; 2017. [Google Scholar]
- 88.Fenway Institute National LGBT Health Education Center About CME/CEU and HEI Credit. 2018. [Accessed December 28, 2017]. Available from: https://www.lgbthealthe-ducation.org/lgbt-education/cme/
- 89.Vanderleest JG, Galper CQ. Improving the health of transgender people: transgender medical education in Arizona. J Assoc Nurses AIDS Care. 2009;20(5):411–416. doi: 10.1016/j.jana.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 90.Ton H, Eidson-Ton WS, Iosif A-M, Sitkin N, Henderson S, Callahan EJ. Using a retreat to develop a 4-year sexual orientation and gender identity curriculum. Acad Psychiatry. 2016;40(5):796–801. doi: 10.1007/s40596-015-0474-y. [DOI] [PubMed] [Google Scholar]
- 91.Lelutiu-Weinberger C, Pollard-Thomas P, Pagano W, et al. Implementation and evaluation of a pilot training to improve transgender competency among medical staff in an Urban Clinic. Transgend Health. 2016;1(1):45–53. doi: 10.1089/trgh.2015.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]