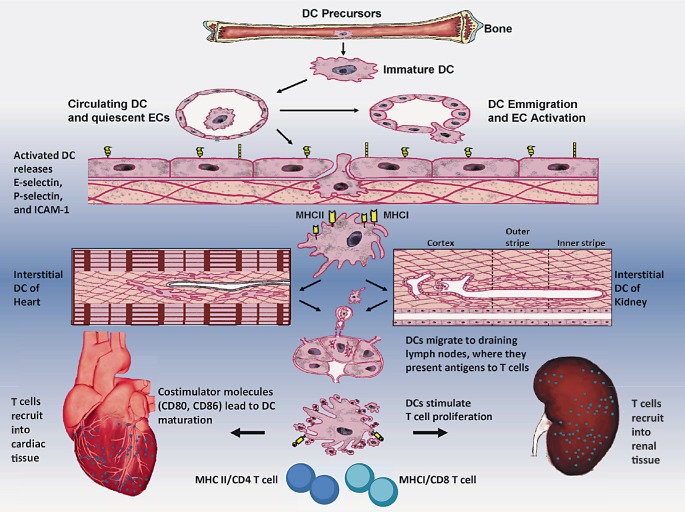
Fig. 1.
Schematic diagram showing DCs as professional antigen-presenting cells (APCs), ECs as nonprofessional APCs, and CD4 and CD8 T cells as immune effector cells in the innate and adaptive immune response in CRS, particularly in type 2 and type 4, based on animal studies. The sequence of events leading to the immunity may be described as: (1) DCs are derived from their precursors in bone marrow and circulate in the vessels; (2) upon exposure to cell adhesion molecules (selectins, ICAM-1) on the surface of ECs, DCs can emigrate from blood vessels to the interstitial spaces; (3) immature DCs residing in the heart and kidney have an immature phenotype (a high propensity of antigen capture but relatively poor capacity to stimulate naïve T cells); (4) upon exposure to costimulatory molecules like CD80 and CD86, and danger signals from injured tissues, interstitial DCs with MHC class II (or I) antigen molecules undergo a maturation process; (5) DCs then migrate to draining lymph nodes, where they present antigens to T cells, trigger CD4 or CD8 T cell proliferation; and (6) mature DCs recruit into inflammatory interstitial cardiac and renal tissues, leading to cardiac dysfunction and renal dysfunction, and finally contributing to combined end-organ damage. During this immune process, the cells of innate response are DCs and ECs, whereas the immune cells for adaptive responses are predominant T cells.