Abstract
Dysphagia is a common problem and an indication for upper endoscopy. There is no data on the frequency of the different endoscopic findings and whether they change according to demographics or by single versus repeat endoscopy. To determine the prevalence of endoscopic findings in patients with dysphagia and whether findings differ in regard to age, gender, ethnicity, and repeat procedure. This was a retrospective study using a national endoscopic database (CORI). A total of 30,377 patients underwent esophagogastroduodenoscopy (EGD) for dysphagia of which 4,202 patients were repeat endoscopies. Overall frequency of endoscopic findings was determined by gender, age, ethnicity, and single vs. repeat procedures. Esophageal stricture was the most common finding followed by normal, esophagitis/ulcer (EU), Schatzki ring (SR), esophageal food impaction (EFI), and suspected malignancy. Males were more likely to undergo repeat endoscopies and more likely to have stricture, EU, EFI, and suspected malignancy (P = 0.001). Patients 60 years or older had a higher prevalence of stricture, EU, SR, and suspected malignancy (P < 0.0001). Esophageal stricture was most common in white non-Hispanic patients compared to other ethnic groups. In patients undergoing repeat EGD, stricture, SR, EFI, and suspected malignancy were more common (P < 0.0001). The prevalence of endoscopic findings differs significantly by gender, age, and repeat procedure. The most common findings in descending order were stricture, normal, EU, SR, EFI, and suspected malignancy. For patients undergoing a repeat procedure, normal and EU were less common and all other abnormal findings were significantly more common.
Keywords: Dysphagia, Endoscopy, Eosinophilic esophagitis, Esophagitis, Schatzki ring, Deglutition, Deglutition disorders
Dysphagia refers to a subjective sensation of difficulty swallowing. There are many well-known causes for dysphagia but the epidemiology of dysphagia is not well established. The exact prevalence of dysphagia is uncertain but it is estimated to be 6–9% in all age groups and 16–22% in patients above 50 years old [1-3]. It is estimated to affect as many as 15 million Americans, with approximately one million people annually receiving a new diagnosis of this condition [4]. Dysphagia has been shown to significantly impact the quality of life in affected individuals, with patients reporting panic and anxiety about eating as well as developing depression [5, 6]. Upper endoscopy (esophagogastroduodenoscopy, EGD) is the most common initial diagnostic procedure performed in the evaluation of esophageal dysphagia as this allows direct visualization of the entire esophagus and tissue acquisition via biopsy.
The common endoscopic findings in patients with dysphagia are well known but the relative prevalence of these findings has not been reported. In addition, there is little or no data regarding the frequencies of these findings or if they vary with patient demographics or in patients who undergo repeat endoscopy as compared to primary endoscopy. The purpose of this study was to determine the prevalence of the endoscopic findings associated with dysphagia in a large endoscopic database and to further examine if age, gender, ethnicity/race, and other demographic factors affect the prevalence of these endoscopic findings.
Materials and Methods
This is an institutional review board-approved retrospective analysis of data from the Clinical Outcomes Research Initiative (CORI) database prospectively collected from January 2000 to September 2006. CORI is a computerized national database established in 1995 to study the use and outcomes of endoscopy in diverse practice settings. All participating sites use a standardized computerized report generator to create endoscopy reports and comply with quality control requirements. The sites’ data files are transmitted electronically to a central data repository: the National Endoscopic Database (NED). Before transmission, all patient and physician identifiers are removed from the data file to protect both patient and physician confidentiality. Only the practice sites that had contributed data continuously for the entire study period were used; comprising 26 stable practice sites from 14 states. The majority of procedure reports were from community practices (91%) and 9% from university hospitals. VA/military sites were not included in this study as all the needed demographic details were not available.
All patients 18 years or older who had undergone one or more upper endoscopies during the study period for the indication of dysphagia were included in the study. Patients with gastrointestinal bleeding were not included in this study. Among the patients who had undergone multiple procedures, data from the first and second endoscopic procedures were included. Patients with more than one endoscopic finding were included in all the diagnostic categories.
The prevalence of selected endoscopic findings was determined overall and also stratified by gender, age group (< 60 or ≥60 years), race/ethnicity, and need for repeat procedures (single vs. multiple). Ethnicity/race was grouped into white non-Hispanic, Black non-Hispanic, Hispanic, Asian/Pacific Islander, Native American, and multiracial. Endoscopic findings were grouped as normal esophagus, esophagitis/ulcer (EU), esophageal food impaction (EFI), suspected malignancy, stricture, and Schatzki ring (SR). SR was considered separate from other strictures according to standard CORI practice.
Categorical variables were compared using the χ2 test. The relationship between ordered variables and outcomes was analyzed with the Mantel Haenszel test of trend (χ2 test for linear association). All analyses were performed using SAS software ver. 9.1 (SAS Institute, Cary, NC). A P value ≤0.05 was considered statistically significant.
Results
A total of 30,377 unique patients who had undergone upper endoscopy with an indication of dysphagia were identified, although other indications may have coexisted simultaneously as well. Of these patients, 26,175 (86.2%) had a single endoscopy and 4,202 (13.8%) had undergone repeat procedures during the time period. Excluding the 1,040 (3%) patients whose information on race/ethnicity was missing, the demographic breakdown of the patients is given in Table 1.
Table 1.
Patient demographics (N = 30,377)
| Number | % | |
|---|---|---|
| Gender | ||
| Female | 17,356 | 57.1 |
| Male | 13,021 | 42.9 |
| Age group (years) | ||
| 18–50 | 8,303 | 27.3 |
| 50–59 | 6,711 | 22.1 |
| 60–69 | 6,391 | 21.0 |
| 70–79 | 5,810 | 19.1 |
| C80 | 3,162 | 10.4 |
| Race/ethnicitya | ||
| White NH | 26,282 | 89.6 |
| Black NH | 1,017 | 3.5 |
| Hispanic | 1,146 | 3.9 |
| Asian/Pacific Islander NH | 381 | 1.3 |
| Native American NH | 475 | 1.6 |
| Multiracial NH | 43 | 0.2 |
NH non-Hispanic
1,040 missing race/ethnicity excluded
For the entire cohort, esophageal stricture was the most common finding (40.8%) followed by normal esophagus (32.1%), EU (22.1%), SR (13.3%), EFI (2.2%), and suspected malignancy (0.9%). Women were more likely to have a normal exam than men (37.2 vs. 25.4%; P < 0.0001) and underwent proportionately more endoscopies for dysphagia than men (57.1 vs. 42.8%). The prevalence of a SR among males and females was not different (P = 0.90) (Fig. 1). All abnormal endoscopic findings were more common in men than women (P < 0.001 for all comparisons). Patients over 60 years compared with those ≤60 years had a higher prevalence of suspected malignancy (1.3 vs. 0.4%), stricture (45.9 vs. 35.6%), and SR (14.7 vs. 11.9%), while patients ≤60 years were more likely to have EU and EFI (P < 0.0001 for all comparisons) (Fig. 2).
Fig. 1.
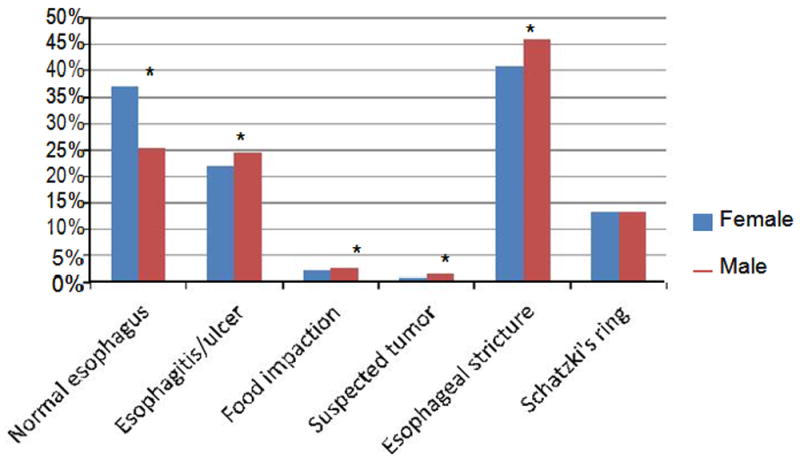
Prevalence of endoscopic findings in patients presenting with dysphagia by gender
Fig. 2.
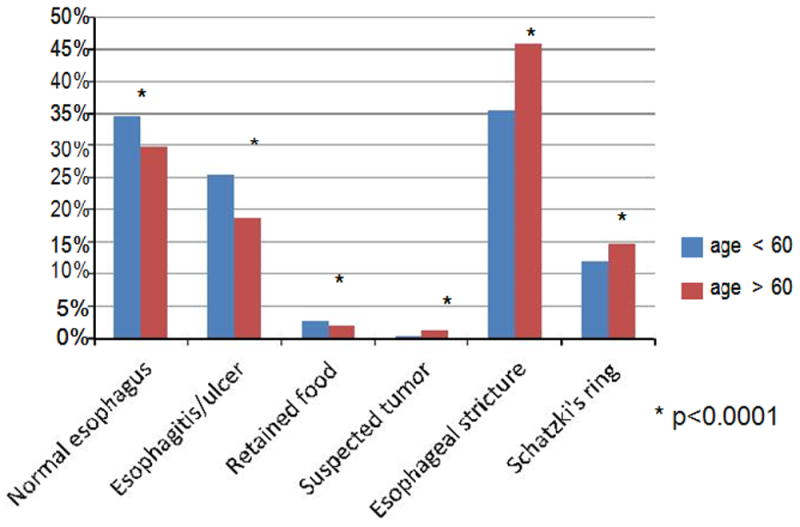
Prevalence of endoscopic findings in patients presenting with dysphagia by age
When compared by race/ethnicity, esophageal strictures were most common in non-Hispanic white patients. Asian/ Pacific Islander patients were more likely to have normal exams (65.5 vs. 30.7%) and a lower prevalence of stricture (9.4 vs. 42.3%), EU (22.3 vs. 10.7%), and SR (3.7 vs. 13.8%) compared to non-Hispanic whites (Fig. 3).
Fig. 3.
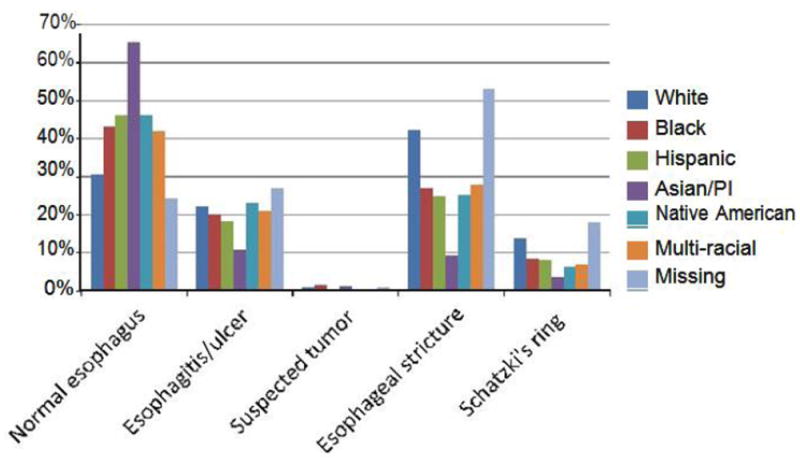
Prevalence of endoscopic findings in patients presenting with dysphagia by race/ethnicity
A total of 4,202 (13.8%) patients underwent repeat endoscopy for dysphagia during the time period. Males were more likely to have undergone multiple endoscopies than females (15.3 vs. 12.8%, P = 0.001). A normal exam or EU was found more frequently in those who underwent just one examination. Esophageal stricture, EFI, suspected malignancy, and SR were more frequent findings in patients who underwent repeat endoscopy (P < 0.0001 for all comparisons) (Fig. 4).
Fig. 4.
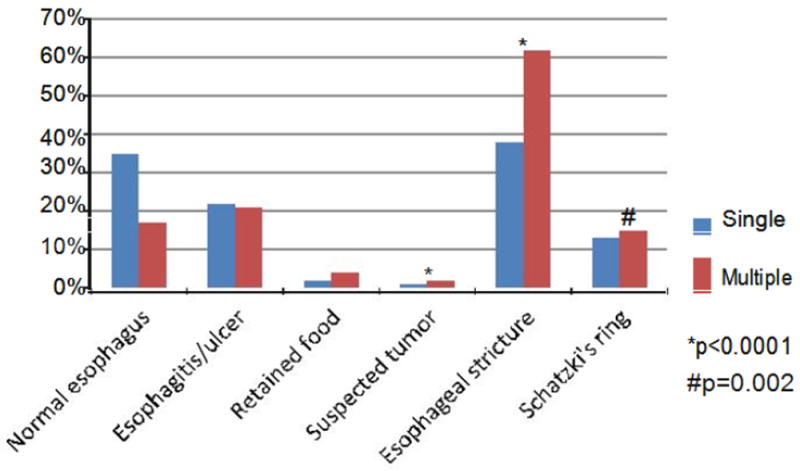
Prevalence of endoscopic findings in patients presenting with dysphagia by single versus multiple upper endoscopies
Discussion
There are numerous studies that have established the different etiologies and common endoscopic findings in patients presenting with dysphagia [7-9]. However, these are older studies that did not report the relative frequency of the common endoscopic findings in patients with dysphagia or how these findings may have differed with specific demographic groups. This is the first study to evaluate a large, diverse population to describe the prevalence of common endoscopic findings in patients who underwent upper endoscopy to investigate dysphagia. Dysphagia is reported to be associated with recurrent aspiration, inadequate nutrition, and weight loss and to have a high estimated economic burden. Early identification of dysphagia and therapeutic intervention are critical to preventing complications. Our study was an attempt to provide helpful information that could help manage expectations in preprocedure discussion and better prepare both patients and physicians for potential therapeutic interventions.
Esophageal strictures were the most common abnormal finding overall, regardless of gender, age, and demographic group. Gastroesophageal reflux disease (GERD) is reported to be the third most common GI disorder in the US, with an approximately 20% prevalence [3, 10, 11], and peptic strictures account for about 70–80% of all esophageal strictures [12, 13]. This is not a novel observation, however, in light of the recent emergence of eosinophilic esophagitis (EoE) as a possible new diagnosis with similar presentation [14- 17]. We speculate that EoE is possibly a reason for stricture or normal exam in many of our patients. However, at the time of this study, endoscopic procedural reports did not have a specific diagnosis for EoE, and we suspect it was misclassified under a variety of other diagnoses.
We found that women underwent more endoscopies for dysphagia than males, although women were also more likely to have normal exams than males. This may be consistent with the increased health-seeking behavior in women [18-20]. Alternatively, the dysphagia of those with normal findings on endoscopy could be caused by something that would not be recognized at initial endoscopy and/or would not able to be diagnosed with endoscopy alone, including esophageal motility disorders, nonerosive reflux disease, or misdiagnosed oropharyngeal dysphagia. Males had higher rates of repeat endoscopies and were more likely to have pathological diagnoses of EU, food impaction, stricture, and suspected malignancy.
The diagnosis of SR was similar between males and females in this study, in contrast to the study by Byrne et al. [21] that showed a significant association of female gender with SR, especially in the older age group (>50 years). This may be secondary to the greater power of the present study (N = 30,377). As one might expect, we found patients who were ≥60 years old had significantly higher rates of suspected malignancy, stricture, and SR.
Patients who had only one exam during the time period were more likely to have a normal esophagus or EU, whereas stricture, EFI, suspected malignancy, and SR were more common findings on repeat upper endoscopies. It is possible that the need for repeat endoscopy in this subset of patients could be secondary to findings missed on the initial exam, relapsing or refractory disease not responding to initial management, and/or the need for additional endoscopic treatment, i.e., repeated dilation or stent placement. It is noteworthy that normal findings decreased by 17.7% in patients who underwent repeat procedures, suggesting that repeat endoscopy for dysphagia has a higher yield than initial endoscopy.
As mentioned previously, esophageal stricture was more common in non-Hispanic whites than in other ethnic groups, whereas Asian/Pacific Islanders were more likely to have had a normal exam with a significantly lower prevalence of EU, stricture, and SR. We speculate that this reflects the lower incidence of GERD in Asian populations compared to Western non-Hispanic white populations [22]. Further studies are required to evaluate this trend.
The strengths of this study include its large number of patients and many diverse practice sites that contributed data. Every patient included in the database was required to have an endoscopic diagnosis entered into the procedure report; equivocal findings were not recognized. This is also a limitation of the study in that only the diagnostic findings in the procedure template were available for analysis and other findings may not have been accurately captured.
Additional limitations of this study include the fact that the CORI database is not detailed enough to fully evaluate other causes of esophagitis such as virus-, bacteria-, and pill-induced etiology or Zenker’s diverticula. Diagnoses requiring additional testing (i.e., mucosal biopsies/histology, esophageal manometry, esophagogram) were also not available from the database. Therefore, causes for dysphagia, including EoE, achalasia, scleroderma, or other esophageal motility disorders were not available for analysis. Finally, we believe that the Asian/Pacific Islander population was not robust enough to generalize the finding.
Conclusion
Overall, this study allows for better preprocedural discussions with patients and other physicians regarding the investigation of dysphagia by upper endoscopy. This is the first study to describe the prevalence of different endoscopic findings in patients with dysphagia referred for upper endoscopy. The prevalence of endoscopic findings among patients with dysphagia differs significantly by gender, age, race/ethnicity, and repeat procedure. In this study, esophageal stricture was the most common finding followed by normal exam, EU, SR, EFI, and suspected malignancy. For patients who underwent repeat endoscopy, abnormal findings were significantly more likely to be identified. This study provides baseline prevalence data of the existing major endoscopic findings in patients who underwent upper endoscopy for dysphagia. Future studies can compare changing trends in these existing causes of dysphagia and evaluate the emergence of new causes using these data.
Contributor Information
Chaya Krishnamurthy, Division of Gastroenterology, Department of Internal Medicine, University of Utah School of Medicine, 30 North 1900 East, SOM 4R118, Salt Lake City, UT 84132, USA.
Kristen Hilden, Division of Gastroenterology, Department of Internal Medicine, University of Utah School of Medicine, 30 North 1900 East, SOM 4R118, Salt Lake City, UT 84132, USA.
Kathryn A. Peterson, Division of Gastroenterology, Department of Internal Medicine, University of Utah School of Medicine, 30 North 1900 East, SOM 4R118, Salt Lake City, UT 84132, USA.
Nora Mattek, Clinical Outcomes Research Initiative, Portland, OR 97239, USA.
Douglas G. Adler, Division of Gastroenterology, Department of Internal Medicine, University of Utah School of Medicine, 30 North 1900 East, SOM 4R118, Salt Lake City, UT 84132, USA.
John C. Fang, Division of Gastroenterology, Department of Internal Medicine, University of Utah School of Medicine, 30 North 1900 East, SOM 4R118, Salt Lake City, UT 84132, USA.
References
- 1.Cook I, Kahrilas P. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999;116:455–78. doi: 10.1016/s0016-5085(99)70144-7. [DOI] [PubMed] [Google Scholar]
- 2.Lindgren S, Janzon L. Prevalence of swallowing complaints and clinical findings among 50 70 year old men and women in an urban population. Dysphagia. 1991;6:187–92. doi: 10.1007/BF02493524. [DOI] [PubMed] [Google Scholar]
- 3.Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ., III Dyspepsia and dyspepsia subgroups: a population-based study. Gastroenterology. 1992;102:1259–68. [PubMed] [Google Scholar]
- 4.American Speech-Language-Hearing Association. Prevalence of speech, voice and language disorders in the United States. Rockville, MD: American Speech-Language-Hearing Association; 1994. [Google Scholar]
- 5.Eslick GD, Talley NJ. Dysphagia: epidemiology, risk factors and impact on quality of life—a population-based study. Aliment Pharmacol Ther. 2008;27:971–9. doi: 10.1111/j.1365-2036.2008.03664.x. [DOI] [PubMed] [Google Scholar]
- 6.Ekberg O, Hamdy S, Wojsard V, Hannig-Wuttge A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. In: Mackenzie SH, Go M, Chadwick B, Thomas KL, Fang JC, editors. Dysphagia. Vol. 17. 2002. pp. 139–46. [DOI] [PubMed] [Google Scholar]
- 7.Lind CD. Dysphagia: evaluation and treatment. Gastroenterol Clin N Am. 2003;32:553–75. doi: 10.1016/s0889-8553(03)00024-4. [DOI] [PubMed] [Google Scholar]
- 8.Wilkins T, Gillies RA, Thomas AM, Wagner PG. The prevalence of dysphagia in primary care patients: a HamesNet Research Network Study. J Am Board Fam Med. 2007;20:144–50. doi: 10.3122/jabfm.2007.02.060045. [DOI] [PubMed] [Google Scholar]
- 9.Richter JE. Practical approach to the diagnosis and treatment of esophageal dysphagia. Compr Ther. 1998;24:446–53. [PubMed] [Google Scholar]
- 10.Locke GR, III, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., III Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmstead County, Minnesota. Gastroenterology. 1997;112:1448–56. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 11.Locke GR, III, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., III Risk factors associated with symptoms of gastroesophageal reflux. Am J Med. 1999;106:642–9. doi: 10.1016/s0002-9343(99)00121-7. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman DA, DeGarmo PL, Fleischer DE, Eisen GM, Helfand M. Patterns of endoscopy use in the United States. Gastroenterology. 2000;118:619–24. doi: 10.1016/s0016-5085(00)70269-1. [DOI] [PubMed] [Google Scholar]
- 13.Marks RD, Richter JE. Peptic strictures of the esophagus. Am J Gastroenterol. 1993;88:1160–73. [PubMed] [Google Scholar]
- 14.Kovalak M, Peterson KA, Thomas KL, et al. Eosinophilic esophagitis and gastroesophageal reflux: independent or interactive relationship? Gastroenterology. 2008;134:A290. [Google Scholar]
- 15.Attwood SE, Lamb CA. Eosinophilic oesophagitis and other non-reflux inflammatory conditions of the oesophagus: diagnostic imaging and management. Best Pract Res Clin Gastroenterol. 2008;22:639–60. doi: 10.1016/j.bpg.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Baxi S, Gupta SK, Swigonski N, et al. Clinical presentation of patients with eosinophilic inflammation of the esophagus. Gastrointest Endosc. 2006;64:473–8. doi: 10.1016/j.gie.2006.03.931. [DOI] [PubMed] [Google Scholar]
- 17.Kuwada S, Lamphier S, Hilden K, Peterson KA. Eosinophilic oesophagitis in patients presenting with dysphagia—a prospective analysis. Aliment Pharmacol Ther. 2008;28:1140–6. doi: 10.1111/j.1365-2036.2008.03795.x. [DOI] [PubMed] [Google Scholar]
- 18.Westbrook JL. Trends in the utilization of diagnostic upper GI endoscopy in New South Wales, Australia, 1988 to 1998. Gastrointest Endosc. 2002;55:847–53. doi: 10.1067/mge.2002.124634. [DOI] [PubMed] [Google Scholar]
- 19.Galvez C, Garrigues V, Ortiz V, Ponce M, Nos P, Ponce J. Healthcare seeking for constipation: a population-based survey in the Mediterranean area of Spain. Aliment Pharmacol Ther. 2006;24:421–8. doi: 10.1111/j.1365-2036.2006.02981.x. [DOI] [PubMed] [Google Scholar]
- 20.Parslow R, Jorm A, Christensen H, Jacomb PA, Rodgers B. Gender differences in factors affecting use of health services: an analysis of a community study of middle-aged and older Australians. Soc Sci Med. 2004;59:2121–9. doi: 10.1016/j.socscimed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 21.Byrne KR, Panagiotakis PH, Hilden K, Thomas KL, Peterson KA, Fang JC. Retrospective analysis of esophageal food impaction: differences in etiology by age and gender. Dig Dis Sci. 2006;52:717–21. doi: 10.1007/s10620-006-9499-0. [DOI] [PubMed] [Google Scholar]
- 22.Wu JC. Gastroesophageal reflux disease: an Asian perspective. J Gastroenterol Hepatol. 2008;23:1785–93. doi: 10.1111/j.1440-1746.2008.05684.x. [DOI] [PubMed] [Google Scholar]


