Abstract
Purpose of review
Posterior cruciate ligament (PCL) injuries are relatively uncommon injuries. As such, there is a dearth of high-quality studies in the literature examining the operative management of PCL injuries and a lack of clear consensus on what the optimal method should be. The goal of this review was to conduct a comprehensive evaluation of recent literature and provide an evidence-based algorithm to optimize surgical decision-making and outcomes for PCL reconstruction.
Recent findings
Recent literature confirms that transtibial PCL reconstruction is a reliable and reproducible method to manage PCL injuries and results in satisfactory patient outcomes. However, there does not yet appear to be enough new, compelling information to conclusively determine an optimal method for surgical management.
Summary
Our preferred method of management for operative PCL injuries is a single bundle transtibial PCL reconstruction, which is supported by the current body of literature. Future high-quality research studies are necessary to further guide treatment algorithms.
Keywords: Posterior cruciate ligament, Transtibial, Knee, Arthroscopy, Sports medicine
Introduction
Our knowledge about the posterior cruciate ligament, including its function, anatomy, and biomechanics, has increased over the years. Despite this, there remains a lack of clarity regarding optimal operative and non-operative management of posterior cruciate ligament (PCL) injuries. The current available data and associated outcomes demonstrate that the existing techniques for PCL reconstruction, including arthroscopic transtibial and open tibial inlay, produce satisfactory patient outcomes. The following review will briefly discuss the relevant highlights of PCL anatomy, diagnosis, outcomes of arthroscopic transtibial PCL reconstruction, and our preferred surgical technique for arthroscopic single bundle transtibial PCL reconstruction.
Anatomy
The primary function of the PCL is to restrict posterior translation of the tibia, though it has also been found to serve as a secondary restraint to internal and external rotation [1–8]. The PCL consists of two bundles, anterolateral and posteromedial, both of which restrain posterior translation of the tibia throughout the range of knee flexion. Previously, it had been suggested that the two bundles maintained a reciprocal relationship. However, recent data have demonstrated that their relationship may be more co-dominant in nature, functioning synergistically throughout the entire arc of knee motion [9, 10]. The PCL complex also includes the anterior and posterior meniscofemoral ligaments commonly referred to as the ligaments of Humphrey and Wrisberg, respectively. The precise function of these meniscofemoral ligaments has been debated but is currently appreciated to be that of secondary restraints to posterior tibial translation [11, 12].
Diagnosis
Proper diagnosis of PCL injuries begins with a comprehensive patient history, physical examination, and diagnostic imaging. The history of PCL injury most commonly includes a direct posterior force on the proximal tibia, often during sports participation such as a fall on a flexed knee, or a traumatic event, such as the classic “dashboard injury” during a motor vehicle accident. Acutely, the patient may report posterior knee pain and a mild to moderate effusion, whereas patients with chronic PCL insufficiency may complain of vague, anterior knee pain and difficulty with certain activities such as ascending and descending stairs. Pure instability is an uncommon complaint in both the acute and chronic setting. The incidence of acute PCL injury reported in the literature ranges from 1–44% [13]. Given the higher energy mechanism in the acute setting, isolated PCL injuries are rare and concomitant injuries to the ACL, medial collateral ligament (MCL), and PLC are frequently present. Fanelli et al. reported in their study that 46, 31, and 62% of PCL injuries in the trauma setting had concomitant injuries to the ACL, MCL, and PLC, respectively [14].
Performing a thorough physical exam and comprehensive diagnostic imaging are important in identifying other associated injuries. The presence of other injuries can affect the treatment algorithm, and therefore, special care should be taken to thoroughly evaluate all relevant intra-articular structures of the knee. The posterior drawer test is the most sensitive and specific test to clinically assess for PCL insufficiency [15]. Additional clinical exam maneuvers that can supplement the posterior drawer test include assessing for the posterior sag sign, the quadriceps active test and the reverse pivot shift test. Imaging, in the form of plain radiographs and MRI, can help with diagnosis and evaluation of other injuries such as fractures, cartilage lesions, meniscus injury, and damage to other ligamentous structures. MRI has been found to be a very sensitive and specific tool in evaluation of acute PCL injuries [16–18]. This sensitivity and specificity is reduced in the chronic setting, in which case stress radiographs can provide a better objective means to assess PCL integrity [19–21].
After an accurate diagnosis of PCL injury has been made, the indication to proceed with surgical intervention will vary based upon the severity of clinical symptoms. Indications for PCL reconstruction following an acute injury can include a combined PCL injury such as a multiligamentous injury, a grade III PCL injury with failure of conservative treatment or a complete PCL tear with an associated meniscus tear/root avulsion. Surgical indications for a chronic PCL injury are not as clear and often involve a failure of initial conservative management, which includes activity modification, physical therapy, and non-steroidal anti-inflammatory medications. When these measures are insufficient, patients will present with some level of functional limitations, which can include subjective complaints of difficulty and pain with stairs, difficulty with descent on inclines and/or vague instability. Frequently, surgical intervention is indicated secondary to the detrimental effects of PCL deficiency on the quality of life and function of the patient.
Outcomes
Early studies examining the biomechanical differences between the transtibial and tibial inlay techniques were significant for concerns regarding the “killer turn” that the graft had to traverse as a part of the arthroscopic transtibial reconstruction. These studies suggested that because of this acute angle, the graft sustained damage to its structural integrity with cyclic loading and eventually became attenuated, which led to increased posterior laxity [22–24]. In contrast, there have been other cadaveric studies that have shown no significant differences between open tibial inlay and arthroscopic transtibial techniques, when comparing objective knee laxity and posterior tibial translation [25, 26]. In general, these concerns regarding the killer turn and its effect on the PCL graft have not demonstrated clinical significance to date. Some theorize that concerns regarding graft abrasion and eventual attenuation may not be applicable in a biologic environment where remodeling may occur [27]. Apprehension over the open tibial inlay technique is largely related to potential post-operative complications, risk to the posterior neurovascular structures, the need for prone positioning, and increased operating room time [28]. Complications that have been reported in the literature associated with the open tibial inlay technique include post-operative hematoma at the incision site, transient saphenous nerve numbness, popliteal vein laceration, infection at the incision site, failure of bone plug fixation, and bone plug breakage during screw fixation [28–31].
Short-term outcomes have been largely equivalent when comparing transtibial and tibial inlay techniques [32, 33]. A study by MacGillivray et al. found no significant differences in posterior drawer testing, objective knee laxity, functional test results, or subjective knee outcome scores between the two techniques [32]. Panchal et al. conducted a systematic review of biomechanical and clinical studies comparing open tibial inlay and arthroscopic transtibial PCL reconstructions. They concluded that due to the conflicting results of biomechanical studies, as well as the limitations of many of the clinical studies, a definitive conclusion could not be reached regarding superiority of one technique over the other [34]. Despite this, concerns continue to exist that with longer follow-up, the transtibial graft could eventually undergo structural damage due to repetitive cyclic loads and lead to attenuation and laxity. Song et al. conducted a cohort study comparing 36 transtibial PCL reconstructions to 30 tibial inlay PCL reconstructions, with mean follow-up of 148 months. They found that there were no significant differences between the groups when looking at subjective outcome scores, objective knee laxity, mean side-to-side difference, and development of arthritic changes on radiographs [35••]. Boutefnouchet et al. reported that 93% of their patients had good/excellent Lysholm knee scores, and all patients had normal or nearly normal KT-2000 arthrometer measurements at a mean 4.1 years after a single bundle arthroscopic transtibial reconstruction with hamstring autograft [36]. A recent systematic review by Shin et al. confirms the current consensus that outcomes between the two techniques are equivalent. Their review included seven prior studies directly comparing transtibial and tibial inlay single bundle PCL reconstruction, with primary outcomes consisting of postoperative knee outcome scores and residual posterior laxity. They found no clinically significant differences between transtibial and tibial inlay techniques regarding post-operative Tegner and Lysholm scores or residual posterior laxity that was based upon radiographic or clinical assessment [37••].
Similarly, the debate between single and double bundle grafts has yet to be resolved. The literature thus far has proven to be largely equivalent regarding clinical outcomes, though there is a lack of high-quality studies. Various studies have tried to quantify the differences between these two techniques. Two studies in particular suggest that although clinical outcomes (Lysholm knee and Tegner activity scores) between the two techniques were comparable at short to midterm follow-up, the objective findings of posterior translation (compared with the contralateral side) and objective IKDC scores were significantly improved with the double bundle reconstruction technique [38•,39]. It remains unclear at this time if these differences in objective findings will affect long-term clinical outcomes.
Additional technical variations have been examined in the literature including graft choice and, more recently, remnant preservation of the native ligament. Remnant preservation has been described as a possible adjunct to graft healing in single bundle reconstruction [40]. Preservation and juxtaposition of the PCL remnant to the graft may improve vascular ingrowth and thus provide an accelerated scaffold for healing and graft integration [40]. While multiple studies have shown reasonably good clinical outcomes with remnant preservation in PCL reconstruction, there is a lack of prospective comparative studies and, to the authors’ knowledge, no data exists demonstrating whether remnant preservation can lead to superior outcomes [41•,42].
Allograft and autograft tissue have both been shown to have satisfactory outcomes [43, 44]. Recently, Li et al. specifically compared hamstring autograft and tibialis anterior allograft in a cohort of patients that underwent arthroscopic transtibial PCL reconstruction. They found that both groups improved significantly after reconstruction and did not find substantial differences in outcomes including knee laxity and function between the two groups [45•]. Rates of tibial tunnel enlargement have also not been found to be different between allograft and mixed autograft/allograft (hybrid graft) PCL reconstruction. The overall rates of enlargement appear to be low at short-term follow-up with improved functional outcomes in both the allograft and hybrid graft groups [46•].
At this time, there is insufficient evidence in the existing literature to support an optimal method of reconstruction. The current, small body of literature regarding PCL reconstruction consists mainly of heterogeneous level III and IV studies with conflicting outcomes. However, there is potential for future clarity on the subject with the onset of higher quality research and long-term outcome studies.
Author’s Preferred Surgical Technique
In this section, we describe our preferred technique for a single bundle transtibial PCL reconstruction with Achilles allograft.
Following standard perioperative procedure, the patient is transported into the operating room, intubated and given pre-operative antibiotics. A non-sterile tourniquet is placed on the upper thigh, and the patient is positioned in the supine position with a lateral post at the level of the tourniquet and a footrest or a beanbag affixed to the table near the foot so that the knee can be flexed and maintained at 90° of flexion when necessary. A sequential compression device is placed on the contralateral extremity for the duration of the procedure to minimize the risk of deep venous thrombosis.
A thorough bilateral knee exam under anesthesia is performed prior to the sterile prep to again confirm the diagnosis and identify other potential unexpected or undetected ligamentous injuries. We recommend performing a posterior drawer, assessing for posterior sag as well as evaluating for ACL, PLC, or PMC and collateral ligament injuries with dynamic exam maneuvers.
After completion of the exam under anesthesia, the limb is prepped and draped in the standard sterile fashion. A standard anterolateral portal is made, and a diagnostic arthroscopy is conducted using a standard 30° arthroscope.
Surgical Tip: care should be taken to create this portal immediately abutting the patellar tendon to maximize notch and posterior compartment visualization.
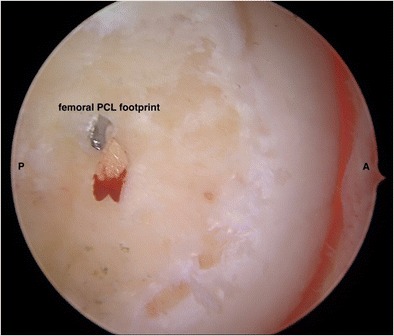
Diagnostic arthroscopy begins with visualization of both gutters, the suprapatellar pouch and the patellofemoral joint. An anteromedial portal is then established in the standard fashion. Again, care should be taken to create this portal immediately abutting the patellar tendon. The medial and lateral compartments as well as the notch are assessed for any chondral or meniscal injuries. The ACL and PCL should then be visualized, and a posterior drawer stress can be placed on the knee to arthroscopically visualize the degree of ligament laxity. This is particularly useful in the setting of chronic injury where the ligament may be scarred to adjacent intra-articular structures. The PCL remnant is debrided utilizing a shaver and/or a radiofrequency ablation device, leaving a small amount of remnant on the femoral condyle for footprint visualization (Fig. 1). Our preference is to preserve the meniscofemoral ligaments if they are intact and do not impede surgical exposure or visualization. At this point, an accessory posteromedial portal is established under arthroscopic visualization with a spinal needle, followed by a stab incision and blunt intra-articular dissection.
Fig. 1.
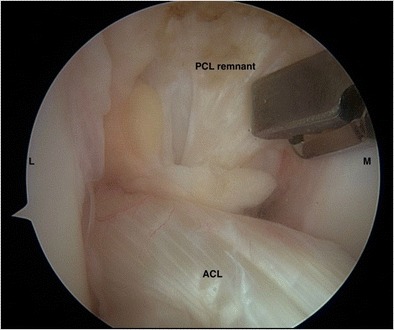
Intraoperative arthroscopic view of the PCL remnant of a right knee. An intact ACL can be visualized in the lower half of the screen. L lateral, M medial
Surgical Tip: The posteromedial portal should be established in the “soft spot” between the semimembranosus and medial head of the gastrocnemius with the knee flexed to 90°. The knee should be distended with arthroscopic fluid prior to establishing this portal to minimize the risk iatrogenic injury to the saphenous nerve. A 0.062 guide wire can be used as a percutaneous guide wire to introduce a cannulated 5.0 mm cannula to establish and maintain the posteromedial portal. This allows ease of instrumentation exchange including visualization with the arthroscope and minimizes posterior fluid extravasation.
The tibial PCL footprint is identified with careful subperiosteal dissection using a radiofrequency ablation device and shaver placed through the posteromedial portal while visualizing through the anterolateral portal. A 70° arthroscope is then utilized through the posteromedial portal to complete the proximal tibial dissection and final preparation of the tibial footprint. This dissection detaches the tibial PCL attachment approximately 12 to 15-mm along the posterior aspect of the proximal tibia until the proximal-most fibers of the popliteus muscle are visualized (Fig. 2). Once adequate dissection is completed, a 3-cm incision is made along the anteromedial aspect of the tibia from the tibial tubercle distally and midway between the anterior tibial spine and posteromedial tibial ridge. The pes anserinus is identified and subperiosteal dissection is conducted immediately proximal to this area with care taken to minimize disruption of the MCL attachment at the position of the desired PCL tunnel. A PCL tibial guide set at 65° is placed flush against the tibial spines and between 10 and 15-mm distal to the joint line to precisely locate the tibial footprint for tunnel drilling (Fig. 3).
Fig. 2.
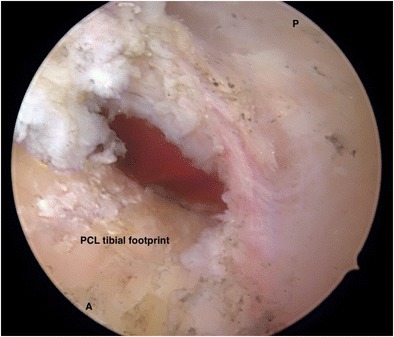
Intraoperative arthroscopic view of a right knee tibial PCL footprint that has been dissected subperiosteally and exposed. A anterior, P posterior
Fig. 3.

Intraoperative arthroscopic view of a PCL tibial guide centered over the tibial PCL footprint in a right knee prior to guidewire insertion
Surgical Tip: A switching stick can be used to exchange the posteromedial cannula with the arthroscope cannula thereby allowing direct visualization of the tibial footprint during guide placement, pin advancement, and reaming through the posteromedial portal. A 70° scope can be utilized at this time to help with visualization.
A guidewire is advanced into the tibial guide and fluoroscopic imaging is used to confirm appropriate placement, after which an 11-mm tibial socket is reamed under direct fluoroscopic and arthroscopic visualization (Fig. 4). Due to the close proximity of the posterior neurovascular structures, completion of the reaming through the posterior cortex of the tibia can be done by hand.
Fig. 4.
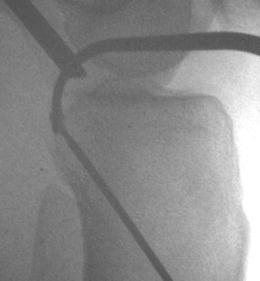
Intraoperative fluoroscopic image confirming correct guidewire placement to the PCL tibial footprint
Surgical Tip: It can be helpful at this time to contour the anterior aperture of the tibial footprint with a shaver or a rasp to minimize any sharp edges to facilitate graft passage and minimize graft abrasion once it is passed.
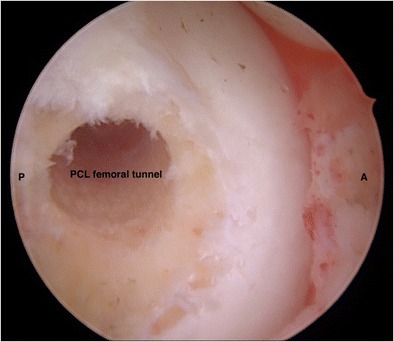
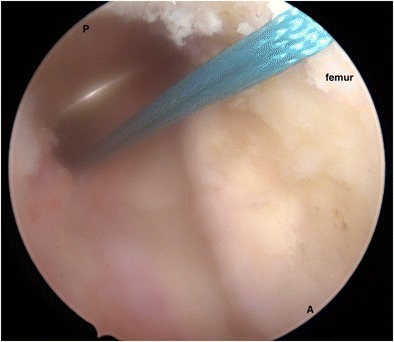
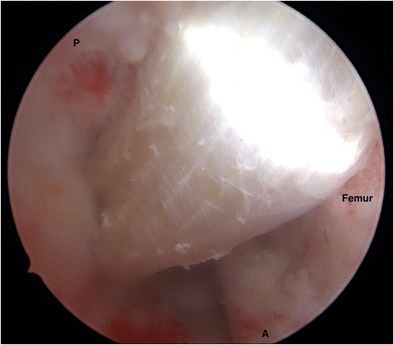
The femoral tunnel is created using a two-incision technique. A 3-cm vertical incision along the anteromedial aspect of the distal femur is made, and dissection is carried down through the skin and subcutaneous tissue to the vastus medialis obliquus (VMO). The fascia overlying the VMO is incised along its fibers, and the VMO is bluntly retracted laterally to expose the anteromedial aspect of the distal femur. A small periosteal window is made, and the PCL femoral guide is angled such that the guide pin inserts immediately distal to the anteromedial femoral metadiaphyseal junction and enters the PCL intraarticular femoral footprint with the 8-mm position aligned with the medial femoral condyle osteochondral margin. When drilling an 11-mm tunnel, this position will provide a safe subchondral bone bridge and allow positioning within the native PCL femoral footprint (Fig. 5). After the guide has been positioned properly, a guidewire is placed with fluoroscopic and arthroscopic confirmation (Fig. 6). An 11-mm tunnel is reamed outside-in over the guidewire under direct visualization (Fig. 7). Care should be taken to ensure that there is a 2-mm bridge of bone between the tunnel and the anterior aspect of the femur. Subchondral bone should be preserved to minimize the chances of osteonecrosis.
Fig. 5.
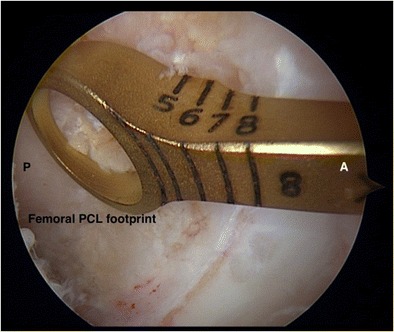
Intraoperative arthroscopic view of the femoral PCL guide centered over the femoral PCL footprint in a right knee. A anterior, P posterior
Fig. 6.
Intraoperative arthroscopic view of the femoral guidewire entering the femoral PCL footprint in a right knee. A anterior, P posterior
Fig. 7.
Intraoperative arthroscopic view of the 11 mm femoral tunnel in a right knee. Note the 2 mm rim of subchondral bone left anterior to the tunnel. A anterior, P posterior
Graft passage and final fixation are then performed. A passing suture is inserted in a retrograde fashion from the tibial tunnel into the femoral tunnel and then retrieved through the anteromedial aspect of the femur (Fig. 8). The passing suture is then utilized to pass the previously prepared Achilles allograft from the femoral tunnel into the tibial tunnel (Fig. 9).
Fig. 8.
Intraoperative arthroscopic view from the anterolateral portal of the passing suture that has been passed retrograde from the tibial tunnel into and out the femoral tunnel of a right knee. A anterior, P posterior
Fig. 9.
Intraoperative arthroscopic view from the anterolateral portal of the PCL graft that has been passed and preliminarily secured on the femoral side of a right knee. A anterior, P posterior
Surgical Tip: The previously placed posteromedial switching stick can be used as a pulley over which the graft can be passed through the tibial tunnel. This switching stick can facilitate directing of the graft over the tibial ridge and minimize graft abrasion.
Once the graft is passed, the 11-mm bone plug is seated flush in the femoral tunnel and secured with a 7 × 20 mm aperture interference screw. After securing the graft on the femoral side, the knee is cycled with tension on the graft to minimize any residual laxity. Attention is then directed to final fixation of the tibial graft. With the knee flexed to 90° and a significant anterior drawer force on the proximal tibia, the graft is tensioned manually and secured in the tibial tunnel with an 11 × 35-mm biocomposite screw. We prefer to back up the tibial-sided fixation with a screw and spiked washer combination to minimize potential graft laxity that could occur from the metaphyseal nature of the biocomposite screw fixation. This screw and spiked washer are placed through a small stab incision in the mid-substance of the remaining limb of the Achilles allograft and within the previously placed sutures. This technique allows both suture and graft fixation simultaneously. A unicortical drill hole and scoring of the anteromedial cortex is then performed followed again by manual traction placed on the Achilles tissue. The screw and washer are then secured directly to the anteromedial tibial cortex. At this point, any remaining excess graft is amputated after the screw and spiked washer are seated.
When satisfactory fixation has been achieved, the stability of the reconstruction is tested with a posterior drawer maneuver and range of motion of the knee is assessed. The incisions and portals are then irrigated thoroughly and hemostasis achieved. The VMO fascia is repaired and closure of the incisions is completed through a standard layered fashion.
Post-operative radiographs are obtained at the 6-week post-operative visit to confirm hardware placement and evaluate fixation (Fig. 10).
Fig. 10.

Post-operative AP and lateral radiographs of a 23-year-old female who underwent arthroscopic single bundle transtibial PCL reconstruction with Achilles allograft. Note the metal interference screw fixation in the femur and the biocomposite screw fixation of the tibia that is backed up with a screw and spiked washer
Conclusions
Transtibial PCL reconstruction has been shown to be a safe and effective method of treating operative PCL injuries while decreasing the potential morbidity associated with an open posterior approach to the knee. The literature has thus far found clinical outcomes associated with arthroscopic transtibial PCL reconstruction to be comparable to those of open tibial inlay techniques. While our preference is for a single bundle transtibial PCL reconstruction, we recommend that each individual surgeon select the technique that he or she is able to reliably and reproducibly perform.
Compliance with Ethical Standards
Conflict of Interest
Travis G. Maak reports personal fees from Arthrex, outside the submitted work. Jessica Shin reports no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors. All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Footnotes
This article is part of the Topical Collection on PCL Update
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Gill TJ, DeFrate LE, Wang C, et al. The biomechanical effect of posterior cruciate ligament reconstruction on knee joint function: kinematic response to simulated muscle loads. Am J Sports Med. 2003;31(4):530–536. doi: 10.1177/03635465030310040901. [DOI] [PubMed] [Google Scholar]
- 2.Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee: a biomechanical study. J Bone Joint Surg Am. 1987;69(2):233–242. doi: 10.2106/00004623-198769020-00010. [DOI] [PubMed] [Google Scholar]
- 3.Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin TM, Woo SL. Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med. 2000;28(2):144–151. doi: 10.1177/03635465000280020201. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Årøen A, Engebretsen L, LaPrade RF. Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. 2013;41(12):2828–2838. doi: 10.1177/0363546513504287. [DOI] [PubMed] [Google Scholar]
- 5.Li G, Gill TJ, DeFrate LE, Zayontz S, Glatt V, Zarins B. Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads—an in vitro experimental study. J Orthop Res. 2002;20(4):887–892. doi: 10.1016/S0736-0266(01)00184-X. [DOI] [PubMed] [Google Scholar]
- 6.Margheritini F, Rihn JA, Mauro CS, Stabile KJ, Woo SL, Harner CD. Biomechanics of initial tibial fixation in posterior cruciate ligament reconstruction. Arthroscopy. 2005;21(10):1164–1171. doi: 10.1016/j.arthro.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 7.Markolf KL, Feeley BT, Tejwani SG, Martin DE, McAllister DR. Changes in knee laxity and ligament force after sectioning the posteromedial bundle of the posterior cruciate ligament. Arthroscopy. 2006;22(10):1100–1106. doi: 10.1016/j.arthro.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Mauro CS, Sekiya JK, Stabile KJ, Haemmerle MJ, Harner CD. Double-bundle PCL and posterolateral corner reconstruction components are codominant. Clin Orthop Relat Res. 2008;466(9):2247–2254. doi: 10.1007/s11999-008-0319-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papannagari R, DeFrate LE, Nha KW, et al. Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med. 2007;35(9):1507–1512. doi: 10.1177/0363546507300061. [DOI] [PubMed] [Google Scholar]
- 10.Ahmad CS, Cohen ZA, Levine WN, Gardner TR, Ateshian GA, Mow VC. Codominance of the individual posterior cruciate ligament bundles: an analysis of bundle lengths and orientation. Am J Sports Med. 2003;31(2):221–225. doi: 10.1177/03635465030310021101. [DOI] [PubMed] [Google Scholar]
- 11.Amis AA, Bull AM, Gupte CM, Hijazi I, Race A, Robinson JR. Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):271–281. doi: 10.1007/s00167-003-0410-7. [DOI] [PubMed] [Google Scholar]
- 12.Gupte CM, Bull AM, Thomas RD, Amis AA. A review of the function and biomechanics of the meniscofemoral ligaments. Arthroscopy. 2003;19(2):161–171. doi: 10.1053/jars.2003.50011. [DOI] [PubMed] [Google Scholar]
- 13.Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1999;27(3):276–283. doi: 10.1177/03635465990270030201. [DOI] [PubMed] [Google Scholar]
- 14.Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients, part II. Arthroscopy. 1995;11(5):526–529. doi: 10.1016/0749-8063(95)90127-2. [DOI] [PubMed] [Google Scholar]
- 15.Rubinstein RA, Jr, Shelbourne KD, McCarroll JR, VanMeter CD, Rettig AC. The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med. 1994;22(4):550–557. doi: 10.1177/036354659402200419. [DOI] [PubMed] [Google Scholar]
- 16.Fischer SP, Fox JM, Del Pizzo W, Friedman MJ, Snyder SJ, Ferkel RD. Accuracy of diagnoses from magnetic resonance imaging of the knee: a multi-center analysis of one thousand and fourteen patients. J Bone Joint Surg Am. 1991;73(1):2–10. doi: 10.2106/00004623-199173010-00002. [DOI] [PubMed] [Google Scholar]
- 17.Gross ML, Grover JS, Bassett LW, Seeger LL, Finerman GA. Magnetic resonance imaging of the posterior cruciate ligament: clinical use to improve diagnostic accuracy. Am J Sports Med. 1992;20(6):732–737. doi: 10.1177/036354659202000615. [DOI] [PubMed] [Google Scholar]
- 18.Polly DW, Jr, Callaghan JJ, Sikes RA, McCabe JM, McMahon K, Savory CG. The accuracy of selective magnetic resonance imaging compared with the findings of arthroscopy of the knee. J Bone Joint Surg Am. 1988;70(2):192–198. doi: 10.2106/00004623-198870020-00005. [DOI] [PubMed] [Google Scholar]
- 19.Jackman T, LaPrade RF, Pontinen T, Lender PA. Intraobserver and interobserver reliability of the kneeling technique of stress radiography for the evaluation of posterior knee laxity. Am J Sports Med. 2008;36(8):1571–1576. doi: 10.1177/0363546508315897. [DOI] [PubMed] [Google Scholar]
- 20.Jung TM, Reinhardt C, Scheffler SU, Weiler A. Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1116–1121. doi: 10.1007/s00167-006-0137-3. [DOI] [PubMed] [Google Scholar]
- 21.Schulz MS, Russe K, Lampakis G, Strobel MJ. Reliability of stress radiography for evaluation of posterior knee laxity. Am J Sports Med. 2005;33(4):502–506. doi: 10.1177/0363546504269723. [DOI] [PubMed] [Google Scholar]
- 22.Bergfeld JA, Graham SM, Parker RD, Valdevit AD, Kambic HE. A bio-mechanical comparison of posterior cruciate ligament reconstructions using single- and double-bundle tibial inlay techniques. Am J Sports Med. 2005;33(7):976–981. doi: 10.1177/0363546504273046. [DOI] [PubMed] [Google Scholar]
- 23.Bergfeld JA, McAllister DR, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstruction techniques. Am J Sports Med. 2001;29(2):129–136. doi: 10.1177/03635465010290020401. [DOI] [PubMed] [Google Scholar]
- 24.Markolf KL, Zemanovic JR Matava MJ, Ellis E, Gruber B. Surgical treatment of posterior cruciate ligament tears: an evolving technique. J Am Acad Orthop Surg. 2009;17(7):435–446. doi: 10.5435/00124635-200907000-00004. [DOI] [PubMed] [Google Scholar]
- 25.McAllister DR. Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods. J Bone Joint Surg Am. 2002;84(4):518–524. doi: 10.2106/00004623-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Margheritini F, Mauro CS, Rihn JA, Stabile KJ, Woo SL, Harner CD. Biomechanical comparison of tibial inlay versus transtibial techniques for posterior cruciate ligament reconstruction: analysis of knee kinematics and graft in situ forces. Am J Sports Med. 2004;32(3):587–593. doi: 10.1177/0363546503261717. [DOI] [PubMed] [Google Scholar]
- 27.Ahn JH, Yang HS, Jeong WK, Koh KH. Arthroscopic transtibial posterior cruciate ligament reconstruction with preservation of posterior cruciate ligament fibers: clinical results of minimum 2-year follow-up. Am J Sports Med. 2006;34(2):194–204. doi: 10.1177/0363546505279915. [DOI] [PubMed] [Google Scholar]
- 28.Noyes FR, Barber-Westin S. Posterior cruciate ligament replacement with a two-strand quadriceps tendon-patellar bone autograft and a tibial inlay technique. J Bone Joint Surg Am. 2005;87(6):1241–1252. doi: 10.2106/JBJS.D.02272. [DOI] [PubMed] [Google Scholar]
- 29.Cooper DE, Stewart D. Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10-year follow-up. Am J Sports Med. 2004;32(2):346–360. doi: 10.1177/0363546503261511. [DOI] [PubMed] [Google Scholar]
- 30.Kim SJ, Kim TE, Jo SB, Kung YP. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009;91(11):2543–2549. doi: 10.2106/JBJS.H.01819. [DOI] [PubMed] [Google Scholar]
- 31.Stannard JP, Riley RS, Sheils TM, McGwin G, Volgas DA. Anatomic reconstruction of the posterior cruciate ligament after multiligament knee injuries. A combination of the tibial-inlay and two-femoral-tunnel techniques. Am J Sports Med. 2003;31(2):196–202. doi: 10.1177/03635465030310020701. [DOI] [PubMed] [Google Scholar]
- 32.MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF. Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy. 2006;22(3):320–328. doi: 10.1016/j.arthro.2005.08.057. [DOI] [PubMed] [Google Scholar]
- 33.Seon JK, Song EK. Reconstruction of isolated posterior cruciate ligament injuries: a clinical comparison of the transtibial and tibial inlay techniques. Arthroscopy. 2006;22(1):27–32. doi: 10.1016/j.arthro.2005.08.038. [DOI] [PubMed] [Google Scholar]
- 34.Panchal HB, Sekiya JK. Open tibial inlay versus arthroscopic transtibial posterior cruciate ligament reconstructions. Arthroscopy. 2011;27(9):1289–1295. doi: 10.1016/j.arthro.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 35.Song EK, Park HW, Ahn YS, Seon JK. Transtibial versus tibial inlay techniques for posterior cruciate ligament reconstruction: long-term follow-up study. Am J Sports Med. 2014;42(12):2964–2971. doi: 10.1177/0363546514550982. [DOI] [PubMed] [Google Scholar]
- 36.Boutefnouchet T, Bentayeb M, Qadri Q, Ali S. Long-term outcomes following single-bundle transtibial arthroscopic posterior cruciate ligament reconstruction. Int Orthop. 2013;37(2):337–343. doi: 10.1007/s00264-012-1609-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shin YS, Kim HJ, Lee DH. No clinically important difference in knee scores or instability between transtibial and inlay techniques for PCL reconstruction: a systematic review. Clin Orthop Relat Res. 2017;475:1239–1248. doi: 10.1007/s11999-016-5176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li Y, Li J, Wang J, Gao S, Zhang Y. Comparison of single-bundle and double-bundle isolated posterior cruciate ligament reconstruction with allograft: a prospective, randomized study. Arthroscopy. 2014;30(6):695–700. doi: 10.1016/j.arthro.2014.02.035. [DOI] [PubMed] [Google Scholar]
- 39.Yoon KH, Bae DK, Song SJ, Cho HJ, Lee JH. A prospective randomized study comparing arthroscopic single-bundle and double-bundle posterior cruciate ligament reconstructions preserving remnant fibers. Am J Sports Med. 2011;39(3):474–480. doi: 10.1177/0363546510382206. [DOI] [PubMed] [Google Scholar]
- 40.Del Buono A, Radmilovic J, Gargano G, Gatto S, Maffulli N. Augmentation or reconstruction of PCL? A quantitative review. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1050–1063. doi: 10.1007/s00167-013-2418-y. [DOI] [PubMed] [Google Scholar]
- 41.Lee DW, Jang HW, Lee YS, Oh SJ, Kim JY, Song HE, Kim JG. Clinical, functional, and morphological evaluations of posterior cruciate ligament reconstruction with remnant preservation: minimum 2-year follow-up. Am J Sports Med. 2014;42(8):1822–1831. doi: 10.1177/0363546514536680. [DOI] [PubMed] [Google Scholar]
- 42.Lee SH, Jung YB, Lee HJ, Jung HJ, Kim SH. Remnant preservation is helpful to obtain good clinical results in posterior cruciate ligament reconstruction: comparison of clinical results of three techniques. Clin Orthop Surg. 2013;5(4):278–286. doi: 10.4055/cios.2013.5.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hudgens JL, Gillette BP, Krych AJ, Stuart MJ, May JH, Levy BA. Allograft versus autograft in posterior cruciate ligament reconstruction: an evidence-based systematic review. J Knee Surg. 2013;26(2):109–1U5. doi: 10.1055/s-0032-1319778. [DOI] [PubMed] [Google Scholar]
- 44.Wang CJ, Chan YS, Weng LH, Yuan LJ, Chen HS. Comparison of autogenous and allogenous posterior cruciate ligament reconstructions of the knee. Injury. 2004;35:1279–1285. doi: 10.1016/j.injury.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 45.Li B, Wang JS, He M, Wang GB, Shen P, Bai LH. Comparison of hamstring tendon autograft and tibialis anterior allograft in arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3077–3084. doi: 10.1007/s00167-014-3267-z. [DOI] [PubMed] [Google Scholar]
- 46.Kwon JH, Han JH, Jo DY, Park HJ, Lee SY, Bhandare N, Suh DW, Nha KW. Tunnel volume enlargement after posterior cruciate ligament reconstruction: comparison of Achilles allograft with mixed autograft/allograft—a prospective computed tomography study. Arthroscopy. 2014;30(3):326–334. doi: 10.1016/j.arthro.2013.12.004. [DOI] [PubMed] [Google Scholar]


