Abstract
Background
Informal neighbor relationships (NRs) are considered a structural aspect of social relationships. Although NRs might affect physical activity (PA), no previous study has simultaneously examined compositional and contextual associations of NRs with PA. In this study, we examined whether individual- and community-level NRs were independently associated with PA.
Methods
We analyzed cross-sectional data from 8592 (4340 men and 4252 women) non-disabled residents aged 65–84 years from all 18 districts of Ota City, Tokyo. PA was assessed by using the International Physical Activity Questionnaire-Short Form. In addition, we calculated moderate-to-vigorous PA (MVPA), its components (vigorous PA [VPA], moderate PA [MPA], and walking time [WT]), and sitting time (ST). Individual-level NRs were categorized as “visiting each other,” “standing and chatting,” “exchange of greetings,” or “none.” Community-level NRs were defined as the proportions of residents with active NRs (i.e., those in the categories visiting each other and standing and chatting) in the 18 districts. Using multilevel regression analyses, we examined independent associations of individual- and community-level NRs with PA variables and adjusted for important confounders.
Results
Individual-level NRs were consistently positively associated with MVPA and its components (VPA, MPA [in men], and WT) in both sexes, and the dose–response relationships were significant (all P < 0.041 for trend). In men, community-level NRs (by 1% estimation) were positively associated with individual MVPA (2.1 metabolic equivalent-hours/week, 95% confidence interval: 0.7–3.4), VPA (8.6 min/week, 2.7–14.4), and WT (11.6 min/week, 2.2–20.9), regardless of the degree of individual-level NRs. Significant cross-level interactions of NRs with MVPA and VPA were observed among men, and the dose–response relationships were significant (both P < 0.037 for trend). Neither individual- nor community-level NRs were associated with ST in either sex.
Conclusions
Men and women with inaccessible neighbors engaged in less MVPA, while men living in communities with active NRs engaged in more MVPA, regardless of individual-level NRs. NRs at the individual and community level might help prevent physical inactivity among men.
Keywords: Physical activity, Sitting time, Sedentary behavior, Social relationships, Social capital, Older adults, Multilevel analysis
Background
Physical inactivity is an important contributor to non-communicable diseases and—after high blood pressure, tobacco use, and high blood glucose—is the fourth most important risk factor for mortality [1, 2]. Among older adults, physical activity (PA) includes recreational or leisure-time activity, transportation, occupation, household chores, play, games, sports, and planned exercise in the context of daily, family, and community activities [1]. Regular PA helps maintain and improve physical and cognitive function among older adults [3–5]. Despite growing evidence of the health benefits of PA and the presence of established recommendations for healthy aging [1, 6], physical inactivity remains a major concern for older and younger adults [7]. Thus, attention has increasingly focused on public health efforts designed to increase PA. In Japan, a new initiative, Healthy Japan 21 (second term)—a 10-year national health promotion campaign to extend healthy life expectancy and reduce health disparities by establishing targets in 53 specific areas [8]—was launched in 2013 by the Ministry of Health, Labor and Welfare. Increasing PA is one of its explicit goals.
Recent public health studies have examined the social connection offered by relationships, as social relationships can affect health behaviors such as PA [9] and outcomes such as mortality [10–12] and are likely to promote healthy communities. Social relationships are broadly defined as the degree to which individuals are interconnected and embedded in communities [13] and have both structural and functional aspects. The structural aspects include social integration, which refers to an individual’s overall level of involvement with informal social relationships (e.g., having a spouse), formal social relationships (e.g., those with volunteer organizations), and the social network, which refers to the web of social relationships surrounding an individual, particularly those structural features such as the type and strength of each social relationship [11]. The functional aspects include social support, which refers to the support exchanged through social relationships [11]. Because these aspects of social relationships can be analyzed at the individual and group level, studies should consider them simultaneously when examining their effects on health behaviors.
A previous systematic review [9] found that people with greater social support for PA (especially when it originated from family members) were more likely to engage in leisure-time PA and highlighted the importance of friends as sources of support for leisure-time PA in older adults. Moreover, a previous study of Japanese older adults reported that active relationships with neighbors might ameliorate infrequent eating habits caused by limited access to food [14]. These findings suggest that informal neighbor relationships (NRs) could affect individual health behaviors through pathways such as social support. However, to our knowledge, no previous study has simultaneously investigated the individual-level (compositional) and community-level (contextual) effects of NRs on PA.
Using data from older adults living in a metropolitan area of Japan, we examined whether individual- and community-level NRs were positively associated with PA. Specifically, we examined if each individual- and community-level NR was independently associated with PA and if observed associations differed by sex.
Methods
Study population
We used baseline data from a community-wide intervention study on preventing and reducing frailty in Ota City, Tokyo, Japan (Ota Genki Senior Project), which was launched in 2016 [15]. The full details of the participant selection process were previously published [15]. Briefly, 15,500 residents aged 65–84 years—approximately 10% of the elderly population of Ota City—were selected by using stratified and random sampling strategies in all 18 districts. All participants were physically and cognitively independent, which was defined as absence of long-term care insurance certification.
Of the 15,500 self-administered questionnaires distributed in July 2016, 11,925 were returned (response rate, 76.9%) [15]. After excluding 79 questionnaires from respondents who did not actually live in Ota City, 38 questionnaires that were mostly or completely blank, 19 questionnaires with missing identification labels, 22 questionnaires that were completed by someone other than the participant, 66 questionnaires from hospital inpatients and nursing home residents, and 3109 questionnaires with missing information on PA and/or NRs, a total of 8592 questionnaires (4340 men and 4252 women) were ultimately included in our analysis (Fig. 1). The mean district response rate was 77.1% (range, 71.8–80.8%), and the number of respondents per district was 255 to 2135 (mean, 477).
Fig. 1.
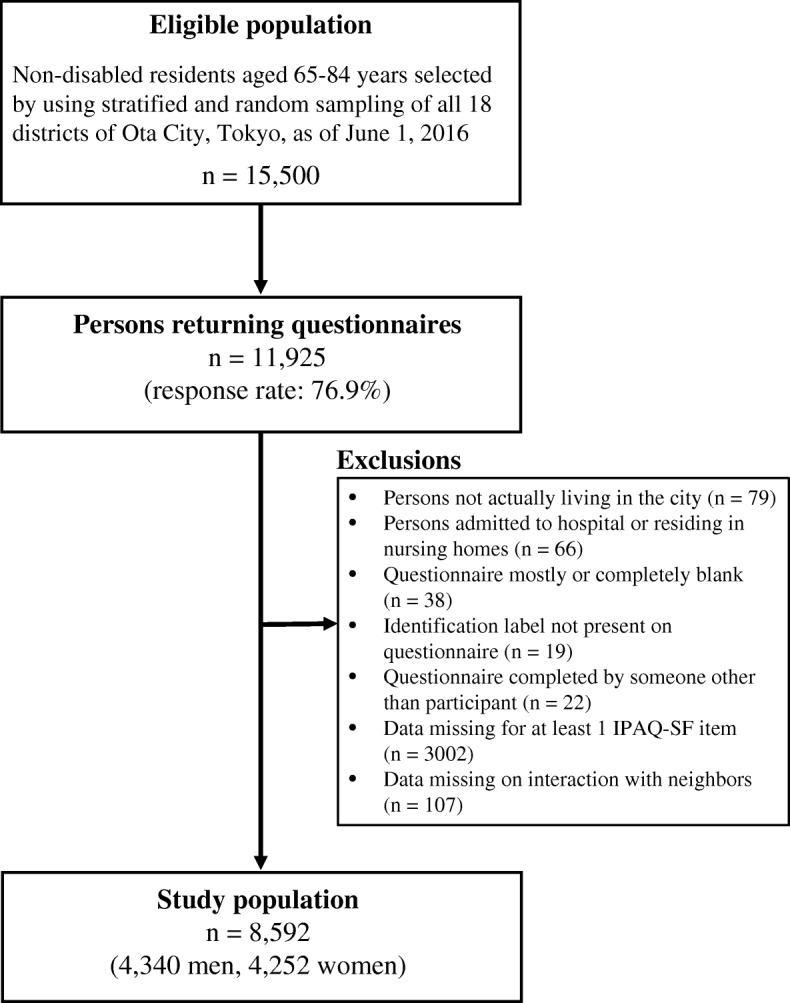
Flow diagram of study participants. IPAQ-SF = International Physical Activity Questionnaire-Short Form
Measurements
PA
PA was evaluated with the Japanese version of the International Physical Activity Questionnaire-Short Form (IPAQ-SF), the external reliability and validity of which have been reported [16, 17]. The IPAQ-SF includes separate items on time spent on vigorous PA (VPA), moderate PA (MPA), walking time (WT), and sitting time (ST) during a typical week. Using these values, we defined total moderate-to-vigorous PA (MVPA) as 7 days × (8.0 metabolic equivalents [METs] × VPA hours/day + 4.0 METs × MPA hours/day + 3.3 METs × walking hours/day) [18]. ST indicates usual weekday ST, apart from sleeping [19].
Individual- and community-level NRs
NR was measured by using the following item: “What kind of relations do you have with people in your neighborhood?” [14] The possible answers were “visiting each other,” “standing and chatting,” “exchange of greetings,” or “none.” We used these categories to categorize individual-level NRs. Community-level NRs were created in accordance with the district units by aggregating individual responses in each district. The proportion of people with an active relationship with neighbors (i.e., the categories visiting each other and standing and chatting) in each district was defined as community-level NRs.
Covariates
The covariates included age, living situation (living with others or alone), duration of residence in the neighborhood (1–29, 30–59, or ≥ 60 years), educational attainment (junior high school, high school, or junior college/vocational college/college/graduate school graduate), equivalent income (< 2.0, 2.0–3.99, ≥4.0 million yen, or unknown), alcohol drinking and tobacco smoking statuses (current, never, or former), body mass index (< 18.5, 18.5–24.9, or ≥ 25 kg/m2), number of chronic diseases (0, 1, or ≥ 2), mobility limitation (presence or absence), self-rated health (excellent to good or fair to poor), depressive mood (presence or absence), employment (yes or no), and social activity (presence or absence). To assess the practical living standard of household members, equivalent income was calculated by dividing household income by the square root of the number of household members [20]. Body mass index was defined as self-rated body weight (kg) divided by self-rated height squared (m2). Number of chronic diseases was defined as the sum of the presence of hypertension, hyperlipidemia, cardiovascular disease, cerebrovascular disease, and diabetes mellitus. Mobility limitation was defined as self-reported difficulty in walking one-quarter of a mile (0.4 km) or climbing 10 steps without resting [21]. Depressive mood was evaluated with the five-item short form of the Geriatric Depression Scale (range, 0–5) [22], and the presence of depression was defined as a score of 2 or greater. Participation in any of the following activities more than once a month was defined as presence of social activity: volunteering, civic action, nonprofit organizations, sports groups, hobby and learning groups, senior citizen clubs, neighborhood associations, or others, but excluding employment. If participants did not respond to the covariates, corresponding observations were assigned to the “missing” categories.
Statistical analyses
All data were analyzed in relation to sex by using Stata 14.2 (StataCorp, TX, USA). The chi-square and unpaired t tests were used to compare individual- and community-level NRs between sexes. To examine whether PA variables were systematically associated with NRs, we used a trend test that extended the Wilcoxon rank-sum test (the “nptrend” command in Stata). The chi-square test was used for other characteristic variables. Because our data had a multilevel structure comprising individuals (at level 1) nested within 18 districts (at level 2), we performed multilevel regression analyses with fixed slopes and random intercept models adjusted for all covariates and calculated partial regression coefficients and 95% confidence intervals (CIs) to identify both the individual-level (compositional) and community-level (contextual) effects of NRs on PA variables. MVPA and its components (VPA, MPA, and WT) and ST were defined as the dependent variables. Individual- and community-level NRs, and their cross-level interaction terms and covariates, were defined as fixed factors. The district was defined as a random factor. A linear trend test was used to assess the dose–response relationship between NR level and PA variables. To avoid issues related to multicollinearity, community-level NRs were centered on their grand mean. An α of 0.05 was considered to indicate statistical significance.
Results
Among 4340 men, 14.9% described their NR status as visiting each other, 30.3% as standing and chatting, 44.3% as exchange of greetings, and 10.5% as none. Among the 4252 women, the responses were 29.8%, 44.6%, 22.1%, and 3.6%, respectively. Overall, women were significantly more likely than men to have active NRs at the individual level (P < 0.001). The mean proportions and standard deviations of people with active NRs (i.e., the categories visiting each other and standing and chatting) in the 18 districts were also significantly higher for women (74.8 ± 2.7%; range, 67.6–81.5%) than for men (45.6 ± 3.0%; range, 37.7–56.4%) (P < 0.001).
Tables 1 and 2 show the PA variables and other participant characteristics, in relation to NR category, for men (Table 1) and women (Table 2). NRs were positively associated with MVPA, VPA, MPA, and WT and inversely associated with ST in men and women (all P < 0.027 for trend). As compared with men who selected the category visiting each other, men with no NRs were younger, more likely to be living alone, and had lived in the neighborhood for less time. They were also more likely to be underweight or obese, had lower equivalent incomes, were less likely to drink alcohol, were less likely to be employed, had less social activity, and had more chronic diseases, more mobility limitations, and more depressive moods and poorer self-rated health (Table 1). Women with no NRs were more likely to be living alone, had lived in the neighborhood for less time, had a lower educational level and equivalent incomes and less chronic disease, were less likely to be employed, and had less social activity, more mobility limitations and depressive moods, and poorer self-rated health.
Table 1.
PA variables and other characteristics of male participants, by category of individual-level NRs
| Variables | Category of NRs | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Visiting each other | Standing and chatting | Exchange of greetings | None | ||||||
| (n = 645, 14.9%) | (n = 1317, 30.3%) | (n = 1923, 44.3%) | (n = 455, 10.5%) | ||||||
| PA, median (interquartile range) | |||||||||
| MVPA, MET-hours/week | 31.8 | (13.2–71.1) | 27.8 | (9.9–59.6) | 23.1 | (8.3–49.5) | 15.4 | (2.2–38.6) | < 0.001b |
| VPA, min/week | 0 | (0–180) | 0 | (0–120) | 0 | (0–60) | 0 | (0–0) | < 0.001b |
| MPA, min/week | 0 | (0–180) | 0 | (0–120) | 0 | (0–75) | 0 | (0–0) | < 0.001b |
| WT, min/week | 300 | (150–600) | 280 | (120–600) | 240 | (90–480) | 180 | (0–420) | < 0.001b |
| ST, min/day | 270 | (180–480) | 300 | (180–480) | 300 | (180–480) | 360 | (180–480) | < 0.001b |
| Age (years), mean (standard deviation) | 74.4 | (5.3) | 74.3 | (5.2) | 73.9 | (5.6) | 72.8 | (5.5) | < 0.001b |
| Living alone, n (%) | 91 | (14.1) | 173 | (13.1) | 291 | (15.1) | 130 | (28.6) | < 0.001 |
| Years of residence in the neighborhood, n (%) | < 0.001 | ||||||||
| 1–29 | 98 | (15.2) | 191 | (14.5) | 411 | (21.4) | 153 | (33.6) | |
| 30–59 | 272 | (42.2) | 635 | (48.2) | 876 | (45.6) | 188 | (41.3) | |
| 60- | 270 | (41.9) | 476 | (36.1) | 621 | (32.3) | 108 | (23.7) | |
| Education, n (%) | 0.132 | ||||||||
| Junior high school graduation | 141 | (21.9) | 315 | (23.9) | 385 | (20.0) | 106 | (23.3) | |
| High school graduation | 199 | (30.9) | 412 | (31.3) | 615 | (32.0) | 136 | (29.9) | |
| Junior college/vocational college/college/graduate school graduation | 289 | (44.8) | 549 | (41.7) | 881 | (45.8) | 197 | (43.3) | |
| Other/missing | 16 | (2.5) | 41 | (3.1) | 42 | (2.2) | 16 | (3.5) | |
| Equivalent income, n (%) | < 0.001 | ||||||||
| < 2.0 million | 221 | (34.3) | 492 | (37.4) | 687 | (35.7) | 164 | (36.0) | |
| 2.0–3.99 million | 198 | (30.7) | 454 | (34.5) | 607 | (31.6) | 125 | (27.5) | |
| ≥ 4.0 million≥4.0 million | 152 | (23.6) | 222 | (16.9) | 384 | (20.0) | 84 | (18.5) | |
| Unknown/missing | 74 | (11.5) | 149 | (11.3) | 245 | (12.7) | 82 | (18.0) | |
| Alcohol drinking status, n (%) | 0.022 | ||||||||
| Current | 476 | (73.8) | 928 | (70.5) | 1397 | (72.7) | 298 | (65.5) | |
| Never or former | 165 | (25.6) | 377 | (28.6) | 515 | (26.8) | 150 | (33.0) | |
| Smoking status, n (%) | 0.101 | ||||||||
| Current | 102 | (15.8) | 260 | (19.7) | 374 | (19.5) | 107 | (23.5) | |
| Never or former | 536 | (83.1) | 1046 | (79.4) | 1533 | (79.7) | 344 | (75.6) | |
| Body mass index, kg/m2 | 0.012 | ||||||||
| < 18.5 | 27 | (4.2) | 56 | (4.3) | 92 | (4.8) | 29 | (6.4) | |
| 18.5–24.9 | 474 | (73.5) | 947 | (71.9) | 1363 | (70.9) | 293 | (64.4) | |
| ≥ 25 | 142 | (22.0) | 310 | (23.5) | 457 | (23.8) | 126 | (27.7) | |
| Number of chronic diseases, n (%)a | 0.027 | ||||||||
| 0 | 144 | (22.3) | 244 | (18.5) | 370 | (19.2) | 102 | (22.4) | |
| 1 | 202 | (31.3) | 416 | (31.6) | 561 | (29.2) | 126 | (27.7) | |
| 2+ | 248 | (38.5) | 556 | (42.2) | 869 | (45.2) | 185 | (40.7) | |
| Mobility limitation, n (%) | 129 | (20.0) | 301 | (22.9) | 501 | (26.1) | 145 | (31.9) | < 0.001 |
| Self-rated health, n (%) | < 0.001 | ||||||||
| Excellent to good | 503 | (78.0) | 1012 | (76.8) | 1447 | (75.3) | 304 | (66.8) | |
| Fair to poor | 103 | (16.0) | 214 | (16.3) | 379 | (19.7) | 123 | (27.0) | |
| Depressive mood, n (%) | 143 | (22.2) | 396 | (30.1) | 694 | (36.1) | 218 | (47.9) | < 0.001 |
| Employment, n (%) | 309 | (47.9) | 507 | (38.5) | 796 | (41.4) | 156 | (34.3) | < 0.001 |
| Social activity, n (%) | 345 | (53.5) | 519 | (39.4) | 653 | (34.0) | 95 | (20.9) | < 0.001 |
PA physical activity, NRs neighbor relationships, MVPA moderate-to-vigorous physical activity, VPA vigorous physical activity, MPA moderate physical activity, WT walking time, ST sitting time
aSum of the presence of hypertension, hyperlipidemia, cardiovascular disease, cerebrovascular disease, and diabetes mellitus
bP for trend test
Table 2.
PA variables and other characteristics of female participants, by category of individual-level NRs
| Variables | Category of NRs | P-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Visiting each other | Standing and chatting | Exchange of greetings | None | ||||||
| (n = 1268, 29.8%) | (n = 1895, 44.6%) | (n = 938, 22.1%) | (n = 151, 3.6%) | ||||||
| PA, median (interquartile range) | |||||||||
| MVPA, MET-hours/week | 29.7 | (13.2–62.7) | 26.4 | (11.9–57.8) | 23.1 | (8.3–55.8) | 11.6 | (0–34.7) | < 0.001b |
| VPA, min/week | 0 | (0–100) | 0 | (0–60) | 0 | (0–20) | 0 | (0–0) | < 0.001b |
| MPA, min/week | 0 | (0–120) | 0 | (0–120) | 0 | (0–105) | 0 | (0–0) | < 0.001b |
| WT, min/week | 300 | (160–630) | 350 | (150–630) | 280 | (120–630) | 180 | (0–420) | < 0.001b |
| ST, min/day | 300 | (180–480) | 300 | (180–480) | 300 | (180–480) | 420 | (240–600) | 0.027b |
| Age (years), mean (standard deviation) | 74.0 | (5.5) | 73.7 | (5.4) | 73.0 | (5.7) | 73.9 | (6.0) | < 0.001b |
| Living alone, n (%) | 339 | (26.7) | 409 | (21.6) | 222 | (23.7) | 60 | (39.7) | < 0.001 |
| Years of residence in the neighborhood, n (%) | < 0.001 | ||||||||
| 1–29 | 169 | (13.3) | 327 | (17.3) | 253 | (27.0) | 54 | (35.8) | |
| 30–59 | 822 | (64.8) | 1144 | (60.4) | 497 | (53.0) | 68 | (45.0) | |
| 60- | 268 | (21.1) | 414 | (21.9) | 182 | (19.4) | 28 | (18.5) | |
| Education, n (%) | 0.008 | ||||||||
| Junior high school graduation | 287 | (22.6) | 389 | (20.5) | 216 | (23.0) | 47 | (31.1) | |
| High school graduation | 569 | (44.9) | 851 | (44.9) | 386 | (41.2) | 63 | (41.7) | |
| Junior college/vocational college/college/graduate school graduation | 364 | (28.7) | 607 | (32.0) | 310 | (33.1) | 35 | (23.2) | |
| Other/missing | 48 | (3.8) | 48 | (2.5) | 26 | (2.8) | 6 | (4.0) | |
| Equivalent income, n (%) | 0.012 | ||||||||
| < 2.0 million | 481 | (37.9) | 652 | (34.4) | 325 | (34.7) | 62 | (41.1) | |
| 2.0–3.99 million | 338 | (26.7) | 545 | (28.8) | 241 | (25.7) | 30 | (19.9) | |
| ≥ 4.0 million | 206 | (16.3) | 288 | (15.2) | 145 | (15.5) | 17 | (11.3) | |
| Unknown/missing | 243 | (19.2) | 410 | (21.6) | 227 | (24.2) | 42 | (27.8) | |
| Alcohol drinking status, n (%) | 0.244 | ||||||||
| Current | 538 | (42.4) | 785 | (41.4) | 378 | (40.3) | 48 | (31.8) | |
| Never or former | 721 | (56.9) | 1098 | (57.9) | 551 | (58.7) | 101 | (66.9) | |
| Smoking status, n (%) | 0.213 | ||||||||
| Current | 64 | (5.1) | 117 | (6.2) | 71 | (7.6) | 6 | (4.0) | |
| Never or former | 1191 | (93.9) | 1757 | (92.7) | 856 | (91.3) | 142 | (94.0) | |
| Body mass index, kg/m2 | 0.056 | ||||||||
| < 18.5 | 117 | (9.2) | 236 | (12.5) | 124 | (13.2) | 17 | (11.3) | |
| 18.5–24.9 | 893 | (70.4) | 1310 | (69.1) | 652 | (69.5) | 102 | (67.6) | |
| ≥ 25 | 246 | (19.4) | 339 | (17.9) | 152 | (16.2) | 30 | (19.9) | |
| Number of chronic diseases, n (%)a | 0.038 | ||||||||
| 0 | 302 | (23.8) | 493 | (26.0) | 259 | (27.6) | 43 | (28.5) | |
| 1 | 393 | (31.0) | 583 | (30.8) | 289 | (30.8) | 41 | (27.2) | |
| 2+ | 457 | (36.0) | 686 | (36.2) | 301 | (32.1) | 48 | (31.8) | |
| Mobility limitation, n (%) | 391 | (30.8) | 552 | (29.1) | 313 | (33.4) | 66 | (43.7) | < 0.001 |
| Self-rated health, n (%) | < 0.001 | ||||||||
| Excellent to good | 1010 | (79.7) | 1492 | (78.7) | 710 | (75.7) | 95 | (62.9) | |
| Fair to poor | 186 | (14.7) | 316 | (16.7) | 182 | (19.4) | 46 | (30.5) | |
| Depressive mood, n (%) | 306 | (24.1) | 630 | (33.3) | 384 | (40.9) | 86 | (57.0) | < 0.001 |
| Employment, n (%) | 339 | (26.7) | 466 | (24.6) | 287 | (30.6) | 34 | (22.5) | < 0.001 |
| Social activity, n (%) | 667 | (52.6) | 904 | (47.7) | 364 | (38.8) | 26 | (17.2) | < 0.001 |
PA physical activity, NRs neighbor relationships, MVPA moderate-to-vigorous physical activity, VPA vigorous physical activity, MPA moderate physical activity, WT walking time, ST sitting time
aSum of the presence of hypertension, hyperlipidemia, cardiovascular disease, cerebrovascular disease, and diabetes mellitus
bP for trend test
Tables 3 and 4 show associations of individual- and community-level NRs with PA variables, as determined by multilevel regression analyses after adjusting for all covariates, in men (Table 3) and women (Table 4). Among men, individual-level NRs were consistently positively associated with MVPA and its components VPA, MPA, and WT, and the dose–response relationships were significant (all P < 0.041 for trend). Community-level NRs (by 1% estimation) were positively associated with male MVPA (2.1 MET-hours/week; 95% CI, 0.7–3.4), VPA (8.6 min/week; 2.7–14.4), and WT (11.6 min/week; 2.2–20.9). Significant cross-level interactions between individual- and community-level NRs were observed for male MVPA, VPA, and WT. The dose–response relationship was significant for MVPA (P = 0.025 for trend) and VPA (P = 0.037 for trend) but not for WT (P = 0.072 for trend).
Table 3.
Multilevel regression analyses of associations between individual- and community-level NRs and PA variables in men (n = 4340)
| Variables | MVPA, MET-hours/week | VPA, min/week | MPA, min/week | WT, min/week | ST, min/day | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | |
| Fixed effects | |||||||||||||||
| Individual-level NRs | |||||||||||||||
| Visiting each other | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||
| Standing and chatting | −4.4 | (−9.6, 0.8) | 0.098 | −22.4 | (−45.2, 0.5) | 0.055 | − 21.4 | (−47.2, 4.4) | 0.104 | 0.6 | (−36.0, 37.2) | 0.975 | 19.6 | (−3.5, 42.7) | 0.097 |
| Exchange of greetings | −6.0 | (−11.0, −1.0) | 0.018 | −20.0 | (−41.9, 1.9) | 0.074 | −25.0 | (−49.8, −0.3) | 0.047 | −30.3 | (−65.5, 4.8) | 0.091 | 16.8 | (−5.4, 39.1) | 0.138 |
| None | −11.8 | (−18.7, −4.9) | 0.001 | −36.9 | (−67.1, −6.7) | 0.017 | −46.7 | (−80.8, −12.7) | 0.007 | −68.0 | (−116.3, −19.6) | 0.006 | 15.8 | (−15.2, 46.7) | 0.318 |
| Trend | 0.001 | Trend | 0.041 | Trend | 0.012 | Trend | 0.001 | Trend | 0.355 | ||||||
| Community-level NRsaCommunity-level NRsa | |||||||||||||||
| 1% estimation | 2.1 | (0.7, 3.4) | 0.002 | 8.6 | (2.7, 14.4) | 0.004 | 4.2 | (−2.4, 10.8) | 0.216 | 11.6 | (2.2, 20.9) | 0.015 | −3.9 | (−9.9, 2.0) | 0.196 |
| Cross-level interaction term | |||||||||||||||
| Visiting each other × community-level NRs | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||
| Standing and chatting × community-level NRs | −1.5 | (−3.2, 0.1) | 0.073 | −6.6 | (−13.9, 0.6) | 0.073 | −0.6 | (−8.8, 7.6) | 0.887 | −10.7 | (−22.3, 0.9) | 0.071 | −0.9 | (−8.3, 6.5) | 0.810 |
| Exchange of greetings × community-level NRs | −1.6 | (−3.2, −0.1) | 0.046 | − 6.3 | (−13.2, 0.7) | 0.076 | −2.0 | (−9.8, 5.9) | 0.623 | −11.7 | (− 22.8, −0.6) | 0.039 | 1.4 | (−5.7, 8.5) | 0.696 |
| None × community-level NRs | −2.5 | (−4.6, −0.4) | 0.018 | −10.7 | (−19.9, −1.5) | 0.022 | −5.5 | (−15.8, 4.9) | 0.300 | −13.4 | (−28.1, 1.3) | 0.075 | 2.8 | (−6.5, 12.2) | 0.550 |
| Trend | 0.025 | Trend | 0.037 | Trend | 0.301 | Trend | 0.074 | Trend | 0.362 | ||||||
| Random effects | |||||||||||||||
| Community-level variance (standard error) | 0.00 | (0.00) | 10.23 | (46.35) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | |||||
| Intraclass correlation coefficient | 0.0000 | 0.0002 | 0.0000 | 0.0000 | 0.0000 | ||||||||||
PA physical activity, NRs neighbor relationships, MVPA moderate-to-vigorous physical activity, METs metabolic equivalent, VPA vigorous physical activity, MPA moderate physical activity, WT walking time, ST sedentary time, B partial regression coefficient, CI confidence interval
All models were adjusted by age, living situation, years of residence in the neighborhood, education, equivalent income, alcohol drinking status, smoking status, body mass index, number of choronic diseases, mobility limitation, self-rated health, depressive mood, employment status, and social activity
aThe proportions of people with active interaction (visiting each other and standing and chatting) in districts were calculated for community-level NRs
Table 4.
Multilevel regression analyses of associations between individual- and community-level NRs and PA variables in women (n = 4252)
| Variables | MVPA, MET-hours/week | VPA, min/week | MPA, min/week | WT, min/week | ST, min/day | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | |
| Fixed effects | |||||||||||||||
| Individual-level NRs | |||||||||||||||
| Visiting each other | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||
| Standing and chatting | −3.1 | (−6.8, 0.6) | 0.100 | −17.3 | (−32.6, −1.9) | 0.028 | −5.8 | (−23.8, 12.1) | 0.525 | −6.3 | (−36.9, 24.4) | 0.688 | 13.6 | (−3.9, 31.2) | 0.127 |
| Exchange of greetings | −5.1 | (−9.5, −0.6) | 0.026 | −17.6 | (−36.2, 1.0) | 0.064 | 1.6 | (−20.1, 23.4) | 0.883 | −55.7 | (−92.9, −18.6) | 0.003 | 3.5 | (−17.8, 24.7) | 0.748 |
| None | −18.8 | (−27.8, −9.8) | < 0.001 | −44.6 | (−82.0, −7.1) | 0.020 | −50.5 | (−94.4, −6.7) | 0.024 | −159.2 | (−233.3, −85.1) | < 0.001 | 39.2 | (−4.4, 82.8) | 0.078 |
| Trend | < 0.001 | Trend | 0.009 | Trend | 0.320 | Trend | < 0.001 | Trend | 0.252 | ||||||
| Community-level NRsaCommunity-level NRsa | |||||||||||||||
| 1% estimation | 0.2 | (−0.9, 1.3) | 0.767 | 0.2 | (−4.2, 4.6) | 0.930 | 0.7 | (−4.5, 5.8) | 0.800 | 0.6 | (−8.2, 9.5) | 0.539 | −2.1 | (−7.2, 2.9) | 0.403 |
| Cross-level interaction term | |||||||||||||||
| Visiting each other × community-level NRs | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||
| Standing and chatting × community-level NRs | −0.2 | (−1.6, 1.1) | 0.769 | −2.8 | (−8.5, 2.8) | 0.321 | −1.4 | (−8.0, 5.2) | 0.678 | 4.7 | (−6.5, 16.0) | 0.406 | 2.3 | (−4.1, 8.6) | 0.488 |
| Exchange of greetings × community-level NRs | −0.1 | (−1.7, 1.4) | 0.863 | 0.0 | (−6.5, 6.5) | 0.998 | 0.1 | (−7.6, 7.7) | 0.982 | −2.4 | (−15.5, 10.6) | 0.713 | 0.3 | (−7.1, 7.8) | 0.929 |
| None × community-level NRs | −1.4 | (−4.6, 1.9) | 0.406 | −4.9 | (−18.5, 8.7) | 0.484 | −1.1 | (−17.0, 14.8) | 0.894 | −13.3 | (−40.2, 13.6) | 0.333 | 2.6 | (−13.2, 18.5) | 0.747 |
| Trend | 0.657 | Trend | 0.734 | Trend | 0.986 | Trend | 0.527 | Trend | 0.823 | ||||||
| Random effects | |||||||||||||||
| Community-level variance (standard error) | 5.65 | (6.44) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | |||||
| Intraclass correlation coefficient | 0.0022 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | ||||||||||
PA physical activity, NRs neighbor relationships, MVPA moderate-to-vigorous physical activity, METs metabolic equivalent, VPA vigorous physical activity, MPA moderate physical activity, WT walking time, ST sedentary time, B partial regression coefficient, CI confidence interval
All models were adjusted by age, living situation, years of residence in the neighborhood, education, equivalent income, alcohol drinking status, smoking status, body mass index, number of choronic diseases, mobility limitation, self-rated health, depressive mood, employment status, and social activity
aThe proportions of people with active interaction (visiting each other and standing and chatting) in districts were calculated for community-level NRs
Among women, individual-level NRs were positively associated with MVPA and its components VPA and WT, and the dose–response relationships were significant, as was the case for men (all P < 0.009 for trends). However, the associations between community-level NRs and PA variables and cross-level interactions were not significant. Neither individual nor community-level NRs were significantly associated with ST in either sex.
The range of interclass correlation coefficients was 0.0000 to 0.0022 for PA variables in both sexes, which indicated that variances in PA variables, as explained by the random effects for districts, were extremely small (0.00–0.22%).
Discussion
The present sex-stratified multilevel analyses revealed three main findings. First, individual-level NRs were consistently positively associated with MVPA and its components VPA and WT in both sexes, and the dose–response relationships were significant. Second, in men, community-level NRs were positively associated with individual MVPA, VPA, and WT, regardless of the degree of individual-level NRs. Finally, significant cross-level interactions between individual- and community-level NRs were observed in PA variables for men.
An association of regular PA with mortality has been reported [23, 24]. The Japanese PA Reference for Health Promotion 2013 [25] recommends PA of 23 MET-hours/week or more at age 18–64 years and 10 MET-hours/week or more at age 65 years or older. Furthermore, the official Japanese PA guidelines for health promotion (the “ActiveGuide”) [26] suggest an additional 10 min of daily PA to increase healthy life expectancy for all generations. A large prospective cohort study [27] reported that 15 min per day or 90 min per week of moderate-intensity exercise resulted in a 14% lower risk of all-cause mortality and increased life expectancy by 3 years, even among individuals at risk for cardiovascular disease. Our findings showed a difference of approximately 6 MET-hours/week (equivalent to 90 min MPA per week) for men and 13 MET-hours/week (equivalent to 195 min MPA per week) for women between respondents who reported an NR status of none and those who reported exchange of greetings. In addition, male MVPA increased by 2.1 MET-hours/week (equivalent to 31.5 min MPA per week) for each 1% increase in community-level NRs. These findings suggest that, in men, activating NRs at the individual and community level contributes to meeting PA recommendations [25–27].
The mechanism by which individual-level NRs enhance MVPA can be explained by a model proposed by Berkman and Krishna [13]. According to this model, social networks are embedded in larger sociocultural contexts, including culture, socioeconomic factors, and politics. Their model also holds that such upstream forces influence network structure and the characteristics of network ties (i.e., NRs in this study). Next, these networks operate at the behavioral level by following primary pathways (i.e., downstream factors), namely, provision of social support, social influence, social engagement, person-to-person contact, access to resources and material goods, and negative social interactions (including conflict and abuse) [13]. Among these pathways, the provision of social support and social engagement may, as compared with other pathways, have a greater direct contribution to MVPA.
A noteworthy finding of this study was that the contextual effects of NRs on PA variables and cross-level interactions were observed only in men. The presence of significant cross-level interaction indicates that men with inactive NRs living in communities in which NRs were inactive had even lower levels of MVPA than did those living in communities in which NRs were active. As to why this was not observed in women, most older women may have already been embedded in more diverse, and larger, informal networks than were men, as was reported in previous studies [28, 29]. Indeed, while 74.4% of women had active NRs in this study, this was the case for only 45.2% of men. This may explain the sex differences in the contextual effects of NRs.
Our findings might also be attributable to the patriarchal values underlying Japanese society (e.g., Japan ranked 157th among 193 countries in female representation in the national parliament, as of 1 December 2017) [30]. The present study area had 217 neighborhood associations in 18 districts, and 68.5% of older adults were members of the 217 neighborhood associations in 2017 [31]. Characteristically, the leaders and executives of these neighborhood associations were almost always men. The neighborhood associations perform various voluntary regional activities in cooperation with the local administration and promote daily exchange of social support among residents. Interestingly, previous studies reported that Japanese men were more likely than women to benefit from interventions that increase social networks [32] and benefited more than women from bonding social capital (i.e., resources accessed within networks or groups in which the members share similar background characteristics, such as sex) [33]. Because the present community-level unit of analysis was the district, NRs from male leaders or executives in the neighborhood associations (i.e., social support between men) could have easily directly influenced the MVPA of male inhabitants.
Our study has several limitations. First, the self-administered questionnaire used for measurement may be subject to recall bias. Although the IPAQ-SF is recommended and widely used for easy assessment of PA, it tends to overestimate reported PA, as compared with objective devices [17]. Second, selection bias is a concern, as 3002 (approximately 25%) of the respondents were excluded because of missing IPAQ-SF items. Third, our findings were obtained by analyzing data from older adults living in a metropolitan area in Japan. Thus, differences between countries and regions (urban or rural) should be considered when extrapolating these data to other settings. Finally, the direction of causality cannot be inferred in a cross-sectional study. We plan to conduct follow-up surveys, to examine longitudinally the associations observed in this study.
Despite these limitations, this study is to our knowledge the first to report associations of NRs with MVPA and its domains among older adults. Moreover, our evidence is strengthened by the use of a multilevel modeling approach to simultaneously examine the compositional and contextual effects of NRs.
In conclusion, although the compositional effects of NRs on PA were observed in both sexes, contextual effects and their cross-level interactions were observed only in men. An approach promoting NRs at both the individual and community level may therefore be important, particularly for preventing physical inactivity among men.
Acknowledgments
We are very grateful to the residents and staff members of Ota City, as well as to our collaborators.
Funding
This study was supported by grants from Ota City, the Japan Health Promotion & Fitness Foundation, the Sugiura Memorial Foundation, and The Japan Foundation for Aging and Health and by JSPS KAKENHI Grant Number 16 K16615.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CIs
Confidence intervals
- IPAQ-SF
International Physical Activity Questionnaire-Short Form
- METs
Metabolic equivalents
- MPA
Moderate physical activity
- MVPA
Moderate-to-vigorous physical activity
- NRs
Neighbor relationships
- PA
Physical activity
- ST
Sitting time
- VPA
Vigorous physical activity
- WT
Walking time
Authors’ contributions
S. Seino conceptualized and designed this study, supervised all aspects of its implementation, performed the data analysis, and drafted the manuscript. As the corresponding author, S. Seino has full access to all aspects of the research and writing process and takes final responsibility for the paper. YT and IT assisted with data collection. AK, YF, and S. Shinkai helped plan the evaluation and supervised its implementation. AK, M. Nishi, YT, YY, HA, M. Narita, TI, YF, and S. Shinkai conducted a scientific review of this study. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study protocol was developed in accordance with the guidelines proposed in the Declaration of Helsinki and was approved by the Ethical Committee of the Tokyo Metropolitan Institute of Gerontology (approved June 1, 2016). All participants gave informed consent before their inclusion in the study.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Satoshi Seino, Phone: +81 (3) 3964-3241, Email: seino@tmig.or.jp.
Akihiko Kitamura, Email: kitamura@tmig.or.jp.
Mariko Nishi, Email: nishi@tmig.or.jp.
Yui Tomine, Email: tomine@tmig.or.jp.
Izumi Tanaka, Email: itanaka@tmig.or.jp.
Yu Taniguchi, Email: yu0717@tmig.or.jp.
Yuri Yokoyama, Email: yokoyama@tmig.or.jp.
Hidenori Amano, Email: amano@tmig.or.jp.
Miki Narita, Email: mwata@tmig.or.jp.
Tomoko Ikeuchi, Email: ikeuchi@tmig.or.jp.
Yoshinori Fujiwara, Email: fujiwayo@tmig.or.jp.
Shoji Shinkai, Email: sshinkai@tmig.or.jp.
References
- 1.World Health Organization. Global Recommendations on Physical Activity for Health. Geneva: World Health Organization; 2010. [PubMed]
- 2.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morey MC, Sloane R, Pieper CF, Peterson MJ, Pearson MP, Ekelund CC, et al. Effect of physical activity guidelines on physical function in older adults. J Am Geriatr Soc. 2008;56:1873–1878. doi: 10.1111/j.1532-5415.2008.01937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity--a systematic review of longitudinal studies. BMC Public Health. 2013;13:813. doi: 10.1186/1471-2458-13-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blondell SJ, Hammersley-Mather R, Veerman JL. Does physical activity prevent cognitive decline and dementia?: a systematic review and meta-analysis of longitudinal studies. BMC Public Health. 2014;14:510. doi: 10.1186/1471-2458-14-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 7.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 8.Ministry of Health, Labour and Welfare, Japan . A basic direction for comprehensive implementation of national health promotion. 2012. pp. 1–25. [Google Scholar]
- 9.Lindsay Smith G, Banting L, Eime R, O’Sullivan G, van Uffelen JGZ. The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act. 2017;14:56. doi: 10.1186/s12966-017-0509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 11.Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. 2010;51 Suppl:S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berkman LF, Krishna A. Social network epidemiology. In: Berkman LF, Kawachi I, Glymour MM, editors. Social epidemiology. New York: OXFORD; 2014. pp. 234–289. [Google Scholar]
- 14.Nakamura H, Nakamura M, Okada E, Ojima T, Kondo K. Association of food access and neighbor relationships with diet and underweight among community-dwelling older Japanese. J Epidemiol. 2017;27:546–551. doi: 10.1016/j.je.2016.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seino S, Kitamura A, Tomine Y, Tanaka I, Nishi M, Nonaka K, et al. A community-wide intervention trial for preventing and reducing frailty among older adults living in metropolitan areas: design and baseline survey for a study integrating participatory action research with cluster trial. J Epidemiol. in press. [DOI] [PMC free article] [PubMed]
- 16.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 17.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kamada M, Kitayuguchi J, Lee IM, Hamano T, Imamura F, Inoue S, et al. Relationship between physical activity and chronic musculoskeletal pain among community-dwelling Japanese adults. J Epidemiol. 2014;24:474–483. doi: 10.2188/jea.JE20140025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bennie JA, Chau JY, van der Ploeg HP, Stamatakis E, Do A, Bauman A. The prevalence and correlates of sitting in European adults - a comparison of 32 Eurobarometer-participating countries. Int J Behav Nutr Phys Act. 2013;10:107. doi: 10.1186/1479-5868-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.OECD. Terms of reference. OECD project on the distribution of household incomes (2017/18 collection). 2017. http://www.oecd.org/els/soc/IDD-ToR.pdf. Accessed 1 May 2018.
- 21.Kim MJ, Seino S, Kim MK, Yabushita N, Okura T, Okuno J, et al. Validation of lower extremity performance tests for determining the mobility limitation levels in community-dwelling older women. Aging Clin Exp Res. 2009;21:437–444. doi: 10.1007/BF03327443. [DOI] [PubMed] [Google Scholar]
- 22.Hoyl MT, Alessi CA, Harker JO, Josephson KR, Pietruszka FM, Koelfgen M, et al. Development and testing of a five-item version of the geriatric depression scale. J Am Geriatr Soc. 1999;47:873–878. doi: 10.1111/j.1532-5415.1999.tb03848.x. [DOI] [PubMed] [Google Scholar]
- 23.Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol. 2011;40:1382–1400. doi: 10.1093/ije/dyr112. [DOI] [PubMed] [Google Scholar]
- 24.Moore SC, Patel AV, Matthews CE, Berrington de Gonzalez A, Park Y, Katki HA, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9:e1001335. doi: 10.1371/journal.pmed.1001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Health, Labour and Welfare, Japan . Physical Activity Reference for Health Promotion 2013 (in Japanese) 2013. [Google Scholar]
- 26.Miyachi M, Tripette J, Kawakami R, Murakami H. “+10 min of Physical Activity per Day”: Japan is looking for efficient but feasible recommendations for its population. J Nutr Sci Vitaminol (Tokyo) 2015;61 Suppl:S7–S9. doi: 10.3177/jnsv.61.S7. [DOI] [PubMed] [Google Scholar]
- 27.Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378:1244–1253. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 28.Campbell KE, Lee BA. Sources of personal neighbor networks: social integration, need, or time? Soc Forces. 1992;70:1077–1100. doi: 10.1093/sf/70.4.1077. [DOI] [Google Scholar]
- 29.Moen P, Chermack K. Gender disparities in health: strategic selection, careers, and cycles of control. J Gerontol B Psychol Sci Soc Sci. 2005;60 Spec No 2:99–108. doi: 10.1093/geronb/60.Special_Issue_2.S99. [DOI] [PubMed] [Google Scholar]
- 30.Inter-Parliamentary Union . Women in national parliaments. 2017. [Google Scholar]
- 31.Ota City. Ota City implementation plan (2017–2019). 2017. http://www.city.ota.tokyo.jp/kuseijoho/ota_plan/ota-jissi-keikaku_sakutei/ota-jissi-keikaku_sakutei_h29/files/h29_01.pdf. Accessed 1 Feb 2018.
- 32.Harada K, Masumoto K, Katagiri K, Fukuzawa A, Chogahara M, Kondo N, et al. Community intervention to increase neighborhood social network among Japanese older adults. Geriatr Gerontol Int. 2018;18:462–469. doi: 10.1111/ggi.13208. [DOI] [PubMed] [Google Scholar]
- 33.Iwase T, Suzuki E, Fujiwara T, Takao S, Doi H, Kawachi I. Do bonding and bridging social capital have differential effects on self-rated health? A community based study in Japan. J Epidemiol Community Health. 2012;66:557–562. doi: 10.1136/jech.2010.115592. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


