Abstract
This chapter describes the various strategies filoviruses use to escape host immune responses with a focus on innate immune and cell death pathways. Since filovirus replication can be efficiently blocked by interferon (IFN), filoviruses have evolved mechanisms to counteract both type I IFN induction and IFN response signaling pathways. Intriguingly, marburg- and ebolaviruses use different strategies to inhibit IFN signaling. This chapter also summarizes what is known about the role of IFN-stimulated genes (ISGs) in filovirus infection. These fall into three categories: those that restrict filovirus replication, those whose activation is inhibited by filoviruses, and those that have no measurable effect on viral replication. In addition to innate immunity, mammalian cells have evolved strategies to counter viral infections, including the induction of cell death and stress response pathways, and we summarize our current knowledge of how filoviruses interact with these pathways. Finally, this chapter delves into the interaction of EBOV with myeloid dendritic cells and macrophages and the associated inflammatory response, which differs dramatically between these cell types when they are infected with EBOV. In summary, we highlight the multifaceted nature of the host-viral interactions during filoviral infections.
1 Introduction
The filovirus family includes three genera, Ebolavirus, Marburgvirus, and Cuevavirus. The genus Marburgvirus has two members (Marburg and Ravn viruses), and Lloviu virus is the only member of the genus Cuevavirus. Five ebolaviruses (Bundibugyo, Ebola, Reston, Sudan, and Taï Forest virus) have been assigned to the genus Ebolavirus (Fig. 1; see chapter Guide to the Correct Use of Filoviral Nomenclature in this book for a closer analysis of filovirus taxonomy). Although the members of the filovirus family differ in their virulence (Mahanty and Bray 2004), they take similar but not identical approaches to the circumvention or inhibition of host defense pathways.
Fig. 1.
The virus family Filoviridae includes three genera, Ebolavirus, Marburgvirus, and Cuevavirus. The genus Ebolavirus has five members: Ebola virus (EBOV), Sudan virus (SUDV), Bundibugyo virus (BDBV), Tai Forest virus (TAFV), and Reston virus (RESTV). The genus Marburgvirus has two members: Marburg virus (MARV) and Ravn virus (RAVV). The genus Cuevavirus has only one member, Lloviu virus (LLOV). Viruses in red are pathogenic to humans, those in green appear to be non-pathogenic to humans, and those in blue are not known to have been in contact with humans
Filoviruses encode at least four proteins that counteract host antiviral defense strategies: glycoprotein (GP), viral protein (VP) 24, VP35, and VP40. These proteins have additional roles in viral attachment, transcription, replication, or virion formation (see chapters Inside the Cell and Filovirus Structural Biology: The Molecules in the Machine in this book for in-depth descriptions of these latter functions).
Much work has been done to elucidate how filoviruses interact with the interferon (IFN) pathway, which is one of the best-studied antiviral host defense systems. Activation of the type I IFN signaling pathway leads to the expression of IFN-stimulated genes (ISGs), the mediators of IFN-induced inhibition to pathogens (Hoffmann et al. 2015). Pretreatment of cells with type I IFNs (IFNα and IFNβ) or type II IFN (IFNγ) efficiently blocks filovirus replication, indicating that at least some of the ISGs are potent inhibitors of filovirus replication (Pinto et al. 2015; Rhein et al. 2015). This chapter will highlight the molecular mechanisms that filoviruses use to inhibit IFN induction and signaling. It will also summarize what is known about the role of ISGs in filovirus infection, which falls into three categories: those that restrict filovirus replication, those that the virus blocks from restricting replication, and others that have no effect on viral replication.
The IFN system is not the only strategy used by cells to control viral infection. Various forms of cell death are used as a crude, last-ditch effort to limit viral replication; by destroying the host cell, virus replication is, at least temporarily, halted. While some viruses actively inhibit cell death signaling, other viruses have co-opted this host defense strategy to facilitate virus spread. Here, we will describe the role that cell death plays during filovirus infection.
Finally, this chapter will review how filovirus infection impacts the functions of macrophages and dendritic cells (DCs). These cells are key players in innate virus control and play central roles in linking innate and adaptive immunity. Importantly, they are also early target cells during filovirus infection.
2 Immune Evasion by Filovirus Proteins
2.1 Inhibition of IFN Induction
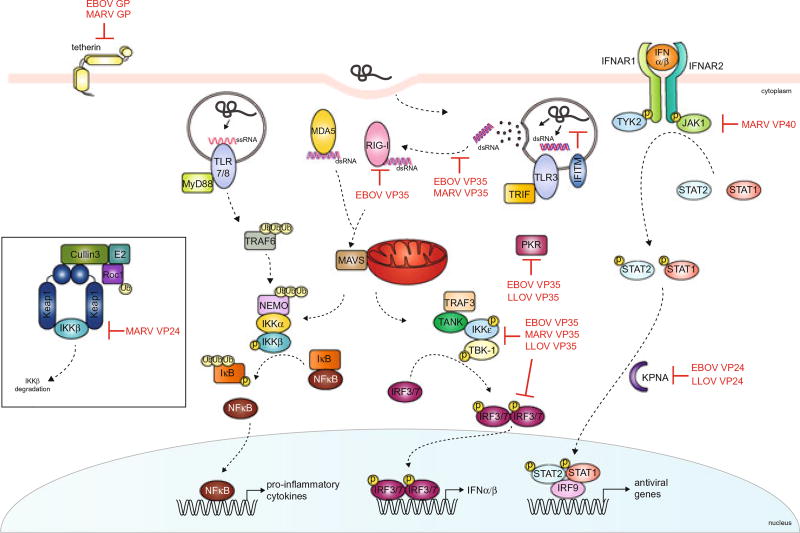
The innate immune system is an evolutionarily conserved branch of the host response that serves as the first line of defense against invading pathogens. Detection of viral infection is mediated by pattern recognition receptors (PRRs), which recognize pathogen associated molecular patterns (PAMPs) absent in the host. Two major types of PRRs are RIG-I-like receptors (RLRs) and Toll-like receptors (TLRs) (Akira et al. 2006; Gerlier 2011). RLRs, including retinoic acid inducible gene I (RIG-I) and melanoma associated differentiation factor 5 (MDA5), are cytoplasmic proteins containing N-terminal caspase activation and recruitment domains (CARDs), central DExD/H box helicase domains, and C-terminal RNA binding domains that recognize PAMPs from viral genomic material, including those generated due to viral replication within the host cells (Leung et al. 2012; Takeuchi and Akira 2008). RIG-I is activated by short double stranded RNA (dsRNA) with 5′-ppp or 5′-OH groups, whereas MDA5 preferentially binds to longer lengths of dsRNA (Leung et al. 2012; Takeuchi and Akira 2008; Schlee et al. 2009; Yoneyama et al. 2005; Schmidt et al. 2009; Li et al. 2009; Akira and Takeda 2004). Signaling through CARD-CARD interaction between RLRs and the mitochondrial activator of viral signaling (MAVS, also known as IPS-1, VISA, or Cardif) located on mitochondria (Sun et al. 2006; Berke and Modis 2012) (Fig. 2) results in the activation of TANK binding kinase (TBK1) and inhibitor of nuclear factor κ-B kinase subunit ε (IKKε) through association with TANK (TRAF family member-associated NF-κB activator) and TRAF3 (TNF receptor-associated factor 3). TBK1/IKKε kinases phosphorylate the transcription factors IFN regulatory factors 3 and 7 (IRF3 and IRF7), which homodimerize and translocate into the nucleus to activate the expression of type I IFNs (Akira et al. 2006).
Fig. 2.
Filoviruses inhibit the type I IFN response at multiple steps. This figure shows a simplified schematic of the type I IFN signal pathway. Viral PAMPs (e.g., dsRNA, endosomal ssRNA) are detected by host PRRs, such as RLRs (e.g., MDA5, RIG-I) and TLRs, which lead to the production of type I IFNs (IFNα/β) and pro-inflammatory cytokines. Binding of IFNα/β to the receptor complex IFNAR1/2 activates the JAK/STAT pathway leading to the expression of IFN-stimulated genes (ISGs). Filovirus proteins (in red) target different steps of these pathways
The filoviral VP35 proteins are multifunctional. In addition to their functions as viral polymerase cofactors (see chapters Inside the Cell and Filovirus Structural Biology: The Molecules in the Machine in this book for more information), they antagonize the antiviral response. Ebola virus (EBOV) and Marburg virus (MARV) VP35 proteins bind viral dsRNA to prevent their recognition by RIG-I and MDA5 (Prins et al. 2010a; Ramanan et al. 2012; Leung et al. 2009, 2010), representing some of the better studied systems of viral antagonism of IFN production through PAMP sequestration. Structural studies of the C-terminal IFN inhibitory domain (IID) of EBOV VP35 in complex with an 8-bp in vitro transcribed RNA show that a series of conserved basic residues facilitate binding of EBOV VP35 to the phosphodiester backbone of dsRNA (Fig. 2) (Leung et al. 2010). Mutational analysis of these residues, particularly Arg312, shows that these basic residues are important for dsRNA binding and IFN inhibition (Prins et al. 2010a). In fact, substitution of Lys319 and Arg322 with alanine residues renders a guinea pig-adapted EBOV avirulent (Prins et al. 2010a). EBOV VP35 also caps the blunt ends of dsRNA through hydrophobic residues Phe235 and Phe239 (Leung et al. 2010). This dual interaction provides a mechanism that allows EBOV VP35 to efficiently sequester dsRNA from detection by and activation of RIG-I and MDA5. Similarly, MARV VP35 coats the dsRNA backbone. Although MARV VP35 is structurally homologous to EBOV VP35, the backbones of their crystal structures have a root mean square deviation of less than 1.0 Ångstrom (Ramanan et al. 2012), MARV VP35 is unable to endcap dsRNA and preferentially binds longer dsRNA that are targeted by MDA5 (Berke and Modis 2012; Ramanan et al. 2012; Peisley et al. 2011; Edwards et al. 2016) (Fig. 2). These differences in MARV VP35 recognition of dsRNA motifs manifests in less-efficient inhibition of RIG-I signaling compared to EBOV VP35 (Edwards et al. 2016). EBOV VP35 also interacts with and sequesters individual components of stress granules, cytoplasmic structures which translationally silence RNAs in response to stress (Nelson et al. 2016; Le Sage et al. 2016). The correspondence between in vitro studies that evaluate RNA sequestration with in vivo studies of corresponding mutant viral infections support the relevance of these mechanisms (Prins et al. 2010a). The inhibition of type I IFN induction by VP35 appears to be a pan-filovirus characteristic, as it has been shown for the VP35 proteins of all five ebolaviruses, both marburgviruses, and Lloviu virus (LLOV) (Edwards et al. 2016; Feagins and Basler 2015; Guito et al. 2016). However, there are species-specific differences. Thus, marburgvirus VP35 proteins might be less efficient in counteracting IFN induction compared to their ebolavirus counterparts (Edwards et al. 2016; Guito et al. 2016).
2.1.1 Suppression of PACT Induced RIG-I Activation
RIG-I can be activated by the cellular protein kinase R (PKR) activator (PACT) (Kok et al. 2011; Iwamura et al. 2001; Luthra et al. 2013), although the exact molecular mechanism is poorly understood. Some viral proteins, such as EBOV and MARV VP35, target PACT to inhibit RIG-I signaling (Edwards et al. 2016; Luthra et al. 2013). PACT induces potent activation of RIG-I-dependent IFNβ promoter activity, which is correlated with an increase in RIG-I ATPase activity. Expression of the EBOV VP35 C-terminal domain suppresses RIG-I ATPase activity, as well as IFNβ promoter activity (Edwards et al. 2016; Luthra et al. 2013). Coimmunoprecipitation studies show that EBOV VP35 binds PACT and disrupts the interaction between PACT and RIG-I in a RNA-independent manner (Luthra et al. 2013). Moreover, EBOV VP35 residues critical for dsRNA binding, including Arg312, Arg322, and Phe239, are required for PACT binding. Interestingly, dsRNA binding does not appear to mediate the interaction between EBOV VP35 and PACT. Further studies are needed to elucidate upon the molecular mechanism of how PACT binding to VP35 regulates RIG-I activity, as well as the role of PACT binding to VP35 on viral polymerase activity as VP35 functions as a cofactor for the filoviral replication complex (Luthra et al. 2013; Prins et al. 2010b; Becker et al. 1998). The function of PACT in promoting translational inhibition through PKR activation requires additional studies to define the cellular role of its impact.
2.1.2 Inhibition of IRF3 and IRF7 Activation
In addition to facilitating RLR signaling, IRF3 and IRF7 are part of the signaling cascade for a number of other PRRs including TLRs and cytoplasmic DNA sensors [reviewed in (Hiscott 2007)]. Whether it is for the purpose of redundant inhibition of the above-mentioned RLR pathway or for the purpose of inhibiting other PRRs, EBOV VP35 also inhibits IRF3- and IRF7-mediated signaling, in part by binding to and inhibiting the function of the upstream kinases TBK1 and IKKε (reviewed in Basler and Amarasinghe 2009; Prins et al. 2009, Fig. 2). Similar to EBOV, MARV VP35 also inhibits IRF3 phosphorylation and IRF3 reporter gene activity, even in the presence of over-expressed TBK1 and IKKε (Ramanan et al. 2012). In a comparative analysis of ebola- and marburgvirus VP35 proteins, marburgvirus VP35 proteins were slightly less efficient at inhibiting IRF3 reporter gene activation than ebolavirus VP35 proteins (Guito et al. 2016). LLOV VP35 is also capable of inhibiting IRF3 activation (Feagins and Basler 2015).
2.2 Inhibition of IFN Signaling by Filoviral Proteins
Type I IFNs, including IFNα and IFNβ are master regulators of antiviral responses (Rawlings et al. 2004; O’Shea et al. 2015). IFNα is predominantly produced by hematopoietic cells, including plasmacytoid dendritic cells, while IFNβ is more broadly expressed (Ivashkiv and Donlin 2014; Chow and Gale 2015). Type I IFNs can act in an autocrine or paracrine fashion and bind to IFNα/β receptor (IFNAR) to activate Janus kinase 1 (JAK1) and tyrosine kinase 2 (TYK2), which phosphorylate Signal transducer and activator of transcription 1 (STAT1) and STAT2. Phosphorylated STAT1 is recognized by a subset of the karyopherin α (KPNA) family of nuclear transport proteins, the NPI-1 subfamily, which translocate STAT1-containing complexes to the nucleus (McBride et al. 2002; Sekimoto et al. 1997). The phosphorylated STAT1/STAT2 heterodimer forms a ternary complex along with IRF9 in the nucleus that induces transcription of ISGs through the IFN-stimulated gene response elements (ISREs). ISGs can inhibit different stages of viral infection including entry, replication, transcription, translation, assembly, and egress (Schneider et al. 2014; Sadler and Williams 2008). As a result of the actions of ISG expression, an overall antiviral state is achieved within the infected and neighboring cells. In addition to inhibition of IFN induction, filoviruses also encode proteins that inhibit the IFN signaling pathway. Below we describe how filoviral components have developed ways to inhibit JAK/STAT activity, interfere with the nuclear transport of transcription factors STAT1 and STAT2, as well as inhibit the activity of ISGs.
2.2.1 Inhibition of Phosphorylation of JAK/STAT Pathway Proteins
IFNα/β binding to IFNAR leads to the phosphorylation of JAK1 and TYK2. Although MARV and EBOV have a similar genome organization, only MARV VP40 inhibits JAK1-dependent signaling pathways (Valmas et al. 2010) (Fig. 2). Expression of MARV VP40 inhibits the tyrosine phosphorylation of JAK1, TYK2, STAT1, and STAT2 in response to IFNγ- and IL6-mediated phosphorylation of STAT1 and STAT3 (Guito et al. 2016; Valmas et al. 2010). This process is similar to a JAK1-deficient phenotype, suggesting that MARV VP40 targets JAK1, and not TYK2. Furthermore, MARV VP40 residues Ala57 and Ala165 appear to be important for inhibition of IFN signaling as mutation of these residues results in loss of JAK1 inhibition (Valmas et al. 2010).
Recent studies analyzing ebola- and marburgvirus proteins for their abilities to counteract the antiviral response suggest that the VP40 proteins of MARV, RAVV, and to a lesser extent TAFV and SUDV, inhibit IFN- and Sendai virus (SeV)-induced ISG production (Guito et al. 2016). Initial studies analyzing LLOV show that LLOV VP40 is unable to inhibit IFN signaling, similar to EBOV VP40 (Feagins and Basler 2015).
2.2.2 Inhibition of Nuclear Transport of STATs
In contrast to MARV VP40, which inhibits JAK1 phosphorylation, ebolavirus VP24 proteins block the nuclear translocation of phosphorylated STAT1 (pY-STAT1) complexes by targeting the STAT1 transporter KPNA (Guito et al. 2016; Reid et al. 2006, 2007; Xu et al. 2014). Recent biochemical and structural studies have elucidated how EBOV VP24 affects STAT1 nuclear accumulation while maintaining other KPNA-mediated cargo delivery (Xu et al. 2014). All KPNA recognize cargo containing a classical nuclear localization signal (CNLS) through a major site on armadillo repeats (ARM) 2–4 and a minor site on ARM 6–8 (Conti et al. 1998; Conti and Kuriyan 2000; Chook and Blobel 2001; Conti and Izaurralde 2001). However, pY-STAT1 is transported by the nucleoprotein-interacting protein 1 (NPI-1) subfamily, including KPNA1, KPNA5, and KPNA6, which can recognize a relatively uncharacterized nonclassical NLS (ncNLS) (Sekimoto et al. 1997). EBOV VP24 binds to KPNA with a significantly higher affinity than pY-STAT1, suggesting that EBOV VP24 competes with pY-STAT1 for binding to KPNA (Xu et al. 2014). The crystal structure of EBOV VP24 in complex with the minimal binding region of KPNA5 has a large surface area of interaction with a hydrophobic core and high shape complementarity (Xu et al. 2014). The binding surface is formed by residues in KPNA that are conserved only among the NPI-1 subfamily and residues of EBOV VP24 that vary in the closely related MARV VP24 (Xu et al. 2014). Use of the ncNLS allows STAT1 transport to occur independently of other nucleocytoplasmic trafficking of cargoes containing cNLSs. This may be important in EBOV pathogenesis by maintaining certain cellular functions that can facilitate viral replication.
VP24 from all ebolaviruses, but not MARV VP24, inhibit IFN signaling, although BDBV and RESTV VP24 are less efficient at inhibition. This may in part be due to decreased KPNA binding (Guito et al. 2016; Schwarz 2016). LLOV VP24 inhibits the IFN pathway in a manner similar to EBOV VP24 by inhibiting IFN-induced STAT1 nuclear translocation and ISG induction presumably due to its ability to bind KPNA (Feagins and Basler 2015).
2.3 ISGs in Filovirus Infection
As mentioned above, pretreatment of cells with IFNα/β or IFNγ drastically reduces filovirus infectivity, suggesting an inhibitory role for ISGs (Pinto et al. 2015; Rhein et al. 2015; Bjorndal et al. 2003). Some well-studied ISGs include the antiviral proteins myxovirus resistance 1 (Mx1), IFN-inducible dsRNA-dependent protein kinase R (PKR), 2′-5′-oligoadenylate synthetase (OAS), IFN-induced proteins with tetratricopeptide repeats (IFITs), apolipoprotein B mRNA-editing enzyme catalytic polypeptide (APOBEC1), tripartite motif-containing proteins (TRIM) molecules, and tetherin (Schneider et al. 2014; Sadler and Williams 2008; Yan and Chen 2012; Haller et al. 2015; Garcia et al. 2006; Rebouillat and Hovanessian 1999; Diamond and Farzan 2013; Vladimer et al. 2014; Ozato et al. 2008; Kuhl et al. 2011). Here we review the literature regarding the ability of ISGs to restrict filovirus infection.
2.3.1 PKR
Protein kinase R (PKR) is a PRR that uses an N-terminal dsRNA binding domain to sense viral infection [reviewed in (Garcia et al. 2007)]. Kinase activity of PKR is activated upon dsRNA binding, leading to the phosphorylation of targets, including eukaryotic translation initiation factor 2α (eIF2α), which results in the shutdown of translation and viral protein synthesis (Garcia et al. 2007; Nanduri et al. 1998; Dauber and Wolff 2009). In addition to inhibiting the previously mentioned dsRNA-sensing proteins RIG-I and MDA5, EBOV VP35 can prevent dsRNA-dependent PKR activation (Feng et al. 2007; Schümann et al. 2009). Three residues within the C-terminus of EBOV VP35, R305, K309, and R312, are critical for inhibition of PKR as mutation of all three of these amino acids to alanine greatly reduces the ability of VP35 to inhibit PKR activation (Schümann et al. 2009). Intriguingly, inhibition of PKR activation by EBOV VP35 does not appear to be dependent upon the ability to bind dsRNA, since the R312A mutant of VP35, which lacks dsRNA binding ability, can still prevent PKR activation (Schümann et al. 2009). More recently, LLOV VP35 was shown to inhibit SeV-induced PKR activation, indicating that inhibition of PKR activation by VP35 may be a pan-filovirus function (Feagins and Basler 2015).
2.3.2 PML Protein
Promyelocytic leukemia (PML) protein is a component of antiviral ISG forming nuclear bodies, often referred to as PML nuclear bodies (PML-NB) or Nuclear Domain 10 (ND10), which aggregate the replication and transcriptional machinery of many viruses (Everett and Chelbi-Alix 2007; Geoffroy and Chelbi-Alix 2011). While present in non-activated cells, PML expression is greatly enhanced upon stimulation of cells with type I or type II IFNs (Regad and Chelbi-Alix 2001; Chelbi-Alix et al. 1995; Lavau et al. 1995). The antiviral capacity of PML applies to certain RNA viruses as PML overexpression results in the restriction of both vesicular stomatitis Indiana virus and influenza A virus, but not encephalomyocarditis virus (Chelbi-Alix et al. 1998; Jin et al. 2014).
As of today, there is only one study looking at the role of PML in filovirus infection. PML expression is upregulated in EBOV-infected IFN-competent MCF7 cells (human breast cancer cell line), whereas only a minor change of PML expression occurs in infected Vero cells (african green monkey kidney epithelial cell line), which cannot produce IFN. Interestingly, PML expression does not change in surrounding, noninfected cells, indicating an IFN-independent mechanism of increased PML expression directly induced by EBOV infection (Bjorndal et al. 2003). Viral replication occurs readily in PML-expressing cells, suggesting that PML has no major inhibitory effect on EBOV replication, which was not analyzed in this study (Bjorndal et al. 2003).
2.3.3 IFIT Proteins
The IFN-induced protein with tetratricopeptide repeats (IFIT) family of proteins contains five members in humans, IFIT1, 1B, 1C, 2, 3, and 5. With the exception of IFIT1B, the expression of IFIT proteins are strongly induced by IFN and possess antiviral activity against specific RNA viruses (Pinto et al. 2015; Vladimer et al. 2014; Fensterl and Sen 2015; Hyde and Diamond 2015; Fensterl and Sen 2011; Young et al. 2016). There are two antiviral mechanisms that have been attributed to members of the IFIT family. IFIT1 binds to and inhibits the translation of viral mRNAs lacking 2′-O cap methylation. It also sequesters RNA of uncapped viral genomes and antigenomes containing 5′ triphosphates and prevents their translation with the help of IFIT2 and IFIT3 (Vladimer et al. 2014; Hyde and Diamond 2015; Pichlmair et al. 2011; Kumar et al. 2014; Daffis et al. 2010). The antiviral activity of IFIT1 is lacking or is minimal against wild-type flaviviruses but is greater against mutant forms of these viruses lacking 2′-O methyltransferases (2′OMTases) (Daffis et al. 2010; Szretter et al. 2012; Li et al. 2013; Kimura et al. 2013). These data indicate that the antiviral activity of IFIT1 against some viruses is overcome by viral 2′OMTase activity. The EBOV polymerase is predicted to have 2′OMTase activity (Zhao et al. 2016; Bujnicki and Rychlewski 2002; Ferron et al. 2002). Consistent with this prediction, EBOV replication does not seem to be affected by IFIT1. EBOV titers are similar in mouse macrophages lacking IFIT1 compared to wild-type (wt) cells (Pinto et al. 2015). Whether other IFITs have an antiviral function against EBOV or whether MARV is influenced by the IFIT family has not yet been reported.
2.3.4 IFITM Proteins
The IFN-induced transmembrane (IFITM) family includes IFITM1, 2, 3, and 5 in humans. A broad range of enveloped RNA viruses are restricted by at least one member of the IFITM family. IFITM proteins act at late stages of viral entry and restrict fusion from late endosomes (Huang et al. 2011; Alber and Staeheli 1996; Brass et al. 2009; Mudhasani et al. 2013; Lu et al. 2011; Everitt et al. 2013; Anafu et al. 2013; Bailey et al. 2014). The various members of the IFITM protein family are able to inhibit filoviral GP-mediated entry, as shown for retroviruses (murine leukemia virus) pseudotyped with distinct filoviral GPs, including those of all ebolavirus species, MARV, and LLOV to varying degrees (Huang et al. 2011; Wrensch et al. 2015) (Fig. 2). Importantly, the IFITM proteins also inhibit infection with EBOV and MARV (Huang et al. 2011). The inhibition of filovirus GP-mediated entry likely occurs in the late endosome (Huang et al. 2011). The exact mechanism remains unclear, but it appears that modulation of cathepsin activity is not involved (Huang et al. 2011).
2.3.5 Tetherin
Tetherin is a cell surface-localized transmembrane protein which acts as an antiviral ISG by inhibiting the budding of various viruses (Sakuma et al. 2009; Neil et al. 2008). Budding of filoviral particles is mediated by the matrix protein VP40, and tetherin blocks the release of virus-like particles (VLPs) from cells expressing EBOV, MARV, or RAVV VP40 (Sakuma et al. 2009; Kaletsky et al. 2009; Radoshitzky et al. 2010; Feagins and Basler 2014). However, tetherin-mediated restriction of VLP release can be overcome by co-expression of GP (Fig. 2). While the mechanism of the antagonizing function of GP has not been determined, EBOV GP and tetherin interact directly, suggesting a direct mechanism of action (Kaletsky et al. 2009; Lopez et al. 2010). While the mucin-like domain of EBOV GP was initially hypothesized to play a role in overcoming tetherin-mediated restriction, it does not seem to play a critical role in this process (Kaletsky et al. 2009; Radoshitzky et al. 2010). Interestingly, mutations in the VP40 gene in mouse-adapted RAVV increase the sensitivity of the virus to restriction by human, but not mouse, tetherin (Feagins and Basler 2014).
2.3.6 ISG15
ISG15 is a small, ubiquitin-like protein whose main antiviral function appears to be ISGylation, the covalent attachment to cellular and viral proteins in a manner similar to ubiquitinyl or SUMOyl conjugation. While the targets and functions of ISGylation remain relatively poorly characterized, ISG15 is generally characterized as harboring antiviral activity (Zhang and Zhang 2011). Similar to tetherin, ISG15 inhibits budding of VLPs containing EBOV VP40. Overexpression of a dominant-negative form of the ubiquitin ligase Nedd4 abolishes this inhibition, indicating a role for Nedd4 in ISG15-mediated restriction of EBOV (Malakhova and Zhang 2008; Okumura et al. 2008). Inhibition of VLPs containing EBOV VP40 is observed in the absence of other viral proteins. It is not known if ISG15 is able to inhibit budding of other filoviruses besides EBOV.
2.3.7 ZAP
Zinc finger antiviral protein (ZAP) is a zinc finger-containing ISG which has antiviral activity against a number of RNA viruses, although its antiviral activity is not universal (Gao et al. 2002; Bick et al. 2003). While the exact mechanism of ZAP antiviral function remains to be determined, initial studies show that ZAP post-transcriptionally reduces viral RNAs in a zinc finger-dependent manner (Mao et al. 2013). Additional studies indicate that ZAP binds to and destabilizes target viral RNAs by facilitating the removal of the mRNA caps and poly A tails as well as recruiting the 3′–5′ exosome to facilitate transcript degradation of RNAs (Guo et al. 2007; Zhu et al. 2011). EBOV and SUDV and, to a lesser extent MARV, replicate to lower titers in Rat2 and 293T cells expressing rat ZAP (Muller et al. 2007). Expression of ZAP leads to a reduction in the mRNA amounts of mainly EBOV and MARV L mRNAs, suggesting that ZAP interferes with L mRNA synthesis or stability (Muller et al. 2007).
2.4 Inhibition of RNA Interference Pathways
The related miRNA and RNAi pathways serve as cellular antiviral defense systems aside from their roles in normal cellular functions (Umbach and Cullen 2009; Haasnoot and Berkhout 2011; Vasselon et al. 2013). Three EBOV proteins, VP30, VP35, and VP40, each inhibit RNA interference (RNAi) in co-transfection experiments (Haasnoot et al. 2007; Fabozzi et al. 2011). EBOV VP35, the most effective of these EBOV proteins at inhibiting the RNAi pathway, does so in a dsRNA binding-dependent manner (Haasnoot et al. 2007). Inhibition the RNAi pathway by VP30 and VP35 may in part be due to their ability to interact with individual components of the RNAi pathway; VP30 interacts with Dicer and TRBP, while VP35 interacts with Dicer, TRBP, and PACT, independent of its dsRNA binding domain (Fabozzi et al. 2011). The VP35 proteins from both EBOV and MARV are able to inhibit Dicer-dependent production of virus-derived siRNAs (vsiRNAs) during infection of cells with influenza A virus lacking NS1, suggesting that VP35 may perform the same function during filovirus infections (Li et al. 2016). Interestingly, a lipid nanoparticle-delivered siRNA cocktail targeting VP35 and L is efficacious in rhesus monkeys up to 3 days post exposure to an otherwise lethal EBOV dose (Thi et al. 2015).
3 Cell Death in Filovirus Infection
Viruses rely on a functional cellular machinery to replicate. Cell death is an efficient way to disable this cellular machinery and therefore, is considered as an antiviral strategy. Some forms of cell death trigger a pro-inflammatory response, leading to additional cell damage (Labbe and Saleh 2008). Cell death caused by filovirus infection occurs in both animal (in vivo) and cell culture (in vitro) models.
3.1 Filovirus-Induced Cell Death in Animal Models and Patients
3.1.1 Cell Death of Permissive Cells in Vivo
Both in vivo and in vitro infection models suggest that filovirus-infected cells undergo non-apoptotic cell death, including necrosis (Baskerville et al. 1978; Connolly et al. 1999; Geisbert et al. 2000, 2003a; Ryabchikova et al. 1996a, 1999; Ryabchikova 2004; Murphy et al. 1971; Warfield et al. 2007; Groseth et al. 2012; Warfield et al. 2009; Qiu et al. 2014; Bird et al. 2016; Cross et al. 2015; Herbert et al. 2015; Ludtke et al. 2015; Zumbrun et al. 2012; Ebihara et al. 2013; Lever et al. 2012; Warren et al. 2010; Gibb et al. 2001; Bray et al. 2001; Olejnik et al. 2011; Schmidt et al. 2011). Although expression of apoptotic markers increases during EBOV infection in humans and in animal models (Geisbert et al. 2003a; Baize et al. 1999; Hensley et al. 2002; Leroy et al. 2001; Rubins et al. 2007), apoptosis is not observed in infected cells directly (Baskerville et al. 1978; Connolly et al. 1999; Geisbert et al. 2000, 2003a; Ryabchikova et al. 1996b, 1999; Ryabchikova 2004; Murphy et al. 1971; Gibb et al. 2001; Olejnik et al. 2011, 2013). A hallmark of filovirus infection is liver damage, which is associated with tissue necrosis and hepatocyte death (Baskerville et al. 1978; Ryabchikova et al. 1999; Ryabchikova 2004; Murphy et al. 1971; Warfield et al. 2007; Groseth et al. 2012; Warfield et al. 2009; Qiu et al. 2014; Bird et al. 2016; Cross et al. 2015; Herbert et al. 2015; Zumbrun et al. 2012; Ebihara et al. 2013; Lever et al. 2012; Ryabchikova et al. 1996b; Ellis et al. 1978; Zaki et al. 1999; Gedigk et al. 1968; Rippey et al. 1984). Hepatocytes and Kupffer cells in various rodent models of EBOV disease undergo apoptosis (Groseth et al. 2012; Ebihara et al. 2013; Bradfute et al. 2010). However, it is not clear whether apoptosis is induced in infected cells or in noninfected bystander cells or in both (Groseth et al. 2012; Ebihara et al. 2013; Bradfute et al. 2010). Inhibition of apoptosis delays liver dysfunction in mice, suggesting that the extent of hepatic cell death plays a crucial role in EBOV pathogenesis (Groseth et al. 2012; Ebihara et al. 2013; Bradfute et al. 2010).
3.1.2 Cell Death of Non-Permissive Cells in Vivo
Although lymphocytes are not permissive to filovirus infection, they are depleted in infected patients and in infected animals, presumably through apoptotic cell death (Geisbert et al. 2000, 2003a; Warfield et al. 2007, 2009; Cross et al. 2015; Ebihara et al. 2013; Baize et al. 1999, 2002; Leroy et al. 2000; Bradfute et al. 2007, 2008, 2010; Gupta et al. 2007; Reed et al. 2004; Brannan et al. 2015). Apoptotic lymphocytes are detected by various methods, including histology staining, electron microscopy, TUNEL assay, and flow cytometry in the tissues or peripheral blood mononuclear cells (PBMCs) of filovirus-infected animals (Geisbert et al. 2000, 2003a; Warfield et al. 2007, 2009; Cross et al. 2015; Ebihara et al. 2013; Bradfute et al. 2008, 2010; Reed et al. 2004; Brannan et al. 2015). Various apoptotic markers, including cleavage of the 41/7 nuclear matrix protein (NMP), DNA fragmentation, and increased Fas/CD95 expression are detected in lymphocytes from fatally EBOV-infected patients and macaques (Baize et al. 1999; Reed et al. 2004; Wauquier et al. 2010). In a mouse model of EBOV infection, lymphocyte apoptosis was shown to be dependent on both death receptor and intrinsic apoptosis signaling (Bradfute et al. 2010). Surprisingly, blocking lymphocyte apoptosis in an EBOV mouse model does not increase survival (Bradfute et al. 2010). A recent study analyzing the immune signature in patients infected with EBOV did not observe significant differences in the number of circulating white blood cells between fatal cases and survivors of infection. However, fatal cases showed a high percentage of CD4+ and CD8+ T cells expressing CTLA-4 and PD-1, both markers of T cell exhaustion (Ruibal et al. 2016). An increase in the number of white blood cells followed by only moderate lymphopenia was observed in nonhuman primates (NHPs) fatally infected with EBOV (Marzi et al. 2015). Initial increases in white blood cell numbers are also observed in survivors of EBOV infection (Kreuels et al. 2014; Wolf et al. 2015), suggesting that temporal changes in the T cell compartment might play a role in EBOV pathogenesis.
3.2 In Vitro Analysis of Filovirus-Induced Cell Death
In cell culture models, filovirus infection generally leads to a visible cytopathic effect (CPE) including cell blebbing, cell rounding, vacuolization, and detachment (Schmidt et al. 2011; Olejnik et al. 2013; Alazard-Dany et al. 2006; Barrientos and Rollin 2007; Hoenen et al. 2013; Geisbert et al. 2003b; Boehmann et al. 2005; Gupta et al. 2010). The degree of CPE caused by infection varies with different ebolaviruses (Boehmann et al. 2005). EBOV-infected cells, including human monocyte-derived macrophages, undergo necrotic cell death rather than apoptosis (Olejnik et al. 2013). There are conflicting results about the fate of EBOV-infected monocytes and macrophages in a human PBMC infection model. Although no signs of apoptosis were detected in EBOV-infected macrophages during PBMC infection in one study (Geisbert et al. 2000), apoptotic markers were found on monocytes and macrophages in EBOV- and BDBV-infected PBMCs by another group (Gupta et al. 2007, 2010). Whether differences in the experimental protocol account for the conflicting results remains to be determined.
EBOV-infected cells remain sensitive to the induction of apoptosis through both the intrinsic and extrinsic pathways (Olejnik et al. 2013). Interestingly, stimulation of dsRNA-dependent apoptosis in EBOV-infected cells inhibits EBOV replication (Olejnik et al. 2013). These data indicate that apoptotic pathways can be successfully induced to inhibit EBOV propagation. Intriguingly and in contrast to EBOV, MARV infection leads to the activation of cytoprotective responses in infected cells to prolong cell viability (as discussed below) (Page et al. 2014; Edwards and Basler 2015; Zhang et al. 2014; Johnson et al. 2016).
3.2.1 Filovirus Cytotoxic Proteins
Signs of cytotoxicity, including cell rounding and detachment have been associated with EBOV GP and VP40 (Alazard-Dany et al. 2006; Takada et al. 2000; Yang et al. 2000; Chan et al. 2000; Volchkov et al. 2001; Simmons et al. 2002; Ray et al. 2004; Sullivan et al. 2005; Han et al. 2007; Francica et al. 2009; Hacke et al. 2015; Melito et al. 2008). The mechanism of cell death in VP40-expressing cells remains undetermined but seems to be related to transient overexpression of the protein (Alazard-Dany et al. 2006; Melito et al. 2008). Since VP40 mediates budding (Hartlieb and Weissenhorn 2006), it is conceivable that the observed cytopathic effects are caused by massive membrane loss.
The mechanisms of GP-induced cytotoxicity are not entirely understood. Reduced activation of the ERK2 kinase and reduced integrin cell surface levels might play a role (Sullivan et al. 2005; Francica et al. 2009; Zampieri et al. 2007). While some studies report the induction of cell death in GP-expressing cells (Yang et al. 2000; Ray et al. 2004; Zampieri et al. 2007), other reports did not observe cell disruption (Chan et al. 2000; Simmons et al. 2002). A possible explanation for these conflicting results might be differences in the expression levels of GP in the various studies. Notably, low levels of EBOV GP expression comparable to GP levels in EBOV-infected cells do not lead to the induction of cytotoxic effects (Alazard-Dany et al. 2006). GP is processed from a precursor protein (preGP) into two subunits, GP1 and GP2, which both have cytotoxic effects (Yang et al. 2000; Han et al. 2007; Francica et al. 2009; Hacke et al. 2015; Zampieri et al. 2007). For GP1, the heavily glycosylated mucin-like domain is sufficient to mediate these effects (Yang et al. 2000; Francica et al. 2009; Zampieri et al. 2007). Increased expression of membrane-bound GP from a recombinant EBOV resulted in elevated cytotoxicity (Volchkov et al. 2001). Interestingly, this recombinant virus was less virulent in a guinea pig model, suggesting that early cell death of infected cells limits viral spread (Volchkova et al. 2015). A decrease in tumor necrosis factor α–converting enzyme (TACE)-mediated shedding of GP leads to increased cytotoxic effects and enhanced viral growth and infectivity (Dolnik et al. 2004, 2015). This suggests that GP-mediated cytotoxicity in EBOV infection is controlled by regulating both the levels of expression and shedding of GP. Intriguingly, no cytotoxic effects have been associated with overexpression of MARV GP (Chan et al. 2000). Cell surface expression of EBOV, MARV, or LLOV GP interferes with Fas/CD95 binding by steric shielding, thereby preventing the subsequent induction of apoptosis (Noyori et al. 2013). Whether this effect plays a role in the prevention of apoptosis in infected cells has yet to be determined.
3.2.2 Regulation of the Oxidative Stress Response by MARV VP24
MARV activates expression of genes with promoters that contain antioxidant response elements (AREs). ARE genes encode proteins that facilitate cellular survival under conditions of stress, including oxidative stress. MARV VP24 interacts with KELCH-like ECH-associated protein 1 (Keap1) (Page et al. 2014; Edwards and Basler 2015; Pichlmair et al. 2012). Keap1 interacts with proteins such as the transcription factor nuclear factor (erythroid-derived 2)-like 2 (Nrf2), and directs their Cul3 ubiquitin ligase-dependent poly-ubiquitinylation, thereby activating expression of ARE-containing genes. However, cell stresses trigger alteration in Keap1–Nrf2 interaction, leading to Nrf2 stabilization and activation of ARE gene expression (Copple et al. 2008). MARV VP24 interacts with Keap1 via one of the C-terminal six-bladed beta propeller Kelch domains. Interaction occurs through a loop (K-loop), which projects out from the MARV VP24 structure, and contains a GE amino acid motif that is preceded by acidic residues. This domain is similar to interaction motifs found in other Keap1 targets, including Nrf2. Biophysical studies indicate that MARV VP24 and Nrf2 interact with the same region of the KELCH domain (Edwards and Basler 2015; Zhang et al. 2014; Johnson et al. 2016). MARV VP24 binding to Keap1 disrupts Keap1-Nrf2 binding leading to ARE gene expression (Page et al. 2014; Edwards and Basler 2015). ARE gene expression is upregulated after MARV infection, but not after EBOV infection, which is consistent with the observation that MARV VP24 interacts with Keap1 but EBOV VP24 does not (Edwards and Basler 2015). Further, Nrf2-deficient mice are resistant to disease caused by mouse-adapted MARV (Page et al. 2014). These data suggest that MARV VP24 activates Nrf2 to facilitate viral replication, perhaps by activating the cytoprotective ARE response; infected cells survive longer and produce more virus. Alternatively, the ARE response may protect viral products from oxidative damage to facilitate replication. Keap1 also modulates stability of the kinase IKKβ, which regulates NF-κB expression, and MARV VP24 relieves the suppressive activity of Keap1 on NF-κB activation. As NF-κB can also exert cytoprotective effects, MARV VP24–Keap1 interaction may represent a general strategy of the virus to sustain the viability of infected cells (Edwards and Basler 2015).
4 Interaction of Filoviruses with Host Immune Cells
Antigen-presenting cells, including monocytes, macrophages, and myeloid dendritic cells, are considered the primary target cells of filoviruses and play crucial roles in filovirus pathogenesis (Bray and Geisbert 2005; Martinez et al. 2012). Infection of these cells by filoviruses severely impacts their function in mediating an appropriate innate immune response and might play a role in the excessive pro-inflammatory response observed during filovirus disease (Geisbert et al. 2003a, c; Hensley et al. 2002; Leroy et al. 2001; Rubins et al. 2007; Baize et al. 2002; Wauquier et al. 2010; Ruibal et al. 2016; Rougeron et al. 2015; Feldmann and Geisbert 2011; Villinger et al. 1999; McElroy et al. 2016; Gupta et al. 2001; McElroy et al. 2014a, b; Sanchez et al. 2004; Hutchinson and Rollin 2007; Ignatiev et al. 2000; Ebihara et al. 2011; Marzi et al. 2013; Martins et al. 2015; van Paassen et al. 2012; Fritz et al. 2008; Hensley et al. 2011; Alves et al. 2010; Geisbert et al. 2007; Lin et al. 2015; Connor et al. 2015; Fernando et al. 2015; Ignat’ev et al. 1995; Caballero et al. 2014, 2016; Marzi et al. 2016). In addition, comparative data on the cytokine and chemokine responses in EBOV-infected patients and nonhuman primates suggest that a broadly dysregulated inflammatory response is associated with severe or fatal EBOV disease (Baize et al. 1999, 2002; McElroy et al. 2014a; Martins et al. 2015).
4.1 Monocytes and Macrophages
Substantial data from studies of human infections and experimental animal infections demonstrate the replication of filoviruses in macrophage infection in vivo [reviewed in (Martinez et al. 2012)]. Macrophages are among the earliest cell types infected and remain targets of infection throughout the course of disease (Geisbert et al. 2003a). Human monocyte-derived macrophages are permissive for filovirus infection in vitro (Feldmann et al. 1996; Stroher et al. 2001; Martinez et al. 2013). Monocytes obtained from human blood also appear to be permissive for filovirus infection in vitro (Stroher et al. 2001). This observation seems to contradict studies that found monocytes to be resistant to viral entry by viruses pseudotyped with EBOV GP (Yonezawa et al. 2005; Dube et al. 2008). An explanation that may resolve this apparent contradiction is that as monocytes differentiate towards a macrophage or DC phenotype, they acquire permissiveness for GP-mediated entry (Martinez et al. 2013). This hypothesis suggests that monocytes that are infected by EBOV are in the process of differentiating, a process that may be facilitated by interaction of the cells with GP.
In vitro studies suggest that monocytes and macrophages may be significant sources of the cytokines that are characteristic of severe filovirus disease. Substantial cytokine and chemokine expression is induced early in filovirus infection of monocytes or macrophages (Hensley et al. 2002; Gupta et al. 2001; Stroher et al. 2001; Martinez et al. 2013; Wahl-Jensen et al. 2011; Ayithan et al. 2014; Olejnik et al. 2017). Similar responses are elicited by inactivated EBOV and by Ebola VLPs generated by co-expressing EBOV VP40 and GP (Hensley et al. 2002; Stroher et al. 2001; Wahl-Jensen et al. 2011; Olejnik et al. 2017; Wahl-Jensen et al. 2005). This shows that viral genome replication and transcription within the infected cells are not required for the induction of the observed inflammatory response. VLP studies revealed that EBOV GP is sufficient to stimulate cytokine and chemokine expression. Intriguingly, EBOV GP activates Toll-like receptor 4 (TLR4) and induces downstream inflammatory responses (Okumura et al. 2010; Escudero-Perez et al. 2014). TLR4 activation is mediated by both GP inserted on the surface of viral particles and shed GP, a truncated form of membrane-bound GP lacking the transmembrane domain (Olejnik et al. 2017; Escudero-Perez et al. 2014). In contrast, soluble GP, the carboxy terminal part of which differs from transmembrane GP and shed GP, cannot activate TLR4-mediated inflammatory responses (Wahl-Jensen et al. 2005; Escudero-Perez et al. 2014). There are conflicting results regarding the activation of human macrophages by RESTV infection. In one study, RESTV infection led to a robust activation of human monocytes and macrophages similar to EBOV, whereas RESTV-infected macrophages remained remarkably silent in another study (Stroher et al. 2001; Olejnik et al. 2017). It is conceivable that different procedures to generate virus stocks might account for this discrepancy (Hartman et al. 2008). VLPs containing RESTV GP fail to stimulate a pro-inflammatory response in primary human macrophages, indicating that RESTV GP does not trigger TLR4 signaling (Olejnik et al. 2017). The inability of RESTV GP to activate human macrophages through TLR4 might contribute to lower pathogenicity by preventing the cytokine storm observed in EBOV infection. Interestingly, EBOV GP-mediated TLR4 activation of macrophages can be inhibited by using TLR4 antagonists or anti-TLR4 antibodies which opens up potential treatment options (Olejnik et al. 2017; Escudero-Perez et al. 2014). Further studies are needed, however, to determine to what extent GP drives monocyte and macrophage pro-inflammatory responses, whether TLR4 signaling is the dominant pathway inducing this response and if TLR4 activation is correlated with pathogenicity. Although it seems counterproductive for a virus to induce a strong inflammatory response in the infected cells, GP-mediated TLR4 activation might be beneficial for the virus. Among the upregulated host proteins detected in GP-activated macrophages are suppressor of cytokine signaling 1 and 3 (SOCS1 and SOCS3). Intriguingly, SOCS3 enhances EBOV particle budding supporting the hypothesis that the induction of a pro-inflammatory response promotes EBOV infection (Olejnik et al. 2017; Okumura et al. 2010, 2015).
4.2 Dendritic Cells
DCs play a critical role in linking the innate and adaptive immunity. They respond to pathogens by undergoing a maturation process that facilitates presentation of antigen to and stimulation of T cell responses (Lanzavecchia 1999). Like macrophages, DCs are productively infected by filoviruses (Bosio et al. 2003; Mahanty et al. 2003). However, whereas EBOV infection of monocytes and macrophages leads to substantial cytokine production, as discussed above, a much more muted cytokine response is produced by infected human monocyte-derived DCs. In each case, a minimal response and an absence of IFN responses, as assessed by cytokine production or gene expression changes, occurs following infection (Hensley et al. 2002; Bosio et al. 2003; Mahanty et al. 2003; Lubaki et al. 2013). Further, other measures of DC maturation are also suppressed, including the upregulation of cell surface markers and activation of T cell responses (Bosio et al. 2003; Mahanty et al. 2003; Lubaki et al. 2013, 2016).
Stimulation of human DCs with VLPs exposing EBOV GP or recombinant shed EBOV GP leads to activation of cells and secretion of cytokines and chemokines (Escudero-Perez et al. 2014; Bosio et al. 2004; Martinez et al. 2007; Ye et al. 2006). Inflammatory responses after stimulation with recombinant shed EBOV GP are inhibited by anti-TLR4 antibodies, suggesting GP-TLR4 mediated activation comparable to macrophages as discussed above (Escudero-Perez et al. 2014). In addition, EBOV GP delivered by VLPs interacts with C-type lectin domain family 4 member G (CLEC4G/LSECtin) on DCs, leading to the induction of an inflammatory response (Zhao et al. 2016).
The major inhibitor of DC maturation in EBOV infection appears to be the VP35 protein. VP35, when delivered to DCs with alphavirus replicons, from herpes simplex virus (HSV), or from lentiviral vectors, is effective in suppressing DC responses (Bosio et al. 2003; Yen and Basler 2016; Yen et al. 2014; Jin et al. 2010). Delivery by lentivirus allowed the comparison of wild-type and mutant VP35s and their capacity to counteract different DC maturation stimuli and signaling pathways (Yen et al. 2014). Wild-type EBOV VP35 effectively suppresses DC maturation induced by stimuli that signal via either the RIG-I or MDA5 pathways. The suppression is manifested by impairment of IFNA or IFNB gene expression, a decrease in inflammatory cytokine production, suppressed upregulation of cell surface markers of maturation, and impaired capacity to stimulate T cell responses (Yen et al. 2014). VP35 mutants previously described to lose dsRNA binding and RIG-I inhibitory activities lost the capacity to suppress each of these measures of DC maturation and function (Yen et al. 2014). Delivery of MARV VP35 has the same effect as EBOV VP35 (Yen and Basler 2016). Delivery of the other defined innate immune antagonists of either EBOV or MARV, including EBOV VP24, MARV VP40, and MARV VP24, has only limited impact on DC maturation (Yen and Basler 2016). Both EBOV VP24 and MARV VP40 effectively suppress ISG upregulation following either infection with the RIG-I activating SeV or following treatment of cells with IFN. Nonetheless, these effects of EBOV VP24 or MARV VP40 are insufficient to prevent upregulation of cell surface markers of maturation or to impair T cell activation. Similarly, although MARV VP24 can modulate expression of genes connected to the antioxidant response, it had no impact on other measures of DC maturation (Yen and Basler 2016).
The findings obtained by studying individual filovirus proteins are consistent with the results obtained with recombinant EBOVs possessing mutations in VP35 or VP24 proteins important for inhibition of IFN induction and signaling. In contrast to EBOV encoding wild-type IFN antagonists, recombinant EBOV containing mutant VP35 triggers robust IFN and cytokine responses, upregulates cell surface markers, and becomes able to stimulate T cell responses (Lubaki et al. 2013). Mutation of EBOV VP24 had modest impact on DC maturation (Lubaki et al. 2013). These findings therefore suggest that VP35 plays a critical role in suppressing DC maturation in the context of EBOV infection. Studies of lentivirus-transduced DCs indicate that VP35 potently inhibits RIG-I and MDA5 signaling but has only a very modest effect on DC responses after LPS induced signaling, mediated by TLR4 (Yen et al. 2011). These data therefore suggest that RLR signaling plays the determining role in DC maturation induced by the VP35 mutant. Why GP signaling via TLR4 is not sufficient to induce DC maturation remains to be clarified.
Plasmacytoid DCs (pDCs) represent a special class of DCs that produce copious amounts of IFNα in response to viral stimulation. In pDCs, response to RNA viruses such as EBOV is largely TLR7-dependent. When the EBOV VP35 protein is delivered to pDCs via a recombinant Newcastle disease virus (NDV), it is ineffective at countering pDC IFNα production (Leung et al. 2011). Consistent with an inability to block IFNα production in this system, VP35 is unable to block signaling by TLR7 when TLR7 is expressed by transfection in 293T cells. Interestingly, in in vitro infections EBOV fails to trigger IFNα production by pDCs and EBOV particles fail to enter pDCs (Leung et al. 2011). IFNα–producing pDCs have been detected in the spleen of MARV-infected macaques, but it was not determined if these cells were infected with MARV or were noninfected cells (Fritz et al. 2008). It remains to be determined whether pDCs are activated during EBOV infection in vivo and if EBOV and MARV differ in their ability to activate IFN responses in this cell type.
Contributor Information
Judith Olejnik, Department of Microbiology and National Emerging Infectious Diseases Laboratories, Boston University School of Medicine, 620 Albany Street, Boston, MA 02118 USA.
Adam J. Hume, Department of Microbiology and National Emerging Infectious Diseases Laboratories, Boston University School of Medicine, 620 Albany Street, Boston, MA 02118 USA
Daisy W. Leung, Department of Pathology and Immunology, Washington University School of Medicine in St. Louis, St. Louis, MO 63110 USA
Gaya K. Amarasinghe, Department of Pathology and Immunology, Washington University School of Medicine in St. Louis, St. Louis, MO 63110 USA
Christopher F. Basler, Microbial Pathogenesis, Georgia State University, Institute for Biomedical Sciences, Atlanta, GA 30303 USA
Elke Mühlberger, Department of Microbiology and National Emerging Infectious Diseases Laboratories, Boston University School of Medicine, 620 Albany Street, Boston, MA 02118 USA.
References
- Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol. 2004;4(7):499–511. doi: 10.1038/nri1391. [DOI] [PubMed] [Google Scholar]
- Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124(4):783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Alazard-Dany N, et al. Ebola virus glycoprotein GP is not cytotoxic when expressed constitutively at a moderate level. J Gen Virol. 2006;87(Pt 5):1247–1257. doi: 10.1099/vir.0.81361-0. [DOI] [PubMed] [Google Scholar]
- Alber D, Staeheli P. Partial inhibition of vesicular stomatitis virus by the interferon-induced human 9–27 protein. J Interferon Cytokine Res. 1996;16(5):375–380. doi: 10.1089/jir.1996.16.375. [DOI] [PubMed] [Google Scholar]
- Alves DA, et al. Aerosol exposure to the Angola strain of Marburg virus causes lethal viral hemorrhagic fever in cynomolgus macaques. Vet Pathol. 2010;47(5):831–851. doi: 10.1177/0300985810378597. [DOI] [PubMed] [Google Scholar]
- Anafu AA, et al. Interferon-inducible transmembrane protein 3 (IFITM3) restricts reovirus cell entry. J Biol Chem. 2013;288(24):17261–17271. doi: 10.1074/jbc.M112.438515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayithan N, et al. Ebola virus-like particles stimulate type I interferons and proinflammatory cytokine expression through the toll-like receptor and interferon signaling pathways. J Interferon Cytokine Res. 2014;34(2):79–89. doi: 10.1089/jir.2013.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey CC, et al. IFITM-family proteins: the cell’s first line of antiviral defense. Annu Rev Virol. 2014;1:261–283. doi: 10.1146/annurev-virology-031413-085537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baize S, et al. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat Med. 1999;5(4):423–426. doi: 10.1038/7422. [DOI] [PubMed] [Google Scholar]
- Baize S, et al. Inflammatory responses in Ebola virus-infected patients. Clin Exp Immunol. 2002;128(1):163–168. doi: 10.1046/j.1365-2249.2002.01800.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrientos LG, Rollin PE. Release of cellular proteases into the acidic extracellular milieu exacerbates Ebola virus-induced cell damage. Virology. 2007;358(1):1–9. doi: 10.1016/j.virol.2006.08.018. [DOI] [PubMed] [Google Scholar]
- Baskerville A, et al. The pathology of experimental Ebola virus infection in monkeys. J Pathol. 1978;125(3):131–138. doi: 10.1002/path.1711250303. [DOI] [PubMed] [Google Scholar]
- Basler CF, Amarasinghe GK. Evasion of interferon responses by Ebola and Marburg viruses. J Interferon Cytokine Res. 2009;29(9):511–520. doi: 10.1089/jir.2009.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S, et al. Interactions of Marburg virus nucleocapsid proteins. Virol. 1998;249(2):406–417. doi: 10.1006/viro.1998.9328. [DOI] [PubMed] [Google Scholar]
- Berke IC, Modis Y. MDA5 cooperatively forms dimers and ATP-sensitive filaments upon binding double-stranded RNA. EMBO J. 2012;31(7):1714–1726. doi: 10.1038/emboj.2012.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bick MJ, et al. Expression of the zinc-finger antiviral protein inhibits alphavirus replication. J Virol. 2003;77(21):11555–11562. doi: 10.1128/JVI.77.21.11555-11562.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird BH, et al. Humanized mouse model of Ebola virus disease mimics the immune responses in human disease. J Infect Dis. 2016;213(5):703–711. doi: 10.1093/infdis/jiv538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorndal AS, Szekely L, Elgh F. Ebola virus infection inversely correlates with the overall expression levels of promyelocytic leukaemia (PML) protein in cultured cells. BMC Microbiol. 2003;3:6. doi: 10.1186/1471-2180-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehmann Y, et al. A reconstituted replication and transcription system for Ebola virus Reston and comparison with Ebola virus Zaire. Virology. 2005;332(1):406–417. doi: 10.1016/j.virol.2004.11.018. [DOI] [PubMed] [Google Scholar]
- Bosio CM, et al. Ebola and Marburg viruses replicate in monocyte-derived dendritic cells without inducing the production of cytokines and full maturation. J Infect Dis. 2003;188(11):1630–1638. doi: 10.1086/379199. [DOI] [PubMed] [Google Scholar]
- Bosio CM, et al. Ebola and Marburg virus-like particles activate human myeloid dendritic cells. Virology. 2004;326(2):280–287. doi: 10.1016/j.virol.2004.05.025. [DOI] [PubMed] [Google Scholar]
- Bradfute SB, et al. Lymphocyte death in a mouse model of Ebola virus infection. J Infect Dis. 2007;196(Suppl 2):S296–S304. doi: 10.1086/520602. [DOI] [PubMed] [Google Scholar]
- Bradfute SB, Warfield KL, Bavari S. Functional CD8 + T cell responses in lethal Ebola virus infection. J Immunol. 2008;180(6):4058–4066. doi: 10.4049/jimmunol.180.6.4058. [DOI] [PubMed] [Google Scholar]
- Bradfute SB, et al. Mechanisms and consequences of ebolavirus-induced lymphocyte apoptosis. J Immunol. 2010;184(1):327–335. doi: 10.4049/jimmunol.0901231. [DOI] [PubMed] [Google Scholar]
- Brannan JM, et al. Interferon alpha/beta receptor-deficient mice as a model for ebola virus disease. J Infect Dis. 2015;212(Suppl 2):S282–S294. doi: 10.1093/infdis/jiv215. [DOI] [PubMed] [Google Scholar]
- Brass AL, et al. The IFITM proteins mediate cellular resistance to influenza A H1N1 virus, West Nile virus, and dengue virus. Cell. 2009;139(7):1243–1254. doi: 10.1016/j.cell.2009.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray M, Geisbert TW. Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola hemorrhagic fever. Int J Biochem Cell Biol. 2005;37(8):1560–1566. doi: 10.1016/j.biocel.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Bray M, et al. Haematological, biochemical and coagulation changes in mice, guinea-pigs and monkeys infected with a mouse-adapted variant of Ebola Zaire virus. J Comp Pathol. 2001;125(4):243–253. doi: 10.1053/jcpa.2001.0503. [DOI] [PubMed] [Google Scholar]
- Bujnicki JM, Rychlewski L. In silico identification, structure prediction and phylogenetic analysis of the 2′-O-ribose (cap 1) methyltransferase domain in the large structural protein of ssRNA negative-strand viruses. Protein Eng. 2002;15(2):101–108. doi: 10.1093/protein/15.2.101. [DOI] [PubMed] [Google Scholar]
- Caballero IS, et al. Lassa and Marburg viruses elicit distinct host transcriptional responses early after infection. BMC Genom. 2014;15:960. doi: 10.1186/1471-2164-15-960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero IS, et al. In vivo Ebola virus infection leads to a strong innate response in circulating immune cells. BMC Genom. 2016;17:707. doi: 10.1186/s12864-016-3060-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan SY, Ma MC, Goldsmith MA. Differential induction of cellular detachment by envelope glycoproteins of Marburg and Ebola (Zaire) viruses. J Gen Virol. 2000;81(Pt 9):2155–2159. doi: 10.1099/0022-1317-81-9-2155. [DOI] [PubMed] [Google Scholar]
- Chelbi-Alix MK, et al. Induction of the PML protein by interferons in normal and APL cells. Leukemia. 1995;9(12):2027–2033. [PubMed] [Google Scholar]
- Chelbi-Alix MK, et al. Resistance to virus infection conferred by the interferon-induced promyelocytic leukemia protein. J Virol. 1998;72(2):1043–1051. doi: 10.1128/jvi.72.2.1043-1051.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chook YM, Blobel G. Karyopherins and nuclear import. Curr Opin Struct Biol. 2001;11(6):703–715. doi: 10.1016/s0959-440x(01)00264-0. [DOI] [PubMed] [Google Scholar]
- Chow KT, Gale M., Jr Snapshot: interferon signaling. Cell. 2015;163:1808. doi: 10.1016/j.cell.2015.12.008. [DOI] [PubMed] [Google Scholar]
- Connolly BM, et al. Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis. 1999;179(Suppl 1):S203–S217. doi: 10.1086/514305. [DOI] [PubMed] [Google Scholar]
- Connor JH, et al. Transcriptional profiling of the immune response to Marburg virus infection. J Virol. 2015;89(19):9865–9874. doi: 10.1128/JVI.01142-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti E, Izaurralde E. Nucleocytoplasmic transport enters the atomic age. Curr Opin Cell Biol. 2001;13(3):310–319. doi: 10.1016/s0955-0674(00)00213-1. [DOI] [PubMed] [Google Scholar]
- Conti E, Kuriyan J. Crystallographic analysis of the specific yet versatile recognition of distinct nuclear localization signals by karyopherin alpha. Struct. 2000;8(3):329–338. doi: 10.1016/s0969-2126(00)00107-6. [DOI] [PubMed] [Google Scholar]
- Conti E, et al. Crystallographic analysis of the recognition of a nuclear localization signal by the nuclear import factor karyopherin alpha. Cell. 1998;94(2):193–204. doi: 10.1016/s0092-8674(00)81419-1. [DOI] [PubMed] [Google Scholar]
- Copple IM, et al. The Nrf2-Keap1 defence pathway: role in protection against drug-induced toxicity. Toxicology. 2008;246(1):24–33. doi: 10.1016/j.tox.2007.10.029. [DOI] [PubMed] [Google Scholar]
- Cross RW, et al. Modeling the disease course of Zaire ebolavirus Infection in the outbred Guinea Pig. J Infect Dis. 2015;212(Suppl 2):S305–S315. doi: 10.1093/infdis/jiv237. [DOI] [PubMed] [Google Scholar]
- Daffis S, et al. 2′-O methylation of the viral mRNA cap evades host restriction by IFIT family members. Nature. 2010;468(7322):452–456. doi: 10.1038/nature09489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauber B, Wolff T. Activation of the antiviral kinase PKR and viral countermeasures. Viruses. 2009;1(3):523–544. doi: 10.3390/v1030523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond MS, Farzan M. The broad-spectrum antiviral functions of IFIT and IFITM proteins. Nat Rev Immunol. 2013;13(1):46–57. doi: 10.1038/nri3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolnik O, et al. Ectodomain shedding of the glycoprotein GP of Ebola virus. EMBO J. 2004;23(10):2175–2184. doi: 10.1038/sj.emboj.7600219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolnik O, et al. Shedding of Ebola virus surface glycoprotein is a mechanism of self-regulation of cellular cytotoxicity and has a direct effect on virus infectivity. J Infect Dis. 2015;212(Suppl 2):S322–S328. doi: 10.1093/infdis/jiv268. [DOI] [PubMed] [Google Scholar]
- Dube D, et al. Cell adhesion promotes Ebola virus envelope glycoprotein-mediated binding and infection. J Virol. 2008;82(14):7238–7242. doi: 10.1128/JVI.00425-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebihara H, et al. Host response dynamics following lethal infection of rhesus macaques with Zaire ebolavirus. J Infect Dis. 2011;204(Suppl 3):S991–S999. doi: 10.1093/infdis/jir336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebihara H, et al. A Syrian golden hamster model recapitulating ebola hemorrhagic fever. J Infect Dis. 2013;207(2):306–318. doi: 10.1093/infdis/jis626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards MR, Basler CF. Marburg virus VP24 protein relieves suppression of the NF-kappaB pathway through interaction with kelch-like ECH-associated protein 1. J Infect Dis. 2015;212(Suppl 2):S154–S159. doi: 10.1093/infdis/jiv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards MR, et al. Differential regulation of interferon responses by Ebola and Marburg virus VP35 proteins. Cell Rep. 2016;14(7):1632–1640. doi: 10.1016/j.celrep.2016.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis DS, et al. Ultrastructure of Ebola virus particles in human liver. J Clin Pathol. 1978;31(3):201–208. doi: 10.1136/jcp.31.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escudero-Perez B, et al. Shed GP of Ebola virus triggers immune activation and increased vascular permeability. PLoS Pathog. 2014;10(11):e1004509. doi: 10.1371/journal.ppat.1004509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett RD, Chelbi-Alix MK. PML and PML nuclear bodies: implications in antiviral defence. Biochimie. 2007;89(6–7):819–830. doi: 10.1016/j.biochi.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Everitt AR, et al. Defining the range of pathogens susceptible to Ifitm3 restriction using a knockout mouse model. PLoS ONE. 2013;8(11):e80723. doi: 10.1371/journal.pone.0080723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabozzi G, et al. Ebolavirus proteins suppress the effects of small interfering RNA by direct interaction with the mammalian RNA interference pathway. J Virol. 2011;85(6):2512–2523. doi: 10.1128/JVI.01160-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feagins AR, Basler CF. The VP40 protein of Marburg virus exhibits impaired budding and increased sensitivity to human tetherin following mouse adaptation. J Virol. 2014;88(24):14440–14450. doi: 10.1128/JVI.02069-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feagins AR, Basler CF. Lloviu virus VP24 and VP35 proteins function as innate immune antagonists in human and bat cells. Virol. 2015;485:145–152. doi: 10.1016/j.virol.2015.07.010. [DOI] [PubMed] [Google Scholar]
- Feldmann H, Geisbert TW. Ebola haemorrhagic fever. Lancet. 2011;377(9768):849–862. doi: 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H, et al. Filovirus-induced endothelial leakage triggered by infected monocytes/macrophages. J Virol. 1996;70(4):2208–2214. doi: 10.1128/jvi.70.4.2208-2214.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Z, et al. The VP35 protein of Ebola virus inhibits the antiviral effect mediated by double-stranded RNA-dependent protein kinase PKR. J Virol. 2007;81(1):182–192. doi: 10.1128/JVI.01006-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fensterl V, Sen GC. The ISG56/IFIT1 gene family. J Interferon Cytokine Res. 2011;31(1):71–78. doi: 10.1089/jir.2010.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fensterl V, Sen GC. Interferon-induced Ifit proteins: their role in viral pathogenesis. J Virol. 2015;89(5):2462–2468. doi: 10.1128/JVI.02744-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernando L, et al. Immune response to Marburg virus angola infection in nonhuman primates. J Infect Dis. 2015;212(Suppl 2):S234–S241. doi: 10.1093/infdis/jiv095. [DOI] [PubMed] [Google Scholar]
- Ferron F, et al. Viral RNA-polymerases--a predicted 2′-O-ribose methyltransferase domain shared by all Mononegavirales. Trends Biochem Sci. 2002;27(5):222–224. doi: 10.1016/s0968-0004(02)02091-1. [DOI] [PubMed] [Google Scholar]
- Francica JR, Matukonis MK, Bates P. Requirements for cell rounding and surface protein down-regulation by Ebola virus glycoprotein. Virology. 2009;383(2):237–247. doi: 10.1016/j.virol.2008.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz EA, et al. Cellular immune response to Marburg virus infection in cynomolgus macaques. Viral Immunol. 2008;21(3):355–363. doi: 10.1089/vim.2008.0023. [DOI] [PubMed] [Google Scholar]
- Gao G, Guo X, Goff SP. Inhibition of retroviral RNA production by ZAP, a CCCH-type zinc finger protein. Science. 2002;297(5587):1703–1706. doi: 10.1126/science.1074276. [DOI] [PubMed] [Google Scholar]
- Garcia MA, et al. Impact of protein kinase PKR in cell biology: from antiviral to antiproliferative action. Microbiol Mol Biol Rev. 2006;70(4):1032–1060. doi: 10.1128/MMBR.00027-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia MA, Meurs EF, Esteban M. The dsRNA protein kinase PKR: virus and cell control. Biochimie. 2007;89(6–7):799–811. doi: 10.1016/j.biochi.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Gedigk P, Bechtelsheimer H, Korb G. Pathological anatomy of the “Marburg virus” disease (the so-called “Marburg monkey disease”) Dtsch Med Wochenschr. 1968;93(12):590–601. doi: 10.1055/s-0028-1105101. [DOI] [PubMed] [Google Scholar]
- Geisbert TW, et al. Apoptosis induced in vitro and in vivo during infection by Ebola and Marburg viruses. Lab Invest. 2000;80(2):171–186. doi: 10.1038/labinvest.3780021. [DOI] [PubMed] [Google Scholar]
- Geisbert TW, et al. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: evidence that dendritic cells are early and sustained targets of infection. Am J Pathol. 2003a;163(6):2347–2370. doi: 10.1016/S0002-9440(10)63591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert TW, et al. Pathogenesis of Ebola hemorrhagic fever in primate models: evidence that hemorrhage is not a direct effect of virus-induced cytolysis of endothelial cells. Am J Pathol. 2003b;163(6):2371–2382. doi: 10.1016/S0002-9440(10)63592-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisbert TW, et al. Treatment of Ebola virus infection with a recombinant inhibitor of factor VIIa/tissue factor: a study in rhesus monkeys. Lancet. 2003c;362(9400):1953–1958. doi: 10.1016/S0140-6736(03)15012-X. [DOI] [PubMed] [Google Scholar]
- Geisbert TW, et al. Marburg virus Angola infection of rhesus macaques: pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J Infect Dis. 2007;196(Suppl 2):S372–S381. doi: 10.1086/520608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geoffroy MC, Chelbi-Alix MK. Role of promyelocytic leukemia protein in host antiviral defense. J Interferon Cytokine Res. 2011;31(1):145–158. doi: 10.1089/jir.2010.0111. [DOI] [PubMed] [Google Scholar]
- Gerlier D, Lyles DS. Interplay between innate immunity and negative-strand RNA viruses: towards a rational model. Microbiol Mol Biol Rev. 2011;75(3):468–490. doi: 10.1128/MMBR.00007-11. (second page of table of contents) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb TR, et al. Pathogenesis of experimental Ebola Zaire virus infection in BALB/c mice. J Comp Pathol. 2001;125(4):233–242. doi: 10.1053/jcpa.2001.0502. [DOI] [PubMed] [Google Scholar]
- Groseth A, et al. The Ebola virus glycoprotein contributes to but is not sufficient for virulence in vivo. PLoS Pathog. 2012;8(8):e1002847. doi: 10.1371/journal.ppat.1002847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guito JC, et al. Novel activities by ebolavirus and marburgvirus interferon antagonists revealed using a standardized in vitro reporter system. Virol. 2016;501:147–165. doi: 10.1016/j.virol.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X, et al. The zinc-finger antiviral protein recruits the RNA processing exosome to degrade the target mRNA. Proc Natl Acad Sci U S A. 2007;104(1):151–156. doi: 10.1073/pnas.0607063104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta M, et al. Monocyte-derived human macrophages and peripheral blood mononuclear cells infected with ebola virus secrete MIP-1alpha and TNF-alpha and inhibit poly-IC-induced IFN-alpha in vitro. Virology. 2001;284(1):20–25. doi: 10.1006/viro.2001.0836. [DOI] [PubMed] [Google Scholar]
- Gupta M, Spiropoulou C, Rollin PE. Ebola virus infection of human PBMCs causes massive death of macrophages, CD4 and CD8 T cell sub-populations in vitro. Virology. 2007;364(1):45–54. doi: 10.1016/j.virol.2007.02.017. [DOI] [PubMed] [Google Scholar]
- Gupta M, et al. Reduced virus replication, proinflammatory cytokine production, and delayed macrophage cell death in human PBMCs infected with the newly discovered Bundibugyo ebolavirus relative to Zaire ebolavirus. Virology. 2010;402(1):203–208. doi: 10.1016/j.virol.2010.03.024. [DOI] [PubMed] [Google Scholar]
- Haasnoot J, Berkhout B. RNAi and cellular miRNAs in infections by mammalian viruses. Methods Mol Biol. 2011;721:23–41. doi: 10.1007/978-1-61779-037-9_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haasnoot J, et al. The Ebola virus VP35 protein is a suppressor of RNA silencing. PLoS Pathog. 2007;3(6):e86. doi: 10.1371/journal.ppat.0030086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacke M, et al. Inhibition of Ebola virus glycoprotein-mediated cytotoxicity by targeting its transmembrane domain and cholesterol. Nat Commun. 2015;6:7688. doi: 10.1038/ncomms8688. [DOI] [PubMed] [Google Scholar]
- Haller O, et al. Mx GTPases: dynamin-like antiviral machines of innate immunity. Trends Microbiol. 2015;23(3):154–163. doi: 10.1016/j.tim.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Han Z, et al. Permeabilization of the plasma membrane by Ebola virus GP2. Virus Genes. 2007;34(3):273–281. doi: 10.1007/s11262-006-0009-4. [DOI] [PubMed] [Google Scholar]
- Hartlieb B, Weissenhorn W. Filovirus assembly and budding. Virology. 2006;344(1):64–70. doi: 10.1016/j.virol.2005.09.018. [DOI] [PubMed] [Google Scholar]
- Hartman AL, et al. Whole-genome expression profiling reveals that inhibition of host innate immune response pathways by Ebola virus can be reversed by a single amino acid change in the VP35 protein. J Virol. 2008;82(11):5348–5358. doi: 10.1128/JVI.00215-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensley LE, et al. Proinflammatory response during Ebola virus infection of primate models: possible involvement of the tumor necrosis factor receptor superfamily. Immunol Lett. 2002;80(3):169–179. doi: 10.1016/s0165-2478(01)00327-3. [DOI] [PubMed] [Google Scholar]
- Hensley LE, et al. Pathogenesis of Marburg hemorrhagic fever in cynomolgus macaques. J Infect Dis. 2011;204(Suppl 3):S1021–S1031. doi: 10.1093/infdis/jir339. [DOI] [PubMed] [Google Scholar]
- Herbert AS, et al. Niemann-pick C1 is essential for ebolavirus replication and pathogenesis in vivo. MBio. 2015;6(3):e00565–15. doi: 10.1128/mBio.00565-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiscott J. Convergence of the NF-kappaB and IRF pathways in the regulation of the innate antiviral response. Cytokine Growth Factor Rev. 2007;18(5–6):483–490. doi: 10.1016/j.cytogfr.2007.06.002. [DOI] [PubMed] [Google Scholar]
- Hoenen T, et al. A novel Ebola virus expressing luciferase allows for rapid and quantitative testing of antivirals. Antiviral Res. 2013;99(3):207–213. doi: 10.1016/j.antiviral.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann HH, Schneider WM, Rice CM. Interferons and viruses: an evolutionary arms race of molecular interactions. Trends Immunol. 2015;36(3):124–138. doi: 10.1016/j.it.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang IC, et al. Distinct patterns of IFITM-mediated restriction of filoviruses, SARS coronavirus, and influenza A virus. PLoS Pathog. 2011;7(1):e1001258. doi: 10.1371/journal.ppat.1001258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson KL, Rollin PE. Cytokine and chemokine expression in humans infected with Sudan Ebola virus. J Infect Dis. 2007;196(Suppl 2):S357–S363. doi: 10.1086/520611. [DOI] [PubMed] [Google Scholar]
- Hyde JL, Diamond MS. Innate immune restriction and antagonism of viral RNA lacking 2-O methylation. Virology. 2015;479–480:66–74. doi: 10.1016/j.virol.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignat’ev GM, et al. Mechanisms of protective immune response in models of Marburg fever in monkeys. Vopr Virusol. 1995;40(3):109–113. [PubMed] [Google Scholar]
- Ignatiev GM, et al. Immune and pathophysiological processes in baboons experimentally infected with Ebola virus adapted to guinea pigs. Immunol Lett. 2000;71(2):131–140. doi: 10.1016/s0165-2478(99)00169-8. [DOI] [PubMed] [Google Scholar]
- Ivashkiv LB, Donlin LT. Regulation of type I interferon responses. Nat Rev Immunol. 2014;14(1):36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamura T, et al. PACT, a double-stranded RNA binding protein acts as a positive regulator for type I interferon gene induced by Newcastle disease virus. Biochem Biophys Res Commun. 2001;282(2):515–523. doi: 10.1006/bbrc.2001.4606. [DOI] [PubMed] [Google Scholar]
- Jin H, et al. The VP35 protein of Ebola virus impairs dendritic cell maturation induced by virus and lipopolysaccharide. J Gen Virol. 2010;91(Pt 2):352–361. doi: 10.1099/vir.0.017343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin G, Gao Y, Lin HK. Cytoplasmic PML: from molecular regulation to biological functions. J Cell Biochem. 2014;115(5):812–818. doi: 10.1002/jcb.24727. [DOI] [PubMed] [Google Scholar]
- Johnson B, et al. Dimerization controls Marburg virus VP24-dependent modulation of host antioxidative stress responses. J Mol Biol. 2016;428(17):3483–3494. doi: 10.1016/j.jmb.2016.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaletsky RL, et al. Tetherin-mediated restriction of filovirus budding is antagonized by the Ebola glycoprotein. Proc Natl Acad Sci U S A. 2009;106(8):2886–2891. doi: 10.1073/pnas.0811014106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura T, et al. Ifit1 inhibits Japanese encephalitis virus replication through binding to 5′ capped 2′-O unmethylated RNA. J Virol. 2013;87(18):9997–10003. doi: 10.1128/JVI.00883-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok KH, et al. The double-stranded RNA-binding protein PACT functions as a cellular activator of RIG-I to facilitate innate antiviral response. Cell Host Microbe. 2011;9(4):299–309. doi: 10.1016/j.chom.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Kreuels B, et al. A case of severe Ebola virus infection complicated by gram-negative septicemia. N Engl J Med. 2014;371(25):2394–2401. doi: 10.1056/NEJMoa1411677. [DOI] [PubMed] [Google Scholar]
- Kuhl A, et al. The Ebola virus glycoprotein and HIV-1 Vpu employ different strategies to counteract the antiviral factor tetherin. J Infect Dis. 2011;204(Suppl 3):S850–S860. doi: 10.1093/infdis/jir378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P, et al. Inhibition of translation by IFIT family members is determined by their ability to interact selectively with the 5′-terminal regions of cap0-, cap1- and 5′ppp- mRNAs. Nucleic Acids Res. 2014;42(5):3228–3245. doi: 10.1093/nar/gkt1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labbe K, Saleh M. Cell death in the host response to infection. Cell Death Differ. 2008;15(9):1339–1349. doi: 10.1038/cdd.2008.91. [DOI] [PubMed] [Google Scholar]
- Lanzavecchia A. Dendritic cell maturation and generation of immune responses. Haematologica. 1999;84(Suppl EHA-4):23–25. [PubMed] [Google Scholar]
- Lavau C, et al. The acute promyelocytic leukaemia-associated PML gene is induced by interferon. Oncogene. 1995;11(5):871–876. [PubMed] [Google Scholar]
- Le Sage V, et al. Ebola virus VP35 blocks stress granule assembly. Virol. 2016;502:73–83. doi: 10.1016/j.virol.2016.12.012. [DOI] [PubMed] [Google Scholar]
- Leroy EM, et al. Human asymptomatic Ebola infection and strong inflammatory response. Lancet. 2000;355(9222):2210–2215. doi: 10.1016/s0140-6736(00)02405-3. [DOI] [PubMed] [Google Scholar]
- Leroy EM, et al. Early immune responses accompanying human asymptomatic Ebola infections. Clin Exp Immunol. 2001;124(3):453–460. doi: 10.1046/j.1365-2249.2001.01517.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, et al. Structure of the Ebola VP35 interferon inhibitory domain. Proc Natl Acad Sci U S A. 2009;106(2):411–416. doi: 10.1073/pnas.0807854106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, et al. Structural basis for dsRNA recognition and interferon antagonism by Ebola VP35. Nat Struct Mol Biol. 2010;17(2):165–172. doi: 10.1038/nsmb.1765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung LW, et al. Ebolavirus VP35 suppresses IFN production from conventional but not plasmacytoid dendritic cells. Immunol Cell Biol. 2011a;89(7):792–802. doi: 10.1038/icb.2010.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung LW, et al. Ebola virus failure to stimulate plasmacytoid dendritic cell interferon responses correlates with impaired cellular entry. J Infect Dis. 2011b;204(Suppl 3):S973–S977. doi: 10.1093/infdis/jir331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung DW, Basler CF, Amarasinghe GK. Molecular mechanisms of viral inhibitors of RIG-I-like receptors. Trends Microbiol. 2012;20(3):139–146. doi: 10.1016/j.tim.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lever MS, et al. Lethality and pathogenesis of airborne infection with filoviruses in A129 alpha/beta-/-interferon receptor-deficient mice. J Med Microbiol. 2012;61(Pt 1):8–15. doi: 10.1099/jmm.0.036210-0. [DOI] [PubMed] [Google Scholar]
- Li X, et al. Structural basis of double-stranded RNA recognition by the RIG-I like receptor MDA5. Arch Biochem Biophys. 2009;488(1):23–33. doi: 10.1016/j.abb.2009.06.008. [DOI] [PubMed] [Google Scholar]
- Li SH, et al. Rational design of a flavivirus vaccine by abolishing viral RNA 2′-O methylation. J Virol. 2013;87(10):5812–5819. doi: 10.1128/JVI.02806-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, et al. Induction and suppression of antiviral RNA interference by influenza A virus in mammalian cells. Nat Microbiol. 2016;2:16250. doi: 10.1038/nmicrobiol.2016.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin KL, et al. Temporal characterization of Marburg virus Angola infection following aerosol challenge in Rhesus Macaques. J Virol. 2015;89(19):9875–9885. doi: 10.1128/JVI.01147-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez LA, et al. Ebola virus glycoprotein counteracts BST-2/Tetherin restriction in a sequence-independent manner that does not require tetherin surface removal. J Virol. 2010;84(14):7243–7255. doi: 10.1128/JVI.02636-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu J, et al. The IFITM proteins inhibit HIV-1 infection. J Virol. 2011;85(5):2126–2137. doi: 10.1128/JVI.01531-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubaki NM, et al. The lack of maturation of Ebola virus-infected dendritic cells results from the cooperative effect of at least two viral domains. J Virol. 2013;87(13):7471–7485. doi: 10.1128/JVI.03316-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubaki NM, et al. The Ebola interferon inhibiting domains attenuate and dysregulate cell-mediated immune responses. PLoS Pathog. 2016;12(12):e1006031. doi: 10.1371/journal.ppat.1006031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludtke A, et al. Ebola virus disease in mice with transplanted human hematopoietic stem cells. J Virol. 2015;89(8):4700–4704. doi: 10.1128/JVI.03546-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthra P, et al. Mutual antagonism between the Ebola virus VP35 protein and the RIG-I activator PACT determines infection outcome. Cell Host Microbe. 2013;14(1):74–84. doi: 10.1016/j.chom.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahanty S, Bray M. Pathogenesis of filoviral haemorrhagic fevers. Lancet Infect Dis. 2004;4(8):487–498. doi: 10.1016/S1473-3099(04)01103-X. [DOI] [PubMed] [Google Scholar]
- Mahanty S, et al. Cutting edge: impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J Immunol. 2003;170(6):2797–2801. doi: 10.4049/jimmunol.170.6.2797. [DOI] [PubMed] [Google Scholar]
- Malakhova OA, Zhang DE. ISG15 inhibits Nedd4 ubiquitin E3 activity and enhances the innate antiviral response. J Biol Chem. 2008;283(14):8783–8787. doi: 10.1074/jbc.C800030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao R, et al. Inhibition of hepatitis B virus replication by the host zinc finger antiviral protein. PLoS Pathog. 2013;9(7):e1003494. doi: 10.1371/journal.ppat.1003494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Valmas C, Basler CF. Ebola virus-like particle-induced activation of NF-kappaB and Erk signaling in human dendritic cells requires the glycoprotein mucin domain. Virology. 2007;364(2):342–354. doi: 10.1016/j.virol.2007.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, Leung LW, Basler CF. The role of antigen-presenting cells in filoviral hemorrhagic fever: gaps in current knowledge. Antiviral Res. 2012;93(3):416–428. doi: 10.1016/j.antiviral.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez O, et al. Ebola virus exploits a monocyte differentiation program to promote its entry. J Virol. 2013;87(7):3801–3814. doi: 10.1128/JVI.02695-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins K, et al. Characterization of clinical and immunological parameters during Ebola virus infection of rhesus macaques. Viral Immunol. 2015;28(1):32–41. doi: 10.1089/vim.2014.0085. [DOI] [PubMed] [Google Scholar]
- Marzi A, et al. Antibodies are necessary for rVSV/ZEBOV-GP-mediated protection against lethal Ebola virus challenge in nonhuman primates. Proc Natl Acad Sci U S A. 2013;110(5):1893–1898. doi: 10.1073/pnas.1209591110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzi A, et al. Delayed disease progression in Cynomolgus macaques infected with Ebola virus Makona strain. Emerg Infect Dis. 2015;21(10):1777–1783. doi: 10.3201/eid2110.150259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzi A, et al. A hamster model for Marburg virus infection accurately recapitulates Marburg hemorrhagic fever. Sci Rep. 2016;6:39214. doi: 10.1038/srep39214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride KM, et al. Regulated nuclear import of the STAT1 transcription factor by direct binding of importin-alpha. EMBO J. 2002;21(7):1754–1763. doi: 10.1093/emboj/21.7.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy AK, et al. Ebola hemorrhagic fever: novel biomarker correlates of clinical outcome. J Infect Dis. 2014a;210(4):558–566. doi: 10.1093/infdis/jiu088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy AK, et al. Biomarker correlates of survival in pediatric patients with Ebola virus disease. Emerg Infect Dis. 2014b;20(10):1683–1690. doi: 10.3201/eid2010.140430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy AK, et al. Kinetic analysis of biomarkers in a cohort of US patients with Ebola virus disease. Clin Infect Dis. 2016;63(4):460–467. doi: 10.1093/cid/ciw334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melito PL, et al. The creation of stable cell lines expressing Ebola virus glycoproteins and the matrix protein VP40 and generating Ebola virus-like particles utilizing an ecdysone inducible mammalian expression system. J Virol Methods. 2008;148(1–2):237–243. doi: 10.1016/j.jviromet.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Mudhasani R, et al. IFITM-2 and IFITM-3 but not IFITM-1 restrict Rift Valley fever virus. J Virol. 2013;87(15):8451–8464. doi: 10.1128/JVI.03382-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller S, et al. Inhibition of filovirus replication by the zinc finger antiviral protein. J Virol. 2007;81(5):2391–2400. doi: 10.1128/JVI.01601-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy FA, et al. Marburg virus infection in monkeys. Ultrastructural studies. Lab Invest. 1971;24(4):279–291. [PubMed] [Google Scholar]
- Nanduri S, et al. Structure of the double-stranded RNA-binding domain of the protein kinase PKR reveals the molecular basis of its dsRNA-mediated activation. EMBO J. 1998;17(18):5458–5465. doi: 10.1093/emboj/17.18.5458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neil SJ, Zang T, Bieniasz PD. Tetherin inhibits retrovirus release and is antagonized by HIV-1 Vpu. Nature. 2008;451(7177):425–430. doi: 10.1038/nature06553. [DOI] [PubMed] [Google Scholar]
- Nelson EV, et al. Ebola virus does not induce stress granule formation during infection and sequesters stress granule proteins within viral inclusions. J Virol. 2016;90(16):7268–7284. doi: 10.1128/JVI.00459-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noyori O, et al. Suppression of Fas-mediated apoptosis via steric shielding by filovirus glycoproteins. Biochem Biophys Res Commun. 2013;441(4):994–998. doi: 10.1016/j.bbrc.2013.11.018. [DOI] [PubMed] [Google Scholar]
- Okumura A, Pitha PM, Harty RN. ISG15 inhibits Ebola VP40 VLP budding in an L-domain-dependent manner by blocking Nedd4 ligase activity. Proc Natl Acad Sci U S A. 2008;105(10):3974–3979. doi: 10.1073/pnas.0710629105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okumura A, et al. Interaction between Ebola virus glycoprotein and host toll-like receptor 4 leads to induction of proinflammatory cytokines and SOCS1. J Virol. 2010;84(1):27–33. doi: 10.1128/JVI.01462-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okumura A, et al. Suppressor of cytokine signaling 3 is an inducible host factor that regulates virus egress during Ebola virus infection. J Virol. 2015;89(20):10399–10406. doi: 10.1128/JVI.01736-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olejnik J, et al. Intracellular events and cell fate in filovirus infection. Viruses. 2011;3(8):1501–1531. doi: 10.3390/v3081501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olejnik J, et al. Ebola virus does not block apoptotic signaling pathways. J Virol. 2013;87(10):5384–5396. doi: 10.1128/JVI.01461-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olejnik J, et al. Ebolaviruses associated with differential pathogenicity induce distinct host responses in human macrophages. J Virol. 2017 doi: 10.1128/JVI.00179-17. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea JJ, et al. The JAK-STAT pathway: impact on human disease and therapeutic intervention. Annu Rev Med. 2015;66:311–328. doi: 10.1146/annurev-med-051113-024537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozato K, et al. TRIM family proteins and their emerging roles in innate immunity. Nat Rev Immunol. 2008;8(11):849–860. doi: 10.1038/nri2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page A, et al. Marburgvirus hijacks nrf2-dependent pathway by targeting nrf2-negative regulator keap1. Cell Rep. 2014;6(6):1026–1036. doi: 10.1016/j.celrep.2014.02.027. [DOI] [PubMed] [Google Scholar]
- Peisley A, et al. Cooperative assembly and dynamic disassembly of MDA5 filaments for viral dsRNA recognition. Proc Natl Acad Sci U S A. 2011;108(52):21010–21015. doi: 10.1073/pnas.1113651108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pichlmair A, et al. IFIT1 is an antiviral protein that recognizes 5′-triphosphate RNA. Nat Immunol. 2011;12(7):624–630. doi: 10.1038/ni.2048. [DOI] [PubMed] [Google Scholar]
- Pichlmair A, et al. Viral immune modulators perturb the human molecular network by common and unique strategies. Nature. 2012;487(7408):486–490. doi: 10.1038/nature11289. [DOI] [PubMed] [Google Scholar]
- Pinto AK, et al. Human and Murine IFIT1 proteins do not restrict infection of negative-sense rna viruses of the orthomyxoviridae, bunyaviridae, and filoviridae families. J Virol. 2015;89(18):9465–9476. doi: 10.1128/JVI.00996-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins KC, Cardenas WB, Basler CF. Ebola virus protein VP35 impairs the function of interferon regulatory factor-activating kinases IKKepsilon and TBK-1. J Virol. 2009;83(7):3069–3077. doi: 10.1128/JVI.01875-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins KC, et al. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J Virol. 2010a;84(6):3004–3015. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins KC, et al. Basic residues within the ebolavirus VP35 protein are required for its viral polymerase cofactor function. J Virol. 2010b;84(20):10581–10591. doi: 10.1128/JVI.00925-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu X, et al. Establishment and characterization of a lethal mouse model for the Angola strain of Marburg virus. J Virol. 2014;88(21):12703–12714. doi: 10.1128/JVI.01643-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radoshitzky SR, et al. Infectious Lassa virus, but not filoviruses, is restricted by BST-2/tetherin. J Virol. 2010;84(20):10569–10580. doi: 10.1128/JVI.00103-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramanan P, et al. Structural basis for Marburg virus VP35-mediated immune evasion mechanisms. Proc Natl Acad Sci U S A. 2012;109(50):20661–20666. doi: 10.1073/pnas.1213559109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawlings JS, Rosler KM, Harrison DA. The JAK/STAT signaling pathway. J Cell Sci. 2004;117(Pt 8):1281–1283. doi: 10.1242/jcs.00963. [DOI] [PubMed] [Google Scholar]
- Ray RB, et al. Ebola virus glycoprotein-mediated anoikis of primary human cardiac microvascular endothelial cells. Virology. 2004;321(2):181–188. doi: 10.1016/j.virol.2003.12.014. [DOI] [PubMed] [Google Scholar]
- Rebouillat D, Hovanessian AG. The human 2′,5′-oligoadenylate synthetase family: interferon-induced proteins with unique enzymatic properties. J Interferon Cytokine Res. 1999;19(4):295–308. doi: 10.1089/107999099313992. [DOI] [PubMed] [Google Scholar]
- Reed DS, et al. Depletion of peripheral blood T lymphocytes and NK cells during the course of ebola hemorrhagic fever in cynomolgus macaques. Viral Immunol. 2004;17(3):390–400. doi: 10.1089/vim.2004.17.390. [DOI] [PubMed] [Google Scholar]
- Regad T, Chelbi-Alix MK. Role and fate of PML nuclear bodies in response to interferon and viral infections. Oncogene. 2001;20(49):7274–7286. doi: 10.1038/sj.onc.1204854. [DOI] [PubMed] [Google Scholar]
- Reid SP, et al. Ebola virus VP24 binds karyopherin alpha1 and blocks STAT1 nuclear accumulation. J Virol. 2006;80(11):5156–5167. doi: 10.1128/JVI.02349-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid SP, et al. Ebola virus VP24 proteins inhibit the interaction of NPI-1 subfamily karyopherin alpha proteins with activated STAT1. J Virol. 2007;81(24):13469–13477. doi: 10.1128/JVI.01097-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhein BA, et al. Interferon-gamma inhibits Ebola virus infection. PLoS Pathog. 2015;11(11):e1005263. doi: 10.1371/journal.ppat.1005263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rippey JJ, Schepers NJ, Gear JH. The pathology of Marburg virus disease. S Afr Med J. 1984;66(2):50–54. [PubMed] [Google Scholar]
- Rougeron V, et al. Ebola and Marburg haemorrhagic fever. J Clin Virol. 2015;64:111–119. doi: 10.1016/j.jcv.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubins KH, et al. The temporal program of peripheral blood gene expression in the response of nonhuman primates to Ebola hemorrhagic fever. Genome Biol. 2007;8(8):R174. doi: 10.1186/gb-2007-8-8-r174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruibal P, et al. Unique human immune signature of Ebola virus disease in Guinea. Nature. 2016;533(7601):100–104. doi: 10.1038/nature17949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryabchikova E, Price BBS. Ebola and Marburg viruses: a view of infection using electron microscopy. Columbus, Ohio, USA: Battelle Press; 2004. [Google Scholar]
- Ryabchikova E, et al. Ebola virus infection in guinea pigs: presumable role of granulomatous inflammation in pathogenesis. Arch Virol. 1996a;141(5):909–921. doi: 10.1007/BF01718165. [DOI] [PubMed] [Google Scholar]
- Ryabchikova E, et al. Respiratory Marburg virus infection in guinea pigs. Arch Virol. 1996b;141(11):2177–2190. doi: 10.1007/BF01718224. [DOI] [PubMed] [Google Scholar]
- Ryabchikova EI, Kolesnikova LV, Luchko SV. An analysis of features of pathogenesis in two animal models of Ebola virus infection. J Infect Dis. 1999;179(Suppl 1):S199–S202. doi: 10.1086/514293. [DOI] [PubMed] [Google Scholar]
- Sadler AJ, Williams BR. Interferon-inducible antiviral effectors. Nat Rev Immunol. 2008;8(7):559–568. doi: 10.1038/nri2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakuma T, et al. Inhibition of Lassa and Marburg virus production by tetherin. J Virol. 2009;83(5):2382–2385. doi: 10.1128/JVI.01607-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez A, et al. Analysis of human peripheral blood samples from fatal and nonfatal cases of Ebola (Sudan) hemorrhagic fever: cellular responses, virus load, and nitric oxide levels. J Virol. 2004;78(19):10370–10377. doi: 10.1128/JVI.78.19.10370-10377.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlee M, et al. Recognition of 5′ triphosphate by RIG-I helicase requires short blunt double-stranded RNA as contained in panhandle of negative-strand virus. Immun. 2009;31(1):25–34. doi: 10.1016/j.immuni.2009.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt A, et al. 5′-triphosphate RNA requires base-paired structures to activate antiviral signaling via RIG-I. Proc Natl Acad Sci U S A. 2009;106(29):12067–12072. doi: 10.1073/pnas.0900971106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt KM, et al. Recombinant Marburg virus expressing EGFP allows rapid screening of virus growth and real-time visualization of virus spread. J Infect Dis. 2011;204(Suppl 3):S861–S870. doi: 10.1093/infdis/jir308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider WM, Chevillotte MD, Rice CM. Interferon-stimulated genes: a complex web of host defenses. Annu Rev Immunol. 2014;32:513–545. doi: 10.1146/annurev-immunol-032713-120231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schümann M, Gantke T, Mühlberger E. Ebola virus VP35 antagonizes PKR activity through its C-terminal interferon inhibitory domain. J Virol. 2009;83(17):8993–8997. doi: 10.1128/JVI.00523-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz TM, et al. VP24-karyopherin alpha binding affinities differ between Ebolavirus species influencing interferon inhibition and VP24 stability. J Virol. 2016 doi: 10.1128/JVI.01715-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekimoto T, et al. Extracellular signal-dependent nuclear import of Stat1 is mediated by nuclear pore-targeting complex formation with NPI-1, but not Rch1. EMBO J. 1997;16(23):7067–7077. doi: 10.1093/emboj/16.23.7067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons G, et al. Ebola virus glycoproteins induce global surface protein down-modulation and loss of cell adherence. J Virol. 2002;76(5):2518–2528. doi: 10.1128/jvi.76.5.2518-2528.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroher U, et al. Infection and activation of monocytes by Marburg and Ebola viruses. J Virol. 2001;75(22):11025–11033. doi: 10.1128/JVI.75.22.11025-11033.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan NJ, et al. Ebola virus glycoprotein toxicity is mediated by a dynamin-dependent protein-trafficking pathway. J Virol. 2005;79(1):547–553. doi: 10.1128/JVI.79.1.547-553.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Q, et al. The specific and essential role of MAVS in antiviral innate immune responses. Immun. 2006;24(5):633–642. doi: 10.1016/j.immuni.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Szretter KJ, et al. 2′-O methylation of the viral mRNA cap by West Nile virus evades ifit1-dependent and -independent mechanisms of host restriction in vivo. PLoS Pathog. 2012;8(5):e1002698. doi: 10.1371/journal.ppat.1002698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada A, et al. Downregulation of beta1 integrins by Ebola virus glycoprotein: implication for virus entry. Virology. 2000;278(1):20–26. doi: 10.1006/viro.2000.0601. [DOI] [PubMed] [Google Scholar]
- Takeuchi O, Akira S. MDA5/RIG-I and virus recognition. Curr Opin Immunol. 2008;20(1):17–22. doi: 10.1016/j.coi.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Thi EP, et al. Lipid nanoparticle siRNA treatment of Ebola-virus-Makona-infected nonhuman primates. Nature. 2015;521(7552):362–365. doi: 10.1038/nature14442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umbach JL, Cullen BR. The role of RNAi and microRNAs in animal virus replication and antiviral immunity. Genes Dev. 2009;23(10):1151–1164. doi: 10.1101/gad.1793309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valmas C, et al. Marburg virus evades interferon responses by a mechanism distinct from ebola virus. PLoS Pathog. 2010;6(1):e1000721. doi: 10.1371/journal.ppat.1000721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Paassen J, et al. Acute liver failure, multiorgan failure, cerebral oedema, and activation of proangiogenic and antiangiogenic factors in a case of Marburg haemorrhagic fever. Lancet Infect Dis. 2012;12(8):635–642. doi: 10.1016/S1473-3099(12)70018-X. [DOI] [PubMed] [Google Scholar]
- Vasselon T, et al. RNAi and retroviruses: are they in RISC? Biomol Concepts. 2013;4(1):43–52. doi: 10.1515/bmc-2012-0041. [DOI] [PubMed] [Google Scholar]
- Villinger F, et al. Markedly elevated levels of interferon (IFN)-gamma, IFN-alpha, interleukin (IL)-2, IL-10, and tumor necrosis factor-alpha associated with fatal Ebola virus infection. J Infect Dis. 1999;179(Suppl 1):S188–S191. doi: 10.1086/514283. [DOI] [PubMed] [Google Scholar]
- Vladimer GI, Gorna MW, Superti-Furga G. IFITs: emerging roles as key anti-viral proteins. Front Immunol. 2014;5:94. doi: 10.3389/fimmu.2014.00094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volchkov VE, et al. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science. 2001;291(5510):1965–1969. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- Volchkova VA, et al. RNA editing of the GP gene of Ebola virus is an important pathogenicity factor. J Infect Dis. 2015;212(Suppl 2):S226–S233. doi: 10.1093/infdis/jiv309. [DOI] [PubMed] [Google Scholar]
- Wahl-Jensen V, et al. Role of Ebola virus secreted glycoproteins and virus-like particles in activation of human macrophages. J Virol. 2005;79(4):2413–2419. doi: 10.1128/JVI.79.4.2413-2419.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl-Jensen V, et al. Ebola virion attachment and entry into human macrophages profoundly effects early cellular gene expression. PLoS Negl Trop Dis. 2011;5(10):e1359. doi: 10.1371/journal.pntd.0001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warfield KL, et al. Development of a model for marburgvirus based on severe-combined immunodeficiency mice. Virol J. 2007;4:108. doi: 10.1186/1743-422X-4-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warfield KL, et al. Development and characterization of a mouse model for Marburg hemorrhagic fever. J Virol. 2009;83(13):6404–6415. doi: 10.1128/JVI.00126-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren TK, et al. Antiviral activity of a small-molecule inhibitor of filovirus infection. Antimicrob Agents Chemother. 2010;54(5):2152–2159. doi: 10.1128/AAC.01315-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wauquier N, et al. Human fatal Zaire Ebola virus infection is associated with an aberrant innate immunity and with massive lymphocyte apoptosis. PLoS Negl Trop Dis. 2010;4(10) doi: 10.1371/journal.pntd.0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf T, et al. Severe Ebola virus disease with vascular leakage and multiorgan failure: treatment of a patient in intensive care. Lancet. 2015;385(9976):1428–1435. doi: 10.1016/S0140-6736(14)62384-9. [DOI] [PubMed] [Google Scholar]
- Wrensch F, et al. Interferon-induced transmembrane protein-mediated inhibition of host cell entry of Ebolaviruses. J Infect Dis. 2015;212(Suppl 2):S210–S218. doi: 10.1093/infdis/jiv255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu W, et al. Ebola virus VP24 targets a unique NLS binding site on karyopherin alpha 5 to selectively compete with nuclear import of phosphorylated STAT1. Cell Host Microbe. 2014;16(2):187–200. doi: 10.1016/j.chom.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan N, Chen ZJ. Intrinsic antiviral immunity. Nat Immunol. 2012;13(3):214–222. doi: 10.1038/ni.2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang ZY, et al. Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injury. Nat Med. 2000;6(8):886–889. doi: 10.1038/78645. [DOI] [PubMed] [Google Scholar]
- Ye L, et al. Ebola virus-like particles produced in insect cells exhibit dendritic cell stimulating activity and induce neutralizing antibodies. Virology. 2006;351(2):260–270. doi: 10.1016/j.virol.2006.03.021. [DOI] [PubMed] [Google Scholar]
- Yen BC, Basler CF. Effects of filovirus interferon antagonists on responses of human monocyte-derived dendritic cells to RNA virus infection. J Virol. 2016;90(10):5108–5118. doi: 10.1128/JVI.00191-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen JY, et al. Therapeutics of Ebola hemorrhagic fever: whole-genome transcriptional analysis of successful disease mitigation. J Infect Dis. 2011;204(Suppl 3):S1043–S1052. doi: 10.1093/infdis/jir345. [DOI] [PubMed] [Google Scholar]
- Yen B, et al. Molecular basis for ebolavirus VP35 suppression of human dendritic cell maturation. J Virol. 2014;88(21):12500–12510. doi: 10.1128/JVI.02163-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoneyama M, et al. Shared and unique functions of the DExD/H-box helicases RIG-I, MDA5, and LGP2 in antiviral innate immunity. J Immunol. 2005;175(5):2851–2858. doi: 10.4049/jimmunol.175.5.2851. [DOI] [PubMed] [Google Scholar]
- Yonezawa A, Cavrois M, Greene WC. Studies of ebola virus glycoprotein-mediated entry and fusion by using pseudotyped human immunodeficiency virus type 1 virions: involvement of cytoskeletal proteins and enhancement by tumor necrosis factor alpha. J Virol. 2005;79(2):918–926. doi: 10.1128/JVI.79.2.918-926.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young DF, et al. Human IFIT1 inhibits mRNA translation of rubulaviruses but not other members of the Paramyxoviridae family. J Virol. 2016 doi: 10.1128/JVI.01056-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki SR, et al. A novel immunohistochemical assay for the detection of Ebola virus in skin: implications for diagnosis, spread, and surveillance of Ebola hemorrhagic fever. Commission de Lutte contre les Epidemies a Kikwit. J Infect Dis. 1999;179(Suppl 1):S36–47. doi: 10.1086/514319. [DOI] [PubMed] [Google Scholar]
- Zhang AP, et al. Crystal structure of Marburg virus VP24. J Virol. 2014 doi: 10.1128/JVI.03565-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zampieri CA, et al. The ERK mitogen-activated protein kinase pathway contributes to Ebola virus glycoprotein-induced cytotoxicity. J Virol. 2007;81(3):1230–1240. doi: 10.1128/JVI.01586-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang D, Zhang DE. Interferon-stimulated gene 15 and the protein ISGylation system. J Interferon Cytokine Res. 2011;31(1):119–130. doi: 10.1089/jir.2010.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z, et al. Drug repurposing to target Ebola virus replication and virulence using structural systems pharmacology. BMC Bioinform. 2016a;17:90. doi: 10.1186/s12859-016-0941-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao D, et al. The Myeloid LSECtin is a DAP12-coupled receptor that is crucial for inflammatory response induced by Ebola virus glycoprotein. PLoS Pathog. 2016b;12(3):e1005487. doi: 10.1371/journal.ppat.1005487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, et al. Zinc-finger antiviral protein inhibits HIV-1 infection by selectively targeting multiply spliced viral mRNAs for degradation. Proc Natl Acad Sci U S A. 2011;108(38):15834–15839. doi: 10.1073/pnas.1101676108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zumbrun EE, et al. Development of a murine model for aerosolized ebolavirus infection using a panel of recombinant inbred mice. Viruses. 2012;4(12):3468–3493. doi: 10.3390/v4123468. [DOI] [PMC free article] [PubMed] [Google Scholar]