Figure 1.
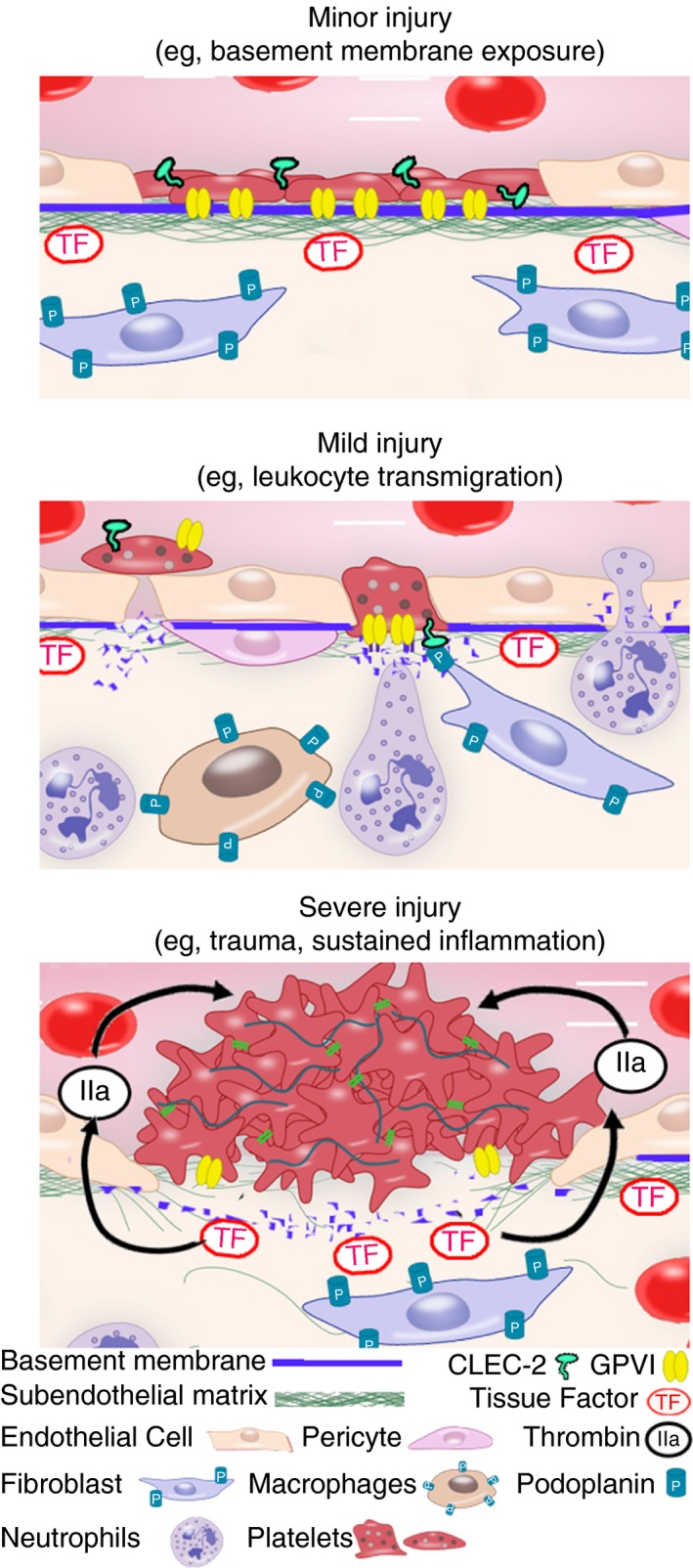
Platelets can maintain vascular integrity in multiple ways depending on the type and severity of vascular injury. Upper panel: The early work of Hans R. Baumgartner showed that in case of minor injury restricted to the endothelial layer (e.g, endothelial denudation, vasodilatation, and opening of endothelial junctions), platelets adhere and spread over the exposed basement membrane acting as “bouche‐trou”, either individually or through the formation of a nonthrombogenic “pseudo‐endothelium” in wider areas of denuded basement membrane. Notably, the adhesion of platelets to the exposed subendothelial matrix is collagenase‐sensitive, indicating a possible role for platelet/collagen interactions, and thus for GPVI, in this function. Middle panel: Recent and early studies indicate that, in case of mild injury where the basement is damaged (e.g, by neutrophil infiltration during acute inflammatory reactions), platelets seal vascular breaches by filling endothelial gaps and/or bridging endothelial junctions over areas of basement membrane disruption. Platelet GPVI contributes to the recruitment and adhesion of platelets to these sites. Engagement of platelets through CLEC‐2 by podoplanin‐expressing cells in direct vicinity of blood vessels (e.g, fibroblasts and inflammatory macrophages) provides a backup mechanism in the absence of GPVI. Lower panel: In a more classical view of hemostasis, in case of severe injury like in trauma or sustained inflammatory reactions, the exposure of the deeper layers of the vessel wall and/or of tissues surrounding vessels leads to thrombin generation and full platelet activation, thereby triggering platelet aggregation through integrin αIIbβ3
