Advanced chronic kidney disease (CKD; Stage G4+) affects only 0.5% of the population, but results in a high burden of morbidity and mortality and an increased risk of multiple adverse events.1, 2 Patients with this severe level of decline in kidney function suffer from multiple biochemical and physiological abnormalities, and relationships between conventional risk factors and renal and cardiovascular outcomes may be altered in this population.3
There are 3 important competing outcomes that affect patients with advanced CKD at disproportionately high rates. These include kidney failure requiring dialysis or transplantation, cardiovascular events requiring hospitalization, and all-cause death.1 As expected, younger patients with advanced CKD tend to progress to kidney failure, whereas very old individuals often die before developing symptoms of kidney failure requiring dialysis.4 However, for other risk factors, such as blood pressure, the relationship may be more complex.5 Understanding these relationships, and how they differ for each risk factor and outcome, may be important for clinical decision making and patient-provider communication.4
As an example, a patient with CKD Stage 4 and multiple risk factors for cardiovascular events and death before dialysis, and reduced risk for progression to kidney failure, may benefit preferentially from optimization of cardiac risk, including interventional and surgical procedures, at the potential expense of kidney function, which may decline from intervention-related acute kidney injury.6 In contrast, patients with a very high risk of CKD progression to kidney failure, and a low risk of cardiovascular or all-cause mortality, may prefer medical management for cardiovascular risk factors.
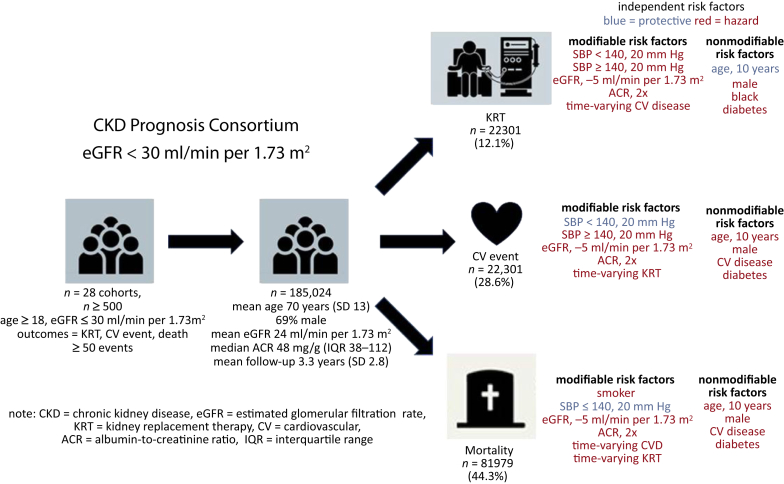
In this issue of Kidney International Reports, Dr. Evans and colleagues from the CKD Prognosis Consortium7 explore in detail the relationships of traditional risk factors with outcomes in advanced CKD, and highlight key differences in risk estimates for kidney failure and the competing CKD outcomes of cardiovascular events and death. The authors studied more than 185,000 individuals with CKD Stage G4+ from 28 cohorts spanning 30 countries. The average age of the participants was 70, and the mean estimated glomerular filtration rate was 24 ml/min per 1.73 m2 and the median urine albumin-to-creatinine ratio was 48 mg/g (Figure 1).
Figure 1.
CKD Prognosis Consortium7: the average age of the participants was 70, the mean estimated glomerular filtration rate was 24 ml/min per 1.73 m2, and the median urine albumin-to-creatinine ratio was 48 mg/g. SBP, systolic blood pressure.
Rates of kidney failure ranged from 1.7% to 30.0%, with 22,301 events occurring over the mean follow-up period of 3.3 years. Cardiovascular and all-cause mortality were more common, and occurred 2 (44,401 cardiovascular events) to 4 (81,979 deaths) times as often as kidney failure. The authors then performed a random-effects meta-analyses of cause-specific hazard ratios for kidney failure and cardiovascular events and Cox proportional hazards model for all-cause mortality. They focused primarily on conventional risk factors (e.g., age, sex, race, history of cardiovascular disease, smoking, blood pressure, diabetes mellitus, estimated glomerular filtration rate, albumin-to-creatinine ratio) and highlighted differences in the relationships between these risk factors and the 3 outcomes of interest.
In particular, male gender, black race, higher albuminuria, lower estimated glomerular filtration rate, and the occurrence of a cardiovascular event during follow-up were strongly associated with kidney failure, whereas older age was not. In contrast, older age, a history of cardiovascular disease or diabetes, and the need for kidney replacement therapy during follow-up were associated with cardiovascular events. For all-cause mortality, the strongest relationships were with older age, smoking, and cardiovascular or kidney failure events during the follow-up period. Importantly, estimated glomerular filtration rate and albuminuria were associated with all 3 outcomes.
Associations were also similar between risk factors and outcomes in subgroups of age; however, diabetes was a stronger risk factor in younger individuals for kidney failure and cardiovascular events. Male gender was more strongly associated with kidney failure in older individuals, and no other risk factors were noted to have differential relationships by age.
Evans and colleagues from the CKD Prognosis Consortium7 present the largest analysis to date evaluating the association between conventional risk factors and important clinical outcomes in advanced CKD. The analysis demonstrates remarkable consistency in the strength of the association despite the diversity of the 28 cohorts, all of which had unique inclusion/exclusion criteria, and differing rates of the individual outcomes. These findings suggest that conventional risk factors are indeed important in patients in advanced CKD, and physicians and patients should work together on risk reduction to potentially avoid these adverse events.
There are, however, some limitations. First, the analysis focused on a limited number of conventional risk factors, some of which are nonmodifiable. Common risk factors, such as low-density lipoprotein cholesterol, were available in only a limited number of cohorts, and as such, definitive conclusions about the relationship between low-density lipoprotein cholesterol and the outcomes of interest could not be drawn. Other more controversial associations, such as ones with body mass index or waist-hip ratio and all-cause mortality, or with cardiac biomarkers, such as troponin and cardiovascular events in advanced CKD, were also not performed.3, 8 In addition, the cohorts, although representative of diverse ethnicities and health systems, did not measure or examine other modifiable factors, such as physical activity and access to care.9, 10 These associations have not been well studied in previous cohorts of advanced CKD, and a definitive study examining these relationships in a large sample size would add to the literature.
It is also important to note that the current study also focused on relative risk, and its findings, when translated to absolute risk, could be used to create predictive models for all 3 adverse outcomes. Validated models exist for kidney failure and all-cause mortality in patients with CKD, but models for cardiovascular events are needed, and could help physicians determine the relative risk/benefit from invasive cardiac procedures that carry a risk of acute kidney injury. An approach incorporating the output from these prediction models in an usable format for physicians who care for these patients could help with clinical decision making.
Future studies should also aim to study some of these risk factors, and examine them and others in patients with CKD Stage 5D, and in subgroups of patients treated with hemodialysis or peritoneal dialysis. There is considerable uncertainty about conventional risk factors in these patients, and a rigorously conducted large multinational study would help improve understanding. Data for the dialysis study could be derived from national dialysis registries, and linkages with administrative data would enable a study evaluating cardiovascular, infectious, and other nonfatal outcomes. Nonetheless, it is important to recognize the present study from the CKD Prognosis Consortium7 as an important contribution, as it definitively establishes the relationship between conventional risk factors and outcomes in patients with advanced CKD.
Disclosure
NT has received consulting fees from Otsuka Inc., Tricida Inc., and AstraZeneca Inc., as well as research support from AstraZeneca Inc. The other author declared no competing interests.
Footnotes
See Clinical Research on Page 625
References
- 1.Go A.S., Chertow G.M., Fan D. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 2.Coresh J., Selvin E., Stevens L.A. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 3.Elsayed E.F., Tighiouart H., Weiner D.E. Waist-to-hip ratio and body mass index as risk factors for cardiovascular events in CKD. Am J Kidney Dis. 2008;52:49–57. doi: 10.1053/j.ajkd.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tangri N., Grams M.E., Levey A.S. Multinational assessment of accuracy of equations for predicting risk of kidney failure: a meta-analysis. JAMA. 2016;315:164–174. doi: 10.1001/jama.2015.18202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Upadhyay A., Earley A., Haynes S.M., Uhlig K. Systematic review: blood pressure target in chronic kidney disease and proteinuria as an effect modifier. Ann Intern Med. 2011;154:541–548. doi: 10.7326/0003-4819-154-8-201104190-00335. [DOI] [PubMed] [Google Scholar]
- 6.James M.T., Tonelli M., Ghali W.A. Renal outcomes associated with invasive versus conservative management of acute coronary syndrome: propensity matched cohort study. BMJ. 2013;347:f4151. doi: 10.1136/bmj.f4151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evans M., Grams M.E., Sang Y. Risk factors for prognosis in patients with severely decreased GFR. Kidney Int Rep. 2018;3:625–637. doi: 10.1016/j.ekir.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bansal N., Hyre Anderson A., Yang W. High-sensitivity troponin T and N-terminal pro-B-type natriuretic peptide (NT-proBNP) and risk of incident heart failure in patients with CKD: the Chronic Renal Insufficiency Cohort (CRIC) Study. J Am Soc Nephrol. 2015;26:946–956. doi: 10.1681/ASN.2014010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walker S.R., Gill K., Macdonald K. Association of frailty and physical function in patients with non-dialysis CKD: a systematic review. BMC Nephrol. 2013;14:228. doi: 10.1186/1471-2369-14-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Komenda P., Lavallee B., Ferguson T.W. The prevalence of CKD in rural Canadian indigenous peoples: results from the First Nations Community-Based Screening to Improve Kidney Health and Prevent Dialysis (FINISHED) screen, triage, and treat program. Am J Kidney Dis. 2016;68:582–590. doi: 10.1053/j.ajkd.2016.04.014. [DOI] [PubMed] [Google Scholar]