Abstract
There are many benefits of online patient access to their medical records through technologies such as patient portals. However, patients often have difficulties understanding the clinical data presented in portals. In response, increasingly, patients go online to make sense of this data. One commonly used online resource is health forums. In this pilot study, we focus on one type of clinical data, laboratory results, and one popular forum, MedHelp. We examined patient question posts that contain laboratory results to gain insights into the nature of these questions and of the answers. Our analyses revealed a typology of confusion (i.e., topics of their questions) and potential gaps in traditional healthcare supports (i.e., patients’ requests and situational factors), as well as the supports patients may gain through the forum (i.e., what the community provides). These results offer preliminary evidence of opportunities to redesign patient portals, and will inform our future work.
Introduction
The clinical data (e.g., laboratory results, clinician notes) contained in medical records have long been a product of, and central to, the interactions that take place between patient and physician in a clinical encounter. These data were traditionally created, updated, and used almost exclusively by physicians. However, research suggests that providing ready access to medical records facilitates patient engagement,1 which can lead to improved health outcomes and reduced costs.2 While patients have had the right to access these records since 1996,3 the process of requesting a paper copy has tended to be prohibitive and, once obtained, can soon become difficult to manage and are easily lost.4 To address these barriers, U.S. health IT policies such as Meaningful Use,5 and initiatives such as OpenNotes,6 have encouraged that patients be given direct, electronic access to their medical records. In response, many healthcare organizations have deployed patient-facing technology, commonly referred to as patient portals, connected to their electronic health record systems. The literature suggests that patient use of these portals may have numerous benefits, including improved quality of patient records,7 home monitoring infrastructure,8 satisfaction with patient-provider communication,9 and health status.10 However, despite these potential benefits, patients have not accessed the portals11 at the rates predicted based on the high level of interest.12 In fact, according to the 2015 U.S. Health Information National Trends Survey, only about 27% of Americans had accessed their health data online, including through patient portals, in the past year.13 Even more concerning is the significant disparities in use found among certain groups, including some minorities,11 adolescents,14 and incarcerated patients.15
So, why has ready access not resulted in more access? According to the literature, a key barrier to realizing the full potential of patient portals is the lack of useful information despite the abundance of data they make available. For example, a recent study found that many patients’ needs for online portals were not just for accessing the data, but for obtaining personalized and actionable knowledge.16 These needs, however, have not been adequately met in the pervasive patient portal design. Relatedly, low health literacy and numeracy, meaning a lower “capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions,”17 can be a barrier to patient portal use.18 Many portals present data to patients in the same or similar way that it is presented to healthcare providers; however, studies have shown that patients may have difficulty understanding medical jargons used in free-text document, such as clinician notes,18 and interpreting quantitative data, such as laboratory results.19 These findings suggest that current patient portals may have been designed at too high of a level of health literacy and numeracy, or do not provide enough, or the right, support to aid patient understanding.
At the same time, there is often not enough time during a clinical encounter to fully meet patients’ needs for knowledge. While it varies by healthcare setting (e.g., primary care, specialty care), there is evidence suggesting that, on average, physicians are spending less time with each patient - from over 20 minutes per patient in 1998, to around 17, or even lower, in 2016.20,21 A related issue is that studies have found that some physicians frequently interrupt patients,22 which may make it difficult for patients to get their questions answered. These factors can also negatively affect the patient-physician relationship,23 which may reduce the likelihood that patients will trust their physician. In sum, while healthcare provider institutions are expanding patients’ access to clinical data through patient portals, this technology often does not adequately meet patients’ knowledge needs, and access to healthcare’s traditional social supports,24 including informational, is shrinking.
Therefore, in order to actually use the available data for personalized decision-making, patients must often tap into supplemental sources of knowledge. Increasingly, this means searching online for general and/or individualized health information.25 In fact, according to one study, 72% of U.S. internet users reported doing this.25 There are, of course, a variety of online resources of varying levels of interactivity and quality from which patients may choose, but health forums have been growing in popularity (e.g. MedHelp.org, CrowdMed26). These forums provide users with a platform to ask their health-related questions, so that others (typically peer patients) can provide assistance.
Among the myriad of patient questions, we were particularly interested in questions accompanied by data that appeared to be directly copied from the individual’s medical record, and pasted into the forum post (or in some instances transcribed; referred to just as copy/paste below). Examples of such data include laboratory results, vital signs, and excerpts from radiology reports and discharge summaries. This content is usually posted publicly, which provides an opportunity for researchers to understand the nature of patients’ questions about their clinical data. This offers direct evidence of comprehension issues, as well as additional forms of support that may be needed. Similarly, the nature of the answers to these questions, especially those that patients find useful, point towards the supports those patients may gain through the forum discussions. While the insights from these analyses may have broader implications for patient-provider communication channels, in this study, we focused on their opportunities to improve patient portal design to better meet patients’ needs.
In this study, we preliminarily assessed the feasibility of this approach by focusing on a particular type of clinical data, laboratory results, which are widely available and frequently viewed in patient portals,18 a common source of questions,27 and tend to be easier to identify in question posts. Similarly, we focused on MedHelp (medhelp.org), which is one of the most popular online health forums.
Methods
Dataset:
All questions and threaded replies from MedHelp were downloaded in September 2016. This dataset contains over 2 million questions and over 8 million answers posted by over 2 million unique users on numerous health conditions (e.g., diabetes, asthma) and health-related topics (e.g., healthy recipes). Question posts on MedHelp are very diverse; for example, patients may present symptoms and/or laboratory results in order to determine whether a clinic visit is necessary, and/or request emotional support during a stressful time (see Figure 1).
Figure 1.
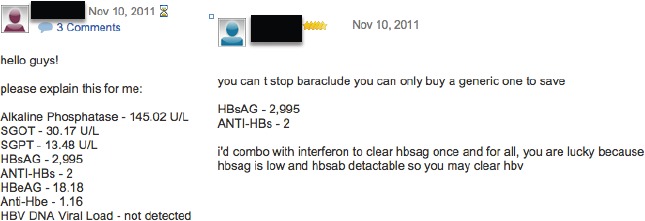
Screenshot of a MedHelp forum post illustrating the copied/pasted laboratory results. Response to question superimposed and outlined in blue.
Identifying Potentially Relevant Posts:
Before we could address our research objective - to understand the nature of question posts containing laboratory results that seem to be copied/pasted from medical records, and their threaded replies - we first needed to identify relevant posts. We did this in four steps.
The goal of Step 1 was to iteratively develop a list of keywords, and determine the number of posts containing copied/pasted laboratory results (relevant posts) returned by each. To do this, we utilized the live MedHelp website. Specifically, for each keyword (e.g., “lab result help”), we reviewed the first 90 posts (3 pages) of the results to (a) count the number of relevant posts; and (b) examine the “Related Questions” section for additional keywords to test.
Since it is difficult to develop a comprehensive list of keywords, and missing keywords could result in missing relevant posts, in the second step, we sought to identify features (patterns) that distinguish relevant posts from other posts. To do this, we translated the three keywords with the highest number of relevant posts (“Lab,” “Blood work,” and “Profile”), and their common alternative spellings, into three queries in the Indri Query language.28 The final queries were run against an inverted index built over all MedHelp question posts. We then manually reviewed the retrieved results to identify the patterns indicative of copying/pasting (e.g., specific test name plus numeric result, such as TSH 0.11). During the review of the last 100 results (a total of 600 were reviewed), no additional general patterns were found, suggesting theoretical saturation had been reached.29
In Step 3, we encoded the identified patterns as regular expressions in Python v2.7. These regular expressions were tested against the annotated corpus created in the second step, and iteratively refined until at least 80% recall was achieved - i.e., if there are 100 relevant posts in the annotated corpus, at least 80 are retrieved.
In the fourth step, we applied the final regular expressions to the entire dataset, which returned 64,922 potentially relevant question posts - matched a pattern indicative of laboratory results copied/pasted from medical records.
Analyses:
We generated an initial random sample of 1,000 of the potentially relevant question posts, and then retrieved all their peer replies. At least two research assistants independently (1) reviewed posts for relevance, and (2) analyzed relevant posts, using a qualitative content analysis approach,3” until no new information was emerging (theoretical saturation).29 In addition, where possible, a “satisfactory” response(s) was identified based on the feedback of the person posting the original question (e.g., “Thanks for info explains a lot.”), and the codes assigned to these posts were eventually compared to the codes assigned to posts not identified as “satisfactory” responses. The content analysis team met weekly to discuss and merge category/theme lists; all disagreements were resolved through discussion. Importantly, if we had not reached theoretical saturation29 after reviewing all posts in the initial sample, we would have repeated this procedure until we reached theoretical saturation.
For (1), question posts were determined to be irrelevant, and therefore excluded, if they did not contain any laboratory results, or contained results that were not from the individual’s medical records (e.g., from a scientific study). Of the 400 question posts reviewed before theoretical saturation, 146 were relevant and, therefore, further analyzed (in 2). Likewise, when reviewing the threaded replies to relevant question posts, any duplicate posts or posts not attempting to answer the original question (e.g., using the thread to ask their own related questions) were excluded. Of the 500 reply posts reviewed before saturation was reached, 417 were eligible for further analysis (in 2), including 289 answers to questions and 128 replies from the original question poster.
Results
Question Posts
The reviewed sample of posts contained an average of 2.1 questions per post, with a range of zero questions (e.g., just providing an update) to six. Questions covered laboratory results not pertaining to any specified conditions, as well as to a wide range of identifiable conditions or concerns, including sexually transmitted infections (e.g., herpes); heart-related concerns (e.g., hypercholesterolemia); liver conditions (e.g., hepatitis); kidney and pulmonary function; hormone imbalances (e.g., testosterone); cancers (e.g., breast); and autoimmune (e.g. lupus) and thyroid disorders (e.g., hyperthyroidism). Furthermore, while some posts included questions exclusively about the laboratory results, many asked about laboratory results in the context of their medical history and/or symptoms. We present the results of this analysis in three sub-sections: Topics, Requesting, and Situational factors.
Topics: While some posts included questions pertaining to more than one topic, most (˜71%) focused on one of the following topics: diagnosis/cause, management/treatment, laboratory report, test/diagnostic, risk, and prognosis (see Table 1). In addition, sub-topic categories emerged as more specific descriptors of patients’ questions. In this sample, questions were most commonly about medications, symptoms, and next steps. For example, the subject line of one post reads, “Please tell me what to do next.” In the body of this post, it becomes evident that she is requesting help “…pulling this [relevant medical history, laboratory test results, symptoms, etc.] info together…” in order to get a step closer to identifying the cause of her symptoms. Less common sub-topics include effect of treatment (e.g., potential adverse effect), comorbidities (i.e., existing diagnoses), timing (e.g., how far apart treatments should be), risk behavior (e.g., alcohol use with certain conditions), and life-style (i.e., diet and exercise).
Table 1.
Topics of copying/pasting question posts, and representative quotations.
| Topics | Representative quotation |
|---|---|
| Diagnosis/Cause | “I am VERY afraid that hypercal. is being caused by malignancy, but the Endo. is not worried…” |
| Management/Treatment | “What should my Armour thyroid dose be? Do I need a T3 level? Should I also be on Cytomel…dose to start?” |
| Laboratory report | “What language would you expect to find in a report for a patient who has not been previously diagnosed with cancer via biopsy?” |
| Test/Diagnostic | “… To my knowledge it [Immunophenotype test] would get a stain of the cells in the sample and look for antibodys for HPV…and if it found some it would try to find the type or strain?” |
| Risk | “I have been advised to do RAI therapy, and told that if the uptake is the same, that the nodule will be the only area affected, but that there is a 10% chance of the whole thyroid being affected and the possibility of my going hypothyroid over the following year(s).” |
| Prognosis | “…Just received my week 6 results.HCV RNA PCR Taqman 2.0<25 IU/ml detected.This was after 4 weeks with SOC and an additional 2 with BOC added. Is it looking good that I will beat this monster?” |
Requesting: Several categories emerged describing what patients were requesting with their post to the MedHelp community; specifically, patients requested opinion, advice, generic information, emotional support, and personal experience (see Table 2). Requests for opinions and advice were by far the most common in this sample. Those requesting opinions tended to provide their laboratory results and, often, relevant medical history and symptoms, and ask the community to interpret it in some way (e.g., likely diagnosis). Those requesting advice were asking for actionable opinions, and a sub-set of these were asking for the community’s assistance in deciding between two or more, often treatment-related, options. In addition, less frequently, posters requested information that was not necessarily personalized to them; for instance, one patient wrote, “Looking for information about chest aches/pain…” Others included language indicative of distress, fear (e.g., “I am terrified”), or other emotions, and were categorized as requesting emotional support. Finally, some posters explicitly invited other patients to share personal experiences so that they could learn from them.
Table 2.
Categories describing what patients are requesting, and representative quotations.
| Requesting | Representative quotation |
|---|---|
| Opinion | “Now after showing these results to the doctor he simply increased my dosage of thyroxine sodium to 100mcg once a day.Can u please give me second opinion.” |
| Advice | “Would you recommend more testing?” |
| Decision support | “I’m vascillating between having the rt breast re excised & await the biopsy results - Or just having a mastectomy w/o awaiting any further test results. Your advice is welcomed!!!” |
| Information (generic) | “what treatments are available?” |
| Emotional support | “I am really upset now to think I have something really wrong with me” |
| Personal experience | “I’d like to hear others experiences so I can better understand all this.” |
Situational factors: Two main situational factors emerged; specifically, (1) whether patients are posting prior to discussing their results with a healthcare provider or after, and (2) whether they have a diagnosis or not. These situational factors, as well as sub-categories and representative quotations, are summarized in Table 3.
Table 3.
Situational factor categories and sub-categories with representative quotations.
| Situational factors | Representative quotation |
|---|---|
| Healthcare - Pre-consultation | |
| Waiting | “… Can’t get doctors appointment for 2 months. Any of your doctors have an ideas?????????” |
| Preparing for appointment | “… We r going to the Endo on Monday - what do I ask?” |
| Determining if need medical follow-up | “… She not nor am I a beliver in follow up visits unless something is wrong.” |
| Healthcare - Post-consultation | |
| Second opinion | “I have been talking to another doctor. Can you tell me what you think?” |
| Clarification/explanation | “… My MD stopped the Armour Thyroid. He also said the elevated T3 can have the same sxs as hypothyroidism. I’ve read alot, but I still don’t understand how?…” |
| Doctor does not know | “… Although my numbers look OK I am still very tired… Doctors unsure of why or what to do.” |
| Options | “…I have a choice whether I want to go back on PegIntron. or Pegasys.” |
| Diagnosis status | |
| Diagnosed: Not questioned | “new labs, Im still so frustrated. This is 2.5 grains of erfa and 6.25 mg of levo. A little better but still not good. I met with the pharmacist and my doctor last week.” |
| Diagnosed: Questioned | “The drs office said my results were great, but I dont think thats right. Does this not suggest I am borderline in hyper or hypo?… My doctor is insisting I am depressed.” |
| Not diagnosed | “My husband has an abnormal bloodn test. could you let me know what could be his diagnosis?” “For quite some time, I have had a number of “issues” and have not gotten to the bottom of it.” |
When it was possible to identify the motivation, patients posting questions prior to a healthcare consultation (also referred to as pre-consultation) did so for several reasons, namely waiting, preparing, and determining the need for an appointment. Many patients were waiting for an appointment with their physician, which often was not for several months, but wanted answers or to take action now. These posts tended to exhibit language indicative of distress (as described above). Others were preparing for their upcoming appointment - trying to obtain information that they could utilize in their consultation. In one such post, the patient wrote, “My doctor is very easy to work with but endocrinology is not his specialty (Family Practice). Please provide what information I would need to share with my dostor for any changes/revisions in my current medication.” Still others were trying to understand their results in an effort to determine if they needed to make an appointment with a physician at all.
Similarly, patients posted questions about their laboratory results to Medhelp after discussing them with their physician (also referred to as post-consultation) for variable reasons, including seeking a second opinion, clarification/explanation, answers or a way forward when their physician is at a loss (referred to as ‘Doctor does not know’ in Table 3), and assistance in making a decision when they have been offered options. In this sample, seeking a second opinion was by far the most common reason for post-consultation posts - patients wanted another opinion on their physician’s interpretations and/or recommendations. In many cases, patients seem to doubt, disagree with, dislike, feel uncomfortable with, or mistrust their physician or their physician’s conclusions. In other cases, they received conflicting opinions (e.g., from different specialists). Other patients just wanted clarification or explanation of information that they discussed with their physician. For example, in one post the patient stated, “I asked questions, but I did not understand what deciding factor determines continuing. treatment.” On the other hand, some patients reported that their physician did not know what their results meant or what to do next. Often these patients were still experiencing bothersome symptoms, and they seemed to be seeking fresh ideas. Finally, some patients’ physicians had given them options, and they were struggling to make a decision.
Finally, three different diagnosis statuses were identified in the reviewed posts - diagnosed: not questioned, diagnosed: questioned, and not diagnosed (See examples in Table 3). Some patients posting questions had a diagnosis that they did not question (at least in the post), and were instead often questioning management/treatment aspects, prognosis, or another aspect. On the other hand, some patients had been diagnosed by their physician, but had doubts as to whether that was indeed the issue, and as such often asked diagnosis questions in their post. Finally, there were patients that did not have a diagnosis, and then this tended to be the focus of their post as well. Some were receiving abnormal test results for the first time, and others had been searching for a diagnosis for a while.
Answers
In this sample, there were an average of 2.0 replies per question post, with a range of 0 to 16. The replies that addressed the original question poster provided information, advice/suggestions, opinion, emotional support, and personal experience (See Table 4). They also requested more information from the question poster.
Table 4.
Answers to copying/pasting question posts themes, and representative quotations.
| Providing | Representative quotation |
|---|---|
| Information | |
| Diagnosis/cause | “There are many possible causes. Fatty liver, alcohol related liver disease, problems with the bile ducts are among the common cuses for these elevations.” |
| Tests/Testing | “In addition to fluctuations in actual VL. the actual method of testing being done can produce different actual counts. Hence the sensitivity threshold at which they can measure.” |
| Potential seriousness/risk | “This condition does not have any serios sequela.” |
| Prognosis | “The disease at this point is generally incurable.” |
| Management/Treatment | “Cortisone creams are often prescribed for the patches of red, dry skin but will also leave you at risk for UV exposure in those areas for the rest of your life.” |
| Resources | “. see parathyroid.com for more info on this…” |
| Advice/suggestion | |
| Physician/Medical professional | “Followup with your personal physician is essential.” |
| “Get a new, decent doc who understands the difference between IBS and post-gallbladder problems.” | |
| Addressing/treating health concern | “Take the Statin. It reduces the chance of having a heart attack even in people with normal cholesterol. And your LDL is high.” |
| Further testing | “I’d push for hormonal testing - cortisol and deficencies.” |
| More information | “Arm yourself with as much information as possible and make an informed decision.” |
| Opinion (First or Second) | |
| Primary concern | “I would think your experience of dealing with Narcolepsy, which is awful by the way, should be the primary concern here.” |
| Interpreting test results | “The low PTH suggests that the high Ca++ initially discovered was “non-parathyroid” origin but if it were a malignancy the Ca++ would typically be on the further rise.” |
| Possible/likely diagnosis/cause | “You have positive antibodies (autoimmune thyroid disease) - most likely this is early Hashimoto’s.” |
| Prognosis | “I think you’re going to beat it, yes I do and I haven’t seen anyone relapse yet who has taken the triple therapy.” |
| Risk/seriousness | “Personally I would feel better if your CRP were also in the first quartile of risk (low risk <1.0). facts are you have a high LDL cholesterol and a level of CRP that is above the lowest risk group.” |
| Management/Treatment | “I think Vit D treatment is fine as long as Ca++ is monitored closely.” |
| Emotional support | “it just makes sooooo angry when docs act like that.I know if it were them feeling bad they would take the med!!” |
| Personal experience | “I have Geno 1A and also 1B and two doctors insisted on Intron.But again it’s probably personal perspective.” |
Information: The MedHelp community provided information on a number of topics, including diagnosis/cause, tests/testing, potential seriousness/risk, prognosis, management/treatment, and resources. More specifically, answers provided information on how a diagnosis is made, common symptoms associated with particular diagnoses, and common causes of abnormal test results and/or symptoms. In addition, information on tests/testing was offered, such as the reliability and accuracy of testing methods, reliability of different laboratory values (e.g., TSH), different options for tests, whether tests are invasive and any required preparations (e.g., fasting), and generally what laboratory results mean. Some answers also included information on potential seriousness/risk and prognosis. Furthermore, the community provided information on management/treatment, including general treatment approach for a given condition (e.g., “… doctors typically just monitor it, no real treatment needed. “), goals of treatment (e.g., management, cure), explaining or comparing options, treatment safety/risk, and new treatment options. Finally, answers offered social support and informational resources (e.g., pointing to websites or other MedHelp posts).
Advice: Answers also provided advice/suggestions related to physician/medical professional, addressing/treating health concern, further testing, and more information. Many reply posts suggested that question posters discuss their questions, and information provided by the community, with their physician. They also sometimes recommended that the question poster see a specialist, get a second opinion, or get a new doctor all together. In addition, the community provided advice/suggestions on addressing/treating health concerns, including whether or not treatment is needed, specific types of medication and dosages to try, changes in medication and/or dosage, suggestions for how to proceed with treatment (e.g., timing), and diet and supplementation recommendations. Some answers also recommended additional tests that they feel the question poster should consider. Finally, many answers suggested that the question poster get more information, including by using search engines, going to sites/resources that they felt were particularly helpful, and asking lots of questions of their physician.
Opinion: In addition, community members provided first and second opinions on topics, including primary concern, interpreting test results, possible diagnosis/cause, seriousness/risk, prognosis, and management/treatment. In cases where people had comorbidities or multiple pieces of information that conflicted, some answers provided opinions on the priority; for example, one community member said, “You’re focusing too much on the test results and not enough on how you are feeling.” The community also provided interpretations of laboratory results, often including their opinion on possible or likely diagnosis/cause or prognosis given their interpretation of the results (and symptoms and history, when provided). Finally, answers provided opinions on management/treatment such as whether they think a proposed treatment is appropriate, treatment (often, medication) and/or dosage they feel would be better, and the best way to make treatment decisions for a given issue (e.g., certain laboratory value).
Emotional Support: Replies from the community also provided emotional support through empathizing, encouraging, offering well wishes and congratulations, reassuring, showing concern or caring, and by indicating that the question poster is not alone - others have felt or experienced the same. Many of these were responding to posts where there was language indicative of distress (as discussed above) or another emotion (e.g., cautious excitement); therefore, whether it was bad news (e.g., tests are positive for a certain condition) or good (e.g., tests indicate the poster is pregnant), most responded in an emotionally supportive way (e.g., “Don’tgive up!“). In addition, even if the question poster did not appear to explicitly request emotional support, answers would often still provide it.
Personal Experience: Answers provided personal experiences in order to offer reassurance, or another type of emotional support, as well as to provide information, opinions, or advice. They tended to use their experience to support a claim or recommendation. For example, one community member wrote, “I didn’t hear a heartbeat until i was 10 weeks.So… try not to worry too much.” While another answer provided the following support for her suggestion that the problem may be pulmonary, “I just had 4 days of intense fatigue and being short of breath. It wasn’t until the chest ache and coughing kicked in that I realized it was my asthma being a brat.”
More Information: Finally, community members often asked follow-up questions and requested that the question poster provide more or updated information. Such replies suggest that, given the information provided, they could not help or would be able to help more with additional information.
Sufficient answers: The replies determined to be “sufficient answers,” based on the reply from the original question poster, suggested that the question poster felt somewhat reassured or relieved, perceived themselves to have an improved understanding, and/or that they had or were going to take a recommended action. The largest number of “sufficient answers” were in reply to thyroid- and liver-related questions; however, “sufficient answers” were identified in threads related to infectious diseases, pregnancy, autoimmune disorders, cancer, and unknown condition. “Sufficient answers” more commonly provided opinion and emotional support, and more specifically tests/testing information, as well as concern/caring and encouragement emotional support.
Discussion
The results of this study provide evidence that it is feasible to identify and characterize the nature of patients’ questions related to laboratory results, and to characterize the nature of the answers to these questions. Specifically, they revealed (1) a typology of patient confusion when viewing laboratory results, (2) patients’ social support needs, (3) the contexts of questions, as well as (4) the type of support that patients may gain, and find ‘satisfactory,’ from peers in online health forums. Similar categories have emerged from studies in the human-computer interaction and patient portal literature, beyond laboratory results and outside of peer-to-peer settings, suggesting that our findings are robust. However, our study had several unique aspects - including, a “target-rich” source of actual patient information and knowledge needs across multiple types of health conditions, and the classification of answers, which few studies have previously done - that resulted in a more thorough typology and novel findings. While our results are preliminary, they suggest potential opportunities to improve patient portals to better meet patients needs.
First, we found a typology of patient confusion about their laboratory results, which includes topics such as management/treatment. Although others have identified similar categories, their typologies were not as comprehensive. For example, when analyzing secure messages sent via a portal, Sun et al., found similar categories of questions aimed at patients’ healthcare teams, but we identified categories, such as risk, that they did not. 31 We were likely able to more comprehensively identify types of patient questions because of our rich dataset, which uniquely situates this study to add to the current understanding of the types of patient questions related to their clinical data. For example, compared to Sun et al.’s study,31 we may have identified more clinical topics, because many patients seek information online first.13,16 In fact, Wright et al. reported that patients were much more likely to search the internet after viewing their problem list through a patient portal, rather than contacting their healthcare provider.32 As our results suggest, after searching online, some of these individuals may believe that there is no need to, or may choose not to, follow-up with their physician.
Second, we observed that patients had social support needs, such as informational, that they tried to meet through the forum. Other studies have reported similar categories; for example, Sillence et al. analyzed advice solicitation in an online breast cancer support group, and identified five patterns, (1) requesting advice, (2) requesting opinion or information, (3) disclosing a problem(s), (4) announcing a plan of action, and (5) asking “anyone in the same boat?”33 Despite small differences, the overlap, as well as the fact that we identified our categories across a number of conditions, indicates robustness, and that our results may be relevant beyond this study setting and population.
Third, while other studies have peripherally reported situational factors, it emerged as a central theme in our study. For example, Powell et al. reported motivations for online information seeking, including perceived barriers to traditional information sources, as well as to seek reassurance, a second opinion, and a greater understanding.34 In addition, this study also found that most online health information seeking was associated with consultations, either in preparation for or to find additional information afterwards.34 In the context of our study, there appears to be some differences in the types of questions asked based on situational factors. We are in the process of extending this work by developing a model of the different health information needs in different situations.
Finally, while there is literature characterizing “best answers” on question and answer websites,e.g.,35 to the best of our knowledge, our attempt to examine peer answers that patients perceive to be satisfactory in an online health forum is novel. The results of this pilot suggest that answers perceived to be “sufficient” by patients more often included opinion and emotional support, and they usually provided more specific information on tests and testing, as well as concern/caring and encouragement emotional support. This may be because these elements were better aligned with what question posters were requesting. In terms of the emotional support, it may also be that when answers showed concern/caring or offered encouragement, it elicited more positive responses from the question poster, regardless of whether it actually helped them gain a better understanding of their situations. Our future work will seek a more complete picture of the types of answers that patients find helpful and the underlying reasons.
Implications: These results provide preliminary evidence of opportunities to improve patient portal design. In terms of content, as discussed above, patients often search online first and may not follow-up with their healthcare provider; therefore, it is crucial to provide more of the information and knowledge that patients need at the point of viewing their laboratory results in patient portals. This could reduce the time and effort burdens often inherent in seeking medical information in the vast internet and, at the same time, ensure that they are consuming, and making decisions based on, accurate information carefully curated by their healthcare professionals. One way to provide more of the information patients needs may be better understanding differences in information needs based situational factors, which could offer an opportunity to provide more personalized content in patient portals, based on elements that are often available (e.g., appointment date). In terms of features, since patients tend to seek these social supports in online communities, it suggests that they may be lacking in patient portals and their healthcare encounters, which could present opportunities for additional patient portal features. For example, supporting patients desire for personal stories from patients “in the same boat,” by allowing patients to opt-in to a social feature that enables finding similar patients and/or more fluid groupings based on similar information needs, could be beneficial.
Limitations: There are several limitations to this work. First, the emphasis was to comprehensively identify relevant themes and categories emerging from this rich dataset; therefore, posts were not double coded. Future work will include more quantitative analysis, and validation of qualitative findings. Second, while it is possible to identify posts with indicators that the original question poster perceived the answer to be helpful, there were a relatively large number of answer posts to which the original question poster did not reply. In addition, there may be other factors, independent of perceived usefulness of the answer, that affect how someone responds, including personality, culture, and level of emotional distress. Therefore, the results related to “sufficient answer”’ should be interpreted with caution, and warrant further investigation. Finally, in this pilot we focused on one type of clinical information and one online health forum. While there is support in the existing literature that these are crosscutting categories; however, the extent to which these results extend beyond this study setting is unclear. Based on the results of this pilot, in our future work, we intend to include the other, harder to identify and less frequently available types of clinical information (e.g., discharge summaries and clinical notes), as well as other online health forums.
Despite these limitations, this work provides direct evidence of patients’ comprehension issues related to their laboratory data. The results also highlight the types of supports they need, and the type that they are able to gain, and deem ‘satisfactory,’ through online health forums. This knowledge directly informs how patient portals can better provide social supports for patients. Finally, this study provides a foundation for our future efforts, including collaborating with patient portal stakeholders (e.g., patients, developers, administrators) to assess how this study, and follow-up studies, can be incorporated into the design and redesign processes to improve patient portals.
Conclusion
This pilot study provides evidence for the feasibility of (1) identifying online forum posts containing patients’ laboratory results copied/pasted from their medical record; (2) identifying question topics, patient support needs, and situational factors; and (3) characterizing what patient peers are providing and requesting in response. An extension of this work is currently underway, and will characterize the similarities and differences in information needs based on context. In addition, the results presented in this paper provide a foundation for future quantitative work involving computational methods. Ultimately, this line of work may lead to improving the design of patient portals, and the way that we present clinical data to patients. Such improvements may, eventually, lead to more patients being engaged in their healthcare and, as a result, improved health status and reduced costs.
References
- 1.Skipper J. Individuals’ Access to Their Own Health Information. The Office of the National Coordinator for Health Information Technology; 2012. [Google Scholar]
- 2.Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter? Res Brief. 2008;(8):1–9. [PubMed] [Google Scholar]
- 3.Office for Civil Rights. The HIPAA Privacy Rule. Published; 2008. May 7, [Accessed February 22, 2017]. HHS.gov. https://www.hhs.gov/hipaa/for-professionals/privacy/index.html. [Google Scholar]
- 4.O’Flaherty S, Jandera E, Llewellyn J, Wall M. Personal health records: An evaluation. Arch Dis Child. 1987;62(11):1152–1155. doi: 10.1136/adc.62.11.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare. Meaningful Use Stage 2. Published; 2014. [Accessed April 14, 2015]. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Stage_2.html. [Google Scholar]
- 6.What is OpenNotes?: OpenNotes. [Accessed April 14, 2015]. http://www.myopennotes.org/about-opennotes/
- 7.Hanauer DA, Preib R, Zheng K, Choi SW. Patient-initiated electronic health record amendment requests. J Am Med Inform Assoc JAMIA. 2014;21(6):992–1000. doi: 10.1136/amiajnl-2013-002574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar RB, Goren ND, Stark DE, Wall DP, Longhurst CA. Automated integration of continuous glucose monitor data in the electronic health record using consumer technology. J Am Med Inform Assoc JAMIA. 2016;23(3):532–537. doi: 10.1093/jamia/ocv206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin C-T. Providing a Web-based Online Medical Record with Electronic Communication Capabilities to Patients With Congestive Heart Failure: Randomized Trial. J Med Internet Res. 2004;6(2) doi: 10.2196/jmir.6.2.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lau M, Campbell H, Tang T, Thompson DJS, Elliott T. Impact of Patient Use of an Online Patient Portal on Diabetes Outcomes. Can J Diabetes. 2014;38(1):17–21. doi: 10.1016/j.jcjd.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171(6):568–574. doi: 10.1001/archinternmed.2011.34. [DOI] [PubMed] [Google Scholar]
- 12.Wen K-Y, Kreps G, Zhu F, Miller S. Consumers’ perceptions about and use of the Internet for personal health records and health information exchange: Analysis of the 2007 Health Information National Trends Survey. J Med Internet Res. 2010;12(4):e73p.1–e73p.16. doi: 10.2196/jmir.1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Health Information National Trends Survey (HINTS) 4, Cycle 4. National Cancer Institute; 2015. [Accessed June 1, 2016]. http://hints.cancer.gov/ [Google Scholar]
- 14.Anoshiravani A, Gaskin GL, Groshek MR, Kuelbs C, Longhurst CA. Special requirements for electronic medical records in adolescent medicine. J Adolesc Health Off Publ Soc Adolesc Med. 2012;51(5):409–414. doi: 10.1016/j.jadohealth.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Gaskin GL, Longhurst CA, Anoshiravani A. Internet access and attitudes toward online personal health information among detained youth. Pediatrics. 2012;130(5):914–917. doi: 10.1542/peds.2012-1653. doi: [DOI] [PubMed] [Google Scholar]
- 16.Alpert JM, Krist AH, Aycock RA, Kreps GL. Applying multiple methods to comprehensively evaluate a patient portal’s effectiveness to convey information to patients. J Med Internet Res. 2016;18(5) doi: 10.2196/jmir.5451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nielsen-Bohlman L, Panzer AM, Kindig DA. Introduction. National Academies Press (US); 2004. [Accessed September 19, 2016]. Literacy I of M (US) C on H http://www.ncbi.nlm.nih.gov/books/NBK216033/ [PubMed] [Google Scholar]
- 18.Sarkar U, Karter AJ, Liu JY, et al. The literacy divide: Health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of Northern California (DISTANCE) J Health Commun. 2010;15(SUPPL. 2):183–196. doi: 10.1080/10810730.2010.499988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gee PM, Paterniti DA, Ward D, Miller LMS. e-Patients perceptions of using personal health records for selfmanagement support of chronic illness. CIN - Comput Inform Nurs. 2015;33(6):229–237. doi: 10.1097/CIN.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 20.Mechanic D, McAlpine DD, Rosenthal M. Are patients’ office visits with physicians getting shorter? N Engl J Med. 2001;344(3):198–204. doi: 10.1056/NEJM200101183440307. [DOI] [PubMed] [Google Scholar]
- 21.Peckham C. Medscape Physician Compensation Report 2016: Minutes Personally Spent with Each Patient. [Accessed February 23, 2017];2016 Apr 1; Published http://www.medscape.com/features/slideshow/compensation/2016/public/overview#page=26. [Google Scholar]
- 22.Rhoades DR, McFarland KF, Finch WH, Johnson AO. Speaking and interruptions during primary care office visits. Fam Med. 2001;33(7):528–532. [PubMed] [Google Scholar]
- 23.Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999;14(S1):S34–S40. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wills TA. In: Social Support and Health. San Diego: CA: Academic Press; 1985. Supportive functions of interpersonal relationships; pp. 61–82. [Google Scholar]
- 25.Health Fact Sheet. Pew Research Center’s Internet & American Life Project. [Accessed April 14, 2015]. http://www.pewinternet.org/fact-sheets/health-fact-sheet/
- 26.Meyer AND, Longhurst CA, Singh H. Crowdsourcing Diagnosis for Patients With Undiagnosed Illnesses: An Evaluation of CrowdMed. J Med Internet Res. 2016;18(1):e12. doi: 10.2196/jmir.4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zikmund-Fisher BJ, Exe NL, Witteman HO. Numeracy and literacy independently predict patients’ ability to identify out-of-range test results. J Med Internet Res. 2014;16(8):e187. doi: 10.2196/jmir.3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.INDRI. [Accessed March 8, 2015]. http://www.lemurproject.org/indri/
- 29.Conrad CF. A Grounded Theory of Academic Change. Sociol Educ. 1978;51(2):101. doi: 10.2307/2112242. [DOI] [Google Scholar]
- 30.Mayring P. Qualitative Content Analysis. Forum Qual Sozialforschung Forum Qual Soc Res. 2000;1(2) [Google Scholar]
- 31.Sun S, Zhou X, Denny JC, Rosenbloom T, Xu H. Understanding patient provider communication entered via a patient portal system. Proc ASISTAnnu Meet. 2012;49(1) [Google Scholar]
- 32.Wright A, Feblowitz J, Maloney FL, et al. Increasing patient engagement: patients’ responses to viewing problem lists online. Appl Clin Inform. 2014;5(4):930–942. doi: 10.4338/ACI-2014-07-RA-0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sillence E. Giving and receiving peer advice in an online breast cancer support group. Cyberpsychology Behav Soc Netw. 2013;16(6):480–485. doi: 10.1089/cyber.2013.1512. [DOI] [PubMed] [Google Scholar]
- 34.Powell J, Inglis N, Ronnie J, Large S. The Characteristics and Motivations of Online Health Information Seekers: Cross-Sectional Survey and Qualitative Interview Study. J Med Internet Res. 2011;13(1) doi: 10.2196/jmir.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harper FM, Raban D, Rafaeli S, Konstan JA. Vol. 865. In: ACM Press; 2008. Predictors of answer quality in online Q&A sites. [DOI] [Google Scholar]


