Abstract
Objective: Both infected subdural hematoma (ISH) and Edwardsiella tarda infections are rare in humans. E. tarda is a motile, facultative anaerobic, gram-negative rod bacterium, which is isolated from fresh or brackish water, but not usually from humans. Extra-intestinal E. tarda infections are rare and might cause severe clinical symptoms. However, ISH caused by E. tarda has not been reported previously. We report the first case of ISH due to E. tarda.
Patient: A 76-year-old man was admitted to our hospital with a headache, loss of appetite, and nausea. Computed tomography revealed bilateral subdural hematoma.
Results: We performed burr hole drainage. A hematoma with pus was found on the left side and chronic hematoma was found on the right side. Consequently, we diagnosed him with ISH on the left side and chronic subdural hematoma on the right side. E. tarda was detected in a culture from the hematoma with pus on the left side. As postoperative antibiotic therapy, we administered ceftriaxone and metronidazole for 47 days. The patient was discharged with no residual neurological deficit.
Conclusion: Our case implied that favorable outcomes can be obtained by drainage and appropriate antibiotic therapy for ISH caused by E. tarda.
Keywords: Infected subdural hematoma, subdural empyema, chronic subdural hematoma, Edwardsiella tarda
Introduction
Reports on both infected subdural hematoma (ISH) and Edwardsiella tarda infection in humans are rare. E. tarda is a motile, facultative anaerobic, gram-negative rod bacterium. It is not a resident bacterium in humans. Thus, it is rare that E. tarda is isolated from humans, as opposed to fresh or brackish water environments. E. tarda rarely causes extra-intestinal infections, which might cause severe clinical outcomes in humans. In bacteremia with liver cirrhosis, the mortality is high1). In contrast, ISH due to E. tarda is unknown to our knowledge. We report our case because favorable outcomes were obtained by burr hole drainage and antibiotic therapy.
Patient
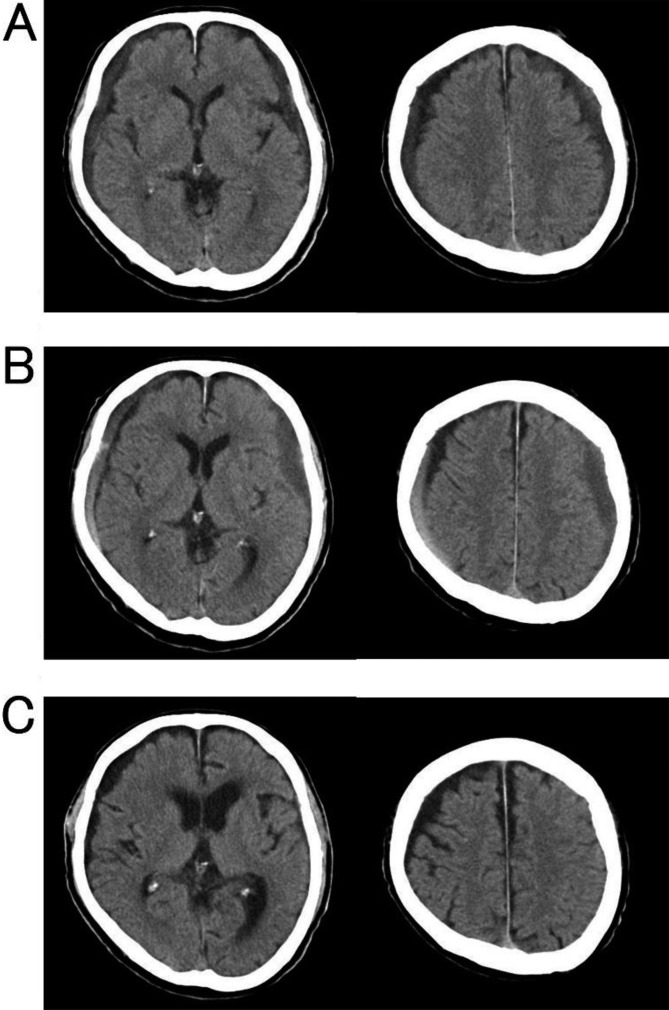
A 76-year-old man presented with only a headache. He had a previous history of common bile duct stones (CBDSs). The travel and dietary history of the patient was unremarkable. He was alert and had no abnormal neurological findings. Computed tomography (CT) revealed thin bilateral chronic subdural hematoma (CSDH) (Figure 1A). He underwent follow-up throughout the clinical course. His headache developed gradually, and worsened to include loss of appetite and nausea. He was admitted to our hospital 20 days after the first visit. He was disoriented (Glasgow Coma Scale score, 14), had right hemiparesis (manual muscle testing score=4), and had a body temperature of 36.2°C. His white blood cell count was 11800/mm3 and serum C-reactive protein levels were 18.92 mg/dL on admission. Follow-up CT revealed that the left subdural effusion had increased slightly (Figure 1B). The follow-up pre-operative diagnosis was progressing CSDH because there were few indications of infection, although the laboratory data indicated elevated inflammation markers. Pre-operative magnetic resonance imaging was not performed because pre-operative diagnosis and indications for surgical treatment were determined based on neurological signs and CT findings. Therefore, we performed burr hole drainage and found hematoma with pus on the left side (Figure 2) and chronic hematoma on the right side. Consequently, he was diagnosed with ISH on the left side and CSDH on the right side. E. tarda was detected in a culture of the hematoma with pus using a MicroScan WalkAway 40 Plus instrument with the Neg Combo EN 1J panel (Beckman Coulter K.K., Tokyo, Japan). No significant findings were detected in the cultures from the hematoma on the right side or from blood. The detected E. tarda was susceptible to most antibiotics. As postoperative antibiotic therapy, we administered ceftriaxone (4 g/day in two divided doses) and metronidazole (1.5 g/day in three divided doses) for 47 days.
Figure 1.
Computed tomography at the first visit (A), admission (B), and 37 days after operation (C). (A) Bilateral chronic subdural hematoma. (B) The left subdural hematoma increased slightly. (C) The left infected subdural hematoma and right chronic subdural hematoma almost disappeared.
Figure 2.
Hematoma with pus evacuated from the left subdural space.
The patient experienced abdominal pain 23 days after admission and was diagnosed with CBDS. A gastroenterologist in our hospital performed endoscopic retrograde cholangiopancreatography. Simultaneously, bile was collected and cultured. However, E. tarda was not detected. The patient’s abdominal pain disappeared following CBDS treatment.
The postoperative course went well after antibiotic therapy. CT revealed that the left ISH and right CSDH almost disappeared 37 days after operation (Figure 1C). The patient became ambulatory and was discharged with no residual neurological deficit.
Discussion
Gastroenteritis is caused by E. tarda, which is isolated from stool samples, after consuming freshwater fish or eels. In contrast, extra-intestinal infections with E. tarda, such as liver abscess, biliary tract infection, bacteremia, skin and soft tissue infection, tubo-ovarian abscess, and meningitis, are rare. In particular, patients with E. tarda infection are more likely to have a history of underlying hepatobiliary disease or an immunocompromised host, and the mortality of patients with E. tarda bacteremia with liver cirrhosis is high1, 2). In our case, the patient with ISH due to E. tarda also had CBDS as a disease of the hepatobiliary system, consistent with previous reports1, 2). To our knowledge, five reports have been published previously detailing intracranial E. tarda infection: four cases of meningitis3,4,5,6) and one case of multiple brain abscess7). Three of the four patients with E. tarda meningitis died early after onset, whereas the fourth had a good recovery. The patient with E. tarda brain abscess also had a good recovery (Table 1).
Table 1. Summary of six cases of intracranial Edwardsiella tarda infection.
| Author, Year | Age | Sex | Disorder | Treatment | Outcome |
|---|---|---|---|---|---|
| Sonnenwirth et al., 19683) | 31-year-old | F | meningitis | – | D |
| Okubadejo et al., 19684) | neonate | F | meningitis | antibiotics (CP, PC, SM, sulphadiazine) | D |
| Sachs JM et al., 19745) | 17-year-old | M | meningitis | antibiotics (ABPC) | GR |
| Vohra et al., 19886) | neonate | F | meningitis | antibiotics (GM, PC) | D |
| Takeuchi et al., 20097) | neonate | F | brain abscess | drainage, V-P shunt, antibiotics (ABPC, CTX, MEPM) |
GR |
| Our case, 2017 | 76-year-old | M | infected subdural hematoma | burr hole drainage, antibiotics (CTRX, MNZ) |
GR |
ABPC: ampicillin, CP: chloramphenicol, CTX: cefotaxime, CTRX: ceftriaxone, D: dead, F: female, GM: gentamicin, GR: good recovery, M: male, MEPM: meropenem, MNZ: metronidazole, PC: penicillin, SM: streptomycin, V-P shunt: ventriculoperitoneal shunt.
Only 47 cases of ISH have been reported in the literature8). In our case, the infectious routes for ISH are unclear because neither the existence of infectious sites except for ISH nor the detection of the pathogen in blood cultures were found. However, we suspect that E. tarda infected the membrane of CSDH hematogenously based on the following reasons. First, both left ISH and right CSDH existed concurrently. Second, the left subdural effusion observed using CT changed with time. Finally, the patient had no history of open head injury or local extensions from paranasal sinusitis or otitis. It is also unclear how E. tarda entered the patient’s body because he denied eating suspicious food or contacting any E. tarda habitat environments before his admission.
No established procedure for ISH treatment exists because of the rarity of the disease, various conditions of patients with ISH, and differential pathogens in each case. However, operation for the drainage and administration of appropriate antibiotics are commonly selected treatments for ISH. The selection of burr holes or craniotomy as the surgical treatment remains controversial. Otsuka et al.9) reported no significant difference between burr hole and craniotomy for ISH outcomes. In contrast, Dabdoub et al.8) reported that craniotomy should be the initial method for surgical drainage because recurrence rates in the burr hole surgery group were higher than those in the craniotomy group in adults. However, we think that the choice of craniotomy for ISH is not always ideal because surgical treatment depends on patient characteristics.
Conclusion
Our case implied that favorable outcomes can be obtained from one-time burr hole surgery and appropriate antibiotic therapy for ISH due to E. tarda, although extra-intestinal E. tarda infections might cause severe clinical symptoms.
Conflicts of Interest
All authors report no conflicts of interest concerning this article.
References
- 1.Hirai Y, Asahata-Tago S, Ainoda Y, et al. Edwardsiella tarda bacteremia. A rare but fatal water- and foodborne infection: Review of the literature and clinical cases from a single centre. Can J Infect Dis Med Microbiol 2015; 26: 313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang IK, Kuo HL, Chen YM, et al. Extraintestinal manifestations of Edwardsiella tarda infection. Int J Clin Pract 2005; 59: 917–921. doi: 10.1111/j.1742-1241.2005.00527.x [DOI] [PubMed] [Google Scholar]
- 3.Sonnenwirth AC, Kallus BA. Meningitis due to Edwardsiella tarda. First report of meningitis caused by E. tarda. Am J Clin Pathol 1968; 49: 92–95. doi: 10.1093/ajcp/49.1.92 [DOI] [PubMed] [Google Scholar]
- 4.Okubadejo OA, Alausa KO. Neonatal meningitis caused by Edwardsiella tarda. BMJ 1968; 3: 357–358. doi: 10.1136/bmj.3.5614.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sachs JM, Pacin M, Counts GW. Sickle hemoglobinopathy and Edwardsiella tarda meningitis. Am J Dis Child 1974; 128: 387–388. [DOI] [PubMed] [Google Scholar]
- 6.Vohra K, Torrijos E, Jhaveri R, et al. Neonatal sepsis and meningitis caused by Edwardsiella tarda. Pediatr Infect Dis J 1988; 7: 814–815. doi: 10.1097/00006454-198811000-00018 [DOI] [PubMed] [Google Scholar]
- 7.Takeuchi H, Fujita Y, Ogawa H, et al. Multiple brain abscesses in neonate caused by Edwardsiella tarda: case report. Neurol Med Chir (Tokyo) 2009; 49: 85–89. doi: 10.2176/nmc.49.85 [DOI] [PubMed] [Google Scholar]
- 8.Dabdoub CB, Adorno JO, Urbano J, et al. Review of the management of infected subdural hematoma. World Neurosurg 2016; 87: 663.e1–663.e8. doi: 10.1016/j.wneu.2015.11.015 [DOI] [PubMed] [Google Scholar]
- 9.Otsuka T, Kato N, Kajiwara I, et al. A case of infected subdural hematoma. No Shinkei Geka 2007; 35: 59–63 (in Japanese, Abstract in English). [PubMed] [Google Scholar]