Abstract
Indoor smoking bans have often been associated with reductions in smoking prevalence. However, few studies have evaluated their association with within-person changes in smoking behaviors. We linked longitudinal data from 5,105 adults aged 18–30 years at baseline from the Coronary Artery Risk Development in Young Adults (CARDIA) Study (1985–2011) to state, county, and local policies mandating 100% smoke-free bars and restaurants by census tract. We used fixed-effects models to examine the association of smoking bans with within-person change in current smoking risk, smoking intensity (smoking ≥10 cigarettes/day on average vs. <10 cigarettes/day), and quitting attempts, using both linear and nonlinear adjustment for secular trends. In models assuming a linear secular trend, smoking bans were associated with a decline in current smoking risk and smoking intensity and an increased likelihood of a quitting attempt. The association with current smoking was greatest among participants with a bachelor’s degree or higher. In models with a nonlinear secular trend, pooled results were attenuated (confidence intervals included the null), but effect modification results were largely unchanged. Findings suggest that smoking ban associations may be difficult to disentangle from other tobacco control interventions and emphasize the importance of evaluating equity throughout policy implementation.
Keywords: fixed-effects models, smoke-free policies, smoking, smoking bans, tobacco use
Cigarette-smoking–related diseases result in approximately 480,000 deaths per year in the United States (1), and an estimated 15% of US adults smoked in 2015 (2). In recent years, many states have implemented policies restricting smoking indoors in public places, including restaurants and bars. Between 1998 and 2012, 30 states enacted 100% smoke-free laws covering both bars and restaurants (3, 4). Numerous county-level and local bans, often preceding state-level bans, have also been implemented (5).
Many prior repeat cross-sectional studies found that smoking prevalence declined after implementation of a smoking ban (6–13). Prior studies also found positive associations of smoking bans with smoking intensity (reductions in the average number of cigarettes smoked per day ranging from −0.6 to −3.7) (6–10, 12, 13). However, not all studies have found associations between bans and individual smoking behavior (14, 15), and in a recent systematic review, Frazer et al. (16) concluded that evidence of smoking ban effects on smoking prevalence and intensity at the national, state, or local level was inconsistent.
Most prior studies have used repeated cross-sectional surveys to assess population-level changes in smoking behavior from before implementation of a smoking ban to after implementation of the ban (6, 8, 11, 13, 14, 17). While this approach provides important information on the public health impact of these policies, it is also of interest to examine associations of smoking bans with within-person changes in smoking behavior. Longitudinal cohort study designs are well suited to evaluate within-person change in smoking behavior, yet relatively few prior studies have used these designs. Past longitudinal cohort studies have largely focused on occupational cohorts of hospitality workers rather than the general population (18–21). Two recent studies linked up to 10 years of data from the National Longitudinal Survey of Youth with state, county, and local smoking ban policies and found that smoking bans were negatively associated with current smoking and smoking intensity among adolescents/young adults (22, 23). However, neither examined associations of bans with quitting attempts or whether associations differed by sex or socioeconomic status (SES). It is important to examine potential differences in associations with smoking bans by SES or sex because smoking disproportionately affects persons of lower SES and men (1). Several prior studies have suggested that smoking bans may have a stronger association with smoking among men (9, 10, 12, 24) and people of higher SES (8, 25); however, results have been mixed (26, 27).
The objective of this study was to assess the association of 100% bans (i.e., no exceptions) on smoking in bars and restaurants with changes in individual-level smoking risk, intensity, and quitting attempts in a large cohort of young to middle-aged adults from multiple regions of the United States in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. We hypothesized that exposure to smoking bans would be associated with reduced smoking risk and intensity and increased likelihood of engaging in a quitting attempt. We further hypothesized that associations would be stronger in men than in women and in persons with higher educational attainment and household income compared with lower education and income.
METHODS
Study population
The CARDIA Study is an ongoing longitudinal cohort study evaluating the evolution of risk factors for cardiovascular disease from young adulthood to middle age (28). The study has currently accrued 30 years of follow-up over the course of 9 examinations. A total of 5,115 black and white men and women aged 18–30 years were enrolled from 4 cities (Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California). The baseline examination was conducted in 1985/1986, and follow-up examinations were conducted after 2, 5, 7, 10, 15, 20, 25, and 30 years. Data for these analyses included those from 1985–2011, corresponding to examination years 0, 7, 10, 15, 20, and 25, as information on participant’s residential address was collected in these years. We excluded participant examination years in which the participant was pregnant (n = 116 examination years (0.4%)) or missing data on smoking status (n = 162 examination years (0.6%)). We included a total of 23,572 person-examinations from 5,105 participants (data were structured such that individuals had 1 record per examination) in the analyses. The CARDIA Study protocol was approved by the institutional review boards at each participating institution.
Smoking outcomes
Smoking outcomes were self-reported at each examination and included smoking status, smoking intensity, and quitting attempts. Smoking status was assessed by means of 2 questions: 1) “Have you ever smoked cigarettes regularly for at least 3 months? By regularly, we meant at least 5 cigarettes per week, almost every week” (ever smoking) and 2) “Do you still smoke cigarettes regularly?” (current smoking). We compared current smokers with non–current smokers in analyses. Smoking intensity was assessed by asking current smokers, “How many cigarettes do you smoke per day on average?”. In smoking intensity analyses, we included participants who had ever reported current smoking during follow-up, and we considered the number of cigarettes smoked to be 0 in examination years where ever smokers reported not currently smoking. We dichotomized this variable at ≥10 cigarettes/day (half a pack, and the mean number smoked per day at baseline) and <10 cigarettes/day to examine differences in heavy smoking. Attempts to quit smoking were assessed by asking current smokers, “Have you made any attempts to stop smoking in the past [number of years since the last examination] years?”
Smoking ban exposures
Data on smoking bans were obtained from the American Nonsmokers’ Rights Foundation’s Local Ordinance Database (3), which compiled a comprehensive data set of the dates of all state, county, and city-level 100% smoking bans implemented in the United States from 1990 to 2014 and whether each ban prohibited smoking in restaurants, bars, and/or other workplaces. To be considered a 100% smoke-free policy, legislation had to ban smoking in attached bars and separately ventilated rooms and not have exemptions based on size.
CARDIA participants’ home addresses were geocoded in examination years 0, 7, 10, 15, 20, and 25. Participants’ state/county/census tract Federal Information Processing Standards codes were converted to census place names (roughly equivalent to city boundaries) using the Missouri Census Data Center’s MABLE/Geocorr Geographic Correspondence Engines for the 1980, 1990, 2000, and 2010 census years (29). Place names and state/county Federal Information Processing Standards codes were linked to state, county, and local-level smoking bans in the American Nonsmokers’ Rights Foundation database, and exposure status was assigned on the basis of participant examination date. In order to ensure that policy changes preceded outcome measurement, we considered participants exposed as of 12 months following implementation of a ban. When a participant’s census tract encompassed multiple municipalities or unincorporated areas where ban status differed (0.2% of person-examinations), participants were assigned an exposure probability ranging from 0 to 1 reflecting the proportion of the tract population residing in municipalities with a ban, according to the most recent census. Smoking ban data were complete for all participants.
To be considered exposed, participants had to live in an area with both restaurant and bar smoking bans. This combined exposure was chosen because, for 97% of observations, exposures to bar bans and exposures to restaurant bans were the same. Nonhospitality workplace bans overlapped with hospitality (bar and restaurant) bans in 95% of observations; however, we focused on hospitality bans only, because survey data indicated that many nonhospitality establishments had voluntarily banned indoor smoking by the late 1990s, far in advance of legislation banning smoking in nonhospitality workplaces (30). We compared participants exposed to 100% hospitality smoking bans with those exposed to less than 100% bans (including weak bans or no bans) because prior research indicates that 100% smoking bans have a stronger association with smoking behavior and health outcomes than weaker bans (16, 31, 32).
Covariates
We included sex and race and the following time-varying covariates: age (years), education (continuous, representing the number of years of education participants had attained), marital status (married/living in a marriage-like relationship vs. not), employment status (unemployed vs. not), living with children (yes or no), and current alcohol use (yes or no). Information on total annual family income was collected as a 9-level ordinal variable and converted to a continuous variable using the average dollar value for each category. Because averages could not be calculated for the lowest (<$5,000) and highest (>$100,000) income categories, we assigned values of $2,500 and $150,000 to those categories. Incomes were translated to year 2000 US dollars using the Consumer Price Index (33). While the other covariates were assessed at each examination, income information was not collected until year 5. We carried back year 5 income to impute income in year 0, which resulted in 834 missing values for year 0.
In addition, monthly state-level tax rates were obtained from The Tax Burden on Tobacco (34) and were translated to 2,000 US dollars. We also included fixed effects for state of residence to control for area-level differences in smoking norms. State was used rather than county because 53% of counties had only 1 participant at a given examination; thus, the county-level effect could not be separated from the participant effect.
Statistical analysis
We conducted multiple imputation by chained equations (35) using the MI package in Stata (StataCorp LP, College Station, Texas) to impute missing covariate values (≥1 covariate missing for 5.9% of person-examination years; data assumed to be missing at random). This approach, also known as sequential regression multivariate imputation (36), is a method with fully conditional specification of prediction equations that can accommodate arbitrary missing-value patterns and handle multiple types of variables. Following guidance for imputation of longitudinal data (35, 37, 38), we reformatted the person-period data set to have 1 row per person in order to simultaneously include all analytical variables from all examinations, so that individuals’ responses for a given variable at other time points as well as other variables were used to impute missing values. We created 10 imputed data sets. Imputed values were dropped for examinations participants did not actually complete. We compared the distributions of covariates between the original and imputed data sets and found them to be similar (see Web Table 1, available at https://academic.oup.com/aje).
In order to examine the association of smoking bans with within-person change in individual smoking behavior, we used longitudinal models with repeated measures for each examination and participant-specific fixed effects. Fixed-effects models estimate the association between within-person changes in exposure and within-person changes in the outcome by treating each individual as his/her own control (39). Estimates are then averaged across individuals. Since fixed-effects models inherently control for all observed and unobserved time-invariant characteristics of study participants included in the model, they eliminate the possibility of bias from time-invariant omitted variables (39). Since all 3 outcomes were dichotomous, we used conditional Poisson fixed-effects models with robust variance estimates to model the relative change in risk of each smoking behavior associated with exposure to a smoking ban (40, 41). Poisson estimation with robust variance was chosen over logistic regression because odds ratios may provide biased estimates of relative risk when the outcome is not rare (40). Fixed-effects models use only within-person variation and include only participants who have had a change in the outcome over the course of follow-up; as such, the analytical sample varied by outcome (current smoking: n = 1,732 participants and 8,290 person-examinations; smoking intensity: n = 1,197 participants and 5,694 person-examinations; quitting attempts: n = 1,153 participants and 4,430 person-examinations). We clustered standard errors by individual (additional detail on statistical models is provided in Web Appendix 1).
Covariates
Models included the following time-varying covariates: age, education, marital status, employment status, income, alcohol use, living with children, state cigarette tax rate, state fixed effect, and time since baseline. Time-invariant covariates (race, sex, and study site) were not directly specified because fixed-effects models only estimate coefficients for time-varying variables; however, we included interactions between time-invariant variables and time where significant (P < 0.05), to allow the association of these variables with outcomes to vary over time.
Time trend
Preliminary graphical assessments (adjusted for covariates) showed an approximately linear time trend for smoking rates; thus models included time since baseline as a linear term. Nevertheless, to provide more robust control for secular trends based on departures from linearity (Web Figure 1), we added a quadratic term for time (time squared) to our models for current smoking and smoking intensity (where departure from linearity was minor) and a penalized cubic spline for time to our models for quitting attempts (where departure from linearity was stronger). Because associations differed for the main models, we present the results from both sets of models. We found no evidence of temporal nonstationarity (see Web Appendix 2 for details).
Effect modification
We examined effect modification using models that included terms for interaction between potential modifiers (selected a priori: sex, education, income) and smoking ban status. We then calculated stratified risk ratios to examine patterns in different subgroups.
Sensitivity analyses
We conducted several sensitivity analyses. First, we tested sensitivity to the length of the exposure lag period by lagging exposures by 6 months rather than 1 year. Second, to ensure that changes in smoking behavior were not explained by diagnosis of a condition that might necessitate smoking cessation, we added a time-varying indicator for whether participants had been diagnosed with cancer, heart disease, diabetes, or hypertension to the models. Third, we implemented models that considered only exposure to a state-level smoking ban rather than a state, county, or local ban. Fourth, we used a negative binomial hybrid-effects model (39) to estimate the association of smoking bans with within-person change in smoking intensity modeled as a count outcome (see Web Table 2 for details on this model). Fifth, we also estimated sensitivity to adjustment for income using nonlinear parameterization; results are presented in Web Table 2.
RESULTS
Table 1 displays the characteristics of the study sample over 25 years of follow-up. Current smoking prevalence declined from 31% to 17%, and the percentage of ever smokers who smoked at least 10 cigarettes/day declined from 52% to 27%. The proportion of current smokers reporting a quitting attempt decreased from 60% in year 0 to 51% in year 7, and then increased again to 62% at the last follow-up examination. More black participants were lost to follow-up than white participants, and slightly more men than women. Educational attainment and income increased over the course of follow-up, as did the proportion of participants who were married and lived with their children, while alcohol use decreased.
Table 1.
Characteristics of Participants in an Analysis of the Association Between 100% Bans on Smoking in Bars and Restaurants and Within-Person Changes in Smoking Outcomes, CARDIA Study, 1985–2011
| Characteristic | CARDIA Examination Year | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year 0 | Year 7 | Year 10 | Year 15 | Year 20 | Year 25 | |||||||
| No. of Persons | % | No. of Persons | % | No. of Persons | % | No. of Persons | % | No. of Persons | % | No. of Persons | % | |
| All Participants | ||||||||||||
| Total no. of participants | 5,071 | 4,006 | 3,895 | 3,644 | 3,510 | 3,446 | ||||||
| Age, yearsa | 24.8 (3.7) | 32.0 (3.6) | 35.0 (3.7) | 40.2 (3.6) | 45.2 (3.6) | 50.2 (3.6) | ||||||
| Sex | ||||||||||||
| Male | 2,304 | 45 | 1,832 | 46 | 1,748 | 45 | 1,615 | 44 | 1,519 | 43 | 1,503 | 44 |
| Female | 2,767 | 55 | 2,174 | 54 | 2,147 | 55 | 2,029 | 56 | 1,991 | 57 | 1,943 | 56 |
| Race | ||||||||||||
| Black | 2,612 | 52 | 1,940 | 48 | 1,903 | 49 | 1,718 | 47 | 1,633 | 47 | 1,609 | 47 |
| White | 2,459 | 48 | 2,066 | 52 | 1,992 | 51 | 1,926 | 53 | 1,877 | 53 | 1,837 | 53 |
| Education, yearsa | 13.8 (2.3) | 14.5 (2.5) | 14.6 (2.6) | 14.9 (2.5) | 15.0 (2.6) | 15.1 (2.7) | ||||||
| Education category | ||||||||||||
| High school diploma or less | 2,011 | 40 | 1,160 | 29 | 1,144 | 30 | 834 | 23 | 837 | 24 | 771 | 22 |
| Some college/associate’s degree | 1,676 | 33 | 1,216 | 31 | 1,096 | 28 | 1,134 | 31 | 955 | 27 | 957 | 28 |
| Bachelor’s degree or more | 1,384 | 27 | 1,606 | 40 | 1,633 | 42 | 1,665 | 46 | 1,703 | 49 | 1,706 | 50 |
| Unemployed | 1,405 | 28 | 900 | 23 | 814 | 21 | 732 | 20 | 780 | 22 | 1,123 | 33 |
| Married | 1,130 | 22 | 1,737 | 44 | 1,906 | 49 | 2,187 | 60 | 2,194 | 63 | 2,109 | 62 |
| Living with children | 1,355 | 27 | 1,934 | 49 | 2,110 | 55 | 2,174 | 60 | 2,012 | 58 | 1,703 | 50 |
| Annual household income (increments of $10,000)a,b | 5.7 (3.7) | 4.7 (3.0) | 4.9 (2.9) | 6.9 (4.6) | 6.8 (4.3) | 6.3 (4.1) | ||||||
| Current alcohol use | 4,366 | 86 | 3,271 | 82 | 3,092 | 80 | 2,878 | 79 | 2,713 | 79 | 2,676 | 78 |
| Current cigarette smoker | 1,545 | 31 | 1,087 | 27 | 1,001 | 26 | 805 | 22 | 687 | 20 | 597 | 17 |
| Exposure to 100% smoking bansc | ||||||||||||
| Restaurant ban | 0 | 0 | 0 | 0 | 17 | <1 | 923 | 25 | 1,085 | 31 | 2,760 | 80 |
| Bar ban | 0 | 0 | 0 | 0 | 2 | <1 | 916 | 25 | 1,022 | 29 | 2,428 | 71 |
| Participants Who Had Ever Smoked During Follow-up | ||||||||||||
| Total no. of participants | 1,913 | 1,468 | 1,419 | 1,284 | 1,200 | 1,200 | ||||||
| Average no. of cigarettes smoked per daya | 10.6 (9.7) | 9.7 (9.9) | 9.1 (9.1) | 7.7 (9.5) | 6.8 (9.1) | 5.5 (7.8) | ||||||
| Smoking intensity, cigarettes/day | ||||||||||||
| <10 | 922 | 48 | 782 | 53 | 780 | 55 | 812 | 63 | 816 | 68 | 870 | 73 |
| ≥10 | 991 | 52 | 686 | 47 | 639 | 45 | 472 | 37 | 384 | 32 | 330 | 27 |
| Current Smokers | ||||||||||||
| Total no. of participants | 1,545 | 1,087 | 1,001 | 805 | 687 | 597 | ||||||
| Attempt to quit smoking in past (2, 3, or 5) yearsd | 922 | 60 | 549 | 51 | 518 | 52 | 483 | 60 | 431 | 63 | 367 | 62 |
Abbreviation: CARDIA, Coronary Artery Risk Development in Young Adults.
a Values are expressed as mean (standard deviation).
b Household income was converted to year 2000 US dollars using the Consumer Price Index (33).
c Participants were linked to state, county, and city-level smoking ban exposures on the basis of their census tract of residence.
d At baseline, participants were asked about attempts to quit smoking in the past 2 years. At follow-up examinations, quitting attempts since the past examination were assessed (2-year interval for year 7, 3-year interval for year 10, and 5-year intervals for years 15, 20, and 25). Examination years 2 and 5 were not included in this analysis.
At baseline, no participants lived in areas with a 100% hospitality smoking ban (Table 1). Ban coverage increased starting in year 10. By year 25 (2010–2011), 80% of participants lived in areas with 100% restaurant bans and 71% lived in areas with 100% bar bans.
Association of 100% hospitality smoking bans with smoking outcomes
Table 2 presents the results of the main fixed-effects models. In models assuming a linear secular trend, participants who lived in a state, county, or municipality that adopted 100% bans in both bars and restaurants had an 8% reduction in the risk of current smoking (risk ratio (RR) = 0.92, 95% confidence interval (CI): 0.87, 0.98). In addition, bans were associated with an 8% decrease in the risk of smoking ≥10 cigarettes/day (RR = 0.92, 95% CI: 0.83, 1.01) and a 10% increase in the likelihood of a quitting attempt among current smokers (RR = 1.10, 95% CI: 1.02, 1.19). In sensitivity analyses that 1) altered the definition of smoking ban exposure, 2) controlled for diagnosis with a chronic condition, or 3) modeled intensity as a count, results were similar (Web Table 2). In models that included a nonlinear (either quadratic or cubic spline) secular trend, results were largely attenuated, and all confidence intervals included the null value (Table 2).
Table 2.
Association of 100% Hospitality Smoking Bansa With Within-Person Change in Smoking Behaviors, Controlling for Secular Time Trends With Linear and Nonlinear Time Variables, CARDIA Study, 1985–2011b
| Smoking Behavior | No. of Persons | Models Including a Linear Time Trend | Models Including a Nonlinear Time Trend | ||
|---|---|---|---|---|---|
| Adjusted RR | 95% CI | Adjusted RR | 95% CI | ||
| Risk of current smokingc | 1,732 | 0.92 | 0.87, 0.98 | 0.99 | 0.92, 1.06 |
| Smoking intensityd among participants who had ever smoked during follow-up | 1,197 | 0.92 | 0.83, 1.01 | 0.99 | 0.89, 1.10 |
| Quitting attemptse by current smokers | 1,153 | 1.10 | 1.02, 1.19 | 1.04 | 0.94, 1.14 |
Abbreviations: CARDIA, Coronary Artery Risk Development in Young Adults; CI, confidence interval; RR, risk ratio.
a A 100% smoking ban was defined as a ban mandating that all bars and restaurants be completely smoke-free, with no exceptions. Exposure was lagged by 1 year to ensure temporality. Participants were linked to state, county, and city-level smoking ban exposures based on their census tract of residence.
b RRs were estimated using fixed-effects Poisson models with robust variance estimates. Models adjusted for the following time-varying covariates: age, education, marital status, employment status, income, living with children, current alcohol use, state cigarette tax rate, and state of residence. In the first set of models, time since baseline (in years) was included as a linear trend. In the second set of models, time and time squared were included for current smoking and smoking intensity, while restricted cubic splines (6 knots) were used for quitting attempts. Interactions between time-invariant variables (sex and race) and time since baseline were retained for current smoking and smoking intensity to allow the associations of these variables with the outcome to change over time (P for interaction < 0.05). Conditional fixed-effects models included only those participants with a change in the outcome during the follow-up period. Because of concerns about collinearity with the time trend, we also repeated analyses without controlling for age in the model and found estimates to be unchanged.
c Versus not current smoking.
d Average number of cigarettes smoked per day (≥10 cigarettes/day vs. <10 cigarettes/day).
e Any attempt to quit smoking versus no quitting attempts.
Differences in associations among subgroups
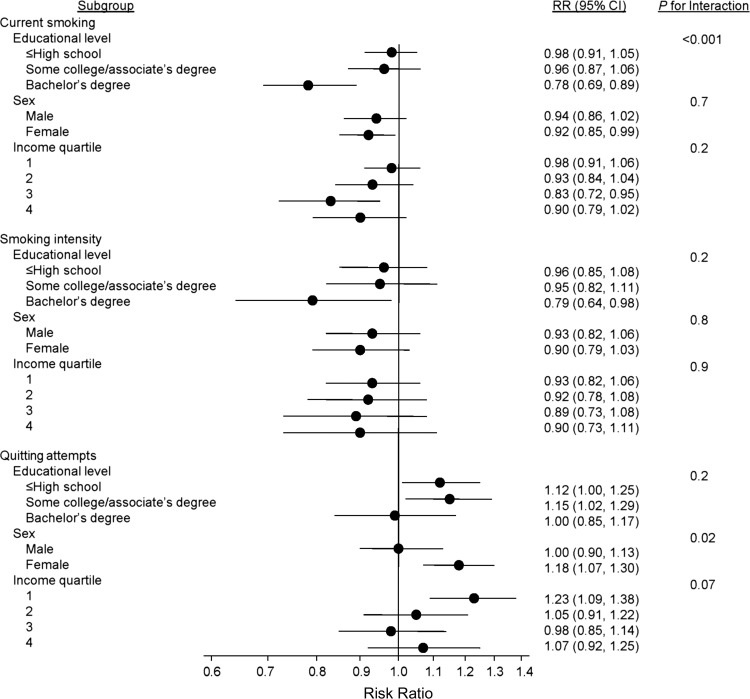
Stratified results suggested that the association of hospitality bans with smoking risk was stronger with higher SES (Figure 1 and Web Table 3). Participants with a bachelor’s degree or more education had a 22% decline in the risk of current smoking (RR = 0.78, 95% CI: 0.69, 0.89) when exposed to a ban, compared with a 4% decline (RR = 0.96, 95% CI: 0.87, 1.06) among those with some college or an associate’s degree and a 2% reduction (RR = 0.98, 95% CI: 0.91, 1.05) among those with a high school diploma or less (P for interaction < 0.001). Smoking bans were associated with the largest reduction in current smoking risk in the 2 highest income quartiles, although the interaction was not statistically significant.
Figure 1.
Association of 100% bans on smoking in bars and restaurants with within-person changes in smoking outcomes, by educational attainment, sex, and income, CARDIA Study, 1985–2011. Risk ratios (RRs) were estimated using fixed-effects Poisson models with robust variance estimates and were adjusted for time-varying covariates: time since baseline (linear trend), age, marital status, employment status, education, income, living with children, current alcohol use, state cigarette tax rate, and state of residence. P values are P’s for interaction between the covariate and hospitality smoking bans. Participants were linked to state, county, and city-level smoking ban exposures on the basis of census tract. Cutpoints for income quartiles (inflation-adjusted values in year 2000 US dollars): quartile 1, ≤$29,086; quartile 2, $29,087–$48,392; quartile 3, $48,393–$83,492; quartile 4, ≥$83,493. Bars, 95% confidence intervals (CIs). CARDIA, Coronary Artery Risk Development in Young Adults.
When smoking intensity was the outcome variable, stratified results suggested that the association with hospitality bans was stronger for higher education (although interaction was not statistically significant), but no differences were observed by income.
Conversely, when quitting attempts was the outcome variable, the association of hospitality bans was stronger with lower SES. The association was strongest among participants in the lowest income quartile (RR = 1.23, 95% CI: 1.09, 1.38; P for interaction = 0.07 (Figure 1, Web Table 3)), and a similar pattern was observed by educational attainment, although the interaction was not statistically significant.
Smoking bans were associated with an increase in quitting attempts among women only (in women, RR = 1.18, 95% CI: 1.07, 1.30; in men, RR = 1.00, 95% CI: 0.90 1.13; P for interaction: 0.02). No patterns were detected by sex for the outcomes smoking risk or intensity.
Results of subgroup analyses were attenuated in models that included a nonlinear time trend, although patterns were similar to those seen in models with a linear secular trend (Web Table 3).
DISCUSSION
Comprehensive bans on smoking in bars and restaurants were associated with a significant decline in individual smoking risk and intensity among young to middle-aged adults over 25 years of follow-up, as well as a significant increase in the likelihood of a quitting attempt under the assumption of a linear secular trend. Bans were associated with the largest reduction in current smoking risk among participants with a bachelor’s degree or higher, were associated with increased quitting attempts among women only, and had a stronger association with quitting attempts among participants with lower household income. The main results were attenuated and nonsignificant when a nonlinear time term was included, although significant associations remained for certain subgroups.
Our findings under the assumption of a linear secular trend are largely consistent with the few prior studies that evaluated associations for smoking bans in longitudinal cohorts. Recent studies that linked the American Nonsmokers’ Rights Foundation database to the National Longitudinal Survey of Youth (22, 23) found that bar bans were associated with lower odds of current smoking and fewer days of smoking by current smokers (23) and that comprehensive bans in bars, restaurants, and nonhospitality workplaces were associated with lower odds of current smoking (22). Our study built on these findings by using a longer follow-up period (over twice the length of prior studies), a large population of young to middle-aged adults, and the ability to link local bans for all participants. In addition, our use of fixed-effects models directly assessed the association of a change in smoking ban exposure with changes in individual-level smoking outcomes, while tightly controlling for any time-invariant unobserved individual covariates (39).
The attenuation of associations upon inclusion of a nonlinear time term suggests that associations of smoking bans with smoking behaviors under an assumption of a linear secular trend may be overestimated. This finding does not necessarily indicate that smoking bans are not associated with smoking behaviors, but rather that their association is difficult to disentangle from that of other simultaneously occurring tobacco control interventions. Smoking bans are often implemented as part of comprehensive tobacco control programs with components including tax increases and educational programs (6, 8, 13). We controlled for cigarette taxes and included state fixed effects to control for time-invariant unmeasured state-level factors and found significant associations. However, the associations estimated in models with linear secular trends may be explained in part by other tobacco control interventions, such as changes in educational messaging and smoking advertisements or other unmeasured secular trends.
Our finding that smoking bans were most strongly associated with current smoking among participants with higher education, which was observed in models with both linear and nonlinear secular trends, is consistent with a systematic review which found that local/regional smoke-free policies often had stronger associations in higher-SES groups (42). Prior studies have found positive associations between education and support for smoke-free policies (43, 44), suggesting that cultural smoking norms may change more quickly among persons with higher education. While smoking bans have been found to change smoking norms (45, 46), within–education-group prosmoking norms may weaken the association of smoking bans among persons with lower educational attainment. In addition, our finding that bans were more strongly associated with quitting attempts (but not with current smoking or intensity) among lower-income individuals suggests that smoking bans promote attempted cessation among people of lower SES but that additional supports may be needed to promote successful cessation in these groups. For example, because lower-SES populations may lack access to smoking cessation aids (47) and may be less likely to use these aids (48), policies that increase access to and support for smoking cessation aids in tandem with hospitality smoking bans may reduce differences based on socioeconomic factors.
This study had several limitations. First, outcomes were assessed by self-report, leading to potential misclassification due to recall or social desirability bias. However, prior validation work in CARDIA that compared self-reported smoking with serum cotinine levels indicated that misclassification of smoking exposure status based on self-reporting was uncommon (misclassification rate: 4.2%) (49). Second, while we included state fixed effects to control for potential geographic differences in smoking norms, we were unable to include county-level fixed effects. Third, we were unable to adjust for state-specific time trends, since most states had few participants living in them at a given time. Fourth, we were unable to control for the presence of antismoking marketing campaigns, as we found no comprehensive database of these campaigns. Fifth, we did not distinguish between daily smokers and persons with less regular smoking patterns, such as social or weekend-only smokers. Sixth, fixed-effects models result in loss of sample size in comparison with other longitudinal methods, as only participants with changes in exposure and outcome contribute to the likelihood. This may have reduced statistical power to detect interactions. Seventh, selection bias may have influenced the results, as black participants were more likely to be lost to follow-up and more likely to smoke and to live in areas without a 100% smoking ban. Following the work of others (22, 23) we compared participants in areas with 100% smoking bans to all others. This approach may have underestimated the magnitude of the association of bans with smoking, since the referent group include persons exposed to weaker bans as well as no bans. Finally, we did not distinguish between participants who lived in an area where a ban was newly implemented and those who moved from an area without a ban to an area with a ban.
In conclusion, adoption of smoking bans in bars and restaurants was associated with a lower risk of current smoking and lower smoking intensity and with a greater likelihood of engaging in a quitting attempt in a longitudinal cohort study of young to middle-aged adults in models assuming a linear secular trend only, indicating potential confounding by unmeasured secular trends. Results underscore the challenge of disentangling associations with bans from associations with other concurrent tobacco control interventions. In addition, weak associations for smoking bans among participants with lower educational attainment emphasize the importance of evaluating equity throughout the policy implementation process and of addressing disparities through policy changes and enhancements when gaps are uncovered.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology and Biostatistics, Dornsife School of Public Health, Drexel University, Philadelphia, Pennsylvania (Stephanie L. Mayne, Amy H. Auchincloss, Loni Philip Tabb); School of Economics, LeBow College of Business, Drexel University, Philadelphia, Pennsylvania (Mark Stehr); Division of Preventive Medicine, School of Medicine, University of Alabama at Birmingham, Birmingham, Alabama (James M. Shikany); Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota (Pamela J. Schreiner, Rachel Widome); and Department of Nutrition, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina (Penny Gordon-Larsen).
The Coronary Artery Risk Development in Young Adults (CARDIA) Study is supported by National Institutes of Health contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute (NHLBI), by the Intramural Research Program of the National Institute on Aging (NIA), and by an intraagency agreement between the NIA and the NHLBI (agreement AG0005). Additional funding was provided by contracts R01HL114091 from the NHLBI, P2CHD050924 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, P30DK56350 from the National Institute of Diabetes and Digestive and Kidney Diseases, and P30ES010126 from the National Institute of Environmental Health Sciences.
All analyses, interpretations, or conclusions reached are those of the authors and not of the National Institutes of Health.
Conflict of interest: none declared.
Abbreviations
- CARDIA
Coronary Artery Risk Development in Young Adults
- CI
confidence interval
- RR
risk ratio
REFERENCES
- 1. Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 2. Jamal A, King BA, Neff LJ, et al. . Current cigarette smoking among adults—United States, 2005–2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1205–1211. [DOI] [PubMed] [Google Scholar]
- 3. American Nonsmokers’ Rights Foundation US Tobacco Control Laws Database. Berkeley, CA: American Nonsmokers’ Rights Foundation; 2017. https://no-smoke.org/materials-services/lists-maps/. Updated January 15, 2015. Accessed November 16, 2017. [Google Scholar]
- 4. American Nonsmokers’ Rights Foundation Overview List—How Many Smokefree Laws?Berkeley, CA: American Nonsmokers’ Rights Foundation; 2017. http://no-smoke.org/wp-content/uploads/pdf/mediaordlist.pdf. Accessed March 28, 2018. [Google Scholar]
- 5. Shipan CR, Volden C. Bottom-up federalism: the diffusion of antismoking policies from US cities to states. Am J Pol Sci. 2006;50(4):825–843. [Google Scholar]
- 6. Coady MH, Jasek J, Davis K, et al. . Changes in smoking prevalence and number of cigarettes smoked per day following the implementation of a comprehensive tobacco control plan in New York City. J Urban Health. 2012;89(5):802–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325(7357):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Frieden TR, Mostashari F, Kerker BD, et al. . Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Am J Public Health. 2005;95(6):1016–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gallus S, Zuccaro P, Colombo P, et al. . Smoking in Italy 2005–2006: effects of a comprehensive national tobacco regulation. Prev Med. 2007;45(2–3):198–201. [DOI] [PubMed] [Google Scholar]
- 10. Gualano MR, Bert F, Scaioli G, et al. . Smoking ban policies in Italy and the potential impact of the so-called Sirchia Law: state of the art after eight years. Biomed Res Int. 2014;2014:293219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hahn EJ, Rayens MK, Butler KM, et al. . Smoke-free laws and adult smoking prevalence. Prev Med. 2008;47(2):206–209. [DOI] [PubMed] [Google Scholar]
- 12. Heloma A, Jaakkola MS. Four-year follow-up of smoke exposure, attitudes and smoking behaviour following enactment of Finland’s national smoke-free work-place law. Addiction. 2003;98(8):1111–1117. [DOI] [PubMed] [Google Scholar]
- 13. Kilgore EA, Mandel-Ricci J, Johns M, et al. . Making it harder to smoke and easier to quit: the effect of 10 years of tobacco control in New York City. Am J Public Health. 2014;104(6):e5–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tauras JA. Smoke-free air laws, cigarette prices, and adult cigarette demand. Econ Inq. 2006;44(2):333–342. [Google Scholar]
- 15. Adda J, Cornaglia F. The effect of bans and taxes on passive smoking. Am Econ J Appl Econ. 2010;2(1):1–32. [Google Scholar]
- 16. Frazer K, Callinan JE, McHugh J, et al. . Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2016;2:CD005992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Messer K, Pierce JP, Zhu SH, et al. . The California Tobacco Control Program’s effect on adult smokers: (1) smoking cessation. Tobacco Control. 2007;16(2):85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Braverman MT, Aarø LE, Hetland J. Changes in smoking among restaurant and bar employees following Norway’s comprehensive smoking ban. Health Promot Int. 2008;23(1):5–15. [DOI] [PubMed] [Google Scholar]
- 19. Larsson M, Boethius G, Axelsson S, et al. . Exposure to environmental tobacco smoke and health effects among hospitality workers in Sweden: before and after the implementation of a smoke-free law. Scand J Work Environ Health. 2008;34(4):267–277. [DOI] [PubMed] [Google Scholar]
- 20. Mullally BJ, Greiner BA, Allwright S, et al. . The effect of the Irish smoke-free workplace legislation on smoking among bar workers. Eur J Public Health. 2009;19(2):206–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Semple S, Maccalman L, Naji AA, et al. . Bar workers’ exposure to second-hand smoke: the effect of Scottish smoke-free legislation on occupational exposure. Ann Occup Hyg. 2007;51(7):571–580. [DOI] [PubMed] [Google Scholar]
- 22. Vuolo M, Kelly BC, Kadowaki J. Independent and interactive effects of smoking bans and tobacco taxes on a cohort of US young adults. Am J Public Health. 2016;106(2):374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Song AV, Dutra LM, Neilands TB, et al. . Association of smoke-free laws with lower percentages of new and current smokers among adolescents and young adults: an 11-year longitudinal study. JAMA Pediatr. 2015;169(9):e152285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cesaroni G, Forastiere F, Agabiti N, et al. . Effect of the Italian smoking ban on population rates of acute coronary events. Circulation. 2008;117(9):1183–1188. [DOI] [PubMed] [Google Scholar]
- 25. Fowkes FJ, Stewart MC, Fowkes FG, et al. . Scottish smoke-free legislation and trends in smoking cessation. Addiction. 2008;103(11):1888–1895. [DOI] [PubMed] [Google Scholar]
- 26. Dinno A, Glantz S. Tobacco control policies are egalitarian: a vulnerabilities perspective on clean indoor air laws, cigarette prices, and tobacco use disparities. Soc Sci Med. 2009;68(8):1439–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thomas S, Fayter D, Misso K, et al. . Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tob Control. 2008;17(4):230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Friedman GD, Cutter GR, Donahue RP, et al. . CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol 1988;41(11):1105–1116. [DOI] [PubMed] [Google Scholar]
- 29. Missouri Census Data Center MABLE/Geocorr12: geographic correspondence engine. Version 1.2. http://mcdc.missouri.edu/websas/geocorr12.html. Accessed November 10, 2015.
- 30. Farrelly MC, Evans WN, Sfekas AE. The impact of workplace smoking bans: results from a national survey. Tob Control. 1999;8(3):272–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Albers AB, Siegel M, Cheng DM, et al. . Effect of smoking regulations in local restaurants on smokers’ anti-smoking attitudes and quitting behaviours. Tob Control. 2007;16(2):101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Carton TW, Darden M, Levendis J, et al. . Comprehensive indoor smoking bans and smoking prevalence: evidence from the BRFSS. Am J Health Econ. 2016;2(4):535–556. [Google Scholar]
- 33. Bureau of Labor Statistics, US Department of Labor Consumer Price Index. 2015. http://www.bls.gov/cpi/data.htm. Accessed July 9, 2015.
- 34. Orzechowski W, Walker RC. The Tax Burden on Tobacco. Arlington, VA: Orzechowski and Walker; 2014. [Google Scholar]
- 35. White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–399. [DOI] [PubMed] [Google Scholar]
- 36. Raghunathan TE, Lepkowski JM, Van Hoewyk J, et al. . A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27(1):85–95. [Google Scholar]
- 37. Allison PD. Missing Data. Thousand Oaks, CA: SAGE Publications; 2001. [Google Scholar]
- 38. Young R, Johnson DR. Handling missing values in longitudinal panel data with multiple imputation. J Marriage Fam. 2015;77(1):277–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Allison PD. Fixed Effects Regression Models. 1st ed Thousand Oaks, CA: SAGE Publications; 2009. [Google Scholar]
- 40. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 41. Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22(6):661–670. [DOI] [PubMed] [Google Scholar]
- 42. Brown T, Platt S, Amos A. Equity impact of population-level interventions and policies to reduce smoking in adults: a systematic review. Drug Alcohol Depend. 2014;138:7–16. [DOI] [PubMed] [Google Scholar]
- 43. Gilpin EA, Lee L, Pierce JP. Changes in population attitudes about where smoking should not be allowed: California versus the rest of the USA. Tob Control. 2004;13(1):38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nagelhout GE, van den Putte B, de Vries H, et al. . The influence of newspaper coverage and a media campaign on smokers’ support for smoke-free bars and restaurants and on secondhand smoke harm awareness: findings from the International Tobacco Control (ITC) Netherlands Survey. Tob Control. 2012;21(1):24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Satterlund TD, Lee JP, Moore RS. Changes in smoking-related norms in bars resulting from California’s Smoke-Free Workplace Act. J Drug Educ. 2012;42(3):315–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Orbell S, Lidierth P, Henderson CJ, et al. . Social-cognitive beliefs, alcohol, and tobacco use: a prospective community study of change following a ban on smoking in public places. Health Psychol. 2009;28(6):753–761. [DOI] [PubMed] [Google Scholar]
- 47. Blumenthal DS. Barriers to the provision of smoking cessation services reported by clinicians in underserved communities. J Am Board Fam Med. 2007;20(3):272–279. [DOI] [PubMed] [Google Scholar]
- 48. Honjo K, Tsutsumi A, Kawachi I, et al. . What accounts for the relationship between social class and smoking cessation? Results of a path analysis. Soc Sci Med. 2006;62(2):317–328. [DOI] [PubMed] [Google Scholar]
- 49. Wagenknecht LE, Burke GL, Perkins LL, et al. . Misclassification of smoking status in the CARDIA Study: a comparison of self-report with serum cotinine levels. Am J Public Health. 1992;82(1):33–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.