Abstract
The objectives of this study were to implement, test adherence to and examine the preliminary effectiveness of a summertime weight-gain prevention intervention in youth from a low-income, Rhode Island community. In 2016, 51 children, ages 6–12 years, participated in a daily, summertime intervention, which offered a minimum of two hours of physical activity programming and free lunch through the USDA's Summer Food Service Program (SFSP). Thirty children from the same community with similar SFSP access served as a comparison group. Height and weight were measured before and at the end of summer to assess change in body mass index z-score (BMIz). Diet and physical activity were assessed midsummer. Multivariate mixed models were used to test group differences in change in BMIz over the summer and weight-related behaviors midsummer. Repeated measures ANOVA was used to examine the relationships of intervention participation with change in BMIz and weight-related behaviors in intervention participants. On average, intervention participants attended 65.6% of program sessions. They lost 0.04 BMIz units, while those in the comparison group gained 0.03 BMIz units (p = 0.07). Midsummer, intervention participants spent 4.6% less time sedentary on weekdays as compared to comparison participants (p = 0.03). Among intervention participants, attendance was significantly associated with change in BMIz (p = 0.01), spending 41 more minutes in moderate to vigorous physical activity (MVPA) (p = 0.004) and 8.5% less time sedentary (p < 0.001). Implementing a summertime obesity prevention intervention in a low-income community is feasible. Despite moderate adherence, preliminary findings suggest that participation in the intervention was associated with reductions in BMIz.
Clinical trials registration
Abbreviations: BMI, Body Mass Index; BMIz, Body Mass Index z-score; GEMS, Girls health Enrichment Multisite Studies; MVPA, Moderate to Vigorous Physical Activity; NDSR, Nutrition Data Systems for Research; PHAST, Promoting Health and Activity in the Summer Trial; SDH, Structured Day Hypothesis; SFSP, Summer Food Service Program; SPARK AS, Sports, Play, and Active Recreation for Kids - After School
Keywords: Childhood obesity, Summer, Low-income, Diet, Physical activity
Highlights
-
•
Implementing a weight gain prevention intervention in the summer is feasible.
-
•
Findings suggest that participation was associated with reductions in BMIz.
-
•
Participants were more active and less sedentary on days they attended the program.
-
•
Preventing summer weight gain may be possible in youth from low-income communities.
1. Introduction
Obesity is common and results in worse health outcomes among those from low-income communities (Centers for Disease Control and Prevention - Division of Community Health, 2013; Schreier and Chen, 2013). Nationally representative data suggest that children from the lowest income households are nearly twice as likely to become obese during childhood as compared to those from wealthier households (Cunningham et al., 2014). A multitude of individual-, family- and community-level contextual factors interact to contribute to this health disparity, including poor diet, physical inactivity, and sedentary behavior, an unhealthy home food environment, limited access to low-cost, nutrient-dense foods, and unsafe neighborhoods that provide few opportunities for physical activity (Schreier and Chen, 2013; Gordon-Larsen, 2004)
Nearly 20% of American youth are obese and >90% of youth are enrolled in schools (U.S. Department of Education, National Center for Education Statistics, 2016). Thus, significant efforts have been made to address children's access to healthy nutrition and physical activity within the school environment (Centers for Disease Control and Prevention, 2014). Despite these efforts, income-related disparities in obesity prevalence continue to widen (Wang et al., 2011; May et al., 2013). Convergent findings from several studies suggest that accelerated summer weight gain may be a significant, unrecognized influence, particularly among youth from low-income households, those of minority backgrounds, and those with overweight or obesity (Economos et al., 2013; von Hippel et al., 2007; von Hippel and Workman, 2016; McCue et al., 2013; Moreno et al., 2013; Baranowski et al., 2014; Franckle et al., 2014; Chen et al., 2016; Moreno et al., 2015).
Whereas the cause of excess summer weight gain is not fully understood, Brazendale and colleagues proposed the “Structured Day Hypothesis” (SDH) (Brazendale et al., 2017) as a potential mechanistic framework. The SDH posits that the structured nature of the school day is protective against obesogenic behaviors in youth, as it provides energy-controlled meals and regular physical activity opportunities. By contrast, the summer has less structure and may provide greater exposure to the home food environment and fewer opportunities for physical activity, particularly for children from low-income communities. The SDH is supported by evidence that physical inactivity, increased screen time, and changes in eating behaviors occur over the summer (Rodriguez et al., 2014; Christodoulos et al., 2006; Tovar et al., 2010). Thus, summer represents an ideal intervention period, one that may have specific implications for addressing income-related health disparities in youth.
Few studies have examined the efficacy of summertime weight gain prevention interventions. As part of a larger study, Baronowski et al. conducted a 4-week summer day camp with 8-year old African American girls. They found no significant differences in BMI between intervention and control groups at the end of the camp (Baranowski et al., 2003). In BOUNCE, a 4-week summertime physical activity intervention for minority girls with overweight or obesity and their mothers, Olvera and colleagues found a significant 15 min increase in daily moderate to vigorous physical activity (MVPA) and a significant decrease in BMI (0.65 kg/m2) (Olvera et al., 2010; Olvera et al., 2013a). Similarly, after a 4-week summer physical activity intervention with adolescent, minority females, Bohnert et al. found that participants engaged in an additional 26 min of MVPA (p < 0.001) (Bohnert et al., 2014). These interventions successfully impacted weight or weight-related behaviors(Olvera et al., 2010; Olvera et al., 2013a; Bohnert et al., 2014); however, they included a single sex, were of brief duration (4-weeks), and only one included a comparison group (Baranowski et al., 2003). Therefore, to fully appreciate the potential of summertime weight gain prevention interventions, studies are needed that include both sexes, last the duration of the summer, and include a comparison group.
The Promoting Health and Activity in the Summer Trial (PHAST) was a pilot study designed to assess the implementation and preliminary effectiveness of a summertime weight gain prevention intervention in a diverse, low-income community. The intervention was a daily camp-like summer program for children, ages 6–12 years, which provided physical activity programming and lunch through the USDA's Summer Food Service Program (SFSP). Using a quasi-experimental design, the primary aim of the study was to develop, implement and test adherence to the intervention. Secondary aims were to test preliminary group differences in change in BMIz over the summer and weight-related behaviors midsummer, and to examine the association between intervention participation and weight related behaviors in intervention participants. We anticipated that intervention participants would experience greater reductions in BMIz and would be more active and consume fewer calories midsummer than those in the comparison group, and that intervention participation would be inversely associated with change in BMIz and total energy intake and positively associated with physical activity.
2. Methods
2.1. Study design
PHAST was a quasi-experimental trial designed to compare excess summer weight gain in children who participated in a camp-like physical activity intervention to that of a comparison group of children recruited from the same community. The intervention included daily physical activity programming and a free lunch meal provided by the SFSP. Participants in the comparison group had similar access to the SFSP, but they did not have access to intervention programming. This study was funded by the Hassenfeld Child Health Innovation Institute at Brown University and was approved by the Institutional Review Board at Rhode Island Hospital. It is registered with ClinicalTrials.gov (NCT03118635).
2.2. Participants
Through partnerships with the local housing authority and public school district, we recruited children, ages 6–12 years, from two housing communities within the same low-income community. Given the geographic location of the intervention site (a public park across the street from one of the housing communities), recruitment efforts for the intervention group focused on families living within walking distance of the park. A second housing community within one mile of this park, but not easily walkable due to area traffic patterns, was identified for comparison group recruitment. Flyers inviting families to participate in either the intervention or comparison groups (based on geographic location) were sent out through the housing authority and the school district to families in the spring of 2016. Participants were also recruited through a series of community events during the same period.
Interested families were invited to attend an enrollment visit. To enroll, children had to 1) qualify for free or reduced-price meals at school, 2) speak, read and write English (for purposes of assessment and intervention), and 3) agree, along with their parent(s), to study participation. Participants were excluded if they had a medical condition that interfered with participation in physical activity or were otherwise enrolled in a full-time summer camp. We did not have any restrictions on siblings enrolling together. A total of 55 families expressed interest in the study (85 children in all). Four participants did not complete the baseline assessment, such that the final sample included 81 children (51 intervention and 30 comparison). Parental informed consent was obtained for all children enrolled in the study. Child assent was obtained from those ≥8 years.
Participants in both groups completed study assessments at the end of the school year (baseline), during weeks four and five of the 8-week summer (midsummer), and during the last week of summer (post-intervention). At the baseline assessment visit, a parent/guardian completed a sociodemographic questionnaire on participant age, sex, race/ethnicity, and maternal education. Participants were weighed and measured at baseline and post-intervention. At midsummer, participants completed three 24-h diet recalls and wore an ActiGraph for 24-h per day for seven days.
2.3. Summer intervention
The intervention was offered from 9 AM to 1 PM, Monday through Friday, for 8-weeks over the 2016 summer. Primary intervention components included a minimum of two hours of physical activity programming and lunch offered through the SFSP. The physical activity programming consisted of the Sports, Play, and Active Recreation for Kids - After School (SPARK AS) curriculum (Marcoux et al., 1999) and activity programming offered by six community organizations. SPARK AS, an evidence-based physical activity curriculum for school-age children, is associated with increased MVPA and decreased BMI (Sandoval Iversen et al., 2011). It was offered by eight college-age summer staff. Daily, a separate activity was also offered by a partnering community organization, which included: karate, Lego building, obstacle courses, hip hop dance, and creative movement.
Table 1 shows the schedule of a typical intervention day and examples of games and activities offered throughout the summer. After sign-in and warm-up, participants were broken up into groups by age and assigned to two staff members. Groups rotated through three, 30-min stations: two SPARK AS stations and the activity provided by the community organization. When a community organization was not scheduled, a third SPARK AS station was set-up. At each SPARK AS station, staff chose from a list of five to seven games/activities to do based on the age of the children, the number of children present, and their interests. After the rotations, all participants engaged in competitions with staff including obstacle courses, relay races, and water games.
Table 1.
Typical intervention day schedulea.
| Timing | Activity | Examples |
|---|---|---|
| 9–9:15 | Sign-In and Warm-Up | |
| 9:15–11:00 | Three 30-min physical activity stations Water breaks every 30 min |
SPARK Games: mini soccer, soccer golf, shoot and score, freaky freeze, hospital tag, capture the flag, flag pulling, kickball, SPUD, sugar and fat tag, Frisbee baseball, clothespin tag, and moon ball. |
| Community Partner Activities: Karate, Lego building, obstacle courses, hip hop dance, creative movement, and leadership training. | ||
| 11:00–12:00 | Big Group Activity | Competitions with staff including obstacle courses, relay races, and/or water games |
| 12:00–12:30 | SFSP Lunch | |
| 12:30–1:00 | Wrap-up and Sign out | Group point totals reviewed/campers of the day announced, “Dance Party” |
Intervention was offered in a low-income Rhode Island community in summer 2016.
Lunch was provided daily via the SFSP, which serves free summer lunch meals to children ≤18 years old in communities where ≥50% of children qualify for free or reduced-price school meals (U.S. Department of Agriculture, 2016a). Per federal guidelines, SFSP lunches must include 8 oz. of milk, ¾ cup of fruit/vegetable, 1 serving of grains/breads, and 1 serving of lean protein/equivalent (U.S. Department of Agriculture, 2016b). Within this community, the SFSP is run by the school district's food service provider. After lunch service, camper of the day was awarded to one child in each group who modeled exemplary behavior. Prior to dismissal, camp ended with a dance party.
2.4. Comparison condition
The comparison group had an SFSP open-side at their housing community but no access to the intervention programming.
2.4.1. Process measures
Process data were collected to evaluate the primary aim of testing implementation and adherence to the intervention. We tracked completion of midsummer measures (diet and physical activity) to assess the feasibility of assessing weight-related behaviors in the summer. To assess the feasibility of intervention implementation, program coordinators tracked which SPARK AS games/activities were most frequently played and the number of days activities were provided by community partners. To assess adherence, intervention participation was tracked through daily attendance logs.
2.4.2. Outcome measures
2.4.2.1. Anthropometry
Change in BMIz models change in adiposity longitudinally and was used to measure summer weight gain (Must and Anderson, 2006). It was derived from objective weight and height measurements taken at the baseline and post-intervention assessments. Weight was measured in street clothes, without shoes, using a digital scale to the nearest 0.1 kg. Height was measured using a portable stadiometer to the nearest millimeter.
2.4.2.2. Dietary assessment
Diet was assessed midsummer via three, non-consecutive 24-h diet recalls (2 weekdays, 1 weekend day). Registered dietitians from the Cincinnati Center for Nutrition Research at Cincinnati Children's Hospital Medical Center collected the recalls over the phone using Nutrition Data Systems for Research (NDSR; Nutrition Coordinating Center, University of Minnesota, MN). NDSR is a software program that employs a variation of the USDA's validated Automated Multiple Pass Method to collect detailed information on each food and beverage consumed at each eating occasion over the previous 24-h period (Moshfegh et al., 2008). Participants who were 12 years completed the recalls on their own, whereas proxy-assisted interviews were conducted for all younger participants. In addition to assessing the feasibility of 24-h diet recall collection during the summer, we were also interested in examining preliminary group differences in energy intake.
2.4.2.3. Physical activity & sedentary behavior
Physical activity and sedentary behavior were measured for 24-h per day for one week midsummer using a wrist-worn accelerometer (ActiGraph wGT3X-BT, LLC, Pensacola FL). Participants wore the ActiGraph on their non-dominant wrist, given findings that this improves adherence over waist placement (Tudor-Locke et al., 2015). The ActiGraph measures 3-dimensional movement and was calibrated to store data in one-minute epochs (McClain and Tudor-Locke, 2009). We applied the Crouter et al. vector magnitude regression cut-points for wrist-worn accelerometer data to identify minutes spent sedentary and engaged in MVPA (Crouter et al., 2015). Participant data were considered valid and included in the analyses if daily wear time was ≥8 h on a minimum of two weekdays and one weekend day. We examined the feasibility of objectively measuring physical activity and sedentary behavior in the summer, and preliminarily, we compared minutes of MVPA and sedentary behavior as well as percent time spent sedentary across groups.
2.5. Data analyses
All statistical analyses were conducted using SAS 9.4 (2014; SAS Institute, Inc., Cary, NC), at the two-sided 0.05 level of significance. General descriptive statistics were generated for demographics and anthropometrics at baseline. Group differences were assessed using Student's t- and Chi-square tests as appropriate. To address our primary aim, testing the implementation of and adherence to the intervention, process measures of intervention dose and assessment completion were evaluated with frequencies. This trial was not powered to test for intervention effects on BMIz and weight-related behaviors. Thus, to examine the preliminary effectiveness of intervention participation, we used a multivariable mixed model that included family as a random variable and controlled for age and race / ethnicity to estimate group differences in change in BMIz over the summer. Given that we were unable to measure weight-related behaviors at baseline, we assessed group differences in midsummer physical activity and total energy intake using t-tests and multivariable mixed model as described above. We examined differences on weekday and weekend days separately to account for the fact that the intervention and the SFSP were only offered on weekdays. The random family variable was included in all mixed models to account for clustering of participants within families. Finally, within intervention participants only, we examined differences in physical activity and total energy intake by participation using repeated measures analysis of variance.
3. Results
3.1. Participant characteristics
Table 2 shows the sociodemographic characteristics of intervention and comparison participants. Intervention participants were, on average, one year younger (p = 0.01) and more likely to be from a racial or ethnic minority group (p = 0.03) as compared to those in the comparison group. >95% of both groups qualified for free meals and 5% qualified for reduced-price meals. Further, both groups had comparable rates of overweight and obesity to each other and to national averages (Ogden et al., 2014).
Table 2.
Baseline characteristics of PHAST intervention and comparison participantsa.
| Intervention (n = 51) |
Comparison (n = 30) |
p-value | |
|---|---|---|---|
| Age (mean years (SD)) | 8.6 (1.9) | 9.7 (2.2) | 0.01 |
| Female (%) | 51.9 | 33.3 | 0.09 |
| Race/ethnicity (%) | |||
| Non-Hispanic White | 9.8 | 26.7 | 0.03 |
| Non-Hispanic Black | 11.8 | 26.7 | |
| Non-Hispanic Other | 39.2 | 23.3 | |
| Hispanic, All Races | 39.2 | 23.3 | |
| Maternal education (%) | |||
| High School Degree or Less | 54.0 | 64.3 | 0.18 |
| Some College | 28.0 | 32.1 | |
| College Graduate or more | 18.0 | 3.6 | |
| Qualification for Free Lunch (%) | 95.6 | 96.7 | 0.90 |
| Overweight/Obeseb (%) | 45.1 | 38.0 | 0.53 |
| Attended Camp in Summer 2015 (%) | 19.2 | 26.7 | 0.23 |
Participants were recruited from a low-income Rhode Island community in 2016.
Overweight and Obese status determined by BMI for age and sex ≥85th percentile.
3.2. Primary aims: process data
Of the 81 participants who completed the baseline assessment, 68.6% (n = 34) and 70% (n = 21) of participants completed the midsummer diet recalls and 64.7% (n = 33) and 70% (n = 21) of participants provided usable ActiGraph data in the intervention and comparison groups, respectively. Ninety percent (n = 46) of intervention and 97% (n = 29) of comparison participants completed the post-intervention assessment. The intervention was delivered 39 days of the 8-week summer, with one day off for the Fourth of July. Community partners provided activity programming on 79% (31 of 39) of intervention days (3 days of karate; 7 days of obstacle course training, 13 days of hip hop dance instruction, 5 days of creative movement and 3 days of Lego building). Finally, as a measure of adherence, intervention participants attended the program 65.6 ± 10% of days it was offered (25.6 ± 8.9 of the 39 intervention days). Weekly attendance ranged from a high of 79.6% in week two to a low of 52.1% in week five, and rebounded to 69.0% in week eight.
3.3. Secondary outcomes
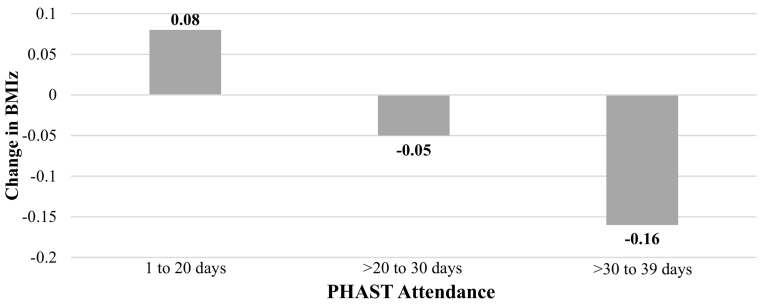
There was a 0.07 unit difference in change in BMIz between the intervention and comparison group (−0.04 + 0.21 vs. 0.03 + 0.13 BMIz units; p = 0.07). The effect size remained comparable after adjusting for clustering by family and controlling for group differences in age and race/ethnicity (b = −0.10; p = 0.07). We also examined the change in BMIz by levels of intervention participation: 1 to 20 days, >20 to 30 days, >30 to 39 days. As depicted in Fig. 1, intervention participants who attended 1–20 days gained 0.08 BMIz units over the summer, whereas those with the highest attendance (>30 to 39 days) lost 0.16 BMIz units (p = 0.01).
Fig. 1.
Change in BMIz by intervention attendance1,2.
1PHAST intervention attendance: 1 to 20 days: n = 13; >20 to 30 days: n = 20; >30 to 39 days: n = 13.
2Mean Change in BMIz values for groups 1 and 3 are statistically significantly different (p = 0.01).
There were no significant differences in average weekday energy intake or minutes of weekday MVPA between groups as shown in Table 3A. The significance of these relationships did not change after controlling for clustering by family and differences in age and race/ethnicity across groups. However, midsummer, intervention participants spent 4.6 less time sedentary on weekdays as compared to comparison participants (p = 0.03). None of these behaviors differed significantly between groups on the weekends (data not shown; ps > 0.05).Table 3B shows the associations between intervention attendance and reported total energy intake, minutes of MVPA, minutes of sedentary behavior and percent time sedentary within the intervention participants only. There were no differences in reported energy intake on weekdays when intervention participants did vs. did not attend the program. However, on days participants attended the intervention, they engaged in 41 more minutes of MPVA (p = 0.004) and spent 8.5% less time sedentary as compared to days they did not attend (p = 0.0004).
Table 3.
Midsummer differences in reported energy intake, minutes of moderate to vigorous physical activity (MVPA) and percent time spent sedentary on weekdays in children in the intervention and comparison groups of PHAST.
| A. t-tests comparing weekday weight-related behaviors between intervention and comparison groups (Mean ± SD) | |||
|---|---|---|---|
| Intervention | Comparison | p-value | |
| Energy intakea | (n = 35) 1644.1 ± 52.3 |
(n = 21) 1603.7 ± 421.1 |
0.64 |
| Minutes of MVPAb | (n = 33) 179.2 ± 35.3 |
(n = 21) 157.1 ± 50.4 |
0.06 |
| Minutes sedentaryc | (n = 33) 452.7 ± 64.2 |
(n = 21) 504.4 ± 54.3 |
0.004 |
| Percent time sedentaryd | (n = 33) 56.4 ± 6.2% |
(n = 21) 61.0 ± 8.9% |
0.03 |
| B. Repeated measures ANOVA comparing weight-related behaviors in the intervention group on weekdays when they attended the program vs weekdays that they did not attend (Mean ± SD) | |||
| Intervention Days | Absent Days | p-value | |
| Energy intakea (n = 34) | 1720.9 ± 103.1 | 1585.4 ± 138.1 | 0.45 |
| Minutes of MVPAb (n = 33) | 193.4 ± 7.3 | 152.5 ± 10.4 | 0.004 |
| Minutes sedentaryc (n = 33) | 317.5 ± 105.1 | 403.2 ± 125.7 | <0.0001 |
| Percent time sedentaryd (n = 33) | 53.7 ± 1.1% | 62.2 ± 1.6% | 0.0004 |
Total reported energy intake averaged over two weekday 24-h diet recalls.
Minutes of Moderate to Vigorous physical activity (Vector Magnitude counts >7320 cpm).
Minutes of Sedentary behavior (Vector Magnitude counts <1200 cpm).
Percent of total wear time spent sedentary.
4. Discussion
The primary aim of this paper was to assess the feasibility of implementation and adherence to the PHAST intervention in youth from a low-income community. We recruited 51 intervention and 30 comparison participants, completed midsummer assessments of diet and physical activity with approximately 70% of participants, and retained 92.5% participants in the study. Moreover, we provided physical activity programming daily for 39 days over 8-weeks of summer vacation, with community partners providing different activities on 79% of those days. Given that average intervention participation was 66%, however, refinement of the intervention protocol is warranted. By comparison, Olvera (Olvera et al., 2013b) and Baranowski (Baranowski et al., 2003) reported 90% and 91.5% participation, respectively (Baranowski et al., 2003). Their studies included mother / daughter pairs and were shorter in duration. They also did considerable formative work to inform their interventions and to ensure their cultural sensitivity (Baranowski et al., 2003; Olvera et al., 2010). By comparison our programming used existing curriculum and was offered in conjunction with the SFSP, which had a predetermined daily menu. Thus, the PHAST intervention may benefit from input from children, parents and community partners so as to identify ways to more consistently engage children in the intervention.
The preliminary effectiveness of the trial in reducing excess summer weight gain supports conducting a sufficiently powered, randomized trial. Overall, intervention participants experienced a 0.04 BMIz unit reduction, while BMIz increased by 0.03 units in the comparison group. Further, intervention participants who attended >30 to 39 sessions lost 0.16 BMIz units over the summer, on average. While these reductions would be considered modest for an obesity treatment intervention, they are encouraging given the objective to prevent excess summer weight gain. They are also similar in magnitude to the average 0.04 to 0.09 BMIz unit increase Moreno and colleagues observed over a five year examination of ethnically diverse elementary school-age children (Moreno et al., 2015). Moreover, they are consistent with results from other summertime interventions (Olvera et al., 2013b; George et al., 2016). Together, these findings support that preventing excess summer weight gain may be feasible.
Intervention participants spent 4.6% less time sedentary on weekdays as compared to those in the comparison group. They also engaged in more MVPA and were less sedentary on days they attended the intervention as compared to days they were absent. These findings are consistent with other interventions that have used the SPARK AS curriculum to increase MVPA in youth (Sandoval Iversen et al., 2011; Fu et al., 2016; Nigg et al., 2012). Specifically, researchers found a 14 min increase in daily out-of-school MVPA after a 6-month after-school intervention in which the SPARK AS curriculum was used (Sandoval Iversen et al., 2011). Unexpectedly, there were no midsummer differences in reported energy intake between groups or among intervention participants on days they did and did not attend the intervention. Consistent with the SDH, we anticipated that participating in the intervention would decrease the opportunity for snacking and reduce exposure to the home food environment, thereby reducing total energy intake. While this study was not powered for this analysis, it is possible that these null findings are due to the half-day design of our program, leaving children more time to engage in obesogenic eating behaviors. It is also possible that the potential correlates of diet recall accuracy, including both parents' and children's social desirability, weight-status, sex, age, and cognitive ability, may have obscured group differences in intake (Baxter, 2009).
This study has several limitations. First, we were unable to measure baseline diet and physical activity in study participants, which precludes us from drawing conclusions on how the intervention affected behavior from baseline. We addressed this limitation by comparing midsummer behaviors between intervention and comparison groups and by examining behaviors within intervention participants on days they did and did not attend the program. Future work should also consider collecting self-report measures of screen time and sleep to complement the Actigraphy data. Second, we could not randomly assign children to groups. Given that the intervention was advertised within a public housing community and conducted at an adjacent public park, we could not deny access to the program to children who enrolled. We addressed this by recruiting a comparison group from a neighboring housing community that was separated from the park by complex traffic patterns but had similar sociodemographic characteristics. Finally, we did not obtain feedback from participants related to barriers to adherence to the program, and thus cannot use this information to refine the intervention.
Despite these limitations, this study has several strengths. First, it was eight weeks in duration and conducted within a real-world setting in a community-park across from a public housing community from which the intervention sample was recruited. More specifically, the intervention targeted a high-risk, eight-week period that has been documented to contribute to long-term weight gain in youth. Lastly, our intervention was offered in conjunction with the SFSP, which is funded by the USDA and offered in communities across the United States. Thus, it has potential for dissemination.
5. Conclusion
Findings from this study suggest that the delivery of a physical activity-based summer program is feasible within a low-income community. They provide preliminary evidence in support of the SDH by showing that children were more physically active and less sedentary on days they attended the intervention versus days they stayed home. Summer interventions like PHAST have significant public health potential, as they may help decrease weight-related health disparities. More work is needed to refine this intervention and to test its effectiveness in a fully powered, randomized trial with baseline and follow-up measures of weight-related behaviors.
Contributor's statement
EWE, RRW, and EJ conceived the study, EWE, DFP, and WCH recruited participants, collected data and delivered the intervention, EWE, DSB, EJ and RRW analyzed and interpreted the data. All authors were involved in writing the paper and had final approval of the submitted version.
Financial disclosure
The authors have no financial relationships relevant to this article to disclose.
Potential conflicts of interest
The authors have no conflicts of interest relevant to this article to disclose.
Funding
Hassenfeld Childhood Health Innovation Institute at Brown University; National Institute of Diabetes and Digestive and Kidney Diseases (K01DK110142, EWE).
References
- Baranowski T., Baranowski J., Cullen K. The fun, food and fitness project (FFFP): the Baylor GEMS pilot study. Ethn. Dis. 2003;13(Supp. 1):S1-30–S31-39. [PubMed] [Google Scholar]
- Baranowski T., O'Connor T., Johnston C. School year versus summer differences in child weight gain: a narrative review. Child Obes. 2014;10(1):18–24. doi: 10.1089/chi.2013.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter S. Cognitive processes in children's dietary recalls: insight from methodological studies. Eur. J. Clin. Nutr. 2009;63(Suppl. 1):S19–S32. doi: 10.1038/ejcn.2008.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert A., Ward A., Burdette K., Silton R., Dugas L. Active summers matter: evaluation of a community-based summertime program targeting obesogenic behaviors of low-income, ethnic minority girls. New Dir. Youth Dev. 2014;(143):133–150. doi: 10.1002/yd.20107. [DOI] [PubMed] [Google Scholar]
- Brazendale K., Beets M.W., Weaver R.G. Understanding differences between summer vs. school obesogenic behaviors of children: the structured days hypothesis. Int. J. Behav. Nutr. Phys. Act. 2017;14(1):100. doi: 10.1186/s12966-017-0555-2. (July 26) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . US Dept of Health and Human Services; Atlanta, GA: 2014. Putting Local School Wellness Policies into Action. [Google Scholar]
- Centers for Disease Control and Prevention - Division of Community Health . 2013. A practitioner's guide for advancing health equity: community strategies for preventing chronic disease. Atlanta, GA. [Google Scholar]
- Chen T.-A., Baranowski T., Moreno J.P. Obesity status trajectory groups among elementary school children. BMC Public Health. 2016;16(1):526. doi: 10.1186/s12889-016-3159-x. (July 07) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christodoulos A., Flouris A., Tokmakidis S. Obesity and physical fitness of pre-adolescent children during the academic year and the summer period: effects of organized physical activity. J. Child Health Care. 2006;10(3):199–212. doi: 10.1177/1367493506066481. [DOI] [PubMed] [Google Scholar]
- Crouter S., Flynn J., Bassett D. Estimating physical activity in youth using a wrist worn accelerometer. Med. Sci. Sports Exerc. 2015;47(5):944–951. doi: 10.1249/MSS.0000000000000502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham S.A., Kramer M.R., Narayan K.M.V. Incidence of childhood obesity in the United States. N. Engl. J. Med. 2014;370(5):403–411. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economos C.D., Hyatt R.R., Must A. Shape up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev. Med. 2013;57(4):322–327. doi: 10.1016/j.ypmed.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Franckle R., Adler R., Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev. Chronic Dis. 2014;11 doi: 10.5888/pcd11.130355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Y., Gao Z., Hannon J., Burns R., Brusseau T. Effect of the SPARK program on physical activity, cardiorespiratory endurance, and motivation in middle-school students. J. Phys. Act. Health. 2016;13(5):534–542. doi: 10.1123/jpah.2015-0351. [DOI] [PubMed] [Google Scholar]
- George G., Schneider C., Kaiser L. Healthy lifestyle fitness camp: a summer approach to prevent obesity in low-income youth. J. Nutr. Educ. Behav. 2016;48(3):208–212. doi: 10.1016/j.jneb.2015.12.010. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P. National Heart, Lung and Blood Institute; Bethesda, MD: 2004. Predictors of Obesity, Weight Gain, Diet and Physical Activity. [Google Scholar]
- von Hippel P., Workman J. From kindergarten through second grade, U.S. children's obesity prevalence grows only during summer vacations. Obesity. 2016;24(11):2296–2300. doi: 10.1002/oby.21613. [DOI] [PubMed] [Google Scholar]
- von Hippel P., Powell B., Downey D., Rowland N. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. Am. J. Public Health. 2007;97(4):696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcoux M., Sallis J., McKenzie T., Marshall S., Armstrong C., Goggin K. Process evaluation of a physical activity self-management program for children: SPARK. Psychol. Health. 1999;14:659–677. [Google Scholar]
- May A., Freedman D., Sherry B., Blanck H. Obesity - United States, 1999-2010. MMWR Morb. Mortal. Wkly Rep. 2013;62(3):120–128. [PubMed] [Google Scholar]
- McClain J.J., Tudor-Locke C. Objective monitoring of physical activity in children: considerations for instrument selection. J. Sci. Med. Sport/Sports Med. Aust. 2009;12(5):526–533. doi: 10.1016/j.jsams.2008.09.012. [DOI] [PubMed] [Google Scholar]
- McCue M., Marlatt K., Sirard J. Examination of changes in youth diet and physical activity over the summer vacation period. Internet J. Allied Health Sci. Pract. 2013;11(1) (Article 8) [Google Scholar]
- Moreno J., Johnston C., Woehler D. Changes in weight over the school year and summer vacation: results of a 5-year longitudinal study. J. Sch. Health. 2013;83(7):473–477. doi: 10.1111/josh.12054. [DOI] [PubMed] [Google Scholar]
- Moreno J., Johnson C., Chen T. Seasonal variability in weight change during elementary school. Obesity. 2015;23:422–428. doi: 10.1002/oby.20977. [DOI] [PubMed] [Google Scholar]
- Moshfegh A.J., Rhodes D.G., Baer D.J. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am. J. Clin. Nutr. 2008;88(2):324–332. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- Must A., Anderson S.E. Body mass index in children and adolescents: considerations for population-based applications. Int. J. Obes. 2006;30(4):590–594. doi: 10.1038/sj.ijo.0803300. [DOI] [PubMed] [Google Scholar]
- Nigg C., Geller K., Adams P., Hamada M., Hwang P., Chung R. Successful dissemination of fun 5 – a physical activity and nutrition program for children. Transl. Behav. Med. 2012;2(3):276–285. doi: 10.1007/s13142-012-0120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden C.L., Carroll M.D., Kit B.K., Flegal K.M. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olvera N., Scherer R., McLeod J. BOUNCE: an exploratory healthy lifestyle summer intervention for girls. Am. J. Health Behav. 2010;34(2):144–155. doi: 10.5993/ajhb.34.2.2. [DOI] [PubMed] [Google Scholar]
- Olvera N., Leung P., Kellam S.F., Liu J. Body fat and fitness improvements in Hispanic and African American girls. J. Pediatr. Psychol. 2013;38(9):987–996. doi: 10.1093/jpepsy/jst041. [DOI] [PubMed] [Google Scholar]
- Olvera N., Leung P., Kellam S.F., Smith D.W., Liu J. Summer and follow-up interventions to affect adiposity with mothers and daugthers. Am. J. Prev. Med. 2013;44(3S3):S258–S266. doi: 10.1016/j.amepre.2012.11.018. [DOI] [PubMed] [Google Scholar]
- Rodriguez A.X., Olvera N., Leung P., O'Connor D.P., Smith D.W. Association between the summer season and body fatness and aerobic fitness among Hispanic children. J. Sch. Health. 2014;84(4):233–238. doi: 10.1111/josh.12141. [DOI] [PubMed] [Google Scholar]
- Sandoval Iversen C., Nigg C., Titchenal T. The impact of an elementary after-school nutrition and physical activity program on children's fruit and vegetable intake, physical activity, and body mass index: fun 5. Hawaii Med. J. 2011;70(suppl):37–41. [PMC free article] [PubMed] [Google Scholar]
- Schreier H., Chen E. Socioeconomic status and the health of youth: a multi-level multi-domain approach to conceptualizing pathways. Psychol. Bull. 2013;139(3):606–654. doi: 10.1037/a0029416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tovar A., Lividini K., Economos C., Folta S.C., Goldberg J., Must A. School's out: what are urban children doing? The summer activity study of Somerville youth (SASSY) BMC Pediatr. 2010;10 doi: 10.1186/1471-2431-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C., Barreira T.V., Schuna J.M. Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the international study of childhood obesity, lifestyle and the environment (ISCOLE) Int. J. Behav. Nutr. Phys. Act. 2015;12(1):11. doi: 10.1186/s12966-015-0172-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture Nutrition Guide: Summer Food Service Program. 2016. http://www.fns.usda.gov/sites/default/files/sfsp/NutritionGuide.pdf
- U.S. Department of Agriculture Summer Food Service Program: Nutrition Guide. 2016. https://fns-prod.azureedge.net/sites/default/files/sfsp/NutritionGuide.pdf
- U.S. Department of Education, National Center for Education Statistics Digest of Education Statistics, 2015. 2016. https://nces.ed.gov/programs/digest/d15/
- Wang Y., Gortmaker S., Taveras E. Trends and racial/ethnic disparities in severe obesity among US children and adolescents, 1976–2006. Int. J. Pediatr. Obes. 2011;6(1):12–20. doi: 10.3109/17477161003587774. [DOI] [PubMed] [Google Scholar]