Abstract
Background
Pictorial warnings on cigarette packs are a cost-effective policy-level intervention for smoking cessation; however, little research has examined changes in the impact of warnings over time, especially shortly following the first exposure to pictorial warnings. We sought to characterize the trajectories of responses to pictorial cigarette pack warnings soon after first exposure.
Methods
Participants were 2149 adult smokers in North Carolina and California, United States. In 2014–2015, we randomized smokers to have pictorial (intervention) or text-only (control) warnings on their cigarette packs for 4 weeks. Weekly surveys assessed psychosocial and behavioral outcomes.
Results
After 1 week, smokers in the intervention arm reported higher levels of most outcomes, compared with the control arm. Over subsequent weeks, smokers in both trial arms had decreases in thinking about the harms of smoking (β = –0.046), positive (β = –0.036), and negative (β = –0.042) smoking reinforcement attitudes, and increases in quit intentions (β = 0.070) and cigarette forgoing (β = 0.137) (all p < .05). Only negative affective reactions decreased more in the intervention versus control condition (pinteraction < .01).
Conclusions
The impact of pictorial cigarette pack warnings on emotions and cognitions may wane over time. In contrast, quit intentions and cigarette forgoing may continue to increase, at least during the initial period after introduction. Rotation of pictorial warnings may help prevent warning wear-out.
Implications
Cigarette smoking is the leading cause of preventable morbidity and mortality and warnings on cigarette packs are a cost-effective policy-level intervention. Prior studies reporting on cigarette pack warning “wear out” have been limited by being short-term single-session experimental studies. Ours are the first study to experimentally examine the trajectories of several outcomes after first exposure and report that the impact of pictorial cigarette pack warnings on emotions and cognitions may wane over time while quit intentions and cigarette forgoing may continue to increase.
Trials Registration
ClinicalTrials.gov identifier: NCT02247908; https://clinicaltrials.gov/ct2/show/NCT02247908.
Introduction
The prevalence of smoking in the United States has declined among adults in the last decade,1 yet cigarette smoking remains the leading cause of preventable morbidity and mortality.2 One cost-effective policy-level intervention for smoking cessation is the requirement for cigarette packs to have warnings about the health consequences of smoking.3 Observational and experimental evidence shows that pictorial warnings are more effective than text-only warnings at garnering attention, changing intentions, and discouraging smoking.4–9 The rationale for the added effectiveness of images is that text-only warnings rely on being noticed and then read and thus require careful attention to be effective, whereas images can be understood at a glance and can elicit affect to add meaning and importance to the “facts” of the message.10–13 Pictorial warnings may also reach a larger audience as they may be more accessible to those with low health literacy.14,15 Indeed, compared with text-only warnings, pictorial warning messages are more likely to be noticed and elicit greater increases in cognitive processing, negative affective reactions, self-efficacy and intentions to quit smoking.5,16 The message impact framework5 suggests that these constructs potentially contribute to changes in smoking behavior.
Little research has examined changes in the impact of warnings over time, especially shortly following the first exposure to pictorial warnings. New warnings may have their greatest impact after the first few exposures,17 with pictorial warnings sustaining their psychological and behavioral effects longer than text-only warnings.18 Nonetheless, all warnings wear-out over time.18,19 Observational studies of the impact of pictorial warnings on adult smokers report immediate increases followed by decreases in cognitive processing of, and behavioral responses to, new warnings over a period of months or years.18,20–23 What is less clear is whether wear-out can occur after even a few weeks of exposure; short-term studies of pictorial warnings have largely been a single-session experiments, and therefore longitudinal data to explore this question are currently lacking.
We previously reported that pictorial cigarette pack warnings effectively increased several psychological outcomes, intentions to quit smoking, forgoing cigarettes, quit attempts, and successfully quitting smoking over 4 weeks in a large randomized trial.9 In the current study, we sought to characterize the trajectories of responses to pictorial cigarette pack warnings in the weeks after first exposure.
Methods
Study Population
This study analyzed longitudinal data from a randomized clinical trial conducted from September 2014 to August 2015. Participants were 2149 adult (≥18 years of age), English-speaking current smokers residing in North Carolina (NC) and California (CA), United States. Details of the trial including study protocols, participant recruitment, and participant characteristics appear elsewhere (NCT02247908).9
Procedures
In brief, using simple randomization, we used a random number generator to create a randomly ordered, pre-populated list of study conditions and assigned trial participants to have their cigarette packs labeled over 4 weeks with either one of four pictorial warnings selected from the FDA’s originally proposed set of images (i.e., intervention condition) or one of four text-only US Surgeon General’s warnings (i.e., control condition). Participants completed a pre-labeling questionnaire had an 8-day supply of cigarette packs labeled, and then immediately after pack labelling completed a post-labeling questionnaire. Over the subsequent 4 weeks, participants returned for labeling of new cigarette packs and to complete a weekly follow-up questionnaire. The University of North Carolina Institutional Review Board approved the study procedures.
Measures
We report on secondary trial outcomes assessed at all follow-up visits. At each of the follow-up weeks (week 1, week 2, week 3, and week 4), the questionnaires assessed cognitive elaboration (thinking about the warning message and thinking about the harms of smoking), smoking reinforcement attitudes (positive and negative reinforcement attitudes), negative affective reactions to the warnings, quit intentions, and cigarette forgoing.
Cognitive Elaboration
Questionnaires assessed cognitive elaboration about the warning message and the harms of smoking using four items.3 Two questions were related to thinking about the warning message: “When you notice your cigarette pack, how often do you think about the message the warning conveys?” and “When your cigarette pack is not in sight, how often do you think about the message that the warning conveys?” and two questions related to thinking about the harms of smoking: “In the last week, how often did you think about the harm your smoking might be doing to you?” and “In the last week, how often did you think about the harm your smoking might be doing to other people?.” The 5-point response scale ranged from “never” (coded as 1) to “all of the time” (coded as 5). We averaged the two items related to thinking about the warning message (r range = 0.70 to 0.80) and the two items related to thinking about the harms of smoking (r range = 0.62 to 0.69) to create two scales with higher scores indicating greater cognitive elaboration.
Smoking Reinforcement Attitudes
Questionnaires assessed positive and negative smoking reinforcement attitudes using eight items from the Smoking Consequences Questionnaire.24 Examples of the positive and negative smoking reinforcement items included, respectively: “When I smoke, the taste is pleasant,” and “If I’m tense, a cigarette helps me relax.” The 5-point response scale ranged from “strongly disagree” (coded as 1) to “strongly agree” (coded as 5). We averaged the four positive (Cronbach’s α range = .95 to .97) and four negative (Cronbach’s α range = 0.93 to 0.96) items to create two scales with higher scores indicating greater smoking reinforcement attitudes.
Negative Affective Reactions
Questionnaires assessed negative affective reactions to the warnings using 15 questions adapted from several sources16,25–27 for the main trial. Participants were asked: “How much did the warning on your cigarette packs make you feel… Afraid, Frightened, Scared, Blue, Depressed, Sad, Ashamed, Guilty, Regretful, Anxious, On edge, Uneasy, Disgusted, Grossed out, and Repelled?.” The 5-point response scale ranged from “not at all” (coded as 1) to “extremely” (coded as 5). We averaged the three items related to fear (Cronbach’s α range = 0.94 to 0.96) and the 12 remaining items (Cronbach’s α range = 0.96 to 0.97) to create two scales with higher scores indicating greater negative affective reactions in response to the cigarette pack warnings.
Quit Intentions
Questionnaires assessed intentions to quit smoking using three questions: “How interested are you in quitting smoking in the next month,” “How much do you plan to quit smoking in the next month?” and “How likely are you to quit smoking in the next month?”28 The 4-point response scales ranged from “not at all,” “not at all interested,” or “not at all likely” (coded as 1) to “very interested,” “very much,” or “very likely” (coded as 4). We averaged the three items (Cronbach’s α range = 0.93 to 0.95) to create a scale with higher scores indicating greater intentions to quit smoking in the next month.
Cigarette Forgoing
At each week, the questionnaire asked: “In the last week, how often have you stopped yourself from having a cigarette because you wanted to smoke less?”29 The 5-point response scale had response options “Never” (coded as 0), “1–2 times,” (coded as 1.5), “3–4 times” (coded as 3.5), “5–9 times” (coded as 7), and “10 or more times” (coded as 10).
Statistical Analysis
Consistent with the analyses of the main trial,9 which was powered to examine group differences in quit attempts between intervention and participants, here we used descriptive statistics to characterize the trajectories of the outcomes, irrespective of specific pictorial or text-only warning group assignment over the four follow-up weeks. At each follow-up week, we examined mean differences in each of the outcomes using PROC TTEST for independent samples t-tests. We fit mixed effects models with random intercepts using PROC MIXED, to assess the impact of trial arm (intervention versus control), time (the number of weeks from the first follow-up assessment to the last assessment), and arm-by-time effects on each outcome, separately. An advantage of the likelihood-based estimation method employed in PROC MIXED is that it uses all available data to generate estimates, rather than omitting subjects with any missing data.30 For each outcome, we calculated the intraclass correlation coefficient from an intercept only model. Intervention and control arms did not differ at baseline on any of the demographic characteristics, as previously reported.9 Therefore all models are unadjusted. Analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
The 2149 participants who enrolled in the trial were around 40 years old on average, non-Hispanic (91%), black (47%) and white (36%), and low-income (54%) based on federal poverty guidelines. The proportions of participants who complete the follow-up surveys at each of the follow-up weeks included 86% at week 1, 82%, at week 2, 81% at week 3, and 88% at week 4.
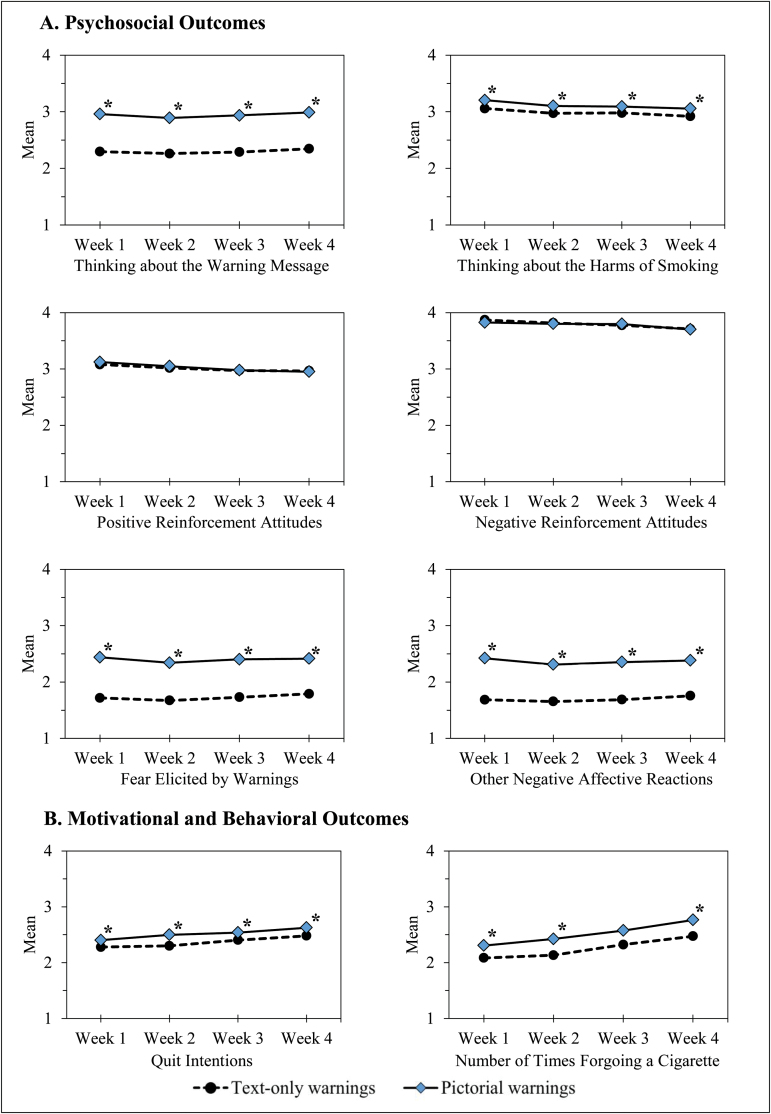
Participants in the intervention arm reported higher levels of most outcomes at each of the four follow-up weeks, compared with participants in the control arm (all t-tests p < .05) (Figure 1). At follow-up week 1, participants exposed to pictorial warnings reported higher cognitive elaboration related to the warning message (Arm β = 0.650, p < .001) and about the harms of smoking (Arm β = 0.136, p < .01), higher fear (Arm β = 0.700, p < .001) and other negative affective reactions (Arm β = 0.711, p < .001), higher quit intentions (Arm β = 0.150, p < .01), and a higher frequency of forgoing a cigarette (Arm β = 0.272, p = .02), compared to those exposed to text-only warnings (Table 1).
Figure 1.
Trajectories of psychosocial (A) and behavioral (B) outcomes by trial arm over the study follow-up (N = 2149). Arm differences at each week were determined using independent samples t-tests; *p < .05.
Table 1.
Intervention effects on psychosocial and behavioral outcomes (N = 2149)
| Arm | Time (weeks) | Arm*Time | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | ICC | β | (SE) | p | β | (SE) | p | β | (SE) | p |
| Thinking about warning message | 0.76 | 0.650 | (0.049) | <.001 | 0.011 | (0.008) | .56 | –0.012 | (0.011) | .18 |
| Thinking about smoking harms | 0.66 | 0.136 | (0.048) | <.01 | –0.046 | (0.009) | <.001 | –0.006 | (0.013) | .63 |
| Positive reinforcement attitudes | 0.80 | 0.047 | (0.050) | .34 | –0.036 | (0.007) | <.001 | –0.016 | (0.010) | .11 |
| Negative reinforcement attitudes | 0.74 | –0.029 | (0.042) | .50 | –0.042 | (0.007) | <.001 | 0.008 | (0.010) | .38 |
| Fear elicited by warnings | 0.81 | 0.700 | (0.054) | <.001 | 0.021 | (0.008) | .56 | –0.035 | (0.011) | <.01 |
| Other negative affective reactions | 0.82 | 0.711 | (0.047) | <.001 | 0.016 | (0.006) | .74 | –0.034 | (0.009) | <.001 |
| Quit intentions | 0.81 | 0.150 | (0.047) | <.01 | 0.070 | (0.006) | <.001 | –0.008 | (0.009) | .36 |
| Number of times forgoing a cigarette | 0.58 | 0.272 | (0.112) | .02 | 0.137 | (0.024) | <.001 | –0.027 | (0.035) | .44 |
Arm βs represent the mean difference in the outcome between intervention and control arms at follow-up week 1. Time βs represent the rate of change in the outcome per week among all participants. Arm*Time βs represent the rate of change in the outcome per week among intervention versus control participants.
ICC, intraclass correlation coefficient.
Over the 4-week follow-up, participants continued to think about the warnings as much as they had at week 1 (Time β = 0.011, p = .56). Thinking about the harms of smoking decreased after the first week (Time β = –0.046, p < .001), as did positive and negative reinforcement attitudes (Time β = –0.036 and –0.042, p < .001). In contrast, quit intentions (Time β = 0.070, p < .001), and cigarette forgoing (Time β = 0.137, p < .001) increased after the first week (Table 1). Fear (Arm*Time β = –0.035) and other negative affective reactions (Arm*Time β = –0.034) were initially high and then slightly decreased in the pictorial warning, but not the text-only, arm (both pinteraction < .01).
Discussion
In this large randomized trial, we found that compared with text-only warnings, pictorial warnings on cigarette packs were more effective in eliciting cognitive and behavioral responses, with differences apparent after just 1 week of follow-up and maintained over the 4 weeks. The largest difference between intervention and control participants at the first follow-up week was for fear and other negative affective reactions, and thinking about the warning message. At the first follow-up week, intervention also participants reported small increases in quit intentions and cigarette forgoing. Although smokers in both arms reported small decreases in several of the psychosocial outcomes investigated, only negative affective reactions decreased more among smokers in the pictorial warning arm, suggesting that although warnings that elicit strong negative emotional reactions may be most effective in conveying the negative health effects of smoking and promoting behavior change,16,31 they are susceptible to wearout even over short periods of time. Of particular importance, quit intentions and cigarette forgoing increased in both arms over the four follow-up weeks.
Prior research on pictorial and text-only cigarette pack warnings has shown that the impact of warnings on thinking about the health risks of smoking, thinking about quitting, and cigarette forgoing, is highest after initial exposure, likely due to their novelty, and these reactions slowly diminish over a period of months or years.18,20–23 Consistent with one prior observational study with 4-month assessments over 2 years,20 we found small declines in cognitive elaboration as well as reinforcement attitudes, suggesting that the initial wear-out effects of pictorial and text-only warnings on psychosocial outcomes may begin to occur within weeks of first exposure; however, at least one other recent observational study22 reported increases in cognitive responses over the 2-year study period. Our results also suggest that the effect of pictorial warnings on behavioral outcomes may be more robust over time; cigarette forgoing increased over time in both our randomized clinical trial and the observational study by Swayampakala et al.22 As suggested by the message impact framework, reactions and changes in cognitions related to the warning are hypothesized to occur before changes smoking behavior;5 it is plausible that over the four follow-up weeks, participants continue to internalize the health warning message leading to sustained behavioral changes. To combat warning wear-out, the 2009 Family Smoking Prevention and Tobacco Control Act, which gave the US Food and Drug Administration (FDA) regulatory authority over cigarette warnings, stipulates that they be changed on a recurring basis in an effort to minimize wear-out resulting from repeated exposure to the same messages.32 Our study’s follow-up period limited our ability to extrapolate our results on changes in psychosocial and behavioral changes beyond 4 weeks; however, our results are in line with longer-term studies of warnings that also find that wear out effects occur with repeated exposure.
Our study had several strengths including the successful randomization that created two arms that did not differ with respect to participant characteristics, a large sample of current smokers, and low attrition over the 4-week study period. An additional strength of this study is the novelty of the research objectives, which aimed to characterize the short-term longitudinal changes associated with exposure to pictorial cigarette pack warnings relative to text-only warnings. To our knowledge, ours is the first study to experimentally examine the trajectories of these psychosocial and behavioral outcomes shortly after first exposure. Despite these strengths, several limitations should be noted. One limitation is that the labeling process may have drawn fresh attention to the current, and oft-ignored, cigarette text warnings, potentially resulting in an underestimation of the impact of pictorial warnings. Second, as with other studies of cigarette pack warnings, our study used self-reported measures. Some researchers have suggested the cross-validation of self-report data with other data such as fMRI and biomarkers, while others have noted that these approaches can be costly, resource-intensive, and burdensome to study participants.14 Third, correlations for the two-item cognitive elaboration subscales ranged from 0.62 to 0.80, which suggests that these scale items have only moderate scale reliability. Finally, the generalizability of our study findings to the general smoking population remains to be confirmed through additional studies. However, study participants were sampled from two states (NC andCA) with very different cultures regarding tobacco and included substantial proportions of poor; gay, lesbian, and bisexual, transgender; and black smokers,33 which helps extend the validity and generalizability of our findings given the wide range of tobacco acceptance across the two populations. Analyses previously reported showed that the warnings were equally effective among various groups and therefore, we did not a priori consider subgroup analyses; however, it should be noted that recently published observational research finds differing patterns of wear-out across sociodemographic groups, including differences by socioeconomic status and age.22 Future research should consider these trajectories across various subgroups.
Future research should continue to investigate the period of wear-out for pictorial cigarette warnings. In particular, research is needed that examines wear-out trajectories over the longer term, but with assessments frequent enough to pinpoint the optimal time for warning rotation. Reasons for such research include that the rates of decline we observed in negative affective reactions in the intervention group compared with the control group were small, and that some observational studies conducted over longer time-periods,21,22 but not all,20,23 report non-linear changes in warning effectiveness. Future research should also examine wear-out as related to the characteristics of warning imagery, which may vary in effectiveness.16 Important groups to study include nonsmokers who may have more limited exposure to cigarette pack warnings as well as youth who are susceptible to smoking.34 Important settings for future research include countries that have already implemented pictorial or text-only warnings or where other anti-smoking campaigns accompany the warnings. Indeed, cigarette pack warnings may have synergistic effects when combined with other coordinated anti-smoking multi-media campaigns.19 Our trial exposed each smoker to a single warning which may underestimate the warnings’ impact when used in a real-world setting. In practice, countries simultaneously adopt several pictorial warnings to create novelty and avoid wear-out over months and years. Understanding these trajectory patterns may help to inform tobacco regulatory policies and campaigns.
The impact of pictorial cigarette pack warnings on emotions and cognitions may wane over time. In contrast, quit intentions and forgoing may continue to increase, at least during the initial period after introduction. Rotation of pictorial warnings may help prevent warning wear-out.
Funding
This work was supported by The National Cancer Institute and FDA Center for Tobacco Products (CTP) under award number P30 CA016086-38S2. The National Institute of Environmental Health Sciences (grant number T32 ES007018) supported HP’s time writing the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Declaration of Interests
None of the authors have received funding from tobacco product manufacturers. The authors declare no conflicts of interest.
Acknowledgements
The authors thank the research participants for taking part in our trial. The authors also thank staff at the Pacific Institute for Research and Evaluation, staff at Ewald and Wasserman, Trent Johnson, Laura Bach, and Jennifer MacKinnon, for assistance with the trial.
References
- 1. Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults — United States, 2005–2015. MMWR Morb Mortal Wkly Rep. 2016;65:1205–1211. https://www.cdc.gov/mmwr/volumes/65/wr/mm6544a2.htm?s_cid=mm6544a2_w. Accessed April 12, 2017. [DOI] [PubMed] [Google Scholar]
- 2. US Department of Health and Human Services. The Health Consequences of smoking—50 Years of Progress: A Report of the Surgeon General.Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 3. Hammond D, Fong GT, McDonald PW, Cameron R, Brown KS. Impact of the graphic Canadian warning labels on adult smoking behaviour. Tob Control. 2003;12(4):391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Borland R. Tobacco health warnings and smoking-related cognitions and behaviours. Addiction. 1997;92(11):1427–1435. http://www.ncbi.nlm.nih.gov/pubmed/9519486. Accessed April 11, 2017. [PubMed] [Google Scholar]
- 5. Noar SM, Hall MG, Francis DB, Ribisl KM, Pepper JK, Brewer NT. Pictorial cigarette pack warnings: a meta-analysis of experimental studies. Tob Control. 2016;25(3):341–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Malouff JM, Schutte NS, Rooke SE, MacDonell G. Effects on smokers of exposure to graphic warning images. Am J Addict. 2012;21(6):555–557. [DOI] [PubMed] [Google Scholar]
- 7. Noar SM, Francis DB, Bridges C, Sontag JM, Brewer NT, Ribisl KM. Effects of strengthening cigarette pack warnings on attention and message processing. Journal Mass Commun Q. October 2016:1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Noar SM, Francis DB, Bridges C, Sontag JM, Ribisl KM, Brewer NT. The impact of strengthening cigarette pack warnings:systematic review of longitudinal observational studies. Soc Sci Med. 2016;164:118–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brewer NT, Hall MG, Noar SM, et al. Effect of Pictorial Cigarette Pack Warnings on Changes in Smoking Behavior: A Randomized Clinical Trial. JAMA Intern Med. 2016;176(7):905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li L, Borland R, Yong H, et al. Longer term impact of cigarette package warnings in Australia compared with the United Kingdom and Canada. Health Educ Res. 2015;30(1):67–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fong GT, Hammond D, Hitchman SC. The impact of pictures on the effectiveness of tobacco warnings. Bull World Health Organ. 2009;87(8):640–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. LeDoux J. Emotion, memory and the brain. The neural routes underlying the formation of memories about primitive emotional experiences, such as fear, have been traced. Sci Am. 1994;270(6):50–57. [DOI] [PubMed] [Google Scholar]
- 13. Andersen PA. Nonverbal Communication. Forms and Functions.Long Grove, Ill: Waveland Press, Inc; 2008. [Google Scholar]
- 14. Thrasher JF, Carpenter MJ, Andrews JO, et al. Cigarette warning label policy alternatives and smoking-related health disparities. Am J Prev Med. 2012;43(6):590–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thrasher JF, Villalobos V, Szklo A, et al. Assessing the impact of cigarette package health warning labels: a cross-country comparison in Brazil, Uruguay and Mexico. Salud Publica Mex. 2010;52(Suppl 2):S206–S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nonnemaker J, Farrelly M, Kamyab K, Busey A, Mann N.. Experimental Study of Graphic Cigarette Warning Labels: Final Results Report.Rockville, MD; 2010. http://www.tobaccolabels.ca/wp/wp-content/uploads/2013/12/USA-2010-Experimental-Study-of-Graphic-Cigarette-Warning-Labels-Final-Results-Report-FDA.pdf. [Google Scholar]
- 17. Calder BJ, Sternthal B. Television Commercial Wearout: An Information Processing View. J Mark Res. 1980;17(2):173. [Google Scholar]
- 18. Hammond D, Fong GT, Borland R, Cummings KM, McNeill A, Driezen P. Text and graphic warnings on cigarette packages: findings from the international tobacco control four country study. Am J Prev Med. 2007;32(3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Strahan EJ, White K, Fong GT, Fabrigar LR, Zanna MP, Cameron R. Enhancing the effectiveness of tobacco package warning labels: a social psychological perspective. Tob Control. 2002;11(3):183–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hitchman SC, Driezen P, Logel C, Hammond D, Fong GT. Changes in effectiveness of cigarette health warnings over time in Canada and the United States, 2002-2011. Nicotine Tob Res. 2014;16(5):536–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Thrasher JF, Abad-Vivero EN, Huang L, et al. Interpersonal communication about pictorial health warnings on cigarette packages:policy-related influences and relationships with smoking cessation attempts. Soc Sci Med. 2016;164:141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Swayampakala K, Thrasher JF, Yong H-H, et al. Over-time impacts of pictorial health warning labels and their differences across smoker subgroups: results from adult smokers in Canada and Australia. Nicotine Tob Res. 2017; doi: 10.1093/ntr/ntx134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thrasher JF, Swayampakala K, Cummings KM, et al. Cigarette package inserts can promote efficacy beliefs and sustained smoking cessation attempts:a longitudinal assessment of an innovative policy in Canada. Prev Med. 2016;88:59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brandon TH, Baker TB. The Smoking Consequences Questionnaire: the subjective expected utility of smoking in college students. Psychol Assess. 1991;3(3):484–491. [Google Scholar]
- 25. Keller PA, Block LG. Increasing the persuasiveness of fear appeals: the effect of arousal and elaboration. J Consum Res. 1996;22(4):448–459. [Google Scholar]
- 26. Leshner G, Bolls P, Wise K. Motivated processing of fear appeal and disgust images in televised anti-tobacco ads. J Media Psychol Theor MethodsAppl. 2011;23(2):77–89. [Google Scholar]
- 27. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. [DOI] [PubMed] [Google Scholar]
- 28. Klein WM, Zajac LE, Monin MM. Worry as a moderator of the association between risk perceptions and quitting intentions in young adult and adult smokers. Ann Behav Med. 2009;38(3):256–261. [DOI] [PubMed] [Google Scholar]
- 29. Li L, Borland R, Fong GT, et al. Smoking-related thoughts and microbehaviours, and their predictive power for quitting. Tob Control. 2015;24(4):354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wolfinger R, Chang M. Comparing the SAS ® GLM and MIXED Procedures for Repeated Measures http://www.ats.ucla.edu/stat/sas/library/mixedglm.pdf. Accessed April 27, 2017.
- 31. Hammond D, Fong GT, McDonald PW, Brown KS, Cameron R. Graphic Canadian cigarette warning labels and adverse outcomes: evidence from Canadian smokers. Am J Public Health. 2004;94(8):1442–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. United States Public Laws. Family Smoking Prevention and Tobacco Control Act of 2009. United States 111th Congress, 1st Session. Public Law 111–31; 2009. [Google Scholar]
- 33. Brodar K, Hall M, Butler E, et al. Recruiting diverse smokers: enrollment yields and cost. Int J Environ Res Public Health. 2016;13(12):1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Peebles K, Hall MG, Pepper JK, Byron MJ, Noar SM, Brewer NT. Adolescents’ responses to pictorial warnings on their parents’ cigarette packs. J Adolesc Health. 2016;59(6):635–641. [DOI] [PMC free article] [PubMed] [Google Scholar]