A 60-year-old man was referred for endoscopic ablation therapy of long-segment Barrett’s esophagus with low-grade dysplasia. It is our practice to perform preablation therapy mapping, with EMR of areas of concern, before ablation therapy. On this examination, we found a long segment of Barrett’s esophagus that was Prague class C5M6 (Fig. 1A). No concerning areas were seen on high-definition white-light endoscopy (HDWLE) or narrow-band imaging (NBI) (Fig. 1B). It is our practice to perform volumetric laser endomicroscopy (VLE) for all preablation mapping examinations to determine whether there are any areas of concern for neoplasia.
Figure 1.
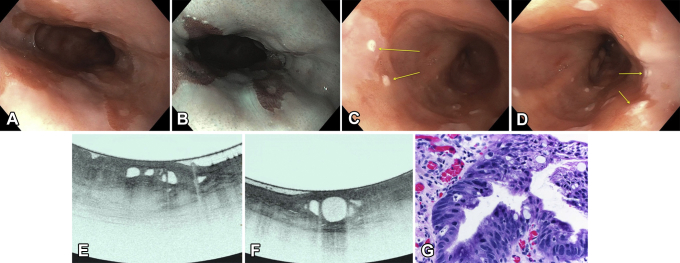
A, Long-segment Barrett’s esophagus without any focal abnormalities concerning for dysplasia. B, The long-segment Barrett’s esophagus examined on narrow-band imaging without any focal abnormalities concerning for dysplasia. C, Laser marks (yellow arrows) placed over a concerning area within the Barrett’s segment. D, Laser marks (yellow arrows) placed over a second area of concern within the Barrett’s segment. E, Volumetric laser endomicroscopic image showing partial effacement and more than 5 atypical glands. F, Volumetric laser endomicroscopic image showing atypical glands and a dark surface intensity. G, Histologic appearance of the first targeted area within the Barrett’s segment showing high-grade dysplasia (H&E, orig. mag. × 400).
The VLE technique is a second-generation optical coherence tomography technology that uses infrared light to produce real-time high-resolution cross-sectional imaging of tissue. It has been cleared by the U.S. Food and Drug Administration for use in the GI tract and is currently marketed to aid in dysplasia detection in Barrett’s esophagus. VLE can scan a 6-cm length of the esophagus in approximately 90 seconds, providing high-resolution wide-field microstructure cross-sectional imaging. Ex-vivo scoring systems have been developed to look at VLE features of dysplasia (Video 1, available online at www.VideoGIE.org).
The VLE was performed by use of a 20-mm balloon (Video 1). Two areas were identified that were of concern for neoplasia. Both were marked with laser marking (Figs. 1C and D). The first area had partial effacement of layers and atypical glands (Fig. 1E), whereas the second area had atypical glands and a dark surface intensity (Fig. 1F). Given the concerning features, EMR was performed. The results of histologic analysis were consistent with high-grade dysplasia in both resection specimens (Fig. 1G).
This video demonstrates that VLE can help aid in the detection of dysplasia in Barrett’s esophagus even when HDWLE or NBI do not show any areas of concern. Studies are needed to show the incremental yield of dysplasia detection using VLE, in-vivo diagnostic accuracy, in-vivo classification for neoplasia associated with Barrett’s esophagus, and cost utility.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Patient undergoing volumetric laser endomicroscopy with laser marking that targeted nonvisible Barrett’s neoplasia.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient undergoing volumetric laser endomicroscopy with laser marking that targeted nonvisible Barrett’s neoplasia.