Abstract
Strengths-based strategies to reduce youth violence in low-resource urban communities are urgently needed. Supportive adolescent-adult relationships may confer protection, but studies have been limited by self-reported composite outcomes. We conducted a population-based case-control study among 10- to 24-year-old males in low-resource neighborhoods to examine associations between supportive adult connection and severe assault injury. Cases were victims of gunshot assault injury (n = 143) and non-gun assault injury (n = 206) from two level I trauma centers. Age- and race-matched controls (n = 283) were recruited using random digit dial from the same catchment. Adolescent-adult connections were defined by: (1) brief survey questions and (2) detailed family genograms. Analysis used conditional logistic regression. There were no significant associations between positive adult connection, as defined by brief survey questions, and either gunshot or non-gun assault injury among adolescents with high prior violence involvement (GSW OR = 2.46, 95% CI 0.81–7.49; non-gun OR = 1.59, 95% CI 0.54–4.67) or low prior violence involvement (GSW OR = 0.92, 95% CI 0.34–2.44; non-gun OR = 1.96, 95% CI 0.73–5.28). In contrast, among adolescents with high levels of prior violence involvement, reporting at least one supportive adult family member in the family genogram was associated with higher odds of gunshot assault injury (OR = 4.01, 95% CI 1.36–11.80) and non-gun assault injury (OR = 4.22, 95% CI 1.48–12.04). We were thus unable to demonstrate that positive adult connections protected adolescent males from severe assault injury in this highly under-resourced environment. However, at the time of injury, assault-injured adolescents, particularly those with high prior violence involvement, reported high levels of family support. The post-injury period may provide opportunities to intervene to enhance and leverage family connections to explore how to better safeguard adolescents.
Electronic supplementary material
The online version of this article (10.1007/s11524-018-0260-8) contains supplementary material, which is available to authorized users.
Keywords: Youth violence, Violence victimization, Adult support, Family connection, Case-control
Introduction
Homicide is the leading cause of death among African American adolescent males, with youth in low-resource urban neighborhoods bearing a disproportionate burden of violent victimization [1–3]. In a sample of Philadelphia youth, 54% reported direct violent victimization, with 40% beaten up and 5% shot during their lifetime [4]. Historically, most interpersonal violence prevention research has focused on identifying and eliminating risk factors for violence; however, more recent work demonstrates the importance of strengths-based strategies to protect adolescents from violence [5].
Adolescent-adult connections, both within family networks and with other adult mentors, promote healthy adolescent development and are associated with lower levels of violence involvement [6–12]. Research examining the role of adult connection in violence prevention among adolescents in under-resourced urban neighborhoods has relied on self-reported violence exposure and often suggests that families struggle to protect youth in these contexts [13–15]. However, other research demonstrates inverse associations between family functioning and support and experiencing or witnessing violence [16, 17]. Given the disproportionate burden of violence experienced by adolescent males living in low-resource urban communities, further study of the potentially protective role of adolescent-adult relationships is warranted. Adolescent-adult relationship theories suggest that relationships and their impact on behavior may change across adolescence [18, 19]. Examining whether associations between adult connections and violent injury vary by age may identify age-specific intervention opportunities. This study, to the best of our knowledge, is the first to use objective measures of assault injury to examine associations between supportive adult connections and violent victimization among male adolescents ages 10–24 in low-resource neighborhoods.
Methods
Overview
We conducted a population-based case-control study among adolescent males to determine associations between adolescent-adult connections and assault injury.
Participants
Case participants were adolescent males, ages 10 to 24, who sustained an assault injury from interpersonal violence and sought care at two level I trauma centers in Philadelphia, PA. Cases were recruited into two participant groups by injury type: (1) gunshot assault injury and (2) non-gunshot assault injury (e.g., fracture, laceration) from 2007 to 2011. Adolescent male controls were recruited using random digit dial from residences in the 12 zip codes accounting for the homes of case subjects [20–22], matched to gunshot cases on age group (10–14, 15–17, and 18–24 years) and race, and used as the comparison group for both the gunshot and non-gunshot case groups. The response rate for controls (52.8%) was similar to other contemporaneous random-sample surveys and suggested enrollment of a reasonably representative sample from the catchment [23, 24]. Female youth were excluded due to low prevalence of female gunshot injury victims at the study sites [25].
Study participants were enrolled using written informed consent for those age 18 or greater, and participant assent with parental permission for minors. Other design considerations were previously described [26, 27]. The study was approved by the University of Pennsylvania and The Children’s Hospital of Philadelphia Institutional Review Boards.
Data Source
All participants underwent a structured in-person interview, led by a trained research coordinator, in the hospital, study office, or their home based on participant preference. Interviews covered violence exposure, school performance, adult and peer connections, and substance use. Case participant interviews occurred within 2 weeks following assault injury.
Measuring Connections
Adolescent-adult connections were defined using two distinct approaches. First, positive adult connection was defined by answering two questions affirmatively: “there are adults in my life that I look up to” and “there are adults in my life that I can go to that help me handle tough situations.” Motivated by prior research demonstrating the importance of both family and external supports [6, 12], these two questions were chosen to broadly and succinctly capture connections both within the family and with other supportive adults. Second, participants created detailed genograms to individually characterize the nature of relationships with adult family members who play an important role in their lives. They used a constellation of pre-specified and participant-generated terms to define relationships (e.g., verbal fighting, supportive, “always there for me”). Relationships were subsequently divided into two categories: supportive and unsupportive based on the constellation of terms reported by youth. Details of the classification method have been previously described [17]. Supportive adult familial connection and supportive parental connection were defined by the presence of ≥ 1 supportive adult family member(s) and by the specific presence of ≥ 1 supportive parent(s), respectively, in family genograms.
Statistical Analysis
Gun assault and non-gun assault cases were separately compared to controls using conditional logistic regression to account for matching controls to cases on age group strata during enrollment [28, 29]. We modeled crude and adjusted associations between: (1) positive adult connection, (2) supportive adult familial connection, and (3) supportive parental connection, and assault injury. Due to presence of effect modification, we stratified adjusted models on high versus low levels of self-reported previous violence involvement, defined by seven survey questions (Supplementary Table 1) coded into two categories (low: ≤ 3 vs. high: > 3). We tested for and found no evidence of effect modification or residual confounding by age, and thus, both age-related variables were excluded from final models.
Additional individual-level variables specified a priori were assessed for evidence of confounding including: school enrollment, school grades, history of school suspension, perceived school safety, involvement in organized activities, current employment, tobacco use, alcohol use, marijuana use, history of probation, witnessing violence, and perceived neighborhood disarray. Supplementary Table 2 provides associations between individual-level covariates and adult connections. We entered covariates into the multivariable model with bivariate p < 0.25 and retained those with p < 0.25 in the adjusted model, or if removing them altered odds ratios of interest by > 10% [30]. We additionally assessed multivariable models for evidence of collinearity. We identified collinearity between tobacco, alcohol, and marijuana use variables as well as between history of suspension and history of probation. Alcohol and history of probation were retained based on the strength of associations with assault injury outcomes. Final analyses adjusted for school enrollment (yes/no), perceived school safety (low/high), involvement in organized activities (yes/no), current employment (yes/no), alcohol use (any lifetime history), history of probation (yes/no), and perceived neighborhood disarray (continuous, range 0–20) (Neighborhood Environment Scale) [31].
Propensity scores were used to efficiently control for multiple features of the participants’ neighborhood context, as defined by home address (median household income, unemployment, % college-educated, racial and ethnic composition, population density, crime density, alcohol outlets, vacant properties, municipal services, and collective efficacy) using data from the 2010 US Census [32], the Philadelphia Police Department, the University of Pennsylvania Cartographic Modeling Lab, and the Philadelphia Health Management Corporation’s Southeastern Pennsylvania Household Survey [33]. Propensity score quartiles were included as a categorical covariate in adjusted models. Missing data (0–7%) was managed with multiple imputation (m = 20). Final adjusted models were tested for collinearity and all variance inflation factors were < 2.5. Statistical tests were two-tailed and α < 0.05 was used as the significance threshold. Analyses were conducted using STATA version 14.0 (College Station, TX).
We conducted sensitivity analyses to assess the potential impact of misclassification bias on our observed associations between adolescent-adult connections and assault injury [34, 35]. We were particularly focused on whether data collection methods inherent to case-control studies, wherein cases were interviewed immediately following an assault injury, may have impacted perceptions of adolescent-adult support. We therefore purposely recoded the exposure status of case participants who identified adult connections to not having identified these supports. We varied the percent recoded from 5 to 40%, re-ran 100 bootstrapped samples at each percent misclassification, and averaged the results to produce mean biased odds ratios.
Results
Characteristics of Participants
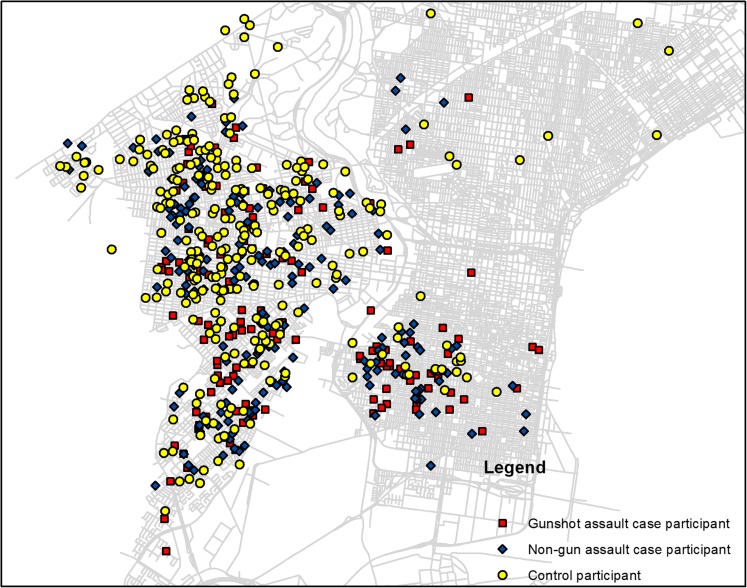
We enrolled 143 gun assault-injured case participants, 206 non-gun assault-injured case participants, and 283 control participants from the 250, 396, and 486 eligible adolescent males who were recruited for study participation. Median participant age was 19.8 years for gun assault-injured cases, 15.8 years for non-gun assault-injured cases, and 18.6 years for controls. The majority of participants was African American (99, 97, and 87%, for the three groups, respectively). Levels of prior violence involvement were similar across the case and control groups; all three groups reported a median 3 out of 7 possible types of prior victimization/perpetration. Positive adult connection, as measured through two interview questions, was common among all three groups (86% of gun cases, 92% of non-gun cases, and 86% of controls). Additional individual and neighborhood contextual factors are summarized in Table 1. The home address locations of case and control participants are depicted in Fig. 1 and have been randomly jittered to protect confidentiality. The address locations demonstrate excellent geographical overlap between case and control participants, as expected with population-based sampling from the 12 selected zip codes.
Table 1.
Characteristics of participants
| Characteristic | Gunshot assault victims (n = 143) | Non-gun assault victims (n = 206) | Controls (n = 283) |
|---|---|---|---|
| Individual | |||
| Age, years, median (IQR) | 19.8 (18.3, 21.6) | 15.8 (14.0, 18.2) | 18.6 (15.8, 20.8) |
| Race | |||
| African American | 96.8% | 87.8% | 98.5% |
| Caucasian | 0.8% | 7.7% | 1.1% |
| Hispanic | 0.8% | 1.5% | 0.0% |
| Asian/Pacific Islander | 1.6% | 3.1% | 0.0% |
| Native American | 0.0% | 0.0% | 0.4% |
| Currently enrolled in school | 42.4% | 82.7% | 67.9% |
| Received good grades (A/Bs) | 27.8% | 43.9% | 39.1% |
| Ever suspended or expelled | 80.2% | 71.9% | 69.0% |
| Currently working | 32.5% | 20.5% | 35.8% |
| Participating in structured activities | 66.7% | 53.7% | 72.4% |
| Ever drank alcohol | 71.4% | 46.9% | 65.3% |
| Ever used marijuana | 68.3% | 34.2% | 45.0% |
| Ever been jumped | 55.2% | 71.3% | 56.1% |
| Ever in a fistfight | 93.7% | 94.9% | 91.9% |
| Ever been to hospital because of a fight | 19.8% | 30.1% | 12.8% |
| Ever carried a weapon | 47.6% | 26.0% | 39.1% |
| Ever been on juvenile probation | 53.2% | 20.5% | 17.7% |
| Neighborhood context (home address) | |||
| Median household income, median ($) | 24,359 | 25,343 | 25,424 |
| Median unemployed population per 1000 residents ≥ 16 | 81.7 | 79.7 | 74.3 |
| Median population per 1000 residents with at least some college education | 170.7 | 176.1 | 187.3 |
| Median black population per 1000 residents | 947.5 | 945.3 | 966.5 |
| Median Hispanic population per 1000 residents | 15.4 | 16.3 | 14.6 |
| Median vacant properties per square mile | 661.8 | 503.5 | 458.63 |
| Median annual narcotics arrests | 349.1 | 332.9 | 328.1 |
| Median annual vandalism arrests | 323.8 | 350.6 | 308.8 |
IQR interquartile range
Fig. 1.
Case and control participant home address locations. *All participant locations have been jittered by a randomly assigned distance between 200 and 1200 ft in both latitude and longitude to protect participant confidentiality
Association between Positive Adult Connection and Assault Injury
In adjusted models, there were no significant associations between positive adult connection and gunshot assault injury (GSW OR = 2.46; 95% CI 0.81, 7.49) or non-gun assault injury (OR = 1.59; 95% CI 0.54, 4.67) among youth with high prior violence involvement. Among youth with low prior violence involvement, the associations between positive adult connection and gunshot assault injury (OR = 0.92; 95% CI 0.34, 2.44) and non-gun assault injury (OR = 1.96; 95% CI 0.73, 5.28) also did not reach statistical significance (Table 2). Supplementary Tables 3 and 4 provide model parameters for all included covariates.
Table 2.
Associations between adolescent-adult connections and assault injury
| Gunshot assault injury | Non-gun assault injury | |||
|---|---|---|---|---|
| Measure of connection | OR (95%CI)* p value |
AOR (95%CI)** p value |
OR (95%CI)* p value |
AOR (95%CI)** p value |
| Positive adult connection | 1.23 (0.66, 2.28) p = 0.52 |
1.44 (0.75, 2.77) p = 0.28 |
||
| Low prior violence involvement | 0.92 (0.34, 2.44) | 1.96 (0.73, 5.28) | ||
| p = 0.86 | p = 0.18 | |||
| High prior violence involvement | 2.46 (0.81, 7.49) | 1.59 (0.54, 4.67) | ||
| p = 0.11 | p = 0.40 | |||
| Supportive adult familial connection | 1.96 (1.03, 3.73) p = 0.04 |
1.91 (1.09, 3.34) p = 0.03 |
||
| Low prior violence involvement | 1.43 (0.53, 3.86) | 1.19 (0.55, 2.55) | ||
| p = 0.48 | p = 0.66 | |||
| High prior violence involvement | 4.01 (1.36, 11.80) | 4.22 (1.48, 12.04) | ||
| p = 0.01 | p = 0.007 | |||
| Supportive parental connection | 1.67 (0.89, 3.13) p = 0.11 |
1.69 (0.98, 2.91) p = 0.06 |
||
| Low prior violence involvement | 1.19 (0.46, 3.06) | 1.21 (0.58, 2.53) | ||
| p = 0.72 | p = 0.60 | |||
| High prior violence involvement | 3.00 (1.01, 8.95) | 2.86 (1.02, 7.97) | ||
| p = 0.049 | p = 0.045 | |||
OR odds ratio, AOR adjusted odds ratio, CI confidence interval
*Odds ratio from conditional logistic regression matched on age group strata
**Adjusted odds ratio from conditional logistic regression matched on age group strata, stratified by self-reported previous violence involvement (low: ≤ 3 vs. high:> 3), and adjusted for individual factors (school enrollment, perceived school safety, involvement in activities, employment, alcohol use, history of probation), perceived neighborhood disarray, and neighborhood context (median household income, % unemployment, % college-educated, racial and ethnic composition, population density, crimes per square mile, alcohol outlets, vacant properties, municipal services, and collective efficacy)
Association between Supportive Adult Familial Connection and Assault Injury
Among youth with high prior violence involvement, identifying at least one supportive adult family member in the family genogram was associated with higher odds of gunshot assault injury (OR = 4.01; 95% CI 1.36, 11.80) and non-gun assault injury (OR = 4.22; 95% CI 1.48, 12.04). Among youth with low prior violence involvement, there were no significant associations between reporting a supportive relationship with at least one adult family member and the odds of gunshot assault injury (OR = 1.43; 95% CI 0.53, 3.86) or non-gun assault injury (OR = 1.19; 95% CI 0.55, 2.55) ( Table 2, Supplementary Tables 3 and 4).
Association between Supportive Parental Connection and Assault Injury
Among youth with high prior violence involvement, significant direct associations between reporting at least one supportive parent and gunshot assault injury (OR = 3.00; 95% CI 1.01, 8.95) and non-gun assault injury (OR = 2.86; 95% CI 1.02, 7.97) emerged. Among youth with low prior violence involvement, there were no significant associations between the odds of gunshot assault injury (OR = 1.19; 95% CI 0.46, 3.06) or non-gun assault injury (OR = 1.21, 95% CI 0.58, 2.53) and reporting a supportive relationship with at least one parent (Table 2, Supplementary Tables 3 and 4).
Sensitivity Analysis
Among youth with low prior violence involvement, randomly recoding 5% of case participants who identified connections to not having these connections resulted in all mean biased odds ratios of the associations between adult connections and assault being < 1 (Table 3). Among youth with high prior violence involvement, higher percentages of random misclassification were required before mean biased odds ratios were < 1. Among youth with high prior violence involvement, 10–15% exposure miscoding for positive adult connection and 20–30% exposure miscoding for supportive familial connection and supportive parental connection were required before mean biased odds ratios were < 1.
Table 3.
Sensitivity analysis
| % of case participants with connections randomly recoded to not having specified connections (OR = odds ratio) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Low prior violence involvement | 0% | 5% | 10% | 15% | 20% | 25% | 30% | 35% | 40% |
| Gunshot assault injury | |||||||||
| Positive adult connection | 0.92 | 0.63 | 0.47 | 0.35 | 0.27 | 0.22 | 0.18 | 0.14 | 0.12 |
| Supportive adult familial connection | 1.43 | 0.98 | 0.72 | 0.56 | 0.44 | 0.35 | 0.28 | 0.23 | 0.19 |
| Supportive parental connection | 1.19 | 0.89 | 0.69 | 0.55 | 0.44 | 0.37 | 0.30 | 0.26 | 0.21 |
| Non-gun assault injury | |||||||||
| Positive adult connection | 1.96 | 0.99 | 0.62 | 0.44 | 0.32 | 0.25 | 0.20 | 0.16 | 0.13 |
| Supportive adult familial connection | 1.19 | 0.81 | 0.61 | 0.47 | 0.37 | 0.30 | 0.24 | 0.20 | 0.17 |
| Supportive parental connection | 1.21 | 0.89 | 0.68 | 0.54 | 0.43 | 0.36 | 0.30 | 0.24 | 0.20 |
| High prior violence involvement | |||||||||
| Gunshot assault injury | |||||||||
| Positive adult connection | 2.46 | 1.67 | 1.20 | 0.93 | 0.73 | 0.57 | 0.46 | 0.37 | 0.31 |
| Supportive adult familial connection | 4.01 | 2.93 | 2.21 | 1.70 | 1.33 | 1.09 | 0.90 | 0.73 | 0.60 |
| Supportive parental connection | 3.00 | 2.33 | 1.83 | 1.46 | 1.20 | 0.98 | 0.79 | 0.68 | 0.56 |
| Non-gun assault injury | |||||||||
| Positive adult connection | 1.59 | 1.10 | 0.82 | 0.62 | 0.50 | 0.40 | 0.32 | 0.26 | 0.22 |
| Supportive adult familial connection | 4.22 | 2.96 | 2.13 | 1.63 | 1.30 | 1.05 | 0.87 | 0.70 | 0.58 |
| Supportive parental connection | 2.86 | 2.15 | 1.71 | 1.35 | 1.13 | 0.93 | 0.77 | 0.67 | 0.55 |
Discussion
In a sample of male adolescents living in low-resource neighborhoods in Philadelphia, both assault-injured and control participants reported high levels of adult support. Youth with high levels of prior violence involvement who reported supportive relationships with at least one adult family member and/or with at least one parent had increased odds of gun assault and non-gun assault injury. At first glance, this finding is surprising as adult connection, and particularly positive parental connection, is known to be protective for so many behaviors and varied contexts [5, 6, 36–40]. In fact, our own prior work with control participants from the current study demonstrated significant protective associations between positive adult connection and self-reported violence involvement and witnessing, as well as between supportive adult familial connection and self-reported violence involvement [17, 41]. Here, however, we were unable to demonstrate that positive adult and family connections protected adolescents from objectively measured severe assault injury in these highly under-resourced urban environments. It is important that we are thoughtful about the potential implications of these associations rather than draw erroneous conclusions such as suggesting that a positive parental connection contributes to greatest risk for violence.
The current work extends prior knowledge by assessing objective rather than self-reported measures of assault injury and focusing on severe assault injury, including gunshot injury. The fact that results differ markedly across our own previous studies [17, 41] and the current study based on utilizing self-reported or objectively measured outcomes, as well as the severity of violence outcomes studied, demonstrates the need for research that employs a diversity of rigorous methods to better understand the nuanced associations between adult connections and violence in low-resource urban neighborhoods. The current findings may also suggest that having been a recent victim of violence changes the way someone perceives, reports, or experiences meaningful family and/or parental connections and highlights the need for longitudinal studies to ascertain directionality.
Our current findings are in keeping with prior literature in low-resource urban settings, which demonstrates that families often struggle to protect adolescents in the context of high levels of neighborhood violence [13–15]. It may be that even protective, caring connections between adults and youth are unable to mitigate the risks regarding severe violent injury in our most under-resourced urban communities. In other words, even though families and other adults play a vital role in supporting and safeguarding adolescents, our findings argue for a need for broad interventions designed to address environmental contextual factors that put youth in low-resource neighborhoods at unacceptably high risk for violence victimization [8, 42, 43]. Low-cost place-based interventions have been associated with decreases in violent crime and may be a critical part of a multi-faceted approach to combating youth violence [44–48]. Understanding the joint role of adult support-focused and place-based interventions may provide critical opportunities to prevent violent injuries in these low-resource contexts.
Rather than a broadly defined adult connection conferring protection, it is possible that more nuanced characteristics of the type and quality of relationships and individual characteristics of adult supports are most closely linked to violent injury prevention. Prior research has shown that the nature of connections (e.g., extended family member versus community-based mentor) as well as the strength of emotional bonds are linked to youth outcomes [49]. Having adult supports who themselves engage in problem behaviors may be linked to youth violence involvement [50]. Attitudes towards violence among youth’s supports and the degree to which these adults sanction risk behaviors may be important mediators of the observed associations [51, 52]. The observed direct associations between supportive familial connection and violent injury may thus, in part, be due to limited pro-social connections.
It is also possible that the nature of case-control studies, wherein exposure status is ascertained after outcomes occur, may explain the observed associations. In our study, assault-injured adolescents were asked to report on the quality of adolescent-adult connections in the immediate post-injury period (within 1–2 weeks following injury). Control participants, in contrast, were asked to report on connections on a random, presumably uneventful day. Suffering a severe assault injury may fundamentally alter the way that youth perceive and classify adolescent-adult connections, and make it challenging to compare responses between case and control participants. Sensitivity analyses revealed that a relatively small degree of exposure misclassification among cases could explain the observed findings.
The experience of suffering a violent assault injury may also garner protective positive connections from parents and family members, suggesting a critical moment for intervention. In other words, the direct associations uncovered in this study between connection and violent injury may actually reveal the protective reaction of families in times of crisis. Our finding that assault-injured adolescents frequently report supportive family connections suggests that severe assault injury might have triggered families’ concentrated attention and protective mechanisms which, in turn, enhanced these youth’s sense of family connection. This may be particularly salient among youth with high levels of prior violence involvement, whose adult supports may appropriately increase resources in the post-injury period in attempt to break the cycle of violence. Rather than reflect a “misclassification,” adolescents’ characterizations of family relationships might reflect high levels of engagement they experience in the post-injury period. Thus, the post-injury period may present a critical time to intervene to enhance and sustain these connections and to explore how they can better safeguard youth.
One promising model of intervention is through hospital-based violence intervention programs (HVIP). These programs focus on engaging youth in the immediate post-injury period to reduce re-injury and recidivism. In HVIP models, interdisciplinary teams of physicians, case managers, social workers, psychologists, and community partners conduct comprehensive assessments, provide individualized case management, and assist with navigation to services. Research suggests such interventions can reduce future violence involvement and improve self-efficacy [53–57]. Specifically engaging with families through hospital-based violence intervention programs to promote and enhance adolescent-adult connections during the immediate post-injury period may play a critical role in reducing the consequences of violence exposure and promoting pro-social development. This intervention strategy might be most salient for youth who have experienced high levels of prior violence involvement, and may afford an opportunity for family-centered engagement to break the cycle of violence.
The current study has several limitations. Nonparticipation bias among cases and/or controls could impact results. Youth with more supportive caregivers may be more likely to be brought to the Emergency Department for injuries. Our objective measure of assault injury thus could also reflect medical service utilization, with the case group being enriched with supportive adults who are more likely to encourage youth to seek care. However, the magnitudes of the observed associations were similar for gun and non-gun assault injuries, reducing the likelihood that differential care utilization alone explains the direct associations between connections and injury since nearly all youth with gunshot injuries seek care, regardless of support systems. Additionally, despite use of rigorous methods to ensure population-based sampling of controls, selection bias is nonetheless possible. We controlled for multiple potential confounders at the individual and neighborhood contextual levels. However, as with all observational research, the potential for bias due to unmeasured confounding remains.
Measuring adolescent-adult relationships during a single in-person interview may not accurately capture the dynamic nature of relationships, and does not account for how adult supports may have evolved over participants’ lifespans. We additionally did not have data on the quality of emotional support or whether relationships promoted pro-social norms, which may be important mediators of the observed associations. Asking youth to reflect on their perceptions of adult support immediately following a violent injury may also fundamentally alter youth perceptions among case participants. Our sensitivity analyses suggest that even somewhat small changes in relationship classifications could alter our observed findings. It is also possible that families rally to aid injured youth, and that the high levels of family support reflect fundamental shifts in relationships in the immediate post-injury period. Given that gunshot injury is a rare outcome among adolescent males, a case-control study is the most feasible and efficient means for studying adult connection and severe assault injury despite these limitations inherent in the design. Importantly, case-controls studies are observational, and observed associations must not be interpreted as causal.
Key strengths of this study include a population-based case-control design and multiple different measures of adolescent-adult connections. To the best of our knowledge, this is the first study to utilize objective measures of assault injury to study associations between adolescent-adult connections and severe violent injury among adolescent males in low-resource neighborhoods.
Conclusions
Male adolescents in low-resource urban neighborhoods bear a disproportionate burden of violent injury. Using a population-based case-control design, this is the first study to examine associations between adolescent-adult connections and objective measures of severe assault injury, including gunshot assault and non-gun assault. Among adolescents with low prior violence involvement, there were no significant associations between adult connections and violence-related injury. Among adolescents with high prior violence involvement, significant direct associations between supportive family connection and gun assault and non-gun assault injury emerged. We hypothesize that severe injury may have triggered families’ focused attention and protective mechanisms which enhanced these youths’ sense of family connection. The post-injury period may be a critical time to intervene to enhance and sustain these connections and to explore how strong family connections can better safeguard adolescents. Family-focused intervention strategies may be a useful component of a multi-faceted approach to reducing youth violence. Families’ ability to protect youth, however, may be limited in environmental contexts filled with multiple challenges, highlighting the need for broader place-based strategies.
Electronic supplementary material
(DOCX 18 kb)
Financial Disclosure
The authors have no financial relationships relevant to this article to disclose.
Funding
The study was supported by NIH grants F32 HD084028 and R01 AA014944.
References
- 1.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). Available at www.cdc.gov/injury. Accessed 15 Jan 2018.
- 2.Centers for Disease Control and Prevention. YRBSS Data, Questionnaires, & Documentation. http://www.cdc.gov/healthyyouth/data/yrbs/data.htm. Accessed 1 Nov 2017.
- 3.Hardaway CR, McLoyd VC, Wood D. Exposure to violence and socioemotional adjustment in low-income youth: an examination of protective factors. Am J Community Psychol. 2012;49(1–2):112–126. doi: 10.1007/s10464-011-9440-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonald CC, Deatrick JA, Kassam-Adams N, Richmond TS. Community violence exposure and positive youth development in urban youth. J Community Health. 2011;36(6):925–932. doi: 10.1007/s10900-011-9391-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Losel F, Farrington DP. Direct protective and buffering protective factors in the development of youth violence. Am J Prev Med. 2012;43(2 Suppl 1):S8–S23. doi: 10.1016/j.amepre.2012.04.029. [DOI] [PubMed] [Google Scholar]
- 6.Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, Tabor J, Beuhring T, Sieving RE, Shew M, Ireland M, Bearinger LH, Udry JR. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–832. doi: 10.1001/jama.1997.03550100049038. [DOI] [PubMed] [Google Scholar]
- 7.Resnick MD, Ireland M, Borowsky I. Youth violence perpetration: what protects? What predicts? Findings from the National Longitudinal Study of Adolescent Health. J Adolesc Health. 2004;35(5):424.e421–424.e410. doi: 10.1016/j.jadohealth.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, Currie C. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–1652. doi: 10.1016/S0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
- 9.Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- 10.Lerner RM, Lerner JV, von Eye A, Bowers EP, Lewin-Bizan S. Individual and contextual bases of thriving in adolescence: a view of the issues. J Adolesc. 2011;34(6):1107–1114. doi: 10.1016/j.adolescence.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Henrich CC, Brookmeyer KA, Shahar G. Weapon violence in adolescence: parent and school connectedness as protective factors. J Adolesc Health. 2005;37(4):306–312. doi: 10.1016/j.jadohealth.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 12.DuBois DL, Silverthorn N. Natural mentoring relationships and adolescent health: evidence from a national study. Am J Public Health. 2005;95(3):518–524. doi: 10.2105/AJPH.2003.031476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gorman-Smith D, Tolan P. The role of exposure to community violence and developmental problems among inner-city youth. Dev Psychopathol. 1998;10(01):101–116. doi: 10.1017/S0954579498001539. [DOI] [PubMed] [Google Scholar]
- 14.Miller LS, Wasserman GA, Neugebauer R, Gorman-Smith D, Kamboukos D. Witnessed community violence and antisocial behavior in high-risk, urban boys. J Clin Child Psychol. 1999;28(1):2–11. doi: 10.1207/s15374424jccp2801_1. [DOI] [PubMed] [Google Scholar]
- 15.Houltberg BJ, Henry CS, Morris AS. Family interactions, exposure to violence, and emotion regulation: perceptions of children and early adolescents at risk. Fam Relat. 2012;61(2):283–296. doi: 10.1111/j.1741-3729.2011.00699.x. [DOI] [Google Scholar]
- 16.Gorman-Smith D, Henry DB, Tolan PH. Exposure to community violence and violence perpetration: the protective effects of family functioning. J Clin Child Adolesc Psychol. 2004;33(3):439–449. doi: 10.1207/s15374424jccp3303_2. [DOI] [PubMed] [Google Scholar]
- 17.Culyba AJ, Ginsburg KR, Fein JA, Branas CC, Richmond TS, Miller E, et al. Examining the role of supportive family connection in violence exposure among male youth in urban environments. J Interpers Violence. 2016; 088626051664609. [DOI] [PMC free article] [PubMed]
- 18.Laursen B, Collins WA. Parent–child relationships during adolescence. In: Handbook of adolescent psychology. John Wiley & Sons, Inc.; 2009.
- 19.Carlivati J, Collins WA. Adolescent attachment representations and development in a risk sample. In: MO SM, editor. Attachment in adolescence Reflections and new angles. New Directions for Child and Adolescent Development. Jossey-Bass: San Francisco; 2007. pp. 91–106. [DOI] [PubMed] [Google Scholar]
- 20.Waksberg J. Sampling methods for random digit dialing. J Am Stat Assoc. 1978;73(361):40–46. doi: 10.1080/01621459.1978.10479995. [DOI] [Google Scholar]
- 21.Hartge P, Brinton LA, Rosenthal JF, Cahill JI, Hoover RN, Waksberg J. Random digit dialing in selecting a population-based control group. Am J Epidemiol. 1984;120(6):825–833. doi: 10.1093/oxfordjournals.aje.a113955. [DOI] [PubMed] [Google Scholar]
- 22.Perneger TV, Myers TL, Klag MJ, Whelton PK. Effectiveness of the Waksberg telephone sampling method for the selection of population controls. Am J Epidemiol. 1993;138(8):574–584. doi: 10.1093/oxfordjournals.aje.a116898. [DOI] [PubMed] [Google Scholar]
- 23.Baruch Y, Holtom BC. Survey response rate levels and trends in organizational research. Hum Relat. 2008;61(8):1139–1160. doi: 10.1177/0018726708094863. [DOI] [Google Scholar]
- 24.Groves R. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006;70(5):646–675. doi: 10.1093/poq/nfl033. [DOI] [Google Scholar]
- 25.Nance ML, Branas CC, Stafford PW, Richmond T, Schwab CW. Nonintracranial fatal firearm injuries in children: implications for treatment. J Trauma. 2003;55(4):631–635. doi: 10.1097/01.TA.0000035090.99483.0A. [DOI] [PubMed] [Google Scholar]
- 26.Basta LA, Richmond TS, Wiebe DJ. Neighborhoods, daily activities, and measuring health risks experienced in urban environments. Soc Sci Med. 2010;71(11):1943–1950. doi: 10.1016/j.socscimed.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wiebe DJ, Richmond TS, Guo W, Allison PD, Hollander JE, Nance ML, Branas CC. Mapping activity patterns to quantify risk of violent assault in urban environments. Epidemiology. 2016;27(1):32–41. doi: 10.1097/EDE.0000000000000395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greenland S, Moolgavkar SH. Partial and marginal matching in case control studies. In: Prentice RL, editor. Modern Statistical Methods in Chronic Disease Epidemiology. New York: Wiley; 1986. pp. 35–49. [Google Scholar]
- 29.King G, Zeng L. Estimating risk and rate levels, ratios and differences in case-control studies. Stat Med. 2002;21(10):1409–1427. doi: 10.1002/sim.1032. [DOI] [PubMed] [Google Scholar]
- 30.Hosmer DWLS, Sturdivant R. Applied Logistic Regression. 3. Hoboken, NJ: John Wiley & Sons, Inc.; 2013. [Google Scholar]
- 31.Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug Alcohol Depend. 1996;43(3):155–161. doi: 10.1016/S0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- 32.Census US. https://www.census.gov/geo/maps-data/data/tiger-line.html.
- 33.Philadelphia Health Management Corporation. Southeastern Pennsylvania Household Survey http://www.chdbdata.org/.
- 34.Fox MP, Lash TL, Greenland S. A method to automate probabilistic sensitivity analyses of misclassified binary variables. Int J Epidemiol. 2005;34(6):1370–1376. doi: 10.1093/ije/dyi184. [DOI] [PubMed] [Google Scholar]
- 35.Lyles RH, Lin J. Sensitivity analysis for misclassification in logistic regression via likelihood methods and predictive value weighting. Stat Med. 2010;29(22):2297–2309. doi: 10.1002/sim.3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Theokas C, Lerner RM. Observed ecological assets in families, schools, and neighborhoods: conceptualization, measurement, and relations with positive and negative developmental outcomes. Appl Dev Sci. 2006;10(2):61–74. doi: 10.1207/s1532480xads1002_2. [DOI] [Google Scholar]
- 37.Youngblade LM, Theokas C, Schulenberg J, Curry L, Huang IC, Novak M. Risk and promotive factors in families, schools, and communities: a contextual model of positive youth development in adolescence. Pediatrics. 2007;119(Suppl 1):S47–S53. doi: 10.1542/peds.2006-2089H. [DOI] [PubMed] [Google Scholar]
- 38.Lerner RM, Lerner JV, Benson JB. Positive youth development: research and applications for promoting thriving in adolescence. Adv Child Dev Behav. 2011;41:1–17. doi: 10.1016/B978-0-12-386492-5.00001-4. [DOI] [PubMed] [Google Scholar]
- 39.Proctor LJ. Children growing up in a violent community: the role of the family. Aggress Violent Beh. 2006;11(6):558–576. doi: 10.1016/j.avb.2005.12.004. [DOI] [Google Scholar]
- 40.Li ST, Nussbaum KM, Richards MH. Risk and protective factors for urban African-American youth. Am J Community Psychol. 2007;39(1–2):21–35. doi: 10.1007/s10464-007-9088-1. [DOI] [PubMed] [Google Scholar]
- 41.Culyba AJ, Ginsburg KR, Fein JA, Branas CC, Richmond TS, Wiebe DJ. Protective effects of adolescent-adult connection on male youth in urban environments. J Adolesc Health. 2016;58(2):237–240. doi: 10.1016/j.jadohealth.2015.10.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Culyba AJ, Jacoby SF, Richmond TS, Fein JA, Hohl BC, Branas CC. Modifiable neighborhood features associated with adolescent homicide. JAMA Pediatr. 2016;170(5):473–480. doi: 10.1001/jamapediatrics.2015.4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gorman-Smith D FL, Cosey-Gay F, Coeling M. Strengthening families and communities to prevent youth violence: a public health approach. Children's Legal Rights J. 2013–2014;34(265).
- 44.Branas CC, Cheney RA, MacDonald JM, Tam VW, Jackson TD, Ten Have TR. A difference-in-differences analysis of health, safety, and greening vacant urban space. Am J Epidemiol. 2011;174(11):1296–1306. doi: 10.1093/aje/kwr273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.MacDonald J, Golinelli D, Stokes RJ, Bluthenthal R. The effect of business improvement districts on the incidence of violent crimes. Inj Prev. 2010;16(5):327–332. doi: 10.1136/ip.2009.024943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garvin EC, Cannuscio CC, Branas CC. Greening vacant lots to reduce violent crime: a randomised controlled trial. Inj Prev. 2013;19(3):198–203. doi: 10.1136/injuryprev-2012-040439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kondo M, Hohl B, Han S, Branas C. Effects of greening and community reuse of vacant lots on crime. Urban Stud. 2015. [DOI] [PMC free article] [PubMed]
- 48.Branas CC, Kondo MC, Murphy SM, South EC, Polsky D, MacDonald JM. Urban blight remediation as a cost-beneficial solution to firearm violence. Am J Public Health. 2016:e1–7. [DOI] [PMC free article] [PubMed]
- 49.DuBois DL, Silverthorn N. Characteristics of natural mentoring relationships and adolescent adjustment: evidence from a national study. J Prim Prev. 2005;26(2):69–92. doi: 10.1007/s10935-005-1832-4. [DOI] [PubMed] [Google Scholar]
- 50.Haddad E, Chen C, Greenberger E. The role of important non-parental adults (VIPs) in the lives of older adolescents: a comparison of three ethnic groups. J Youth Adolescence. 2011;40(3):310–319. doi: 10.1007/s10964-010-9543-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parker EM, Johnson SRL, Jones VC, Haynie DL, Cheng TL. Discrepant perspectives on conflict situations among urban parent–adolescent dyads. J Interpers Violence. 2016;31(6):1007–1025. doi: 10.1177/0886260514564064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beam MR, Gil-Rivas V, Greenberger E, Chen C. Adolescent problem behavior and depressed mood: risk and protection within and across social contexts. J Youth Adolescence. 2002;31(5):343–357. doi: 10.1023/A:1015676524482. [DOI] [Google Scholar]
- 53.Cheng TL, Haynie D, Brenner R, Wright JL, Chung S-E, Simons-Morton B. Effectiveness of a mentor-implemented, violence prevention intervention for assault-injured youths presenting to the emergency department: results of a randomized trial. Pediatrics. 2008;122(5):938–946. doi: 10.1542/peds.2007-2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zun LS, Downey L, Rosen J. The effectiveness of an ED-based violence prevention program. Am J Emerg Med. 2006;24(1):8–13. doi: 10.1016/j.ajem.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 55.Aboutanos MB, Jordan A, Cohen R, Foster RL, Goodman K, Halfond RW, Poindexter R, Charles RS, Smith SC, Wolfe LG, Hogue B, Ivatury RR. Brief violence interventions with community case management services are effective for high-risk trauma patients. J Trauma Acute Care Surg. 2011;71(1):228–237. doi: 10.1097/TA.0b013e31821e0c86. [DOI] [PubMed] [Google Scholar]
- 56.Shibru D, Zahnd E, Becker M, Bekaert N, Calhoun D, Victorino GP. Benefits of a hospital-based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–689. doi: 10.1016/j.jamcollsurg.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 57.Becker MG, Hall JS, Ursic CM, Jain S, Calhoun D. Caught in the crossfire: the effects of a peer-based intervention program for violently injured youth. J Adolescent Health. 2004;34(3):177–183. doi: 10.1016/S1054-139X(03)00278-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 18 kb)