Summary
Background
Intensive community treatment to reduce dependency on adolescent psychiatric inpatient care is recommended in guidelines but has not been assessed in a randomised controlled trial in the UK. We designed a supported discharge service (SDS) provided by an intensive community treatment team and compared outcomes with usual care.
Methods
Eligible patients for this randomised controlled trial were younger than 18 years and had been admitted for psychiatric inpatient care in the South London and Maudsley NHS Foundation Trust. Patients were assigned 1:1 to either the SDS or to usual care by use of a computer-generated pseudorandom code with random permuted blocks of varying sizes. The primary outcome was number of inpatient bed-days, change in Strengths and Difficulties Questionnaire (SDQ) scores, and change in Children's Global Assessment Scale (CGAS) scores at 6 months, assessed by intention to treat. Cost-effectiveness was explored with acceptability curves based on CGAS scores and quality-adjusted life-years (QALYs) calculated from the three-level EuroQol measure of health-related quality of life (EQ-5D-3L), taking a health and social care perspective. This study is registered with the ISRCTN Registry, number ISRCTN82129964.
Findings
Hospital use at 6 months was significantly lower in the SDS group than in the usual care group (unadjusted median 34 IQR 17–63 vs 50 days, 19–125, p=0·04). The ratio of mean total inpatient days for usual care to SDS was 1·67 (95% CI 1·02–2·81, p=0·04), which decreased to 1·65 (0·99–2·77, p=0·057) when adjusted for differences in hospital use before randomisation. Scores for SDQ and CGAS did not differ between groups. The cost-effectiveness acceptability curve based on QALYs showed that the probability of SDS being cost-effective compared with usual care was around 60% with a willingness-to-pay threshold of £20 000–30 000 per QALY, and that based on CGAS showed at least 58% probability of SDS being cost-effective compared with usual care irrespective of willingness to pay. We recorded no adverse events attributable to SDS or usual care.
Interpretation
SDS provided by an intensive community treatment team reduced bed usage at 6 months' follow-up but had no effect on functional status and symptoms of mental health disorders compared with usual care. The possibility of preventing admissions, particularly through features such as reduced self-harm and improved reintegration into school, with intensive community treatment should be investigated in future studies.
Funding
South London and Maudsley NHS Trust.
Introduction
Approximately 4420 adolescents were admitted to specialist child and adolescent mental health units in England and Wales in 2014.1 This number is double that 10 years earlier.2 The number of children and young people who have presented to accident and emergency departments with a psychiatric disorder has also more than doubled from 8358 in 2010–11 to 17 278 in 2013–14.3 Although the proportion of young people being admitted is small, the associated disruption can be substantial and long term, and the accompanying demand on health service resources is very high. Most young people admitted to hospital are likely to have a history of self-harm.4
Urgent psychiatric admissions for adolescents can lead to serious distress, and the highest risks of suicide and self-harm are encountered in the period soon after discharge.5, 6 Despite these concerns, little is known about the optimum models of care.
Clinical guidelines, such as those of the National Institute for Health and Care Excellence (NICE),7 recommend intensive community treatment for several disorders, but only a small number of RCTs, mainly from the USA, have investigated the effects of this approach for adolescent patients requiring psychiatric admission to hospital.8 The results have been mixed, but have shown some beneficial effects on hospital use and patients' satisfaction. Similar research in adults, however, has suggested that initial positive results with intensive community treatment might not be replicable in further RCTs.9, 10 We designed the Supported Discharge Service Versus Inpatient Care Evaluation (SITE) RCT to assess the benefits of an intensive community treatment, termed supported discharge service (SDS), compared with usual care, assessed in terms of hospital inpatient care and changes in symptoms and social functioning, and explored cost-effectiveness.
Research in context.
Evidence before the study
Clinical guidelines recommend intensive community services as a way to reduce dependence on adolescent psychiatric services, but there has been little systematic assessment of their efficacy in the UK. We searched MEDLINE, PsychINFO, and Embase for randomised controlled trials (RCTs) reporting efficacy of intensive community services versus inpatient care in young people, published in English up to Dec 31, 2014, with the search terms “early intervention” and “crisis care”, and common psychiatric diagnostic categories (appendix). We selected RCTs that compared the efficacy of intensive community services with inpatient care in children and adolescents up to age 18 years. Six unique RCTs including 569 young people were identified, which assessed specialist outpatient treatment, multisystemic therapy, day patient treatment, intensive home treatment, and supported discharge services. Intensive community services were associated with similar clinical improvements to inpatient care in most studies but shorter hospital stays, lower costs, and greater patient satisfaction. None of the results, however, had been replicated independently because further studies using these models had not been done. Few studies investigated the use of intensive community treatment as an alternative to inpatient care in high-risk children and adolescents and none had been done in the UK. Independent replication of results achieved by specific intensive community treatment models is a research priority.
Added value of this study
In this multicentre outpatient RCT involving adolescent patients with psychiatric emergencies, we found improved school reintegration with our supported discharge service compared with usual care, and similar clinical and patient satisfaction outcomes, as have been shown in previous studies. Additionally, we found that the proportion of patients with self-harm episodes was reduced.
Implications of all the available evidence
Our findings suggest that intensive community treatment models might be used with and as an alternative to usual inpatient care. Supported discharge services could be cautiously considered for implementation by other treatment centres.
Methods
Study design and patients
This was a single-blind, patient-level, parallel-group, RCT of tertiary inpatient care among adolescents in rural and urban services of one of the largest mental health National Health Service (NHS) Trusts in the UK, the South London and Maudsley NHS Foundation Trust, (SLaM). Patients were admitted for inpatient treatment from the London boroughs of Southwark, Lambeth, Croydon, and Lewisham, and from Kent. The protocol is available online.
Inclusion criteria were hospital admission for inpatient care; age 12 years 0 months to 17 years 11 months; ability and willingness to give oral and written informed consent by children older than 16 years together with assent by parents or guardians or consent by parents or guardians with the assent of children younger than 16 years to participate in the study. Patients were excluded if at the first assessment by clinicians in the inpatient teams they were judged not to have a psychiatric illness warranting inpatient care and were discharged immediately, were discharged within 72 h of admission, were admitted from National and Specialist services with assertive outreach capability, or were admitted when the SDS teams were at full capacity. We did not exclude patients on the basis of risk alone. Ethics approval was obtained from the National Health Service National Research Ethics Service (NHS RES London REC 12/LO/0875).
Randomisation and masking
Randomisation was done after eligibility was confirmed and consent and assent were obtained, via a registered centralised clinical trials unit (King's College London, London, UK). Once baseline assessments of eligible patients were completed by the research staff, patients' details were sent to the clinical trials unit by the trial administrator. Patients were assigned to either SDS treatment or usual care by use of a computer-generated pseudorandom code with random permuted blocks of varying sizes that was created by the clinical trials unit in accordance with their standard operating procedure and stored on a secure server. Patients were allocated 1:1 to each treatment group. Allocations were conveyed to the trial administrator, who relayed this information to the SDS teams and inpatient services.
Patients and treating clinicians were aware of treatment allocation. Researchers were masked to treatment allocation until after the last participant's final 6-month follow-up appointment. Outcome assessors and data managers were masked to study allocation throughout the study and had no access to patients' health service records.
Procedures
The SDS intervention was delivered by two teams, one based in London and one in a rural area in Kent. Each SDS team included one consultant child and adolescent psychiatrist, one administrator, two to four whole-time equivalents of Child and Adolescent Mental Health Services (CAMHS) practitioners with nursing backgrounds, and two to four whole-time equivalents of clinical support workers. The nature of the work included intensive case management, community (including home) treatment, day care in hospital, or any combination of these approaches according to need. The intensity of care was flexible, up to a maximum of daily contacts. Staff tasks included assisting young people with creating customised care plans, psychiatric care, psychological interventions, helping with school reintegration, and optimising physical health care and social support. Further details of care are available online.
The duration of treatment varied by individual need, and the aim was to achieve transfer back to the usual community mental health service, with use of the Care Programme Approach11 as required. The SDS teams operated from 0800 h to 2000 h with out-of-hours cover available at all other times. We used various elements of assertive community treatment: small caseloads (four or five families per whole-time equivalent team member), a team approach, a practising team leader, weekly formal and daily informal team meetings, continuity of staffing, full responsibility for treatment services, responsibility for hospital discharge planning, no dropout policy, assertive engagement mechanisms, and work with informal support systems.12 The teams worked closely with inpatient services, mainly to minimise the potential bias associated with staff enthusiasm in new services. SDS teams aimed to establish contact with each young person assigned to that group within 72 h of admission. As soon as the patient's clinical profile was deemed to be consistent with intensive community treatment (acceptable risk to self and others), he or she and the family were offered SDS, in consultation with inpatient professionals, SDS staff, and the relevant community services.
Usual care was delivered by inpatient services and followed by a return to standard outpatient care, delivered primarily by CAMHS, with or without an interim period of hospital day care. Hospital inpatient care and day care were provided according to the model developed by Corrigall and Mitchell,13 unless all SLaM inpatient beds were full, in which case patients were admitted to private inpatient services. Criteria for inpatient admission included mental illness or suspected mental illness that could not be safely managed by outpatient services due to risk to self or others. Hospital care was delivered by multidisciplinary teams, including psychiatrists, nurses, psychologists, occupational therapists, art psycho-therapists, family therapists, and social workers, and led by a consultant psychiatrist. Each inpatient service had access to a hospital school. Patients in the SDS and usual care groups had access to the full range of local NHS support services open to patients in tertiary care.
Treatment outcomes
The primary outcome, assessed at 6 months after randomisation, was time in psychiatric inpatient treatment (measured as occupied bed-days), change in Strengths and Difficulties Questionnaire (SDQ) score as a broad measure of psychopathology,14 and change in Children's Global Assessment Scale (CGAS) score as a measure of general functioning.15 The SDQ was included to ensure that a self-reported measure was used. We collected SDQ scores from patients and their parents, but because of poor completion by parents, we include only self-reported scores from patients in this analysis. Data on occupied bed-days were collected from the SLaM electronic Patient Journey System (version 5.6.5) repository for patients' records.
Secondary outcomes were also measured at 6 months, and were change from baseline in self-harm measured with the Self-Harm Questionnaire,16 service satisfaction assessed with the Child and Adolescent Service Experience, the proportion of the patients who were attending a community school, and the number of days not in education, employment, or training. The Self-Harm Questionnaire was added as a secondary outcome to provide a formal measure of self-harm rather than an informal measure from medical records. We defined multiple episodes of self-harm as five or more, in line with the DSM-5 definition of non-suicidal self-injury. Further data on secondary outcomes will be reported elsewhere.
Economic outcomes
We did two cost-effectiveness analyses, one based on CGAS scores and one based on quality-adjusted life-years (QALYs), which were calculated from the three-level EuroQol measure of health-related quality of life (EQ-5D-3L).17 We recorded costs and outcomes for the economic assessment at baseline and at 6 months of follow-up. The perspective of the economic evaluation was the NHS and personal social services perspective preferred by NICE.18
Data on resource use were collected with an adapted version of the Child and Adolescent Service Use Schedule (appendix), which was developed in previous research with young people.19, 20, 21 Our version included all-cause uses of the following hospital and community-based health and social care services: staffed accommodation (health care and social services), inpatient stays, outpatient appointments, day patient contacts, accident and emergency contacts, community contacts, and mental-health-related medication. The Child and Adolescent Service Use Schedule was administered at 6 months and covered the period from baseline.
Data on day care contacts with the SDS, which took place in day hospital units, were collected directly from SDS records. Day care appointments were booked per week. To ensure that bookings were costed in full, we assumed that each appointment was allocated and could not be reallocated to another patient, and, therefore, used the number of booked appointments irrespective of attendance. All other contacts with the SDS were provided ad hoc and were recorded in the Child and Adolescent Service Use Schedule. All treatments used as part of usual care were recorded in the Child and Adolescent Service Use Schedule.
Total costs were calculated by applying unit costs to resource use at the individual level. Nationally applicable unit costs were applied to all services (appendix). All costs are reported in pounds sterling at 2014–15 prices. Discounting was not relevant as the follow-up did not exceed 12 months.
Statistical analysis
We calculated the sample size with nQuery Advisor (version 6.01). Results from a Cochrane review12 showed a difference in overall duration of admissions of around 34% in favour of assertive community treatment in seven of 14 RCTs that assessed this outcome. Given the uncertainty of this finding, we allowed for only a 22% reduction in the mean duration of admissions. To achieve 80% power to detect 22% difference between study groups (from a mean of 45 days to a mean of 35 days, range 1–90, SD 18·4) with the two-tailed α set at 0·05, we calculated that we needed to include 54 patients in each treatment group.
All data were analysed with STATA version 14.0. As per our statistical analysis plan, we compared outcomes between groups at 6 months after randomisation with an independent Student's t test without adjustment. In a second step, we controlled for possible imbalances before randomisation by including prerandomisation outcome as a covariate (adjusted ANCOVA approach). The ratio of the geometric means was used for hospital use data because they had to be log-transformed to fulfil assumptions of normality and equal variances. As a sensitivity analysis, we also present the adjusted treatment effect of untransformed hospital use data. Cohen's d (mean difference divided by pooled SD at baseline) values are presented as standardised effect sizes.
We analysed categorical outcomes with logistic regression adjusted for prerandomisation outcome when available. SEs and 95% CIs for all parametric analyses were obtained through non-parametric bootstrap methods to account for possible violations of normality assumptions.22 Differences in the numbers of multiple self-harm episodes were analysed by comparing the proportions of the young people in each group by logistic regression. For inpatient occupied bed-days we used numbers recorded on the electronic records system.
To assess whether missing data altered treatment effect estimates in secondary outcome variables, we did a sensitivity analysis with multiple imputations. We used demographic and clinical baseline and follow-up variables to calculate missing data distributions separately in each treatment group.23 50 imputed datasets were created and were analysed and combined according to Rubin's rules, as implemented in the ice command in STATA.24
The economic analyses focused on the probability of one intervention being cost-effective compared with another given the data available, which is the recommended decision-making approach for funding of treatments, and is preferred over traditional reliance on arbitrary decision rules based on significance.25 Differences in mean costs and outcomes were analysed by ordinary least squares regressions combined with bootstrapping (repeat resampling, 5000 replications, and regression models for costs and outcomes based on the same sample) to account for non-normality.26 The advantage of this approach, as opposed to logarithmic transformation or non-parametric tests, is the ability to make inferences about the mean to determine the total cost for a group of patients.26 To provide more relevant treatment-effect estimates,27 regressions to calculate mean differences in costs and outcomes included baseline covariates that might affect costs and outcomes: number of days as an inpatient before randomisation, baseline CGAS score, baseline EQ-5D-3L, age, sex, ethnicity, social class (based on the main earner of the family), and diagnosis (psychotic vs not psychotic). The primary economic analysis excluded patients with missing cost or outcome data. We tested the effects of missing data in sensitivity analyses (appendix).
Cost-effectiveness was explored with the net benefit approach. We calculated area under the curve values for QALYs with linear interpolation between assessments.28 We used cost-effectiveness acceptability curves to explore uncertainty around costs and cost-effectiveness due to sampling variation and the maximum cost-effectiveness ratio that a decision maker would deem acceptable.29 The curves were created from bootstrapped costs and effects to calculate the probability of each treatment being the optimum choice, subject to a range of possible maximum values that a decision maker might be willing to pay for an increase in either QALYs or CGAS scores. This study is registered with the ISRCTN Registry, number ISRCTN82129964.
Role of the funding source
The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
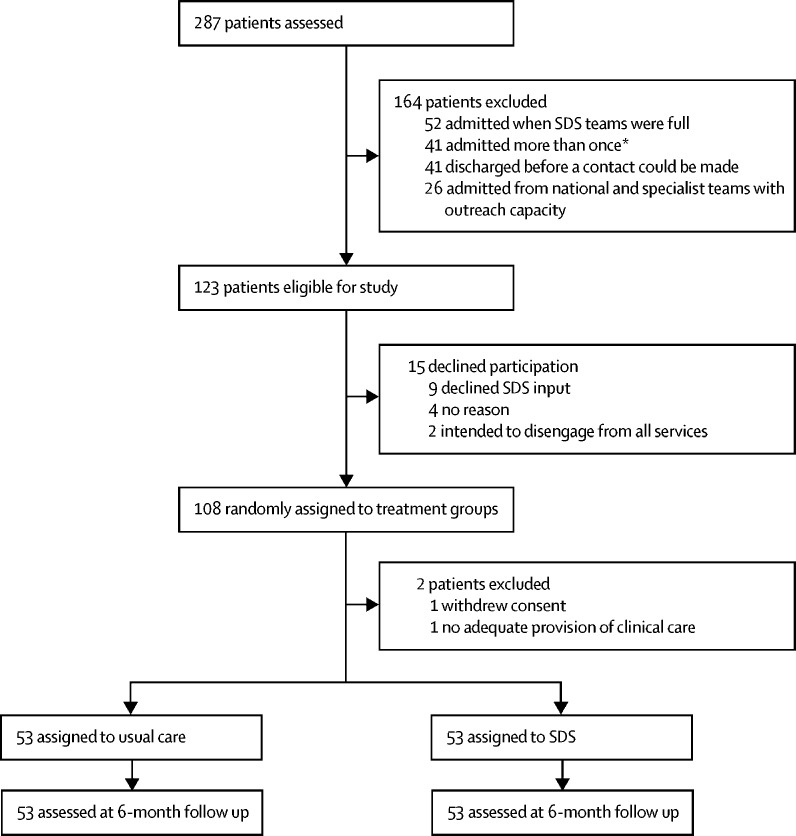
287 patients were referred for inpatient admission during the study recruitment period, of whom 123 were eligible for the study (figure 1). 15 (12%) refused to participate. 108 patients were randomly assigned to a treatment group. 23 patients (21%) were from the Southwark site, 18 (17%) from the Lambeth site, 42 (39%) from the Croydon site, 16 (15%) from the Lewisham site, and nine (8%) from the Kent site. Two patients, one in each treatment group, were withdrawn from the study. One patient, in the SDS group, withdrew consent, and one in the usual care group was withdrawn because of inadequate provision of community clinical care and was cared for by the SDS team. The final study sample, therefore, was 106 patients (53 patients in each group; figure 1), although hospital use data were available for all 108 patients. Sociodemographic and clinical data did not differ between groups at baseline, although self-rated SDQ scores were slightly higher in the SDS group than in the usual care group (table 1, appendix). The mean duration of SDS care was 116·3 days (SD 70·1, 95% CI 90·6–142·0; median 107 days, range 1–274). We recorded no adverse events attributable to SDS or usual care.
Figure 1.
Trial profile
SDS=supported discharge service. *45 exclusions because 37 admitted twice and four admitted three times.
Table 1.
Demographic and clinical characteristics
| Supported discharge service (n=53) | Usual care (n=53) | ||
|---|---|---|---|
| Age (years) | 16·23 (1·54) | 16·3 (1·7) | |
| CGAS score | 44·62 (8·42) | 46·8 (11·3) | |
| Self-reported SDQ score | 20·57 (6·58) | 16·84 (7·00) | |
| Sex | |||
| Boys | 17 (32%) | 20 (38%) | |
| Girls | 36 (68%) | 33 (62%) | |
| Ethnicity | |||
| White British | 28 (53%) | 24 (45%) | |
| Other | 25 (47%) | 29 (55%) | |
| Social class* | |||
| Highly paid professionals | 6 (11%) | 1 (2%) | |
| Low-paid professionals | 7 (13%) | 8 (15%) | |
| Skilled non-manual workers | 8 (15%) | 9 (17%) | |
| Skilled manual workers | 11 (21%) | 10 (19%) | |
| Non-skilled workers | 5 (9%) | 9 (17%) | |
| Unemployed, students | 16 (30%) | 16 (30%) | |
| Psychosis | 15 (31%) | 16 (30%) | |
| Multiple episodes of self-harm (≥5) | 32 (62%)† | 22 (45%)‡ | |
Data are mean (SD) or number (%). CGAS=Clinical Global Assessment Scale. SDQ=Strengths and Difficulties Questionnaire.
Based on main earner in the family.
Data available in 52 patients.
Data available in 49 patients.
In the unadjusted analysis of hospital use (n=108), the overall number of occupied bed-days differed significantly between the SDS and usual care groups (median 34 days, IQR 17–63 vs 50, 19–125, p=0·04). The ratio of the geometric mean total of inpatient hospital-days was 1·67 (95% CI 1·02–2·81) in favour of the SDS group (p=0·04). However, this treatment effect did not remain significant after adjustment for prerandomisation differences in hospital use (ratio 1·65, 95% CI 0·99–2·77, p=0·057). An analysis of untransformed hospital use revealed an adjusted treatment effect of −34·1 days (95% CI −67·5 to −9·4, p=0·01).
6-month CGAS data were available for 102 patients, 52 (98%) of 53 in the SDS group and 50 (94%) of 53 in the usual care group. In the unadjusted analysis we saw no difference in treatment effect difference of 3·4 CGAS points (95% CI −3·3 to 10·1, effect size d=0·10, p=0·32). In adjusted analyses, there was a 6% difference in CGAS scores (SDS mean 63·2 [SD 16·7] vs usual care 59·7 [17·8]). ANCOVA and controlling for baseline CGAS scores revealed a non-significant treatment difference of 4·88 CGAS points (95% CI −1·27 to 11·02, effect size d=0·15, p=0·12).
Self-rated SDQ scores at 6 months were available for 89 patients, 41 (77%) of 53 in the usual care group and 48 (91%) of 53 in the SDS group. Mean scores were 16·2 (SD 7·3) and 17·6 (7·1), respectively. The unadjusted treatment difference was 1·48 points (95% CI −1·45 to 4·54, effect size d=0·10, p=0·33), and the adjusted difference was −0·26 (−2·55 to −2·12, d<0·001, p=0·90). There was insufficient evidence to suggest a difference in clinical symptoms at 6 months with control for prerandomisation SDQ scores.
Patient satisfaction data were available for 81 patients, 45 (85%) of 53 in the SDS group and 36 (68%) of 53 in the usual care group. Mean Child and Adolescent Service Experience scores were similar in the two groups (55·4 [SD 14·0] and 51·1 [15·5], respectively). ANCOVA revealed a treatment difference of 4·2 points (95% CI −2·13 to 10·81, effect size d=0·14, p=0·20).
11 (24%) of 45 patients in the SDS group and 16 (42%) of 38 in the usual care group reported multiple episodes of self-harm at 6 months of follow-up. Binomial logistic regression controlling for baseline scores revealed significantly reduced likelihood that patients assigned to SDS would report multiple episodes of self-harm (odds ratio [OR] 0·18, 95% CI 0·05–0·64, p=0·008).
43 (81%) of 53 patients in the SDS group reintegrated to community schools, as did 27 (51%) of 53 in the usual care group. Binary logistic regression revealed that adolescents assigned to SDS were significantly more likely to be attending a community school at 6 months of follow-up (OR 4·14, 95% CI 1·73–9·92, p=0·001). Data on the total number of days spent not in employment, education, or training were available for 36 (68%) of 53 patients in the usual care group and 46 (87%) of 53 in the SDS group, and the median significantly favoured the SDS group (SDS 49, 23–87 vs usual care 96, 47–102, p=0·04). We found no evidence of differential effects on any of the above variables in adolescents with psychosis or low global functioning or in adolescents from minority ethnic groups (appendix).
Multiple imputation analyses for missing data showed negligible changes of treatment effects and inference and did not alter the conclusions.
Full economic cost and outome data were available for 42 (79%) of 53 patients in the SDS group and 36 (68%) of 53 in the usual care group for the cost-effectiveness analysis based on QALYs, and for 37 (70%) in the SDS group and 45 (85%) in the usual care group for that based on CGAS scores. The mean duration of follow-up was 199 days (SD 31) in the SDS group and 231 days (71) in the usual care group.
EQ-5D-3L-based QALYs and CGAS scores were similar in the two groups at baseline and 6 months of follow-up (table 2). Results based on imputation for missing data did not alter the significance of these results. SDS day patient service costs were substantial at around £24 000 compared with nothing for usual care, whereas health and social care costs excluding SDS day patient services were significantly lower in the SDS group than in the usual care group, by around £29 000 (table 3). Combining all costs, the difference between groups was no longer significant (table 3).
Table 2.
Economic outcomes* at baseline and 6 months
|
Supported discharge service |
Usual care |
Unadjusted mean difference (95% CI) | p value | Adjusted mean difference (95% CI)† | p value | |||
|---|---|---|---|---|---|---|---|---|
| Number of patients | Mean (SD) | Number of patients | Mean (SD) | |||||
| Baseline | ||||||||
| EQ-5D-3L score | 51 | 0·5 (0·3) | 50 | 0·6 (0·4) | −0·1 (−0·2 to 0·1) | 0·21 | −0·1 (−0·2 to 0·1) | 0·39 |
| CGAS | 53 | 44·6 (8·4) | 53 | 46·8 (11·3) | −2·2 (−5·9 to 1·6) | 0·25 | −0·7 (−4·2 to 2·8) | 0·70 |
| 6 months | ||||||||
| EQ-5D-3L score | 44 | 0·6 (0·3) | 38 | 0·73 (0·3) | −0·1 (−0·2 to 0) | 0·09 | −0·1 (−0·2 to 0·1) | 0·44 |
| EQ-5D-3L-based QALYs | 42 | 0·3 (0·1) | 36 | 0·34 (0·1) | 0 (−0·1 to 0) | 0·21 | −0 (−0·1 to 0) | 0·39 |
| CGAS | 52 | 63·2 (16·7) | 50 | 59·7 (17·8) | 3·4 (−3·4 to 10·2) | 0·32 | 3·7 (−2·7 to 10·2) | 0·27 |
| Imputed QALYs | 53 | 0·3 (0·1) | 53 | 0·35 (0·2) | −0·1 (−0·1 to 0) | 0·057 | −0 (0 to 0) | 0·17 |
| Imputed CGAS | 53 | 63·3 (16·3) | 53 | 59·9 (17·4) | 3·4 (−3·0 to 9·9) | 0·29 | 4·5 (−1·6 to 10·5) | 0·14 |
EQ-5D-3L=three-level EuroQol score. CGAS=Clinical Global Assessment Scale. QALYs=quality-adjusted life-years.
Higher EQ-5D-based utility and CGAS scores indicate better outcomes.
Adjusted for baseline Clinical Global Assessment Scale score, baseline 3L-EQ-5D score, inpatient bed-days before randomisation, sex, age, ethnicity, diagnosis, and social class.
Table 3.
Costs for the 6-month treatment period (2014–15 prices)
|
Supported discharge service |
Usual care |
Unadjusted mean difference (95% CI) | p value | Adjusted mean difference (95% CI)* | p value | |||
|---|---|---|---|---|---|---|---|---|
| Number of patients | Mean (SD) cost (£) | Number of patients | Mean (SD) cost (£) | |||||
| SDS day patient services | 53 | 24 150 (20 102) | 53 | 0 | 24 150 (18 819 to 29 481) | <0·001 | 24 052 (18 411 to 29 693) | <0·001 |
| Other health and social care costs | 45 | 37 601 (38 870) | 37 | 64 767 (65 122) | −27 166 (−50 905 to −3 427) | 0·026 | −29 022 (−53 647 to −4 396) | 0·023 |
| Total costs for patients with complete data | 45 | 63 621 (39 604) | 37 | 64 767 (65 122) | −1 146 (−24 949 to 22 657) | 0·93 | −3 675 (−28 487 to 21 138) | 0·773 |
| Total costs with imputed missing data | 53 | 64 355 (36 692) | 53 | 63 463 (55 254) | −892 (−16 926 to 18 710) | 0·92 | −612 (−16 775 to 15 551) | 0·940 |
Adjusted for baseline Clinical Global Assessment Scale score, baseline three-level EuroQol score, inpatient bed-days before randomisation, sex, age, ethnicity, diagnosis, and social class.
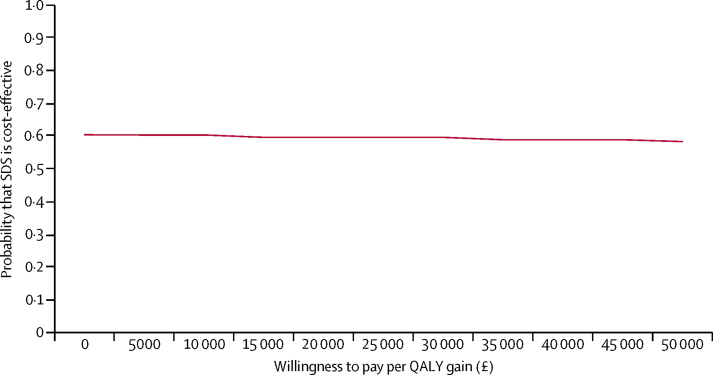
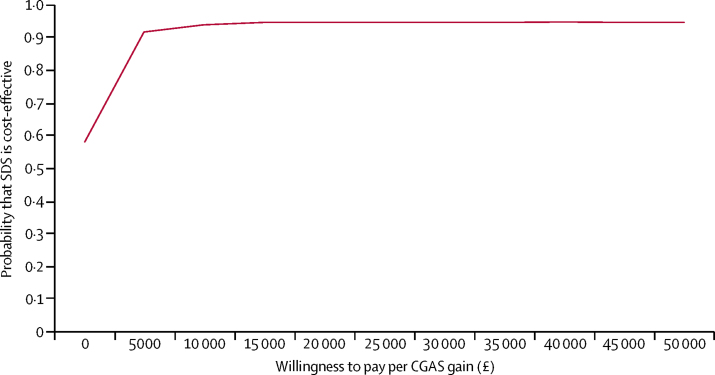
The incremental cost-effectiveness ratio based on QALYs was £183 750, but as usual care was more effective and more expensive than SDS (the reverse of the more common finding that the experimental intervention is more effective and more expensive), this ratio indicates the incremental cost-effectiveness of usual care compared with SDS. The ratio is far above the NICE threshold of £20 000–30 000 per QALY, which suggests that usual care is not cost-effective compared with SDS (appendix). The cost-effectiveness acceptability curve based on QALYs shows that the probability of SDS being cost-effective compared with usual care is around 60% at the NICE preferred willingness-to-pay threshold of £20 000–30 000 per QALY (figure 2). When based on complete data for CGAS, the incremental cost-effectiveness ratio was −£991, indicating that SDS was cheaper and more effective on average than usual care (appendix). The cost-effectiveness acceptability curve based on CGAS scores suggests that SDS has at least 58% probability of being cost-effective compared with usual care, irrespective of the level of willingness to pay, which rises to more than 90% probability at and beyond a willingness-to-pay threshold of £5000 (figure 3). Cost-effectiveness acceptability curves for QALYs and the CGAS did not differ when generated with missing data imputed (appendix), suggesting that the probability of SDS being cost-effective compared with usual care is 50% or greater irrespective of willingness to pay.
Figure 2.
Cost-effectiveness acceptability curve from a health and social care perspective for supported discharge service versus treatment as usual at 6 months based on adjusted analyses of QALYs
QALY=quality-adjusted life-years.
Figure 3.
Cost-effectiveness acceptability curve from a health and social care perspective for supported discharge service versus treatment as usual at 6 months based on adjusted analyses of CGAS scores
CGAS=Clinical Global Assessment Scale.
Discussion
In this RCT of an intensive community treatment approach versus usual care for adolescents with severe psychiatric disorders, we found a significant difference in hospital bed use in favour of SDS in the 6 months after randomisation, but it did not remain significant after controlling for prerandomisation differences in hospital use. Symptom and functioning outcomes that favoured the SDS group were not significantly different from those with usual care. These treatment effects are in line with those noted in an RCT undertaken by an independent research group30 who used the UK SDS model.31, 32
In terms of secondary outcomes, patients in the SDS group were less likely to report multiple episodes of self-harm, more likely to achieve school reintegration, and spent fewer days out of mainstream school than those in the usual care group. Satisfaction with the services did not differ. Additionally, economic analyses suggest that SDS has at least 50% probability of being cost-effective compared with usual care, irrespective of the measure used (QALYs or CGAS) and of willingness to pay for outcome improvements.
So far, five other trials have investigated the use of intensive community care versus inpatient treatment in children and adolescents with severe psychiatric disorders.8 The use of intensive community services in our study was associated with clinical improvements similar to those achieved with inpatient care in most studies. The trials of the SDS intensive community treatment model, however, were unique because they crossed two different mental health systems in the UK and Germany. Additionally, unlike previous studies, the SDS model was tested in pragmatic mental health care settings.
The use of intensive case management, day care in the hospital setting, and community (including home) treatment with small caseloads might account for the effects of SDS. In several studies of intensive community treatment in adults, initial positive results did not seem to be sustained when the model was implemented more widely.9, 10 We have maximised the generalisability of the findings by establishing real-world SDS teams, maximising work crossover between the inpatient and the SDS staff, and by having very broad inclusion criteria. An important finding of the SITE RCT is the significant reduction in the proportion of the young people in the SDS group who repeatedly self-harmed compared with those in the usual care group.
The strengths of the SITE trial include broad inclusion criteria and few exclusion criteria to reflect how services operate in usual NHS care, good follow-up participation rates and the inclusion of school reintegration as an outcome measure. The SDS model has now been shown effective in the largest number of adolescent patients (n=206) of any intensive community care model, across two different countries.31, 32 Our trial provides much-needed empirical evidence of the effectiveness of an intensive community treatment model of care by showing that SDS can lead to reduced hospital use and improve school reintegration and reduce self-harm. No routinely available data exist to show whether the care pathways investigated in this RCT are similar to those for other sites in the UK, but adolescents with psychiatric emergencies might not always receive care in adolescent psychiatric units or have access to intensive community mental health teams.
Limitations of this study include substantial heterogeneity in the quality of the inpatient care received by the adolescents in the usual care group, ranging from multi-award-winning NHS inpatient services in the largest provider of mental health services in the UK to private providers. Nevertheless, we see this limitation as increasing the generalisability of our findings. We will report the data for private inpatient services and reasons for admissions elsewhere. A reported difference at baseline between groups for SDQ scores is probably a chance finding. As this indicated a greater severity of psychopathology in the SDS group, if anything it has led to underestimation of the SDS effects. Our study might have been marginally underpowered to detect differences in inpatient bed use, symptoms, patients' satisfaction, and function at 6 months of follow-up. The finding for patients' satisfaction is surprising in the context of previous research and the results of previous qualitative analyses from this RCT.33 In some patients, illness was more severe and of longer duration than we had expected and needed SDS-associated treatment that extended beyond the 6-month primary outcome endpoint with graduated transfer to aftercare with clear recommendations for ongoing care. We lost some patients during follow-up in this study, but the proportion was lower than in many other service assessments.34 Other important limitations of our study were that full masking was impossible and no detailed procedure of enquiring about unblinding events was in place. However, interview and self-reported outcomes showed similar patterns, suggesting no effect on results.
Our economic analyses also had some limitations. First, length of follow-up varied substantially because of the difficult nature of engagement with this population (the follow-up time ranged from 4 to 11 months). Follow-up times in the usual care group were longer than in the SDS group, which could mean that any difference in costs could be due to a shorter follow-up period. Second, the economic assessment was reliant on self-reported resource use, which is subject to recall bias. This approach was necessary, though, because not all data for health and social care are available from one source. Furthermore, self-reported resource use has been reliable even in populations who have cognitive deficits,35, 36 and there is no reason to believe that any biases related to data collection would be imbalanced between the two trial arms. Thirdly, the willingness to pay for a point improvement on the CGAS is unknown, but is unlikely to be as high as £50 000, the maximum willingness to pay presented in the economic analyses. Finally, the economic results were sensitive to adjustment for baseline covariates and imputation and the sample size was small. Thus, our results must be interpreted with caution.
Assessing effectiveness and cost-effectiveness of SDS beyond 6 months will be important. More studies are needed to confirm whether SDS is generalisable to other well resourced service systems in high-income countries.
For more on the study protocol see http://www.isrctn.com/ISRCTN82129964
For more on the details of care see https://www.national.slam.nhs.uk/services/camhs/supported-discharge-service/
For more on CAMHS see http://www.slam.nhs.uk/our-services/service-finder-details
Acknowledgments
Acknowledgments
DS and ZA were supported by the National Institute for Health Research Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London. We thank Jo Fletcher, Bruce Clark, and Emily Simonoff for helping to obtain research funding and facilitating the creation and running of the supported discharge service teams. We thank also all the research assistants and MSc students who contributed to the study. The views expressed are those of the authors and not necessarily those of the UK National Health Service, National Institute for Health Research, or the Department of Health.
Contributors
DO was the chief investigator and DO and RC obtained funding. DO, RC, TZ, MS, VS, DS, PR, JI, MC, ZA, and ET designed the study. JP was the trial manager, supervised the research assessments, and, with DS and ZA, and KM analysed the data. TZ supervised treatment and TZ, MS, and VS delivered treatment. JI, MC, and DH supervised data collection. DO, RC, TZ, MS, VS, DS, PR, ZA, DH, KM, and ET interpreted the data. SB, MH, and BN designed and did all economic analyses and wrote the economic sections of the paper. All authors were involved in writing the rest of the paper.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.CAMHS Tier 4 Report Steering Group Child and adolescent mental health services (CAMHS) tier 4 report. July, 2014. https://www.england.nhs.uk/wp-content/uploads/2014/07/camhs-tier-4-rep.pdf
- 2.Worrall A, O'Herlihy A, Banerjee S. Inappropriate admission of young people with mental disorder to adult psychiatric wards and paediatric wards: cross sectional study of six months' activity. BMJ. 2004;328:867. doi: 10.1136/bmj.38058.605787.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lamb N. Deparment of Health. Future in mind: promoting, protecting and improving our children and young people's mental health and wellbeing. 2015. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/414024/Childrens_Mental_Health.pdf
- 4.Wolff J, Frazier EA, Esposito-Smythers C, Burke T, Sloan E, Spirito A. Cognitive and social factors associated with NSSI and suicide attempts in psychiatrically hospitalized adolescents. J Abnorm Child Psychol. 2013;41:1005–1013. doi: 10.1007/s10802-013-9743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ougrin D, Banarsee R, Dunn-Toroosian V, Majeed A. Suicide survey in a London borough: primary care and public health perspectives. J Public Health. 2011;33:385–391. doi: 10.1093/pubmed/fdq094. [DOI] [PubMed] [Google Scholar]
- 6.Hawton K, Saunders KE, O'Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379:2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- 7.National Collaborating Centre for Mental Health and National Institute for Health and Care Excellence . British Psychological Society and Royal College of Psyciatrists; London: 2013. Psychosis and schizophrenia in children and young people: recognition and management. Clinical guideline 155. [Google Scholar]
- 8.Kwok KHR, Yuan SNV, Ougrin D. Review: alternatives to inpatient care for children and adolescents with mental health disorders. Child Adolesc Ment Health. 2016;21:3–10. doi: 10.1111/camh.12123. [DOI] [PubMed] [Google Scholar]
- 9.Burns T, Creed F, Fahy T, Thompson S, Tyrer P, White I. Intensive versus standard case management for severe psychotic illness: a randomised trial. Lancet. 1999;353:2185–2189. doi: 10.1016/s0140-6736(98)12191-8. [DOI] [PubMed] [Google Scholar]
- 10.Killaspy H, Mas-Exposito L, Marston L, King M. Ten year outcomes of participants in the REACT (Randomised Evaluation of Assertive Community Treatment in North London) study. BMC Psychiatry. 2014;14:296. doi: 10.1186/s12888-014-0296-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodwin N, Lawton-Smith S. Integrating care for people with mental illness: the Care Programme Approach in England and its implications for long-term conditions management. Int J Integr Care. 2010;10:e040. doi: 10.5334/ijic.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marshall M, Lockwood A. Assertive community treatment for people with severe mental disorders. Cochrane Database Syst Rev. 2000;2 doi: 10.1002/14651858.CD001089. CD001089. [DOI] [PubMed] [Google Scholar]
- 13.Corrigall R, Mitchell B. Service innovations: rethinking in-patient provision for adolescents. The Psychiatrist. 2002;26:388–392. [Google Scholar]
- 14.Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry. 1999;40:791–799. [PubMed] [Google Scholar]
- 15.Shaffer D, Gould MS, Brasic J. A children's global assessment scale (CGAS) Arch Gen Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 16.Ougrin D, Boege I. Brief report: the Self Harm Questionnaire: a new tool designed to improve identification of self harm in adolescents. J Adolesc. 2013;36:221–225. doi: 10.1016/j.adolescence.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 17.EuroQol Group EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 18.NICE . National Institute of Health and Care Excellence; London: 2013. Guide to the methods of technology appraisal 2013. [PubMed] [Google Scholar]
- 19.Byford S, Harrington R, Torgerson D. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry. 1999;174:56–62. doi: 10.1192/bjp.174.1.56. [DOI] [PubMed] [Google Scholar]
- 20.Harrington R, Peters S, Green J, Byford S, Woods J, McGowan R. Randomised comparison of the effectiveness and costs of community and hospital based mental health services for children with behavioural disorders. BMJ. 2000;321:1047. doi: 10.1136/bmj.321.7268.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barrett B, Byford S, Chitsabesan P, Kenning C. Mental health provision for young offenders: service use and cost. Br J Psychiatry. 2006;188:541–546. doi: 10.1192/bjp.bp.105.010108. [DOI] [PubMed] [Google Scholar]
- 22.Good PI. Birkhäuser; Boston, MA: 2006. Resampling methods: a practice guide to data analysis. [Google Scholar]
- 23.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 24.Royston P, Carlin JB, White IR. Multiple imputation of missing values: new features for mim. Stata J. 2009;9:252–264. [Google Scholar]
- 25.Claxton K, Sculpher M, Drummond M. A rational framework for decision making by the National Institute For Clinical Excellence (NICE) Lancet. 2002;360:711–715. doi: 10.1016/S0140-6736(02)09832-X. [DOI] [PubMed] [Google Scholar]
- 26.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320:1197–1200. doi: 10.1136/bmj.320.7243.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Assmann SF, Pocock SJ, Enos LE, Kasten LE. Subgroup analysis and other (mis)uses of baseline data in clinical trials. Lancet. 2000;355:1064–1069. doi: 10.1016/S0140-6736(00)02039-0. [DOI] [PubMed] [Google Scholar]
- 28.Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14:487–496. doi: 10.1002/hec.944. [DOI] [PubMed] [Google Scholar]
- 29.Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry. 2005;187:106–108. doi: 10.1192/bjp.187.2.106. [DOI] [PubMed] [Google Scholar]
- 30.Ougrin D, Zundel T, Corrigall R, Padmore J, Loh C. Innovations in practice: pilot evaluation of the supported discharge service (SDS): clinical outcomes and service use. Child Adolesc Ment Health. 2014;19:265–269. doi: 10.1111/camh.12038. [DOI] [PubMed] [Google Scholar]
- 31.Boege I, Copus N, Schepker R. Effectiveness of home treatment in light of clinical elements, chances, and limitations. Z Kinder Jugendpsychiatr Psychother. 2014;42:27–37. doi: 10.1024/1422-4917/a000267. (in German). [DOI] [PubMed] [Google Scholar]
- 32.Boege I, Corpus N, Schepker R, Kilian R, Fegert JM. Cost-effectiveness of intensive home treatment enhanced by inpatient treatment elements in child and adolescent psychiatry in Germany: a randomised trial. Eur Psychiatry. 2015;30:583–589. doi: 10.1016/j.eurpsy.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 33.Reavey P, Poole J, Corrigall R. The ward as emotional ecology: adolescent experiences of managing mental health and distress in psychiatric inpatient settings. Health Place. 2017;46:210–218. doi: 10.1016/j.healthplace.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 34.Morriss R, Garland A, Nixon N. Efficacy and cost-effectiveness of a specialist depression service versus usual specialist mental health care to manage persistent depression: a randomised controlled trial. Lancet Psychiatry. 2016;3:821–831. doi: 10.1016/S2215-0366(16)30143-2. [DOI] [PubMed] [Google Scholar]
- 35.Calsyn RJ, Allen G, Morse GA, Smith R, Tempelhoff B. Can you trust self-report data provided by homeless mentally ill individuals? Eval Rev. 1993;17:353–366. [Google Scholar]
- 36.Goldberg RW, Seybolt DC, Lehman A. Reliable self-report of health service use by individuals with serious mental illness. Psychiatr Serv. 2002;53:879–881. doi: 10.1176/appi.ps.53.7.879. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.