Abstract
Background:
Head and neck cancers constitute about 5%–8% of total body cancers in Europe, America, but in India, this figure is somewhat higher. The aim of this study is to evaluate the current burden of oral cancers in India, particularly North-East India.
Materials and Methods:
A full-length study starting from patient counseling to clinical and histopathological examination and grading was planned. The study was conducted under the guidance of clinician, oral surgeon, oral pathologists, and statistician.
Results:
In the 3 years study, all the patients with oral lesions are examined clinically, out of them suspected oral cancer patients were histopathologically confirmed as oral squamous cell carcinoma patient. The socioeconomic profile of oral cancer patients in relation to all examined patients was summarized, and results are drawn.
Conclusion:
The studied population is heavily indulgent tobacco consumption. Education for cancer prevention, early detection, and treatment is needed.
Keywords: Histopathology, oral cancer, squamous cell carcinoma, tobacco habits
INTRODUCTION
Cancer always being the greatest social fear represented by an irregular, jagged-shaped crab.[1] Cancer is one of the top five causes of death, of which head and neck cancers account 5–8 percent of the total cancer burden in Europe and America.[2,3,4] The published report on cancer's current scenario in 2015 shows that oral cancer tops among all other cancers in India in males, whereas in females, it is the 3rd highest. The age-adjusted rates of oral cancer vary from over 20/100,000 populations in India, to 10/100,000 in the United States, and < 2/100,000 in the Middle East.[5] In India, head and neck cancer constitute about 30% of all cancers.[6] Common forms of head and neck cancer are in the larynx, trachea, and oral cavity.[7,8] Several types of oral cancers are there such as squamous cell carcinomas, basal cell carcinomas, verrucous carcinomas, nasopharyngeal carcinomas, malignant melanoma, ameloblastoma, and mucoepidermoid carcinoma; but 90% burden is only of squamous cell carcinomas, originating in the tissues that line the mouth and lips.[5] In the northeastern part of India where oral cancer is widely distributed, only a few studies have been conducted and also with limited sample size. Some population-based registries available also lacks the histopathological records. Hence, this study was conducted in the institution which is the only tertiary referral center of the region, with an objective to evaluate the prevalence and aggressiveness of the oral cancer and any association with oral deleterious habits and socioeconomic status. The study sample was collected from the patients referred to the out patient department (OPD) Department of Oral and Maxillofacial Pathology 2010–2013. Data were recorded on a questionnaire designed by an expert statistician; this data sheet contains information about patient's educational status, economic status, occupational status, oral habits, and family profile regarding the history of cancer.
MATERIALS AND METHODS
For the purpose of this study, we considered 1252 patients selected on the basis of inclusion and exclusion criteria out of the patients visiting the OPD of Oral and Maxillofacial pathology for their oro-dental problems (oral lesions). All the patients coming to outdoor were included in the study, except those having the previous history of cancer, and those not willing to participate in the study. These patients were interrogated regarding their oral problems, their personal profile, their family profile, and deleterious habits. Any history of systemic diseases, previous medical history and family history related to cancer, etc., were recorded. Then, thorough extra- and intra-oral clinical examination was done and a provisional diagnosis was made on the basis of those findings (history, signs, and symptoms). Patients suspected to be suffering from oral cancer (oral squamous cell carcinoma [OSCC]) were clinically graded on the basis of tumor, node and metastasis (TNM) classification (tumor size, lymph node involvement, and metastasis to distant sites). Before the biopsy procedure, the patients were thoroughly examined for general health status. Routine blood examination was carried out for hemoglobin %, bleeding time, clotting time, total leukocytes count, differential leukocytes count, erythrocytes sedimentation rate, platelet count, blood sugar level for both fasting (F), and postprandial.
The biopsy procedure was carried out after having written consent of the patient and his/her family members. Then, an incisional biopsy was performed from the most representative part of the tumor under local anesthesia (xylocaine 2%).
Histopathological section was stained with hematoxylin (H) and eosin (E). The H and E stained slide was then examined under light microscope for histopathological grading of oral cancer according to Anneroth's grading system. All the six parameters were graded, and a score (1–4) was provided for all the parameters. Grades were provided on the basis of severity of that parameter. Grade 1 indicates the most favorable degree of that parameter for the patients and Grade 4 had the worst degree of that parameter. A lower grade indicates lesser severity, favorable prognosis, and better survival.
Patients having the previous history of head and neck cancer, the previous history of surgery, radiotherapy, or chemotherapy were not included in this study.
RESULTS
Patients were divided into two groups, namely, cancer group and noncancer group depending on histopathological diagnosis. Cancer group have 480 patients, and the noncancer group have 772 persons.
Majority of patients were in their middle age. Patients in the noncancer group were mostly in their 3rd and 4th decades (younger) in comparison to the cancer group patients which were mostly in their 4th, 5th, and 6th decades of life [Graph 1].
Graph 1.
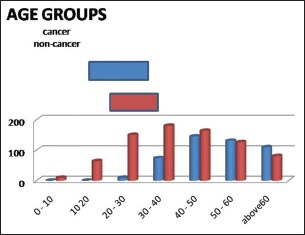
Distribution of cancer and noncancer persons according to age
Males had a higher incidence of cancer, male to female ratio was 1.79:1 in cancer group, but this study as a whole indicate male to female ratio of 1.61:1 [Graph 2].
Graph 2.
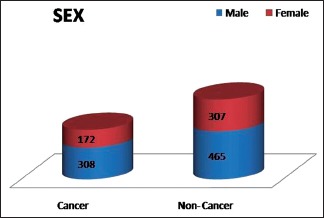
Distribution of cancer and noncancer persons according to sex
Hindu was the main bulk of the study sample. Hence, the Hindu dominates in both categories either in oral cancer or in noncancer patients group. Overall, Hindus had 1.23 times more cancer prevalence than Muslims [Graph 3].
Graph 3.
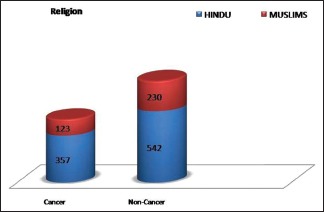
Distribution of cancer and noncancer persons according to religion
Majority of the patients studied in this study were from the general category as 65.62% in cancer group and 54.14% in the noncancer group. The incidence of cancer was higher in general category compared to others [Graph 4].
Graph 4.
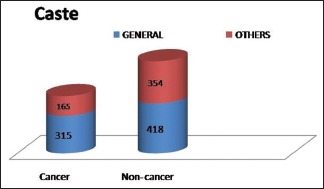
Distribution of cancer and noncancer persons according to casts
Most of the patients in this study as a whole or in cancer group were from higher age groups, and so most of them were married, but only a few cases were either unmarried or widowed or separated [Graph 5].
Graph 5.
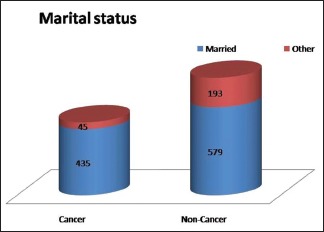
Distribution of cancer and noncancer persons according to marital status
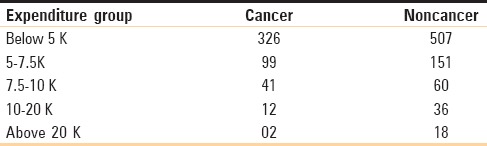
The highest incidence was present in self-employed group [Table 1] as compared to other professions. Oral cancer incidence was inversely proportional to the monthly expenditure for the household of the family [Table 2]. Distribution of the patients included in the study according to the educational status. Around 36.18% of the total study sample was illiterate. In noncancer group, 30.44% of patients were illiterate, and 69.56% are literate. In cancer group, 45.41% of patients are illiterate, and 54.59% are literate, again out of them, most studied up to the 5th standard. Oral cancer incidence is higher in illiterate persons [Graphs 6 and 7].
Table 1.
Distribution of cancer and noncancer persons according to occupation
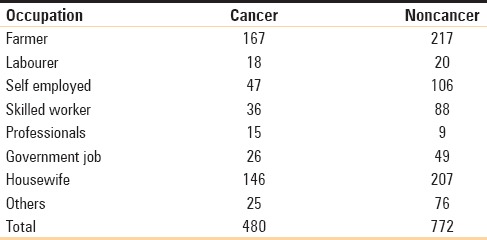
Table 2.
Distribution of cancer and noncancer persons according to expenditure (economic status)
Graph 6.
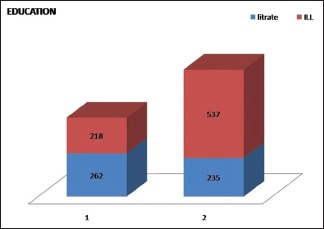
Distribution of cancer and noncancer persons according to education status
Graph 7.
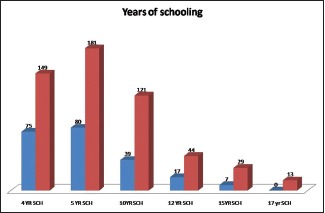
Distribution of cancer and noncancer persons according to education status
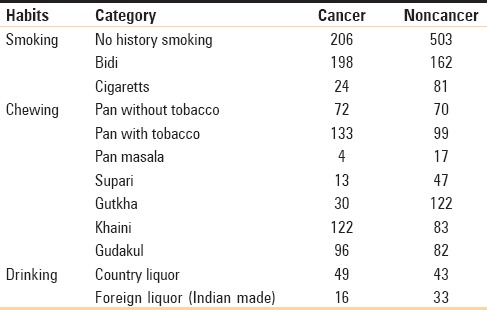
Prevalence and severity of oral habits were strong in the studied population but more concentrated in cancer groups [Table 3].
Table 3.
Distribution of cancer and noncancer persons according to oral deleterious habits
Tumor, node and metastasis stages
This parameter reveals the level of awareness of the disease in the society. Oral squamous cell carcinoma patients reported in later stages of their disease, as TNM stages represent that most of the patients reported in the 3rd and 4th stage (91.45% of total cancer patients). Unawareness may be the region of delayed reporting as the majority of these patients were illiterate and from lower socioeconomic status. Most of the patients were occupationally field workers. Metastases beyond the regional lymph nodes were not reported in any case.
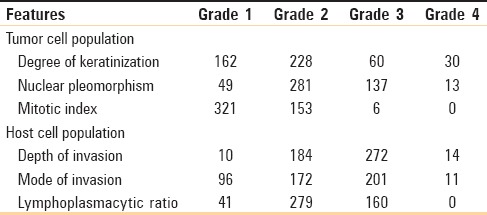
Histopathological grading
This parameter may be the good indicator for aggressiveness of tumor and host response to those tumor cells. The analysis of histopathological findings based on guidelines advocated by Anneroth et al. (1987) has been described. In this histopathological grading system, six parameters were divided into two categories, each incorporating three parameters, namely, tumor cell population parameters included the degree of keratinization, nuclear polymorphism, and mitotic index, whereas tumor-host relationship parameters incorporated mode of invasion, depth of invasion, and plasma-lymphocytic infiltrate [Table 4].
Table 4.
Histopathological grading of H and E stained sections (Anneroth et al. 1987)
DISCUSSION
In the present study, majority of the cancer patients were in their 5th, 6th, and 7th decades of life as 82.71% of cancer patients belong to this category, whereas only 17.29% of cancer patients belong to their 2nd and 3rd decades of life. Although it is well-known that oral cancer is more prevalent in older age groups, but there is a recent trend of rising incidence of oral cancer in younger patients, particularly on the tongue. Studies from India[9,10,11] and the present study also depicts the same trends; Many recent studies report that 4%–6% of oral cancers occur at ages younger than 40 years.[12] Distribution according to sex indicates that male to female ratio being 4:1 in Sri Lanka.[13] Supportively the present study also showed a male predominance in oral carcinoma, as male to female ratio was 1.79:1 in cancer group, whereas it was 1.61:1 in overall studied sample. A high proportion of cases among males may be due to the high prevalence of tobacco consumption habits among males. Moreover, tobacco is consumed in both chewing and smoking form in males, whereas in our society, very few females indulged in tobacco smoking.[11] However, some recent studies had reported a female predominance in the occurrence of squamous cell carcinoma in younger age groups.[13] This could partly be attributed to the increasing and more prolonged tobacco habits and alcohol consumption currently practiced by women.[13] The principal Asian religious community groups are Hindu and Muslims. Significant differences were found in males from these groups with regards to habits and oral cancer awareness. Muslim males use tobacco and pan more than the other groups but avoid alcohol. Habits of Hindu males are variable, Hindu males combine all three habits of alcohol, tobacco, and pan; and are thus considered to be at high risk of developing oral cancer.[11] The present study shows Hindus had 1.23 times greater prevalence of oral cancer compared to Muslims. Analysis of data from study sample conclude that 39.71% of all Hindus involved in this study had cancer, but in case of Muslims, this ratio is slightly less as 33.60% of total Muslims in the study have cancer. The General castes shows somewhat more risks (42.97%) compared to other castes (Other backwards, Scheduled Castes, and Scheduled Tribes) that have risks of cancer incidence around (31.79%). Analysis of data for marital status shows the significant difference as 42.90% of married patients considered in the study have cancer compared to 18.90% of whole patients included in the present study. Buccal mucosa with or without extension to the alveolar ridge was the most preferred site (49.45%), followed by the tongue (12.15%). This may be correlated with the tobacco chewing habit. Smokeless “Spit” tobacco contains over 2000 chemicals many of which have been directly related to causing cancer. “Pan” is the customized form of tobacco in which tobacco is wrapped inside a betel leaf and placed on the side of the mouth; tobacco has been chewed for centuries in India. This is commonly called as “khaini.” However, in the past decade, tobacco companies have started selling a sophisticated form of tobacco in ready-packaged small sachets. Mostly, these quids are kept under lips or below the tongue from where it is gradually absorbed after dilution with saliva. Thus, the buccal mucosa, tongue particularly the side of the tongue (farthest back in the mouth) the floor of the mouth (that area beneath the tongue) and alveolus are the site of maximum insult and thus are maximally affected.[10]
CONCLUSION
Prevalence of oral squamous cell carcinoma was high in the studied population of North-Eastern India. It was more common in poor socioeconomic groups, lower educational, lower income groups. Oral deleterious habits were more common in cancer groups compared to controls. Oral squamous cell carcinoma shows association with tobacco consumption, socioeconomic status, and genetic makeup of an individual. This work is the tip of the iceberg as limited access to our society or population due to hospital-based model of the study. This study raised the need of work in the field of oral cancer with some population-based module including genetic factors also.
Oral cancer is a great economic burden to patients as well as to the nation. Many health reports indicate that it is better to prevent than treat cancer. Our national polices should be skewed toward better health with zero use of tobacco.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to acknowledge Prof. Uma Shankar Pal, Prof. Shaleen Chandra, Prof. Anjana Majumdar, Dr Sourabh Bhattacharya, for their continuous support and guidance during the study.
REFERENCES
- 1.Conway DI, Petticrew M, Marlborough H, Berthiller J, Hashibe M, Macpherson LM, et al. Socioeconomic inequalities and oral cancer risk: A systematic review and meta-analysis of case-control studies. Int J Cancer. 2008;122:2811–9. doi: 10.1002/ijc.23430. [DOI] [PubMed] [Google Scholar]
- 2.WHO Fact Sheet; 2007. Report was published in February. 2007 [Google Scholar]
- 3.Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer. 1999;80:827–41. doi: 10.1002/(sici)1097-0215(19990315)80:6<827::aid-ijc6>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 4.Varghese C, Prasad V. Population Based Cancer Registry, Thiruvananthapuram 1991-1995. Regional Cancer Centre. 1999 [Google Scholar]
- 5.Khan Z. An overview of oral cancer in Indian Subcontinent and recommendations to decrease its incidence. WebmedCentral Cancer. 2012;3:WMC003626. [Google Scholar]
- 6.Murthy NS, Juneja A, Sehgal A, Prabhakar AK, Luthra UK. Cancer projection by the turn of century-Indian science. Indian J Cancer. 1990;27:74–82. [PubMed] [Google Scholar]
- 7.Vora AR, Yeoman CM, Hayter JP. Alcohol, tobacco and paan use and understanding of oral cancer risk among Asian males in Leicester. Br Dent J. 2000;188:444–51. doi: 10.1038/sj.bdj.4800506. [DOI] [PubMed] [Google Scholar]
- 8.Nandakumar A, Thimmasetty KT, Sreeramareddy NM, Venugopal TC, Rajanna, Vinutha AT, et al. A population-based case-control investigation on cancers of the oral cavity in Bangalore, India. Br J Cancer. 1990;62:847–51. doi: 10.1038/bjc.1990.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sankaranarayanan R, Duffy SW, Padmakumary G, Day NE, Krishan Nair M. Risk factors for cancer of the buccal and labial mucosa in Kerala, Southern India. J Epidemiol Community Health. 1990;44:286–92. doi: 10.1136/jech.44.4.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khandekar SP, Bagdey PS, Tiwari RR. Oral cancer and some epidemiological factors: A hospital based study. Indian J Community Med. 2006;31:157–9. [Google Scholar]
- 11.Madani AH, Dikshit M, Bhaduri D, Jahromi AS, Aghamolaei T. Relationship between selected socio-demographic factors and cancer of oral cavity – A case control study. Cancer Inform. 2010;9:163–8. doi: 10.4137/cin.s4774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murthy NS, Mathew A. Cancer epidemiology, prevention and control. Curr Sci. 2004;86:518–27. [Google Scholar]
- 13.Siriwardena BS, Tilakaratne A, Amaratunga EA, Tilakaratne WM. Demographic, aetiological and survival differences of oral squamous cell carcinoma in the young and the old in Sri Lanka. Oral Oncol. 2006;42:831–6. doi: 10.1016/j.oraloncology.2005.12.001. [DOI] [PubMed] [Google Scholar]


