Figure 3.
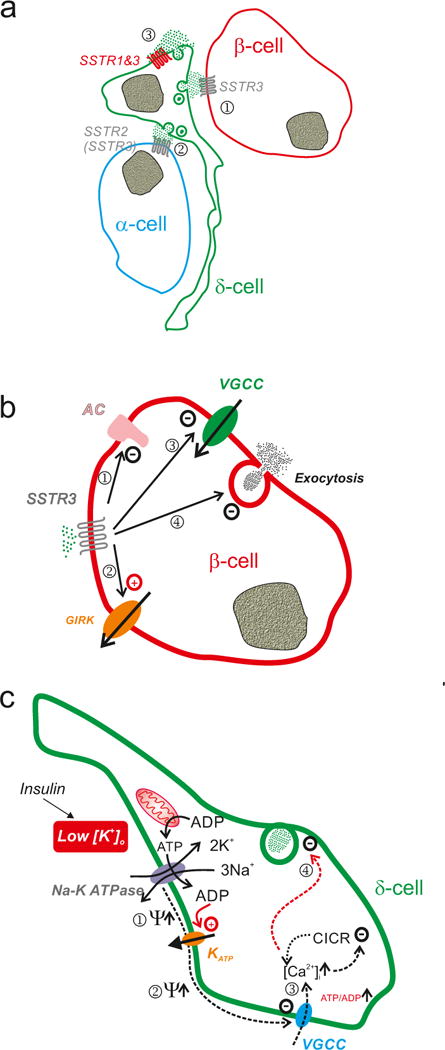
Somatostatin signalling in pancreatic islets. a| Schematic of somatostatin signalling in the islet. Somatostatin released from δ-cells activates SSTR2 (but also some SSTR3) in adjacent α- (1) and SSTR3 in β-cells (2) that are in close proximity to the δ-cell. In addition, somatostatin released from the δ-cells may exert an autocrine inhibitory effect by activation of SSTR1 or SSTR3 in the δ-cell itself (3). b| Effects of somatostatin in α- and β-cells. Activation of SSTR2 leads to: i) inhibition of adenylate cyclase, thereby resulting in lower cytoplasmic cAMP ([cAMP]i)113 and less cAMP-induced exocytosis; ii) inhibition of voltage-gated Ca2+ channels: iii) activation of G protein-regulated GIRK channels (producing membrane repolarization and inhibition of electrical activity)114,115; and iv) a direct inhibitory effect on exocytosis independent of [cAMP]i and that may involve activation of the protein phosphatase calcineurin115. c| Schematic how hypokalaemia (associated with insulin therapy) may stimulate somatostatin secretion. The Na-K pump is electrogenic and for every ATP hydrolysed 3 Na+ and 2 K+ are transported across the cell membrane in opposing directions, leading to a net loss of a positive charge inside the cell. Thus, the activity of the pump tends to repolarise the membrane potential (Ψ↑) (1). In addition, the activity of the pump may lower the submembrane ATP/ADP ratio, which maintains the KATP channels in the open state (potentially leading to further repolarization) (2). Inhibition of the pump (by lowering [K+]o) leads to membrane depolarisation by removal of the repolarising influence of the Na-K pump and exerting an ATP-sparing effect (the Na-K pump accounts for up to 50% of energy expenditure116) leading to closure of KATP channels. This leads to the initiation of electrical activity and Ca2+ entry/CICR (3) and stimulation of somatostatin release (4). Reduced expression of the Na-K pump (following hypokalaemia) may exert similar effects, thus increasing somatostatin secretion under hypoglycaemic conditions. This may account for the increased risk of recurrent hypoglycaemia (via reduced counter-regulatory glucagon secretion) in some insulin-treated patients.
