Abstract
Background: Previous studies have demonstrated the role of pharmacists during periods of transition of care. However, there are minimal studies that evaluate the impact that a pharmacist can have when a patient transitions his or her care to a new primary care provider (PCP). Objective: To assess the impact of a pharmacist-run medication “onboarding” service for patients new to a primary care (PC) practice. Methods: This prospective cohort study was approved by an institutional review board. Patients ≥50 years old and new to a PC practice were called by a pharmacist to obtain a medication list and identify any medication issues and recommendations. Recommendations were documented in the electronic medical record (EMR) and provided to the PCP prior to patients’ first appointments. After each appointment, the EMR was reviewed to determine the status of recommendations. As a comparison, the medication list and PCP’s initial appointment notes were reviewed for a similar cohort of patients not receiving a call. Medication-related actions taken at new patients’ first appointments were then compared between the pharmacist-assisted (intervention) and usual care (control) groups. Results: Forty-two percent versus 15% of medication issues were enacted in the intervention and control groups (P = .001), respectively. Seventy-seven percent of PCPs found the service beneficial and time-saving during initial new patient visits; 85% felt the service helped them manage patients’ medication therapy. Conclusion: A pharmacist-provided medication “onboarding” service results in significantly more medication issues addressed by the PCP compared with new patient visits not preceded by this service.
Keywords: clinical pharmacy, adult medicine, pharmacist/physician issues, medication errors, medication safety
Introduction
The role of a pharmacist during transitions of care (eg, discharge from hospital) in performing medication reconciliation and identifying medication-related issues is quite evident and well documented. However, there is scant evidence on how a pharmacist can influence the successful and efficient transition for a patient to a new primary care (PC) practice. One challenge in caring for new patients includes performing complete medication reconciliation. Medication reconciliation involves a comprehensive evaluation of a patient’s medication regimen any time there is a change in therapy in an effort to avoid medication errors such as omissions, duplications, dosing errors, or drug interactions, as well as to observe adherence patterns.1 Often, when a patient presents to a new primary care provider (PCP) for the first time, much of this initial visit is consumed in recording the past medical history, which frequently leaves little time to address an acute illness or need concerning a chronic illness.
Evidence suggests that pharmacists perform more complete and accurate medication histories by identifying a higher average of home medications per patient, and identifying more medication discrepancies than other health care professionals.1 It has been estimated that the medication profiles of PC patients are accurate in as less as 5.3% of patients.2,3 Inaccurate medication profiles may lead to medication errors or adverse drug events. One study has estimated that adverse drug events occur at a rate of 27.4 per 100 ambulatory patients.4 It is possible that these adverse events may have been preventable if the patients’ medication profiles were accurate. We hypothesized that having a pharmacist contact new patients via telephone prior to their first appointment with a new PCP would provide a more complete and accurate medication history that would be available to the PCP. We hypothesized that this service, termed medication “onboarding,” would lead to an increased identification of medication-related issues and drug cost savings opportunities that would be addressed at the initial appointment.
This study aims to contribute to existing knowledge on the role of pharmacists in medication reconciliation. Furthermore, this study evaluated whether pharmacists performing medication reconciliation and making drug therapy recommendations to a PCP results in more changes to drug therapy than when conducted without a pharmacist. The pharmacist’s recommendations were intended to optimize drug therapy, efficacy, safety, and cost-effectiveness. Documentation of these interventions is a valuable means of identifying the role of pharmacists within the patient care team, and the subsequent impact made on the quality of care provided to patients. The primary outcome for this study is the number of medication recommendations acted upon by the PCP during the patients’ first visit after medication “onboarding,” compared to the number of medication issues addressed by the PCP during the patients’ first visit in the control group. Secondary outcomes include categorization of the types of recommendations identified, results of a PCP satisfaction questionnaire, and financial assessment of the service through calculation of the return on investment.
Objective
The purpose of this study is to assess the impact of implementing a telephonic pharmacist medication “onboarding” phone service, termed Medication Onboarding, for new patients to a PC practice.
Methods
The institutional review board of an affiliated university approved the protocol for this prospective cohort, single-center study. The study was conducted at one of the institution’s PC practice sites located in Massachusetts.
Each week the pharmacist received a list of new patients who had recently joined the PC practice, which was filtered to identify patients who met the specified inclusion criteria. The 261 patients included in the study were new patients to the Internal Medicine (IM) Department, were ≥50 years old, and had been assigned a PCP. The 1156 patients excluded from the study had their first appointment in a specialty clinic rather than in IM, were <50 years old, or were not yet assigned a PCP. Of note, when data collection for the study began the age criteria for inclusion was ≥40 years old. After 28 weeks of data collection, an interim data analysis was performed and it was discovered that it was unnecessary to perform medication “onboarding” for a majority of the patients between the ages of 40 and 50 years because they were not taking any medications. As a result the age criteria was changed in order to capture patients who would benefit most from the service.
Starting in July 2013 the new patient lists were scanned by the pharmacist. During the first 3 months, the patients that met the inclusion criteria did not receive a call from a pharmacist and served as the control group. Additional control patients were those that met inclusion criteria and joined the practice later but whose first IM appointment occurred before the pharmacist was able to contact the patient. Data collection for the intervention group began at the end of September 2013. Data collection for both groups continued until May 2014.
The intervention subjects received a telephone call from the pharmacist prior to their initial IM appointment to obtain their current medication lists and drug allergies, address medication adherence, and to identify any medication issues. Medication issues included drug–drug interactions, duplicate drug therapy, unnecessary medications, and opportunities for switching therapy to cost-saving medications. The pharmacist also recorded each patient’s preferred pharmacy and provided education about the pharmacy located in the practice site. This information was documented in the patient’s electronic medical record (EMR) and accessible for health care providers to see. On identification of a medication issue or concern, the pharmacist electronically sent recommendations in a message to the PCP so that it would be received the day prior to the patient’s first appointment. After the patient’s appointment with the PCP, the pharmacist reviewed the EMR to determine whether or not each recommendation was acted upon.
In the control group, the pharmacist performed a chart review to identify any medication issues and recommendations that were documented in a separate secure database, concealed from the PCPs. The pharmacist reviewed the patient’s medication list and drug allergies that were entered into the EMR by the PCP during the patient’s first appointment and then reviewed the progress note to compare the concealed recommendations the pharmacist had identified to the medication issues addressed by the PCP. By reviewing the initial progress note, the pharmacist was able to determine if the medications issues they had identified were also identified and addressed by the PCP.
Data from a similar Medication Therapy Management Program at our institution showed that medication recommendations sent by the pharmacists to PCPs resulted in a PCP acceptance rate of 75% or 0.8 recommendations per patient. Therefore, we assumed that at least 75% of the recommendations provided during medication onboarding would be accepted. If the percentage of medication issues identified by a pharmacist and acted on by the PCP during usual care is 50% or less, then the impact of medication “onboarding” is considered statistically significant. The number of recommendations required to detect this 25% difference at the 5% level of significance with 80% power is 64 recommendations per group.5 Dividing this value by 0.8 recommendations/patient yields a sample size of 80 patients per group. This value ensured that sufficient data were available for statistical analysis.
Fisher’s exact test was used to compare the percentage of medication issues identified and addressed in each group. Results were considered statistically significant if the observed level of significance was P < .05. In addition, patient demographics, classification of the types of medication recommendations identified and the results of the PCP satisfaction questionnaire were summarized using descriptive statistics, including percentages and means. The Number Cruncher Statistical System software was utilized to perform all statistical analyses.6
Results
A total of 103 patients met inclusion criteria for the intervention group and 158 patients for the control group. All patients in the intervention group were included in the data analysis. A table of random numbers was used to identify 103 control patients to be included in the data analysis. There were no significant differences in baseline characteristics. Seventy-one medication recommendations were identified in the control group versus 79 identified in the intervention group. Recommendations were classified as accepted, amended, rejected, unaddressed, or pending. Table 1 summarizes the classification of recommendations. For the primary outcome, there was a statistically significant difference in the percentage of recommendations addressed by the PCP in the intervention group versus the control group, 42% versus 15%, respectively (P = .001). There was no statistical difference between recommendations that were amended, rejected, or pending.
Table 1.
Classification of Recommendations.
| Classification of Recommendation | Control (n = 71), % (n) | Intervention (n = 79), % (n) | P Value |
|---|---|---|---|
| Accepteda | 15.4 (11) | 41.8 (33) | .001 |
| Amendedb | 2.8 (2) | 1.3 (1) | .603 |
| Rejectedc | 33.8 (24) | 21.5 (17) | .102 |
| Unaddressedd | 28.2 (20) | 17.7 (14) | .171 |
| Pendinge | 19.7 (14) | 17.7 (14) | .835 |
Abbreviations: PCP, primary care physician; EMR, electronic medical record.
PCP implemented the specific recommendation sent by the pharmacist.
PCP did not implement the specific recommendation sent by the pharmacist, but addressed the medication issue. For example, the pharmacist may have recommended a switch from the brand statin Crestor (rosuvastatin) to the generic statin, atorvastatin; however, the PCP may have switched the patient to pravastatin instead.
PCP’s notation in the EMR indicated that he/she did not implement the recommendation.
There was no clear indication in the patient’s EMR that the PCP discussed the recommendation.
The recommendation was not able to be addressed because the patient cancelled the appointment and did not reschedule during the study period.
The secondary outcome of categorization of the types of recommendations is summarized in Table 2. Recom-mendations were categorized as cost saving, cost saving plus quality improvement, or quality improvement. The majority of recommendations made in each group were categorized as cost-saving recommendations, 68% versus 52% (P = .046) in the intervention versus control group, respectively. Figure 1A and B further categorizes the types of cost-saving recommendations into Winback, increased encounters, incomplete medication lists, medication adjustments, drug dose tapers, drug interaction mitigation, switches from nonpreferred to preferred medications, or other. Winback is a term used by our institution to describe transferring prescriptions to our onsite pharmacies.
Table 2.
Types of Recommendations.
| Type | Control (n = 71), % (n) | Intervention (n = 79), % (n) | P Value |
|---|---|---|---|
| Cost savinga | 52.1 (37) | 68.4 (54) | .046 |
| Cost saving + quality improvementb | 40.8 (29) | 10.1 (8) | .001 |
| Quality improvementc | 7.0 (5) | 21.5 (17) | .119 |
Recommendation was associated with savings in health care dollars.
Recommendation was intended to optimize patient care and have savings in health care dollars.
Recommendation was intended to optimize patient care without having a direct saving of healthcare dollars.
Figure 1.
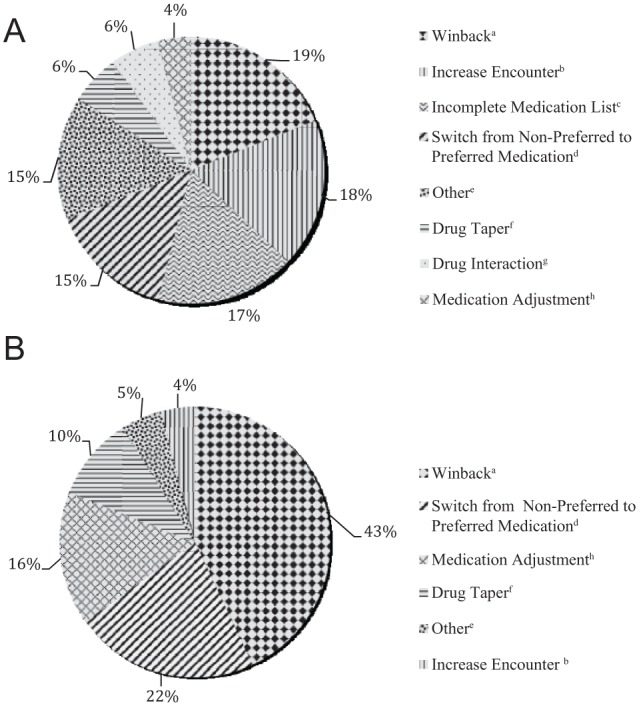
(A) Categorization of cost recommendation made in the control group. (B) Categorization of cost recommendations made in the intervention group.
aWinback is a term used by our institution to describe patient’s filling prescriptions at our onsite pharmacy. bIncreased encounters included scheduling a patient for an IM appointment who was not originally scheduled or had cancelled their appointment. cWhile reviewing the EMR of control patients it was discovered by the clinical pharmacist that the PCP sometimes would discuss the patient being on a certain medication in the progress note, but not enter it into the medication list in the EMR, thus resulting in an incomplete medication list. dSwitching from a nonpreferred to preferred medication included switching from a medication that was not on our institution’s formulary to one that was on the formulary. eExamples of recommendations classified as others include discontinuation of duplicate therapy or unnecessary medication or initiation of a medication. fDrug tapering included tapering a patient off of medications such as a proton pump inhibitor. gDrug interaction included those that would lead to adverse effects or impact patient’s quality of care. hMedication adjustments included changing the dose or schedule of a medication.
PCP satisfaction, a secondary outcome, was measured with an anonymous nonvalidated 5-item questionnaire and distributed to all 13 PCPs who participated in the service. Questions addressed benefit of the service and if it should continue, time the PCP saved, value of pharmacist recommendations, and patient feedback. Seventy-seven percent of PCPs found the service beneficial, and felt it saved them time (average of 5 minutes/patient visit) while 77% of the patients did not provide feedback about the phone call they received from the pharmacist. Eighty-five percent of PCPs felt the service helped them manage patients’ medication therapy and wanted the service to continue.
The service required the pharmacist to allocate time away from his/her normal duties; thus, it was pertinent to determine that the time the pharmacist was investing in the service would result in health care savings for the institution. Health care savings can be defined as savings through actual cost reduction and cost avoidance. This was estimated by comparing the cost of the hours the pharmacist spent performing service, using the pharmacist’s salary, to the direct cost savings or cost avoidance from the accepted recommendations. Table 3 summarizes the health care savings associated with accepted recommendations. The secondary outcome of the financial impact was determined by calculating the return on investment using the equation (amount of health care dollars saved during the duration of the study/[average time spent per patient × number of patients × hourly wage of pharmacist performing service]). It was calculated that for every $7.30 of health care savings, $1 was spent to have a pharmacist perform the service.
Table 3.
Annualized Health Care Savings.
| Control Group | Intervention Group | |
|---|---|---|
| Savings during study period (33 weeks)a | ||
| Savings | $9100 | $18 100 |
| Potential savingsb | $1500 | $5000 |
| Total | $10 600 | $23 100 |
| Estimated annual savings (52 weeks)c | ||
| Savings | $14 000 | $28 400 |
| Potential savingsb | $2400 | $7900 |
| Total | $16 400 | $36 300 |
Healthcare Savings Examples: (1) Savings for Winback for 1 scheduled medication was $25/month or $300/year; (2) Savings for Winback for 1 as-needed medication was $25/year since we were unable to determine how often prescription was filled; (3) Savings for tapering a proton pump inhibitor was $100; (4) Savings for increasing a patient encounter was $102; (5) Equation for calculating savings when switching from nonpreferred to preferred medication included [(Yearly cost of nonpreferred − yearly cost of preferred) − annualized copay differential ($360)].
Potential savings is the amount of health care dollars that could be saved assuming all the pending recommendations will be accepted.
If the measurement period was extended an additional 19 weeks totaling 52 weeks (1 year) and recommendations continued to be made and accepted at the same rate as during the 33 week period we calculated the savings.
Discussion
To our knowledge, the current study is the first to detail a telephonic medication “onboarding” service. This study demonstrated that having a pharmacist telephonically perform medication onboarding for new patients entering a PC practice resulted in a higher percentage of medication issues being identified and addressed. The difference between the percentages of medication issues addressed or recommendations accepted was statistically significant, indicating the positive impact of this service.
Pharmacists are valuable members to the interdisciplinary team and use their professional expertise to enhance the care of patients through medication optimization. Prior to implementation of telephonic medication onboarding, pharmacists were not involved in medication evaluation of new patients at the practice. A medical assistant entered patients’ medication lists and drug allergies into the EMR, and the PCP performed medication reconciliation. This study validated the impact pharmacists can have in optimizing patient’s medication therapy, as well as subsequent cost savings associated with medication evaluation. This study showed that without the assistance of a pharmacist, PCPs appear to address less than one fifth of the medications issues that were identified by the pharmacist.
Caring for patients who are transitioning to a new PC practice can be a laborious and challenging task for the health care team. During an initial appointment a PCP is faced with completing an extensive evaluation of the patient. This may include reviewing the current medication regimen, past medical history, and addressing any acute concerns, all which occur within a limited time frame. Any acute issues the patient is experiencing may consume a significant portion of the appointment, thus limiting the time available to perform a complete medication reconciliation and evaluation. Having a pharmacist reconcile and comment on patients’ medications before the initial appointment resulted in time saved during the initial appointment, which was confirmed by the PCP satisfaction questionnaire. The time saved may allow the PCP to spend more time focusing on patient’s acute issues, prevent appointments from running late, and allow PCPs to schedule more appointments.Due to the high cost of health care, our institution strives to contain medication costs while maintaining patients’ quality of care; Medication Onboarding fulfills this description. The majority of recommendations made by the pharmacist in both groups were categorized as cost-saving recommendations that resulted in health care savings. The estimated annualized cost savings of $18 100 in the intervention group and $9100 in the control group is representative of the 33-week study period. If recommendations continued to be accepted at the same rate for an additional 19 weeks, totaling one full year, savings were projected to be $28 400 in the intervention group and $14 000 in the control group. These results indicate that medication onboarding would result in double the amount of savings. In addition, there are savings associated with recommendations that could not be addressed at the PCP appointments due to cancellation of appointments. These savings are termed “potential savings” and can be found in Table 3.
Medication Onboarding has resulted in adjustments to patient’s medication therapies with subsequent health care savings and was well received by clinicians; thus, it was determined to expand the service to additional IM practice sites of our institution. At these sites, the workflow of the service has been further improved to optimize the pharmacist’s time. An office manager is calling all new patients, welcoming them to the site, and determining whether they are taking any medications. Patients taking medications will either be transferred to the pharmacist or are scheduled for a telephone appointment with the pharmacist for a later time up until the date of the first PCP appointment. This change in the service eliminated the need for the pharmacist to filter through the list of new patients, and allowed them to perform medication onboarding to those patients who are currently taking prescribed medications. The service has also expanded to all ages. Based on the results of this study, it is evident that pharmacist involvement in medication evaluation of new patients at our institution resulted in health care savings from adjusting therapy for clinical optimization.
Limitations
The first limitation of the study includes the reliance on progress notes entered into the EMR to determine the status of recommendations. This led to the inability of the pharmacist to determine the status of all recommendations sent to the PCPs. Eighteen percent of recommendations in the intervention group and 28% of recommendations in the control group were categorized as unaddressed after the first PCP appointment. It is possible that the PCP may have addressed some of the recommendations verbally with the patient, but did not document this information in the EMR, therefore leaving the pharmacist to believe the recommendation was unaddressed.
It is also possible that the PCP did not view the recommendations sent by the pharmacist as the pharmacist did not have a way to identify if the recommendations were reviewed. When reviewing status of recommendations in the intervention group, it was assumed that the PCP had received and reviewed recommendations sent by the pharmacist.
The study was short in duration (33 weeks); therefore, if patients cancelled appointments and did not reschedule during the study time period recommendations sent were lost to follow-up. However, all recommendations sent to the PCPs were documented in the EMR, which would allow the PCP the opportunity to review the recommendations once the patient rescheduled an appointment.
The pharmacist relied on patients to find their medication vials at home and provide a complete medication list. If patients were not home, the pharmacist would call the patient back, schedule a telephone appointment, or provide the patient with a number to call the pharmacist at their convenience to ensure patients had all their medication vials when speaking with the pharmacist. It is possible that patients could have looked at an old medication vial, incorrectly read the medication label, or not have medication vials readily accessible if medications were prepacked, thereby limiting the accuracy of the medication list entered into the EMR.
Unfortunately, there were cost-savings opportunities that were unable to be measured and thus it is unknown how much they would contribute to the health care savings associated with implementation of the service. Examples of nonmeasurable cost-saving opportunities include addressing patients’ medication issues before they resulted in medication errors, retaining patients to the practice by making them feel welcomed, and saving PCP time during appointments, which would help keep the PCPs on schedule and permit them the time to see more patients.
Last, the demographics of the population included in the study may also be a limitation. This study took place at a site in a wealthy suburban area and therefore may not be representative of the overall population.7
Conclusion
A pharmacist can promote optimization of medication regimens by reconciling and evaluating medications prior to patients transitioning their care to a new PC practice. Through interprofessional collaboration with PCPs, medication issues were more frequently identified and resulted in a statistically significant higher percentage of medication issues being acted upon. Collaboration with the PCPs not only ensured patient’s medication regimens were optimized, but also was estimated to have savings in health care dollars. This study adds to the current literature surrounding the role a pharmacist can play during transitions of care; however, it details a unique telephonic approach to medication optimization that is not well studied. It is important to recognize that these results may not be suitable for generalization.
Acknowledgments
To Seth Robin, MBA, Manager of Pharmacy Finance and Reporting, Atrius Health, for retrieving data and Gary Tataronis, MS, Associate Professor of Statistics and Mathematics, MCPHS University, for employing statistical methods.
Footnotes
Authors’ Note: At the time this study was conducted, Emily A. Barker was a PGY1 Pharmacy Resident at MCPHS University/Atrius Health.
This article was presented at the ASHP Midyear Clinical Meeting, Orlando, FL, December 11, 2014; and at the Massachusetts Society of Health-System Pharmacists Annual Meeting, Newton, MA, April 1, 2014.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011;171:1232-1237. [DOI] [PubMed] [Google Scholar]
- 2. Bedell SE, Jabbour S, Goldberg R, et al. Discrepancies in the use of medications: their extent and predictors in an outpatient practice. Arch Intern Med. 2000;160:2129-2134. [DOI] [PubMed] [Google Scholar]
- 3. Kaboli PJ, McClimon BJ, Hoth AB, Barnett MJ. Assessing the accuracy of computerized medication histories. Am J Manag Care. 2004;10(11 pt 2):872-877. [PubMed] [Google Scholar]
- 4. Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556-1564. [DOI] [PubMed] [Google Scholar]
- 5. Hintze J. PASS (Power Analysis and Sample Size). NCSS, LLC. Kaysville, UT: NCSS, LLC; 2008. [Google Scholar]
- 6. Hintze J. NCSS (Number Cruncher Statistical System). Kaysville, UT: NCSS, LLC; 2007. [Google Scholar]
- 7. US Census Bureau. Wellesley CDP, Massachusetts. http://quickfacts.census.gov/qfd/states/25/2574210.html Accessed July 14, 2014.


