Abstract
Background: The consumption of industrially produced trans fatty acids (TFAs) has been associated with an increased risk of heart disease. In recognition of this, countries, states, and cities worldwide have implemented TFA policies aimed at reducing their availability in the food supply.
Objective: This article aims to provide an update of the evidence of the effectiveness of policies aimed at reducing TFAs in the food supply.
Methods: A systematic review of the literature from 2013 onward was conducted, building on a previously published review that examined the evidence of the impact of TFA policies worldwide from 2000 to 2012. Studies that were 1) empirical, 2) examined a TFA policy, and 3) examined the effect of the policy on TFA amounts and availability pre– and post–policy intervention were included. Modeling studies examining the impact of TFA policies on cardiovascular, equity, and economic outcomes were also included.
Results: A total of 18 articles from the updated search were combined with 14 articles from the previous review (total = 32 articles). All types of TFA policies led to their reduction; however, trans fat bans had a larger impact (TFAs virtually eliminated) than did voluntary (range: 20–38% reduction in TFA intakes) or labeling (range: 30–74% reduction in TFA intakes, plasma serum, or breast-milk concentrations) approaches to reducing TFA amounts in the food supply. Product reformulation to reduce TFAs had variable effects on saturated fatty acid (SFA) contents in these foods; however, the combined amount of TFAs and SFAs declined in most products. Overall, the modeling studies indicated that TFA bans would reduce heart disease risk, benefit socioeconomically disadvantaged populations the most, and be cost-saving.
Conclusions: Policies aimed at reducing TFAs in the food supply are effective and will likely reduce the burden of diet-related disease, particularly among the most vulnerable socioeconomic groups. Although all policy approaches lead to reductions in TFAs in foods, TFA bans are likely the most effective, economical, and equitable policy approach to reducing TFAs in the food supply.
Keywords: trans fatty acids, cardiovascular disease prevention, nutrition policy, bans, labeling
Introduction
The consumption of trans FAs (TFAs) has been associated with an increased risk of coronary heart disease (CHD) (1). Although there are small amounts of naturally occurring TFAs in ruminant animal products, the majority of TFAs consumed are industrially produced (2). The main source of industrially produced TFAs is partially hydrogenated oils (PHOs) often found in fried snacks and bakery products. Their removal from the food supply has been deemed one of the most straightforward public health interventions for rapid improvements in health (3) and is considered a “best buy” for tackling diet-related noncommunicable diseases in low- and middle-income countries (LMICs) (4). Policy approaches to address the removal of TFAs from the food supply are likely the most effective in terms of reducing consumption amounts. Despite this, most countries worldwide have yet to introduce strong policy measures to limit TFA intakes and they continue to be widely consumed around the world (5).
The Global Burden of Diseases Study found a 5-fold difference in TFA consumption between countries in 2010, ranging from 0.2% to 6.5% of energy intake, with the mean global TFA intake at 1.4% of total energy intake (5). This exceeds the WHO recommendations to limit consumption to <1% of total energy intake (6). The highest intakes were found in Egypt, Pakistan, Canada, Mexico, and Bahrain (5). Even in countries such as the United States, where there has been significant progress in terms of product reformulation after the introduction of mandatory TFA labeling, intakes remain above recommended levels among some pockets of the population (7).
Countries that have taken action to limit TFA contents in foods have generally adopted mandatory TFA labeling policies or set TFA limits (often referred to as bans). There have also been voluntary approaches to TFA reduction via product reformulation, often spearheaded by nongovernment stakeholders, including industry and public health groups. Denmark was the first country to ban TFAs in 2003, and a handful of other countries have since followed suit (Supplemental Figure 1). Although over the past 20 y there has been a reduction in TFAs in the food supply of the majority of countries that have measured them (8), in recent years there has been growing momentum for adopting TFA bans or limits in an effort to eliminate TFAs from the food supply. In June 2015, the US FDA made a final decision to remove the “generally recognized as safe” (GRAS) status from PHOs in the United States, which will essentially act as a countrywide TFA ban once it goes into effect in June 2018 (9). Canada also recently took steps to ban TFAs, which is planned to go into effect in September 2018; meanwhile, the European Commission is considering setting a TFA limit (10).
This article aims to provide an update of the evidence of policies aimed at reducing TFAs in the food supply. A systematic review of the literature from 2013 onward was conducted, building on a previously published review that examined the evidence of the impact of TFA policies worldwide from 2000 to 2012 (11). This article updates that review by examining the literature from 2013 to 2016 and compiles this with the evidence from the previously published review. Since the initial review, a number of studies examining the impact of TFA policies worldwide have been published. To better inform TFA policy development, updating the current state of the evidence is necessary.
Methods
A systematic literature search was conducted in August 2017 by using the Medline (http://www.ovid.com/site/catalog/databases/901.jsp), Embase (http://www.embase.com), and Cinahl (www.cinahl.com) databases to identify peer-reviewed articles that examined the impact of TFA policy. The main search terms were “trans fat” and “policy.” Additional search terms to represent TFAs were as follows: “trans fatty acid,” “hydrogenation,” “vanaspati,” “elaidic acid,” and “margarine.” Policy terms included “regulation,” “nutrition policy,” “health policy,” “legislation,” “ban,” “intervention,” “labeling,” “law,” “standards,” and “restriction.” Terms were included both as keywords as well as free text searches in titles and abstracts, depending on the database being searched. The search terms and databases used were the same as those in the previously published systematic review. In addition, the first 20 pages of Google were examined to identify additional studies published in the gray literature.
Inclusion criteria
The inclusion criteria for the review were that the studies were 1) empirical, 2) examined a TFA policy (labeling, voluntary limits, bans, etc.), and 3) examined the effect of the policy on TFA contents or availability (in food, blood, dietary consumption, breast milk, etc.). In addition to the aforementioned inclusion criteria, only studies that had pre– and post–policy intervention data were included in the review. This differed from the previous review, which included studies even if they solely presented findings post–policy intervention. Studies included in the previous review that did not present pre- and post-data were not included in this review. Moreover, unlike the previous review, modeling studies of TFA policies were included to enable the inclusions of studies that examined the following: 1) differences in policy impacts on specific segments of the population (e.g., lower socioeconomic groups) and 2) cost-effectiveness studies. Studies that modeled the potential impact of front-of-pack labeling (not specific to TFAs) on TFA intakes were not included. Given that the previous review did not include modeling studies, the modeling studies published between 2000 and 2012 were added to the search conducted as part of the updated review.
Overview of search
The records identified through our searches were exported into EndNote, version X5 (2011; Thomson Reuters), and duplicates were subsequently removed. The records were then imported into Covidence (Veritas Health Innovation; an online software to facilitate the systematic review process) to screen the records. Two researchers (SMD and MZB) independently reviewed the titles and abstracts of all records identified in our search. After removing records that did not meet the inclusion criteria, the full texts of the remaining articles were reviewed by both researchers to determine whether the studies met our inclusion criteria. In the event that the 2 researchers disagreed, a third researcher (JHYW) was consulted and a decision reached by consensus. The reference lists of the full articles were also examined in order to identify additional studies that met the inclusion criteria.
Study extraction
One researcher (MZB) extracted data from the full texts of the articles included in the review. The data extractions were then reviewed by a second researcher (SMD). The following data were extracted from each study: aim, location, design, type and year of intervention, data collection period, population, sample size, outcomes measured and their assessment method, results, summary of findings, conclusions, limitations, assumptions (for modeling studies), and source of funding.
Study quality assessment
To assess the overall quality of the studies that collected primary data (i.e., non–modeling studies) included in the review, the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool was used (12). The tool was adapted to reflect the study designs included in the review. The tool is designed to assess study quality on the basis of 6 domains: selection bias, study design, confounders, blinding, data collection method, and withdrawals or dropouts. Given the types of studies included in the review, blinding and withdrawals or dropouts were not included in our quality assessment. Each study was given a ranking of weak (score = 1), moderate (score = 2), or strong (score = 3) for each of the remaining 4 domains on the basis of the EPHPP quality assessment tool's dictionary (12, 13). An overall score was then generated by compiling the scores for each domain and assigning an overall study quality rating of weak, moderate, or strong. If a study had ≥2 weak ratings it was considered weak, if it had only 1 weak rating it was considered moderate, and if it had no weak ratings it was considered strong.
Results
Overview of included studies
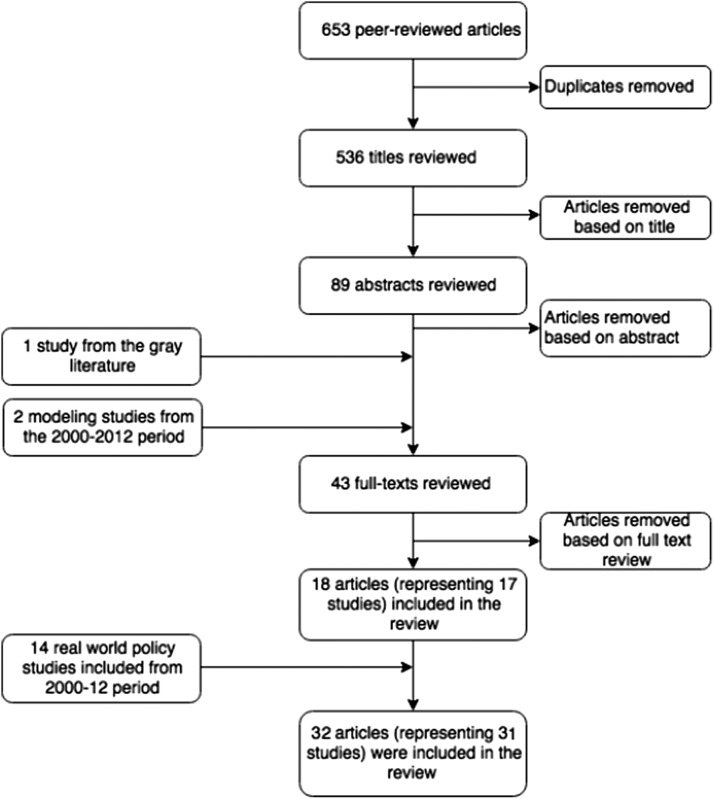
Figure 1 depicts the search flow diagram of this review. We searched the full text of 43 articles [41 identified in our search (including 1 from the gray literature) and 2 modeling studies from 2000 to 2012]. Eighteen articles (representing 17 distinct studies) met our inclusion criteria and were added to the 14 articles from the previous review. The main reasons for excluding articles on the basis of the full-text review were as follows: were duplicates (n = 3), were included in the previous review (n = 5), had no TFA policy (n = 3), were commentaries (n = 3), or did not have a pre-post study design (n = 11). Only one of the included studies was obtained from the gray literature search (14). The majority of the included studies were from high-income countries; only 3 were from LMICs (Argentina, Costa Rica, and Iran).
FIGURE 1.
Flow chart of the systematic review.
TFA interventions in the “real world”
Supplemental Table 1 provides an overview of the “real world” studies included in the review, which combines the updated search with the before and after studies included in the previous review. The studies examined voluntary self-regulation (n = 4; Costa Rica, Netherlands, and the Americas) (15–18), mandatory labeling (n = 8; South Korea and the United States) (3, 19–25), mandatory labeling in addition to voluntary TFA limits (n = 6; Canada) (26–31), mandatory TFA limits in restaurants (n = 4; New York City) (32–35), and mandatory TFA limits in PHOs (n = 1; Iran) (14) and all foods (n = 1; Denmark) (36). In terms of the overall quality of the studies included in this review, nearly all were classified as weak. The main contributing factors to the studies deemed weak by the EPHPP quality assessment tool were related to the weak study designs, high risk of selection bias, and data collection methods that lacked strong validity, reliability, or both.
The impact of different policy approaches on TFAs
All of the studies examined reported a reduction in TFA amounts in food, breast milk, plasma serum, or dietary intakes; however, there were differences based on the type of policy adopted, as described below (Tables 1–3).
TABLE 1.
Impact of TFA policies on dietary intakes, concentrations in plasma serum and breast milk, and cardiovascular outcomes1
| Policy type | Study (ref), country/region | Time period | Measurement | Impact |
|---|---|---|---|---|
| Voluntary self-regulation | Monge-Rojas et al. (16), Costa Rica | 1996–2006 | Dietary intake of TFAs as a percentage of total fats | 38% reduction |
| Colón-Ramos et al. (15), Costa Rica | 1994–1999 to 2000–2003 | TFAs in subcutaneous adipose tissue and risk of MI | • Reduction in TFAs in tissue of those that did not use PHVOs | |
| • TFAs in tissue no longer associated with increased risk of MI | ||||
| Temme et al. (18), Netherlands | 2001 to 2009–2010 | Dietary intake of TFAs as a percentage of total fats | 20% reduction | |
| Mandatory TFA labeling on packaged foods | Vesper et al. (24), United States | 2000–2009 | Plasma TFA concentration | 58% reduction |
| Vesper et al. (23) and Yang et al. (25), United States | 1999–2000 to 2009–2010 | Plasma TFA concentration | 54% reduction | |
| Mandatory TFA labeling + voluntary TFA limits | Friesen and Innis (27), Canada | 1998 to 2004–2006 | Breast-milk TFA concentration | 35% reduction |
| Ratnayake et al. (28), Canada | mid-1990s to 2008 | %TFAs of total fats | 30% reduction | |
| Ratnayake et al. (30), Canada | 1992–2011 | Breast-milk TFA concentration | 74% reduction | |
| Mandatory TFA limits in restaurants | Brandt et al. (34), NYC | 2000–2010 | Stroke and MI rates | Greater decline in stroke than would have been expected based on temporal trends (for younger age group only) |
| Restrepo and Rieger (35), NYC | 1999–2013 | CVD mortality rates | 4.5% reduction in CVD mortality rates | |
| Mandatory TFA limits in foods | Leth et al. (36), Denmark | 1995–2005 | Total amount of TFA in grams | TFAs decreased from 1.5 g/d in 1995 and were virtually eliminated in 2005 |
CVD, cardiovascular disease; NYC, New York City; MI, myocardial infarction; PHVO, partially hydrogenated vegetable oil; ref, reference; TFA, trans fatty acid; %TFA, percentage of trans fatty acid.
Voluntary approaches.
The 4 studies that examined voluntary approaches to reducing TFA intakes found reductions in TFA intakes, concentrations in tissues, and contents in food. In addition, TFA concentrations in tissues were no longer associated with an increased risk of myocardial infarction (MI) in Costa Rica after the introduction of self-regulation; however, in some cases, TFA intakes remained high (15–17). In Costa Rica, where there was industry self-regulation, the number of adolescents who exceeded the WHO recommendations (<1% of total energy intake from TFAs) for TFA consumption declined by 32 percentage points between 1996 and 2006 in a population of urban and rural public school students; however, the number of adolescents exceeding the limit remained high (68% in 2006 compared with 100% in 1996) (16). In comparison, there was a 20-percentage point reduction in TFA intakes in the Netherlands, which coincided with average TFA intakes that were below the WHO recommendations (0.8% of energy intake).
TFA labeling.
The majority of the studies that looked at the impact of mandatory TFA labeling were conducted in the United States and Canada, with the exception of one study conducted in South Korea. Although the TFA-labeling policies differed slightly among these 3 countries (e.g., foods were considered TFA-free at <0.2 g TFAs/serving in South Korea and Canada compared with <0.5 g TFAs/serving in the United States), all were associated with reductions in TFA amounts in foods. However, it is important to note that TFA amounts remained high in some product categories. For example, the TFA content in coffee whiteners was, on average, 38.3% of total fat in Canada (26). Moreover, in 2 product categories (coffee whiteners and lard or vegetable shortenings), the number of products meeting the voluntary TFA limits in Canada actually declined between 2005–2009 and 2010–2011 (26). In addition to observing declines in TFA amounts in foods, for the most part, all studies examining the impact of mandatory labeling policies in the United States and Canada on biological outcomes found large reductions in TFA concentrations in serum plasma (ranging from 54% to 58%) (23–25) and breast-milk and dietary intakes (ranging from 30% to 74%) (27, 30).
Mandatory TFA limits in restaurants.
Four studies (32–35) looked at the impact of the TFA limit in New York City restaurants. Two of the studies examined the impact on MI and stroke, one of which found a 4.5% reduction in cardiovascular disease (CVD) mortality associated with the policy (35) and the second reporting a greater decline in stroke among younger age groups (who also consumed more restaurant foods) than would have been expected if the policy had not been enacted (34). However, it is important to note that the time lag between the introduction of the TFA policy and the analysis of hospital admissions due to MI or stroke was only 3 y. The 2 studies that examined TFA contents in foods found that nearly all (98%) restaurants were using TFA-free oils after the policy came into effect compared with only 50% of restaurants before its enactment (33). Moreover, the purchase of TFA-free meals increased by 86% (32).
Mandatory TFA limits in food.
Only 2 of the included studies examined the impact of TFA limits in foods and oils: one in Iran and another in Denmark. In Denmark, the 2% TFA limit led to the virtual elimination of TFAs from the food supply (36). In Iran, where the TFA limit has been gradually reduced over time from 20% in 2005 to 10% in November 2007, there have been reductions in the quantity of TFAs in edible oils (31.2% in 2004 compared with 5.62% in 2008); however, TFA amounts in oils remain high (14).
TFA-free products.
Table 2 synthesizes the evidence relating to the number of TFA-free products in the food supply coinciding with mandatory and voluntary TFA limits as well as labeling regulation. Mandatory national bans have virtually eliminated TFAs from the food supply, whereas voluntary limits and labeling policies have led to an increase in the number of TFA-free products; however, there is still further progress to be made.
TABLE 2.
Percentage of foods classified as TFA-free post–policy interventions1
| Policy intervention | Countries/regions | Food categories | TFA-free,2% |
|---|---|---|---|
| National bans | Denmark | Overall | Virtually eliminated |
| Local bans (32) | NYC | All fast-food purchases | 59 |
| Mandatory labeling + voluntary limits (26, 29) | Canada | Margarines/spreads | 0–85 |
| Bakery products | 25–100 | ||
| Restaurant food (including restaurants in institutions) | 50–100 | ||
| Overall | 76–97 | ||
| Mandatory labeling (3, 19, 20, 22) | United States, South Korea | Potato chips | 98 |
| Restaurant foods | 80 | ||
| Supermarket foods | 85–95 | ||
| Cookies | 89 | ||
| Spreads (all) | 86 | ||
| Spreads (stick) | 46 | ||
| Spreads (tub or spray) | 99 | ||
| Voluntary TFA limits (18) | Restaurant frying oil | 45 |
Data adapted from reference 11. In Canada, additional requirements include a combined TFAs + SFAs ≤15% of energy. NYC, New York City; TFA, trans fatty acid.
Studies conducted in the United States classify <0.5 g TFAs/serving as TFA-free, whereas other countries classify products with <0.2 g TFAs/serving as TFA-free.
Changes in FA composition with product reformulation.
There is often a concern that if TFAs are removed from a product they will be replaced with SFAs (37), decreasing the potential health benefits of product reformulation. Table 3 synthesizes the evidence related to changes in the FA composition of foods after the implementation of TFA policies. Although all of the studies that reported on the different FAs in products pre– and post–policy interventions found reductions in TFA amounts in foods, there were mixed findings in terms of SFA amounts in foods. Seven studies included information on MUFA and PUFA contents in foods (18–20, 22, 28, 29, 31), 6 of which found increases in either MUFAs or PUFAs (or both). Moreover, 12 studies examined the combined TFA and SFA contents of foods before and after the introduction of a TFA policy, with all but one study (22) reporting a reduction post–policy intervention.
TABLE 3.
Changes in the FA composition of foods after the introduction of a TFA policy1
| Policy intervention | Study (ref) | Country | TFAs | SFAs | MUFAs and/or PUFAs | TFAs + SFAs2 | Total fat |
|---|---|---|---|---|---|---|---|
| Mandatory TFA labeling | Lee et al. (20) | South Korea | ↓ | ↑ Bakery products | ↑ Restaurant food | ↓ | ↓ |
| Mozaffarian et al. (3) | United States | ↓ | ↑ Supermarket foods, | — | ↓ | — | |
| ↓ restaurant foods | |||||||
| Van Camp et al. (22) | United States | ↓ | ↑ Bakery products | ↑ Oils high in PUFAs and MUFAs in chips | NC | NC | |
| Storey and Anderson (21) | United States | ↓ | ↓ | — | ↓ | — | |
| Garsetti et al. (19) | United States | ↓ | ↑ | ↑PUFAs, ↓MUFAs | ↓ | ↓ | |
| Mandatory TFA limits | Angell et al. (33) | NYC, United States | ↓ | ↓ | — | ↓ | — |
| Angell et al. (32) | NYC, United States | ↓ | ↑ | — | ↓ | — | |
| Peymani et al. (14) | Iran | ↓ | ↑ | — | ↓ | — | |
| Mandatory TFA labeling + voluntary limits | Ricciuto et al. (31) | Canada | ↓ | NC | ↑PUFAs, ↓MUFA, | ↓ | ↓ |
| Ratnayake et al. (28) | Canada | ↓ | ↓ | ↑ | ↓ | NC | |
| Ratnayake et al. (29) | Canada | ↓ | ↑ Crackers, cookies, and garlic spreads and donuts | ↑ | ↓ | NC | |
| Voluntary TFA self-regulation | Temme et al. (18) | Netherlands | ↓ | NC | NC (↓ in biscuits) | ↓ | NC |
Data adapted from reference 11. NC, no change; NYC, New York City; ref, reference; TFA, trans fatty acid; ↑, increase; ↓, decrease.
Change in TFA + SFA calculated by adding FAs when the sum was not reported by authors; in these cases, significance was not assessed.
Findings of modeling studies
Eight modeling studies were included in the review (Supplemental Table 2). The majority of the modeling studies were conducted in the United Kingdom (n = 5), whereas other studies were conducted in Argentina, Denmark, and the European Union. Six of these studies (38–43) examined the impact of hypothetical TFA policies and, of these, 3 studies (39–41) examined several food policies simultaneously. In these cases, only results related to the TFA reduction were reported in this review.
Table 4 summarizes the findings of the studies modeling the impact of TFA policies on cardiovascular, equity, and economic outcomes. All of the modeling studies reported a reduction in CHD and CVD deaths attributed to TFA policies. These ranged from 1.3% to 6.35% deaths averted (39–41). Of the modeling studies conducted in the United Kingdom, annual cardiovascular deaths averted with TFA policies ranged from 112 deaths (with a 0.5% reduction in TFAs) (41) averted in 2010 to between 2700 (39) and 3900 (42) deaths averted annually (with a 1% reduction in TFAs) (the specific policy approaches taken to achieve these reductions were not always specified). For the UK modeling studies that examined CVD deaths averted over a longer time horizon, one study found that between 2006 and 2015, 3500–4700 CVD deaths would be averted (40), depending on whether there was a 0.5% or 1% reduction in TFAs, and another found that 7200 deaths would be averted between 2015 and 2020 with a total TFA ban in processed foods when compared with TFA consumption remaining at its current level (38). The modeling studies (n = 4) that included a cost-effectiveness component all reported that TFA policies would lead to net cost savings. However, the European Union model found that a mandatory TFA-labeling policy would not be cost-effective unless initial TFA intakes were quite high (43). For those studies that examined savings per year, health care savings ranged from US$17 million/y (44) to £230 million/y (39). Two studies (38, 42) examined the effects of different TFA policy scenarios on different socioeconomic groups. Both studies were conducted in the United Kingdom and found TFA policies to have a greater effect on lower socioeconomic groups, regardless of type of policy examined (i.e., TFA labeling, ban in restaurants, or total ban in processed foods). The first suggested that a TFA ban would reduce inequality in mortality from CHD by 15%, given the higher TFA intakes among lower socioeconomic groups (38). The second study found that 5 times as many CHD deaths would be prevented in the lowest quintile of socioeconomic status with a 1% reduction in TFA intakes; in addition, they would also gain 6 times as many life-years compared with the most affluent group (42).
TABLE 4.
An overview of the modeling studies included in the systematic review1
| Policy type | Study (ref), country/region | Stroke deaths | CHD/CAD deaths | CVD deaths | CHD/CVD events | DALYs | QALYs/LYs gained | Costs to health system/society | Reduces inequalities in CVD deaths (Y/N) |
|---|---|---|---|---|---|---|---|---|---|
| Modeling of hypothetical policies | |||||||||
| Conservative policy scenario2 | O'Keeffe et al. (41), Republic of Ireland | ↓ | ↓ | — | — | — | — | — | — |
| O'Flaherty et al. (40), United Kingdom | — | — | ↓ | — | — | — | — | — | |
| Pearson-Stuttard et al. (42), England and Wales | — | ↓ | — | — | — | ↑ | ↓ | Y | |
| Voluntary limit on TFA | Martin-Saborido et al. (43), European Union | — | — | — | — | ↓ | — | ↓ | — |
| TFA labeling | Allen et al. (38), England3 | — | — | — | — | — | — | ↓ | Y |
| Martin-Saborido et al. (43), European Union | — | — | — | — | ↓ | — | Not cost-effective | — | |
| Legislative ban | O'Keeffe et al. (41), Republic of Ireland | ↓ | ↓ | — | — | — | — | — | — |
| O'Flaherty et al. (40), United Kingdom | — | — | ↓ | — | — | — | — | — | |
| Barton et al. (39), England and Wales | — | — | ↓ | ↓ | — | ↑ | ↓ | — | |
| Pearson-Stuttard et al. (42), England and Wales | — | ↓ | — | — | — | ↑ | ↓ | Y | |
| Allen et al. (38), England | — | ↓ | — | — | — | — | ↓ | Y | |
| Martin-Saborido et al. (43), European Union | — | — | — | — | ↓ | — | ↓ | — | |
| Modeling of enacted real-world policies | Rubinstein et al. (44), Argentina | — | ↓ | — | ↓ | ↓ | — | ↓ | — |
| Restrepo and Rieger (45), Denmark | — | — | ↓ | — | — | — | — | — |
CAD, coronary artery disease; CHD, coronary heart disease; CVD, cardiovascular disease; DALY, disability-adjusted life-year; LY, life-year; QALY, quality-adjusted life-year; ref, reference; TFA, trans fatty acid; Y, yes; ↑, increase; ↓, decrease.
Article did not provide detailed information about what the policy entails. It solely provided the estimated reduction in TFA intakes.
Modeled policy was improved labeling or TFA limits in restaurants.
Two modeling studies, one in Argentina (44) and another in Denmark (45), modeled the impact of the countries' actual TFA policies, both showing positive impacts in terms of reducing CHD and CVD rates. Over the course of a 10-y period between 2004 and 2014, Argentina went from having a voluntary TFA-labeling policy to having mandatory TFA limits in foods. This study modeled several likely scenarios by linking different assumptions of the likely effect of TFAs on CHD outcomes (e.g., based on individual data on CHD risk factors from a national prospective cohort study compared with the effect of TFAs on CHD blood lipid risk factors from randomized controlled trials) and baseline levels of TFA intake (mean = 1.5% of total energy compared with a lower bound of 1% and an upper bound of 3% of total energy) (44). Across all the scenarios examined in the modeling studies, TFA regulation had a substantial impact, leading to significant reductions in CHD deaths (301–1517) and CHD events (1066–5373), disability-adjusted life-years (5237–26,394) and health-care costs saved (US$17–$87 million) each year (44). In Denmark, a synthetic control group that used CVD mortality data from the Organization for Economic Co-operation and Development countries without TFA policies was used to examine what the CVD mortality rate would have been if the country did not adopt a TFA ban in 2004 (45). They found that CVD mortality decreased by ∼14.2 deaths ⋅ 100,000 persons–1 ⋅ y–1 in Denmark with the TFA policy compared with not having a TFA policy. Supplemental Table 3 provides an overview of the main assumptions of the models included in the review. There were several limitations associated with the assumptions of the various models (e.g., time horizons, current TFA intakes, reductions in TFA due to policy, etc.) that have implications for their overall findings.
Discussion
This study compiles the evidence of the impact of TFA policies on their availability in the food supply, dietary intakes, concentrations in plasma serum and breast milk, as well as changes in burden of disease due to TFAs on the basis of modeling studies. TFA policies coincide with reductions in TFAs in foods as well as intakes. The evidence suggests that, although all of the policy approaches examined in the review will likely lead to reductions in TFA contents in foods and subsequent intakes, stronger policies (e.g., limits or bans) will have more pronounced effects (virtually eliminating TFAs in the food supply) than voluntary (ranging from 20% to 38% reduction in intakes) or labeling approaches (ranging from 30% to 74% reduction in plasma serum and breast-milk concentrations) on reducing TFA contents in the food supply. Moreover, it is likely that they contribute to reductions in heart disease risk and there is some evidence to suggest that TFA bans are cost-saving, as shown in the modeling studies included in this review.
The studies that examined labeling policies found that, although they had coincided with reductions in TFAs in foods, foods high in TFAs remained on the shelves. Given that high-TFA foods tend to be cheaper than their low-TFA counterparts (31, 46), these policy approaches may not deliver for the most disadvantaged segments of the population. Lower-income consumers are generally more sensitive to price differentials and thus more likely to purchase lower-cost, higher-TFA products. Moreover, in countries requiring mandatory labeling of TFA contents in foods, consumers with lower nutrition knowledge and numeracy are less likely to understand or use nutrition labels (47), and thus may continue to purchase products with high amounts of TFAs. This suggests that even in countries where the majority of products are TFA-free—as long as products containing high industrial TFAs remain available—TFA consumption will likely remain a public health problem and contribute to health disparities due to higher consumption by lower socioeconomic groups. In addition, the modeling study examining the impact of different TFA policy approaches in the European Union found that mandatory TFA labeling was unlikely to be cost-effective (43). TFA bans therefore remain the most effective, economical, and equitable approach to reduce TFA consumption.
Although in most countries that have set limits of allowable TFAs in foods the limit has been 2% of total fat (which is often described as a ban), in Iran the TFA limits were set high (initially 20%) and were reduced gradually over time. Additional progress is needed to reduce TFA amounts in edible oils even further in LMIC settings. It is possible that TFA policies in LMICs will need to be adapted to local contexts and perhaps take place alongside additional interventions throughout the food supply chain, given the large informal food sectors in many LMICs (48). For example, in India, it is likely that the mandatory TFA limit of 5% in PHOs, which went into effect in August 2016, will not reach the PHOs produced by small-scale producers in the informal sector (48, 49). Providing incentives for these smaller-scale producers to reformulate their products may be necessary in order to ensure that TFA contents in PHOs are aligned with the policy goal. Additional studies examining the impact of TFA policies in LMICs are needed.
In the past, there have been calls for a global TFA ban (50, 51); however, mandating a global ban would require significant stakeholder buy-in (including from nongovernmental organizations and industry) and is unlikely to be feasible in the short term. However, as more and more countries and regions around the world adopt TFA policies, this buy-in may increase. The US FDA's decision to revoke the GRAS status to PHOs sends a strong message globally. This may facilitate fresh impetus for the Codex Alimentarius to redefine the terms for the use of PHOs. LMICs, in particular, often look to Codex for guidance on issues of food safety and aim to comply with its standards (52). There may be potential for Codex to follow a similar approach to that used by the United States and define PHOs as unsafe for consumption. If Codex were to take these steps, it would essentially act as a pseudo-global ban and prevent TFA regulation from being considered a technical barrier to trade. Although this could be a feasible approach to establishing a global TFA ban, vested interests are strong and the current policy environment (including stakeholder support) may not enable such a measure (53). In the meantime, countries will need to continue to use their own policy tools to improve the quality of fat that is available, affordable, and acceptable in the food supply.
There is often a concern that reducing TFA amounts in foods will lead to increases in SFAs (37). We found mixed evidence of increases in SFAs post–product reformulation to reduce or remove TFAs. It is likely that this will be quite dependent on product category. For example, it may be more difficult to reformulate bakery products with oils higher in MUFAs and PUFAs, given that they are not semi-solid at room temperature; however, fried snack foods can more easily be reformulated with oils high in unsaturated fats. As palm oil, which is high in SFAs, becomes more ubiquitous in the food supply and becomes the preferred substitute for PHOs, it is possible that SFA contents will increase in foods (palm oil is now in ∼50% of all products) (54), arguably an unintended outcome (55). It is likely that incentives for the use of oils higher in MUFAs and PUFAs will be needed, particularly in LMICs (49). Substitution with oils high in unsaturated fats rather than palm oil is likely beneficial to heart health on the basis of metabolic trials and observational studies (55); conversely, there may be less demand for products that are both low in TFAs and SFAs. Therefore, an understanding of consumer sentiment and technical and health impacts of specific fats and oils is paramount in product reformulation to reduce or remove TFAs.
The results of the modeling studies included in this review suggest that it is likely that policies that set TFA limits will be cost-saving and have the greatest impact on lower socioeconomic groups. These are important considerations for policymakers in terms of deciding whether or not to move forward with a TFA policy. These findings suggest that TFA bans make sense from an economic standpoint but also from an ethical perspective, given that they could help to reduce social inequities. Although there is often resistance to implementing regulation pertaining to food, from a public health ethics perspective, regulating TFAs in the food supply is an appropriate policy approach given that the benefits of the policy far outweigh any risk to individual liberties (56).
Limitations of included studies
One of the main limitations of this study is the small number of countries that have had studies examining the impact of their TFA policies. There is a substantial amount of evidence to support TFA labeling in both the United States and Canada but less in countries beyond North America, particularly LMICs. In addition to the evidence compiled from this review, continued country-level monitoring of TFA intakes over time can be used to indirectly assess the impact of different approaches to reducing TFAs. Wanders et al. (8) examined trends in TFA intakes over time and found a reduction in TFA intakes in some European countries (e.g., Sweden, Iceland, Norway) coinciding with the adoption of voluntary TFA reduction measures but not in others (e.g., Spain, United Kingdom, France). These observations suggest that industry reformulated products to reduce TFAs before mandatory measures came into place in some but not all countries. By continuing to monitor trends in intakes over time across a wider range of countries, additional insight into the impact of different approaches to reducing TFAs in the food supply may be possible.
The majority of the studies included in this review were from high-income countries, with limited data from LMICs. Thus, the impact of TFA policies on intakes and cardiovascular outcomes in LMIC settings is less clear. Given that the Global Burden of Diseases estimates indicate that TFA intakes may be higher in many LMICs, particularly North Africa/Middle East and South Asia (5), there is a need for additional research examining the impact of policies in these settings.
There are several limitations to the assumptions used in many of the modeling studies included in the review that need to be considered. The time horizons used for the models were short, with the exception of the article by Martin-Saborido et al. (43). In one study (41), the deaths averted were only examined for 1 y. Longer time horizons would be more appropriate, because the implementation of a TFA policy would not result in instantaneous effects on CVD, the use of a lifetime approach as was used in the model examining the impacts of TFA policies in the European Union (43) would likely be more appropriate. Some of the modeling studies did not address current levels of TFA intake, which may, in part, be explained by limited data availability; however, this has significant implications for the model assumptions. For example, in the United Kingdom, average TFA intakes are already low (0.8% of total energy) (57), so it may not be possible to reduce TFA intake by an additional 1% of total energy intake, as was examined in 3 of the models (39, 41, 42). TFA policies only apply to industrially produced TFAs rather than all TFAs, given the lack of feasibility in terms of implementing a policy that addresses ruminant TFA contents in the food supply. It is therefore unlikely that TFA intakes can be reduced to 0% of total energy intake in the absence of avoiding all ruminant products. Moreover, another area of uncertainty in the models is the assumption that reducing ruminant TFAs would have the same effect on CVD risk as reducing industrially produced TFAs; existing evidence on the cardiovascular effects of ruminant TFA remains mixed and uncertain (38, 41, 42). One of the main strengths of the European Union model is that it focused on reductions in industrially produced TFA contents in food, rather than total TFAs (including ruminants), and it assessed 3 additional initial TFA amounts in the sensitivity analyses, thus giving a better indication of the potential costs and benefits of the different policy options examined.
Limitations in study design are not limited to modeling studies. The majority of the “real world” studies included were weak. However, it is important to note that these studies examined real policies that have been implemented in a number of countries and that the use of more rigorous study designs, such as randomized controlled trials, to examine these policies in a “real world” context is not possible. We only included studies with pre– and post–TFA policy implementation data to ensure that we included higher-quality studies; however, these studies still have limitations. Despite these limitations, the totality of the evidence from both modeling studies as well as the studies conducted in “real world” settings suggest that stronger TFA policies will have a larger impact on TFA contents in foods, their intake, and CVD outcomes.
Conclusions
Policies aimed at reducing TFAs in the food supply are effective and will likely reduce the burden of diet-related disease, particularly among the most vulnerable socioeconomic groups. Although only a handful of countries have adopted strict TFA limits or bans; these policies have dramatically reduced TFA amounts in the food supply. Labeling policies have also led to reductions in the availability of TFAs in the food supply; however, these reductions have not been made across all product categories and high-TFA products remain in the food supply. Moving forward, global, regional, or country-level TFA bans should be adopted. TFA bans are likely the most effective, economical, and equitable policy approach to reducing TFAs in the food supply.
Additional studies need to be conducted to examine the impact of TFA policies in LMIC contexts. LMICs may require additional incentives and interventions alongside mandatory limits in order to reduce TFA contents in all foods in the food supply, including those manufactured by the informal sector. Last, continued monitoring to ensure progress in terms of reducing TFA contents in the food supply over time will be necessary.
Supplementary Material
Acknowledgments
The authors' responsibilities were as follows—JHYW, LV, and SMD: obtained funding; SMD and JHYW: designed the research; SMD and MZB: reviewed articles and extracted data; SMD: drafted the manuscript; and all authors: had input into the data interpretation and read and approved the final manuscript.
Abbreviations
- CHD
coronary heart disease
- CVD
cardiovascular disease
- EPHPP
Effective Public Health Practice Project
- LMIC
low- and middle-income country
- MI
myocardial infarction
- PHO
partially hydrogenated oil
- TFA
trans fatty acid
References
- 1. Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC.. Trans fatty acids and cardiovascular disease. N Engl J Med 2006;354:1601–13. [DOI] [PubMed] [Google Scholar]
- 2. Teegala SM, Willett WC, Mozaffarian D.. Consumption and health effects of trans fatty acids: a review. J AOAC Int 2009;92:1250–7. [PubMed] [Google Scholar]
- 3. Mozaffarian D, Jacobson MF, Greenstein JS.. Food reformulations to reduce trans fatty acids. N Engl J Med 2010;362:2037–9. [DOI] [PubMed] [Google Scholar]
- 4. World Economic Forum; WHO. From burden to “best buys”: reducing the economic impact of non-communicable diseases in low- and middle-income countries. Geneva (Switzerland): World Economic Forum; 2011. [Google Scholar]
- 5. Micha R, Khatibzadeh S, Shi P, Fahimi S, Lim S, Andrews KG, Engell RE, Powles J, Ezzati M, Mozaffarian D Global Burden of Diseases Nutrition and Chronic Diseases Expert Group NutriCoDE . Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys. BMJ 2014;348:g2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nishida C, Uauy R.. WHO scientific ipdate on health consequences of trans fatty acids: introduction. Eur J Clin Nutr 2009;63(Suppl 2):S1–4. [DOI] [PubMed] [Google Scholar]
- 7. Honors MA, Harnack LJ, Zhou X, Steffen LM.. Trends in fatty acid intake of adults in the Minneapolis-St Paul, MN metropolitan area, 1980-1982 through 2007-2009. J Am Heart Assoc 2014;3:e001023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wanders AJ, Zock PL, Brouwer IA.. Trans fat intake and its dietary sources in general populations worldwide: a systematic review. Nutrients 2017;9:E840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. FDA. Final determination regarding partially hydrogenated oils. Washington (DC): FDA; 2015. [Google Scholar]
- 10. European Commission. Initiative to limit industrial trans fats intakes in the EU. Brussels (Belgium): European Commission; 2016. [Google Scholar]
- 11. Downs SM, Thow AM, Leeder SR.. The effectiveness of policies for reducing dietary trans fat: a systematic review of the evidence. Bull World Health Organ 2013;91:262–9H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Effective Public Health Practice Project. Quality assessment tool for quantitative studies dictionary [Internet]. [cited 2016 Mar 25]. Available from: http://www.ephpp.ca/PDF/QADictionary_dec2009.pdf.
- 13. Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG.. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract 2012;18:12–8. [DOI] [PubMed] [Google Scholar]
- 14. Peymani P, Joulaie H, Zamiri N, Ahmadi SM, Dinarvand R, Hosseini H, Hamedani MP, Kamran B.. Iran's experience on reduction of trans-fatty acid content in edible oils. Middle East J Sci Res 2012;11:1207–11. [Google Scholar]
- 15. Colón-Ramos U, Baylin A, Campos H.. The relation between trans fatty acid levels and increased risk of myocardial infarction does not hold at lower levels of trans fatty acids in the Costa Rican food supply. J Nutr 2006;136:2887–92. [DOI] [PubMed] [Google Scholar]
- 16. Monge-Rojas R, Aragón MC, Chinnock A, Campos H, Colón-Ramos U.. Changes in dietary intake and food sources of saturated and cis and trans unsaturated fatty acids in Costa Rican adolescents: 1996 versus 2006. Nutrition 2013;29:641–5. [DOI] [PubMed] [Google Scholar]
- 17. Monge-Rojas R, Colón-Ramos U, Jacoby E, Mozaffarian D.. Voluntary reduction of trans-fatty acids in Latin America and the Caribbean: current situation. Am J Public Health 2011;29:126–9. [DOI] [PubMed] [Google Scholar]
- 18. Temme EH, Millenaar IL, Van Donkersgoed G, Westenbrink S.. Impact of fatty acid food reformulations on intake of Dutch young adults. Acta Cardiol 2011;66:721–8. [DOI] [PubMed] [Google Scholar]
- 19. Garsetti M, Balentine DA, Zock PL, Blom WA, Wanders AJ.. Fat composition of vegetable oil spreads and margarines in the USA in 2013: a national marketplace analysis. Int J Food Sci Nutr 2016;67:372–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lee JH, Adhikari P, Kim SA, Yoon T, Kim IH, Lee KT.. Trans fatty acids content and fatty acid profiles in the selected food products from Korea between 2005 and 2008. J Food Sci 2010;75:C647–52. [DOI] [PubMed] [Google Scholar]
- 21. Storey ML, Anderson PA.. Changes in mean intake of fatty acids and intake of saturated and trans fats from potatoes: NHANES 2005–2006, 2007–2008, and 2009–2010. Adv Nutr 2015;6:376S–82S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Van Camp D, Hooker NH, Lin C-TJ.. Changes in fat contents of US snack foods in response to mandatory trans fat labelling. Public Health Nutr 2012;15:1130–7. [DOI] [PubMed] [Google Scholar]
- 23. Vesper HW, Caudill SP, Kuiper HC, Yang Q, Ahluwalia N, Lacher DA, Pirkle JL.. Plasma trans-fatty acid concentrations in fasting adults declined from NHANES 1999–2000 to 2009–2010. Am J Clin Nutr 2017;105:1063–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vesper HW, Kuiper HC, Mirel LB, Johnson CL, Pirkle JL.. Levels of plasma trans-fatty acids in non-Hispanic white adults in the United States in 2000 and 2009. JAMA 2012;307:562–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yang Q, Zhang Z, Loustalot F, Vesper H, Caudill SP, Ritchey M, Gillespie C, Merritt R, Hong Y, Bowman BA.. Plasma trans-fatty acid concentrations continue to be associated with serum lipid and lipoprotein concentrations among US adults after reductions in trans-fatty acid intake. J Nutr 2017;147:896–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Arcand J, Scourboutakos MJ, Au JT, L'Abbe MR.. trans Fatty acids in the Canadian food supply: an updated analysis. Am J Clin Nutr 2014;100:1116–23. [DOI] [PubMed] [Google Scholar]
- 27. Friesen R, Innis SM.. Trans fatty acids in human milk in Canada declined with the introduction of trans fat food labeling. J Nutr 2006;136:2558–61. [DOI] [PubMed] [Google Scholar]
- 28. Ratnayake WM, L'Abbe MR, Farnworth S, Dumais L, Gagnon C, Lampi B, Casey V, Mohottalage D, Rondeau I, Underhill L, et al. . Trans fatty acids: current contents in Canadian foods and estimated intake levels for the Canadian population. J AOAC Int 2009;92:1258–76. [PubMed] [Google Scholar]
- 29. Ratnayake WMN, L'Abbe MR, Mozaffarian D.. Nationwide product reformulations to reduce trans fatty acids in Canada: when trans fat goes out, what goes in? Eur J Clin Nutr 2009;63:808–11. [DOI] [PubMed] [Google Scholar]
- 30. Ratnayake WMN, Swist E, Zoka R, Gagnon C, Lillycrop W, Pantazapoulos P.. Mandatory trans fat labeling regulations and nationwide product reformulations to reduce trans fatty acid content in foods contributed to lowered concentrations of trans fat in Canadian women's breast milk samples collected in 2009–2011. Am J Clin Nutr 2014;100:1036–40. [DOI] [PubMed] [Google Scholar]
- 31. Ricciuto L, Lin K, Tarasuk V.. A comparison of the fat composition and prices of margarines between 2002 and 2006, when new Canadian labelling regulations came into effect. Public Health Nutr 2009;12:1270–5. [DOI] [PubMed] [Google Scholar]
- 32. Angell SY, Cobb LK, Curtis CJ, Konty KJ, Silver LD.. Change in trans fatty acid content of fast-food purchases associated with New York City's restaurant regulation: a pre-post study. Ann Intern Med 2012;157:81–6. [DOI] [PubMed] [Google Scholar]
- 33. Angell SY, Silver LD, Goldstein GP, Johnson CM, Deitcher DR, Frieden TR, Bassett MT.. Cholesterol control beyond the clinic: New York City's trans fat restriction. Ann Intern Med 2009;151:129–34. [DOI] [PubMed] [Google Scholar]
- 34. Brandt EJ, Myerson R, Perraillon MC, Polonsky T.. Abstract 17878: hospital admission rates for myocardial infarction and stroke in New York City before and after the ban on trans fatty acids. Circulation 2015;132:A17878. [Google Scholar]
- 35. Restrepo BJ, Rieger M.. Trans fat and cardiovascular disease mortality: evidence from bans in restaurants in New York. J Health Econ 2016;45:176–96. [DOI] [PubMed] [Google Scholar]
- 36. Leth T, Jensen HG, Mikkelsen AA, Bysted A.. The effect of the regulation on trans fatty acid content in Danish food. Atheroscler Suppl 2006;7:53–6. [DOI] [PubMed] [Google Scholar]
- 37. Unnevehr LJ, Jagmanaite E.. Getting rid of trans fats in the US diet: policies, incentives and progress. Food Policy 2008;33:497–503. [Google Scholar]
- 38. Allen K, Pearson-Stuttard J, Hooton W, Diggle P, Capewell S, O'Flaherty M.. Potential of trans fats policies to reduce socioeconomic inequalities in mortality from coronary heart disease in England: cost effectiveness modelling study. BMJ 2015;351:h4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Barton P, Andronis L, Briggs A, McPherson K, Capewell S.. Effectiveness and cost effectiveness of cardiovascular disease prevention in whole populations: modelling study. BMJ 2011;343:d4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. O'Flaherty M, Flores-Mateo G, Nnoaham K, Lloyd-Williams F, Capewell S.. Potential cardiovascular mortality reductions with stricter food policies in the United Kingdom of Great Britain and Northern Ireland. Bull World Health Organ 2012;90:522–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. O'Keeffe C, Kabir Z, O'Flaherty M, Walton J, Capewell S, Perry IJ.. Modelling the impact of specific food policy options on coronary heart disease and stroke dea ths in Ireland. BMJ Open 2013;3:e002837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pearson-Stuttard J, Critchley J, Capewell S, O'Flaherty M.. Quantifying the socio-economic benefits of reducing industrial dietary trans fats: modelling study. PLoS One 2015;10:e0132524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Martin-Saborido C, Mouratidou T, Livaniou A, Caldeira S, Wollgast J.. Public health economic evaluation of different European Union-level policy options aimed at reducing population dietary trans fat intake. Am J Clin Nutr 2016;104:1218–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rubinstein A, Elorriaga N, Garay OU, Poggio R, Caporale J, Matta MG, Augustovski F, Pichon-Riviere A, Mozaffarian D.. Eliminating artificial trans fatty acids in Argentina: estimated effects on the burden of coronary heart disease and costs. Bull World Health Organ 2015;93:614–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Restrepo BJ, Rieger M.. Denmark's policy on artificial trans fat and cardiovascular disease. Am J Prev Med 2016;50:69–76. [DOI] [PubMed] [Google Scholar]
- 46. Silveira BM, Kliemann N, Silva DP, Colussi CF, Proença RP.. Availability and price of food products with and without trans fatty acids in food stores around elementary schools in low- and medium-income neighborhoods. Ecol Food Nutr 2013;52:63–75. [DOI] [PubMed] [Google Scholar]
- 47. Hess R, Visschers VH, Siegrist M.. The role of health-related, motivational and sociodemographic aspects in predicting food label use: a comprehensive study. Public Health Nutr 2012;15:407–14. [DOI] [PubMed] [Google Scholar]
- 48. Downs SM, Singh A, Gupta V, Lock K, Ghosh-Jerath S.. The need for multisectoral food chain approaches to reduce trans fat consumption in India. BMC Public Health 2015;15:693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Downs SM, Gupta V, Ghosh-Jerath S, Lock K, Thow AM, Singh A.. Reformulating partially hydrogenated vegetable oils to maximise health gains in India: is it feasible and will it meet consumer demand? BMC Public Health 2013;13:1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Coombes R.. Trans fats: chasing a global ban. BMJ 2011;343:d5567. [DOI] [PubMed] [Google Scholar]
- 51. Kraak V, Colón-Ramos U,Monge-Rojas R.. The case for a global ban. World Nutr 2012;3:570–91. [Google Scholar]
- 52. Downs SM, Thow AM, Ghosh-Jerath S, McNab J, Reddy KS, Leeder SR.. From Denmark to Delhi: the multisectoral challenge of regulating trans fats in India. Public Health Nutr 2013;16:2273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, Lincoln P, Casswell S; Lancet NCD Action Group . Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013;381:670–9. [DOI] [PubMed] [Google Scholar]
- 54. Euromonitor International. Palm oil to create winners and losers in packaged food. London: Euromonitor International; 2014. .
- 55. Sun Y, Neelakantan N, Wu Y, Lote-Oke R, Pan A, van Dam RM.. Palm oil consumption increases LDL cholesterol compared with vegetable oils low in saturated fat in a meta-analysis of clinical trials. J Nutr 2015;145:1549–58. [DOI] [PubMed] [Google Scholar]
- 56. Kass NE.. An ethics framework for public health. Am J Public Health 2001;91:1776–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pot GK, Prynne CJ, Roberts C, Olson A, Nicholson SK, Whitton C, Teucher B, Bates B, Henderson H, Pigott S, et al. . National Diet and Nutrition Survey: fat and fatty acid intake from the first year of the rolling programme and comparison with previous surveys. Br J Nutr 2012;107:405–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.