Abstract
Objective
To describe and compare the scope of practice (SoP) of GPs and FPs between the rural northern, rural southern, urban northern, and urban southern regions of Ontario.
Design
Cross-sectional retrospective analysis of the 2013 College of Physicians and Surgeons of Ontario official register and annual membership renewal survey data.
Setting
Ontario.
Participants
All independently practising GPs and FPs with a primary practice address in Ontario.
Main outcome measures
For each of the 4 regions, we determined the distribution of GPs and FPs, the mean number of hours worked per week, the mean number of clinical activities reported, the proportion of GPs and FPs reporting specific clinical activities, and the proportion of time dedicated to each activity.
Results
The rural north has 2.4% of the province’s GPs and FPs, who on average report working more hours per week (a total of 50.82 hours a week) than practitioners in all other regions do. Rural northern and rural southern GPs and FPs report participating in more types of clinical activities than their urban counterparts do. The types of clinical activities reported vary across regions. For example, 13.3% of GPs and FPs in the urban south reported that emergency medicine was an aspect of their clinical activities, compared with 57.5% in the rural north. Urban GPs and FPs engage in fewer clinical activities and thus spend proportionately more time on each clinical activity than rural GPs and FPs do, indicating that clinical practice concentration and narrower SoP is more common in urban practices.
Conclusion
The SoP for GPs and FPs is not uniform across Ontario. Rural physicians work more hours and engage in a broader spectrum of clinical activities. Clinical activity variation was found across all practice locations, indicating that SoP is driven by patient and community needs, which vary from region to region. Our findings are relevant for rural and northern policy and program development in medical education, continuing professional development, and physician recruitment and retention.
Résumé
Objectif
Décrire et comparer les champs de pratique (CdP) des OP et des MF selon qu’ils travaillent dans des régions rurales du nord ou du sud de l’Ontario, ou dans des régions urbaines du nord ou du sud de cette province.
Type d’étude
Une analyse rétrospective transversale de l’édition 2013 du registre officiel du Collège des médecins et des chirurgiens de l’Ontario et les données de l’enquête sur le renouvellement annuel de ses membres.
Contexte
L’Ontario.
Participants
Tous les OP et les MF pratiquant en solo dont l’adresse principale de travail était en Ontario.
Principaux paramètres à l’étude
On a déterminé la distribution des OP et des MF dans les 4 régions, le nombre moyen d’heures travaillées par semaine, le nombre moyen d’activités cliniques déclarées, la proportion d’OP et de MF mentionnant des activités cliniques spécifiques et la proportion de temps consacrée à chaque activité.
Résultats
La région rurale du nord regroupe 2,4 % des OP et des MF de la province; les médecins de cette région disent travailler un nombre moyen d’heures par semaine plus élevé (un total de 50,82 heures) que les médecins de toutes les autres régions. Les OP et les MF des régions rurales du nord et du sud disent effectuer une plus grande variété d’activités cliniques que leurs confrères urbains. Les types d’activités cliniques mentionnés varient selon les régions. Par exemple, 13,3 % des OP et des MF de la région urbaine du sud déclarent que la médecine d’urgence fait partie de leurs activités cliniques, par rapport à 57,5 % de ceux de la région rurale du nord. Les OP et les MF urbains effectuent moins d’activités cliniques que leurs confrères ruraux et consacrent donc plus de temps à chaque activité que leurs confrères ruraux, ce qui indique qu’une certaine réduction de la pratique et du CdP est plus fréquente en milieu urbain.
Conclusion
Le CdP des OP et des MF n’est pas identique dans les différentes régions de l’Ontario. Les médecins ruraux travaillent plus d’heures et effectuent une plus grande variété d’activités cliniques. On a observé des différences régionales dans les activités un peu partout, ce qui suggère que le CdP des médecins dépend des besoins des patients et de la communauté, un facteur qui varie d’une région à l’autre. Nos observations devraient servir à élaborer des politiques et des programmes de formation médicale axés sur la médecine rurale et sur les régions du nord, sur la formation médicale continue, et sur le recrutement et la rétention des médecins.
To truly understand a physician’s scope of practice (SoP) or “what a physician does,” consideration must be given not only to his or her training and certifications, but also to the mix of clinical practice activities and the environments in which he or she works.1–4 Rural GPs and FPs often provide care that might be considered to be outside the SoP for GPs and FPs in urban areas, as they are required to develop broad competencies in response to population needs.5–16 Researchers have endeavoured to create SoP scales that describe the comprehensiveness of an individual physician’s practice,17 and several descriptive reports9,18,19 have examined physician services in rural and northern Ontario; however, no research to date has been undertaken with the explicit purpose of evaluating differences in SoP between the rural north and other regions of the province. Examining scopes of practice in Ontario’s rural and northern areas is essential for ensuring competence and patient safety. It is important that physicians contemplating practising in the rural north have the skills, knowledge, and attitudes required to provide high-quality care in this unique practice setting.20–24 Additionally, understanding rural northern practice will enable educators and policy makers to better support physicians and retain them in communities in these locations.25–28 The objective of our study was to describe and compare the SoP of GPs and FPs between urban and rural and northern and southern regions across Ontario.
METHODS
This study is a cross-sectional retrospective secondary analysis of the 2013 data from the College of Physicians and Surgeons of Ontario (CPSO) official register and annual membership renewal survey. The CPSO is the medical regulatory authority and licensing body for all physicians in the province. The official register contains verified demographic information (eg, sex, date of birth, practice location) and credentialing information (eg, undergraduate and postgraduate medical education and specialty certification). Information regarding physician primary practice location and certification for our study was obtained from the official register. Our study focused on the full population of GPs and FPs with a primary practice address in Ontario. Family physicians are defined as individuals who are certified by the College of Family Physicians of Canada (CFPC), whereas general practitioners are defined as physicians who are certified neither by the CFPC nor by the Royal College of Physicians and Surgeons of Canada.
As part of their annual licensing renewal process, the CPSO distributes a comprehensive survey to its membership. The survey contains questions regarding contact information (eg, all practice addresses), regulatory information (eg, registration in other jurisdictions), continuing professional development activities, and a practice description (eg, work hours and clinical practice activities).
The total number of hours worked in a typical week was extracted from the survey in order to establish a sense of the typical workload of GPs and FPs in each region. Additionally, to examine clinical practice activities in each location, we specifically focused on the following survey question:
Describe your clinical practice and estimate the percentage of time you spend in each area. Percentage should reflect your actual practice (ie: what you do) rather than the certification(s) that you may hold. Total percentage of time spent in practice must add up to 100%.
Physicians were able to select multiple clinical activities from an extensive list and enter the corresponding percentage of time they spent engaged in the activity. Both the clinical activity and the proportion of time spent engaging in each clinical activity were extracted from the survey results to enable us to build a picture of the overall mix of clinical activities performed and the proportion of typical work hours dedicated to each activity per region.
All data were extracted by the CPSO and anonymized before their release to our research team for analysis. Data were shared under a formal data-sharing agreement between the CPSO and Laurentian University in Sudbury, Ont, and ethical approval for this study was provided by the Laurentian University Research Ethics Board.
Defining regions
There are multiple ways to define rural and northern. We linked primary practice address 6-character postal codes to Canadian census geographic areas (census subdivisions) using Statistics Canada Postal Code Conversion Files.29 Practices located in census metropolitan areas with populations of at least 100 000, and those located in census agglomerations with populations of at least 10 000, were considered urban. Primary practices located outside of census metropolitan areas and census agglomerations were classified as rural. A primary practice location was considered northern if it was situated within the boundaries of the North East Local Health Integration Network or the North West Local Health Integration Network.30 This definition of northern was selected because the Local Health Integration Networks are primarily responsible for the planning, funding allocation, and integration of local health care services in Ontario. Thus, our selection of geographic definitions has relevance on a meaningful policy-making level.
Analysis
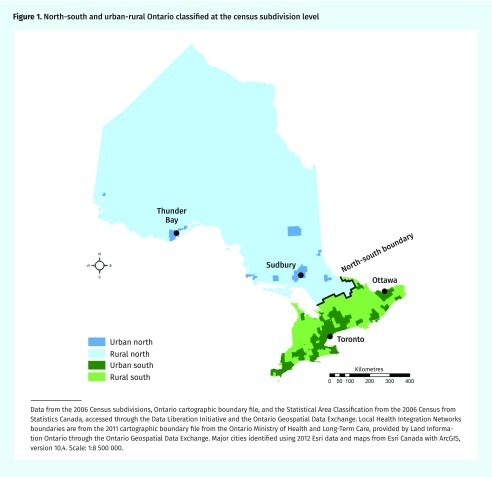
We compared GPs and FPs with primary practice addresses in the rural north, rural south, urban north, and urban south (Figure 1). For each region, we calculated the mean total hours worked per week, the mean number of activities reported, the proportion of physicians reporting specific activities, and the proportion of overall time dedicated to each of those activities. To provide a closer look at physicians who focus their practices on family practice activities, we additionally repeated the analysis exclusively with the data of those GPs and FPs who reported spending 50% or more of their time in general and family practice clinical activities (referred to henceforth as the 50%-plus subpopulation). By examining the time spent per activity and how frequently an activity was reported as part of practice within a region, we were able to get a more nuanced representation of the complexity and breadth of work hours in each location. For example, providing only the proportion of time spent per activity does not indicate how many physicians engage in those activities in a region.
Figure 1.
North-south and urban-rural Ontario classified at the census subdivision level
Data from the 2006 Census subdivisions, Ontario cartographic boundary file, and the Statistical Area Classification from the 2006 Census from Statistics Canada, accessed through the Data Liberation Initiative and the Ontario Geospatial Data Exchange. Local Health Integration Networks boundaries are from the 2011 cartographic boundary file from the Ontario Ministry of Health and Long-Term Care, provided by Land Information Ontario through the Ontario Geospatial Data Exchange. Major cities identified using 2012 Esri data and maps from Esri Canada with ArcGIS, version 10.4. Scale: 1:8 500 000.
Given that our analysis includes the full population of GPs and FPs practising in Ontario, inferential statistics for comparisons were unnecessary.
RESULTS
By far most physicians are located in urban areas (90.7%), with the smallest proportion of Ontario GPs and FPs located in the rural north (2.4%) (Table 1). The mean hours worked per week were highest in the rural north at 50.82 hours a week and lowest in the urban south at 38.56 hours a week across all settings. Rural GPs and FPs consistently reported participating in more clinical activities than their urban counterparts did. In the rural north and rural south, 74.7% and 64.9% of physicians, respectively, reported engaging in more than 1 clinical activity compared with 54.0% in the urban north and 40.5% in the urban south. The opposite trend was found regarding the proportion of professional time spent per clinical activity. Urban GPs and FPs spend a higher percentage of their time per clinical activity than rural physicians do, indicating that clinical practice concentration and narrower SoP are more common in urban practices.
Table 1.
Geographic distribution, work hours, numbers of clinical activities, and time per clinical activity of Ontario GPs and FPs: N = 12 273.
| CHARACTERISTIC | RURAL NORTH | RURAL SOUTH | URBAN NORTH | URBAN SOUTH |
|---|---|---|---|---|
| Total no. of GPs and FPs per region (proportion of all GPs and FPs in Ontario) | 292 (2.4) | 845 (6.9) | 554 (4.5) | 10 582 (86.2) |
| Mean hours worked per week reported per GP or FP | 50.82 | 44.14 | 41.56 | 38.56 |
| Mean proportion of time per clinical activity, % | 51.4 | 59.2 | 67.2 | 76.1 |
| Mean no. of clinical activities reported per GP or FP | 2.70 | 2.34 | 2.00 | 1.66 |
| GPs and FPs reporting only 1 clinical activity, n (%) | 74 (25.3) | 297 (35.1) | 255 (46.0) | 6295 (59.5) |
| GPs and FPs reporting 2–5 clinical activities, n (%) | 202 (69.2) | 508 (60.1) | 291 (52.5) | 4187 (39.6) |
| GPs and FPs reporting ≥ 6 clinical activities, n (%) | 16 (5.5) | 40 (4.7) | 8 (1.4) | 100 (0.9) |
| GPs and FPs reporting 50% or more of their clinical time in general or family practice, n (%) | 194 (66.4) | 577 (68.3) | 302 (54.5) | 5368 (50.7) |
The types of clinical activities and the proportion of physicians participating in each activity vary from location to location (Table 2). For example, although general or family practice was, not surprisingly, reported as the most common clinical activity across all settings, only 56.8% of GPs and FPs in the urban south reported general or family practice as an aspect of their clinical activities in contrast to 85.3% in the rural north. Almost 60% of rural northern GPs and FPs report emergency medicine as part of their practices, whereas only 13.3% do so in the urban south. More northern physicians report engaging in teaching activities than do their southern counterparts. Very few GPs and FPs in the south reported including obstetrics with labour and delivery in their practices, whereas 13.0% of rural northern physicians reported this clinical activity. Last, general or family practice with no hospital privileges was reported by 22.8% of urban southern physicians versus only 4.5% of rural northern physicians.
Table 2.
Proportion of GPs and FPs reporting specific clinical activities and mean proportion of practice time spent in that clinical activity per region: N = 12 273.
| CLINICAL ACTIVITY | RURAL NORTH | RURAL SOUTH | URBAN NORTH | URBAN SOUTH | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| GPS AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | GPS AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | GPS AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | GP AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | |
| General or family practice | 85.3 (1) | 66.6 | 77.5 (1) | 74.6 | 67.1 (1) | 75.5 | 56.8 (1) | 83.4 |
| Emergency medicine | 57.5 (2) | 33.4 | 40.1 (2) | 38.9 | 25.6 (2) | 61.5 | 13.3 (3) | 64.1 |
| Hospitalist medicine | 21.2 (3) | 22.6 | 13.0 (3) | 14.2 | 10.3 (4) | 33.4 | 5.8 (5) | 46.4 |
| Teaching | 13.7 (4) | 8.2 | 7.3 (8) | 6.8 | 14.4 (3) | 9.3 | 6.5 (4) | 12.6 |
| Obstetrics with labour and delivery | 13.0 (5) | 14.4 | 6.8 (10) | 13.1 | 4.9 (8) | 14.7 | 2.7 (*) | 16.7 |
| Long-term care | 11.0 (6) | 14.6 | 12.8 (4) | 16.4 | 4.3 (10) | 25.5 | 4.4 (7) | 27.5 |
| Anesthesia | 7.2 (7) | 41.4 | 8.8 (6) | 43.8 | 4.5 (*) | 60.5 | 1.2 (*) | 69.2 |
| Administrative medicine | 6.9 (8) | 10.5 | 5.6 (*) | 12.2 | 6.7 (7) | 26.0 | 4.5 (6) | 34.0 |
| Coroner | 6.5 (9) | 10.0 | 4.0 (*) | 14.4 | 2.7 (*) | 11.0 | 1.0 (*) | 18.3 |
| Housecalls | 5.5 (10) | 3.0 | 7.5 (7) | 6.4 | 2.4 (*) | 4.3 | 3.0 (*) | 7.2 |
| Surgical assist | 5.1 (*) | 20.5 | 6.6 (9) | 15.2 | 7.2 (6) | 27.3 | 3.8 (9) | 41.4 |
| General or family practice without hospital privileges | 4.5 (*) | 82.9 | 9.9 (5) | 83.1 | 8.3 (5) | 87.6 | 22.8 (2) | 88.0 |
| Palliative care | 3.4 (*) | 4.2 | 5.4 (*) | 8.6 | 4.5 (9) | 26.8 | 3.4 (10) | 42.1 |
| Walk-in clinic or episodic care | 2.1 (*) | 5.5 | 2.4 (*) | 12.6 | 4.3 (10) | 19.8 | 4.1 (8) | 34.4 |
| Psychotherapy | 0.0 (*) | NA | 1.5 (*) | 69.2 | 1.3 (*) | 41.3 | 3.4 (10) | 64.4 |
NA—not applicable.
Denotes that the ranking was not in the top 10 most commonly reported clinical activities by physicians in that location.
For every activity listed, urban southern physicians spend proportionately more time per clinical activity reported and fewer physicians engage in more than 1 clinical activity. This trend was fairly consistent across locations with a gradient moving from urban south to urban north, rural south, and rural north across most clinical activities reported (Table 2).
More rural GPs and FPs spend more than 50% of their clinical time in general or family practice activities than urban GPs and FPs do (Table 1). Only 50.7% of GPs and FPs in the urban south and 54.5% in the urban north are in the 50%-plus subpopulation compared with 66.4% and 68.3% in the rural north and rural south, respectively. When we focus on the clinical activities of the 50%-plus subpopulation (Table 3), we see a shift in some of the rankings for the proportion of GPs and FPs participating in certain activities (eg, in the 50%-plus subpopulation, urban south GPs and FPs report housecalls and obstetrics with labour and delivery more frequently, whereas general or family practice without hospital privileges is reported far less). Additionally, as one might expect, there is an across-the-board decrease in the proportion of GPs and FPs reporting other practice activities and the proportion of time spent on those activities when they are dedicating 50% or more of their time to general or family practice activities. However, it is important to note that, with a few exceptions, the relative differences between regions found in the full GP and FP population for the proportion of GPs and FPs engaging in specific clinical activities are also evident even in this more homogeneous 50%-plus subpopulation. Where the 50%-plus subpopulation noticeably differs from the full population is in the mean percent of time spent per activity.
Table 3.
Clinical activities and mean proportion of practice time spent in that clinical activity per location for GPs and FPs who report spending 50% or more of their overall clinical time in general or family practice: n = 6441.
| CLINICAL ACTIVITY | RURAL NORTH | RURAL SOUTH | URBAN NORTH | URBAN SOUTH | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| GPS AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | GPS AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | GP AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | GPS AND FPS REPORTING ACTIVITY, % (RANK) | MEAN TIME SPENT PER ACTIVITY, % | |
| General or family practice | 100.0 (1) | 76.8 | 100.0 (1) | 81.0 | 100.0 (1) | 88.0 | 100.0 (1) | 90.8 |
| Emergency medicine | 53.6 (2) | 25.7 | 35.7 (2) | 23.6 | 12.3 (2) | 20.4 | 6.6 (3) | 23.4 |
| Hospitalist medicine | 16.0 (3) | 14.7 | 12.7 (4)− | 11.6 | 8.9 (4) | 14.2 | 4.5 (5) | 17.7 |
| Teaching | 11.3 (5)− | 7.6 | 9.0 (5)+ | 6.6 | 14.6 (3) | 8.7 | 7.1 (2)+ | 12.2 |
| Obstetrics with labour and delivery | 12.4 (4)+ | 11.1 | 8.5 (6)+ | 11.8 | 7.0 (5)+ | 14.3 | 4.3 (6)+ | 14.3 |
| Long-term care | 11.3 (5)+ | 8.7 | 14.6 (3)+ | 12.1 | 4.0 (8)+ | 13.1 | 5.1 (4)+ | 17.0 |
| Anesthesia | 4.6 (9)− | 23.9 | 5.7 (9)− | 29.1 | 1.7 (*) | 21.6 | 0.3 (*) | 32.9 |
| Administrative medicine | 5.2 (8) | 6.9 | 4.9 (10)+ | 10.2 | 4.6 (7) | 14.6 | 2.9 (9)− | 16.4 |
| Coroner | 6.2 (6)+ | 4.9 | 3.8 (*) | 6.0 | 2.6 (*) | 10.1 | 1.1 (*) | 9.8 |
| Housecalls | 5.7 (7)+ | 2.3 | 9.0 (5)+ | 3.4 | 3.0 (10)+ | 4.3 | 3.6 (7)+ | 4.3 |
| Surgical assist | 2.1 (*) | 4.0 | 7.3 (7)+ | 7.2 | 6.3 (6) | 10.6 | 3.2 (8)+ | 14.6 |
| General or family practice without hospital privileges | 0.0 (*) | 0.0 | 0.0 (*)− | 0.0 | 0.0 (*)− | 0.0 | 0.1 (*)− | 15.0 |
| Palliative care | 3.6 (10)+ | 3.7 | 6.1 (8)+ | 8.8 | 3.6 (9) | 14.0 | 2.8 (10) | 12.7 |
| Walk-in clinic or episodic care | 0.5 (*) | 3.0 | 2.3 (*) | 10.1 | 4.0 (8)+ | 8.8 | 2.5 (*)− | 15.4 |
| Psychotherapy | 0.0 (*) | 0.0 | 0.3 (*) | 27.5 | 0.3 (*) | 2.0 | 0.9 (*)− | 22.0 |
Denotes that the ranking was not in the top 10 most commonly reported clinical activities by physicians in that location. A + or − symbol denotes an increase or decrease, respectively, in ranking from the full GP and FP population in Table 2.
Although the proportion of time spent per activities is lower for most activities in the subpopulation compared with the full population, the vast differences that were found between locations in the full population are no longer seen in the 50%-plus subpopulation. For example, in the full population rural northern GPs and FPs spent on average 33.4% of their time practising emergency medicine compared with southern urban GPs and FPs, who spend 64.1% of their time on this activity (Table 2). However, in the 50%-plus subpopulation, emergency medicine occupied 25.7% and 23.4% of GP and FP time in the rural north and urban south, respectively (Table 3). Similar narrowing of geographic differences is also seen in the proportion of time spent in anesthesia, surgical assists, and palliative care, where the 50%-plus subpopulation physicians spend their time more similarly to one another (Table 3). Although geographic differences still exist in this subpopulation, these differences are more about who does what, rather than about how much time they spend doing it.
DISCUSSION
As expected, we found that rural physicians, particularly those in the north, engaged in a wider variety of clinical activities, spent less time per activity, and worked more hours per week than physicians in all other regions of the province did. Additionally, the proportion of rural GPs and FPs who concentrate more than half of their clinical time in general or family practice activities is higher than for urban physicians. Rural northern physicians appear to have a broader SoP than physicians in all other regions examined. The longer work hours and variety of clinical activities are important to highlight. Although the proportion of time a rural physician spends on less common areas of clinical practice might be small, the absolute number of hours dedicated to these activities and the total number of physicians participating in these activities might be proportionally greater. Although the largest differences were found between the rural north and the urban south, clinical activity variation occurs across all 4 practice regions. More similarities exist between rural areas (rural north and rural south) than between northern areas (rural north and urban north), suggesting that there is a strong rurality component to our findings. Moreover, this urban-rural difference is further filtered into a north-south division, suggesting that it is not only important to distinguish between rural and urban within an area (ie, rural north vs urban north) but also between rural areas (ie, rural north vs rural south). This finding is consistent with earlier research, which is important to point out, as there has been some tendency in policy and government initiatives to create rural or northern provincial strategies without recognizing the variability between and within these regions.4,31,32
Our findings are relevant for rural and northern policy and program development for medical education (ie, undergraduate through to continuing professional development) and physician resource planning associated with recruitment and retention of physicians.4,26–28,32 Because rural physicians, and rural northern physicians in particular, will be responsible for a wider SoP encompassing a broader spectrum of clinical activities,4 it is imperative that undergraduate and postgraduate medical education appropriately train physicians to practise competently and meet performance requirements in these environments.15,20,23,24,27,28 This has been recognized in other jurisdictions and has led to a specialty certification for rural family practice.21,22,33 For example, in Australia, rural and remote medicine is recognized and certified as a specific specialty of general practice.33 Although this has been previously discussed in Canada, our findings perhaps suggest that these discussions need to be resurrected. A joint CFPC and Society of Rural Physicians of Canada task force, Advancing Rural Family Medicine: The Canadian Collaborative Taskforce, is focused on enhancing equitable access to health care and improving patient outcomes in rural and remote communities in Canada.34 The broader SoP of rural physicians might require targeted continuing professional development programming, customized practice supports, and resources to meet the unique needs of rural physicians and their patients.
From a health system perspective, the recruitment and, more problematically, retention of physicians in rural areas is a global challenge.35–38 Further understanding the breadth of practice activities and clinical competencies required of rural GPs and FPs will allow incoming physicians to know what is expected from a competency and workload perspective, and allow them to make more informed decisions as to whether rural practice is where they wish to anchor their careers. In turn, this also serves to improve retention.
These regional differences in family practice complexity have potential implications for current systems of physician payment to ensure that rural GPs and FPs are fairly compensated.39,40 Under current fee-for-service models, individuals who work more hours and see fewer patients are penalized for practice complexity. Likewise, the breadth of practice within a single physician specialty area is not factored into current salaried systems. The current system rewards physicians who do local shifts in emergency departments and shifts in walk-in clinics rather than devoting all of their time to full-service family practice, which further penalizes rural practitioners who are located in communities that cannot sustain hospitals or walk-in clinics. A reevaluation of compensation for rural practice might further improve retention of GPs and FPs in rural areas.39,40
Limitations
There are several limitations to our research. First, the CPSO survey categorizations of clinical practice activities are potentially problematic and lack nuance. Many GPs and FPs might have solely listed general or family practice and considered many of the other clinical activities to be part of their typical family practice activities, whereas others might have seen this category as solely about office-based practice. Additionally, the general or family practice category itself is complex and does not differentiate the nuances of different patient mixes. For example, practices with patient populations primarily comprising young families and those made up largely of older adults with multiple comorbidities both fall under the general or family practice category, but they are certainly not equivalent in terms of the complexity of care required. Additionally, geography itself might affect how clinical practice categories are interpreted by physicians. For example, how a physician understands hospitalist practice in the rural north might be very different from how it is understood in the urban south. Future work should aim to better understand what all GPs and FPs, including those in rural areas, actually “do” in practice (ie, practice patient case mix and detailed practice activities) to allow for a further refined picture of practice and competency needs. This will assist in better matching physician human resource needs with the needs of the population.
Conclusion
Our study shows that GP and FP SoP is not uniform across Ontario. Rural physicians work more hours and engage in a broader spectrum of clinical activities. Our study demonstrates that physician SoP is not determined by education and certification alone, but is driven by the needs of the patients physicians serve, which varies from region to region. Typically, discussions regarding differences in SoP have been limited and focused on jurisdictions between health professions (ie, who can do what to and with whom). We need to expand our thinking and consider that there are SoP differences within professions, even within specific specialty areas within a profession; understanding these differences might be essential in determining competency needs, thus affecting education and professional development, and resource requirements, affecting health systems planning. This is of particular relevance when examining rural GP and FP practice. With the SoP of rural GPs and FPs, it allows those who wish to be or who are engaged in rural practice to feel that their broad competencies and heavy workloads are appreciated and valued by the population.
Acknowledgments
We thank Jill E. Sherman, formerly of the Centre for Rural and Northern Health Research at Laurentian University in Sudbury, Ont, for creating the map in Figure 1. We thank the College of Physicians and Surgeons of Ontario for providing the data. This work was supported by funds from an Ontario Ministry of Health and Long-Term Care Health Systems Research Fund grant. The views expressed in the publication are those of the authors and do not necessarily reflect those of the College of Physicians and Surgeons of Ontario or the Ontario Ministry of Health and Long-Term Care.
Editor’s key points
▸ This study aimed to examine differences in the scope of practice of GPs and FPs in rural and urban and northern and southern regions of Ontario. Rural physicians, particularly those in the north, engaged in a wider variety of clinical activities, spent less time per activity, and worked more hours per week than physicians in all other regions of the province did. More similarities existed between rural areas (rural north and rural south) than between northern areas (rural north and urban north), suggesting that there is a strong rurality component to the findings.
▸ General or family practice was, not surprisingly, reported as the most common clinical activity across all regions; however, only 56.8% of GPs and FPs in the urban south reported general or family practice as an aspect of their clinical activities in contrast to 85.3% in the rural north. More northern physicians reported engaging in teaching activities than did their southern counterparts. Very few GPs and FPs in the south reported including obstetrics with labour and delivery in their practices, whereas 13.0% of rural northern physicians reported this clinical activity.
▸ More rural GPs and FPs spend more than 50% of their clinical time in general or family practice activities than urban GPs and FPs do. Among these physicians, there was a narrowing of geographic differences in the proportion of time spent on emergency medicine, anesthesia, surgical assists, and palliative care.
Points de repère du rédacteur
▸ Cette étude visait à étudier les différences dans le champ de pratique des omnipraticiens (OP) et des MF selon qu’ils travaillent en milieu rural ou urbain et dans les régions du nord et du sud de l’Ontario. Les médecins ruraux, particulièrement ceux du nord, effectuaient une plus grande variété d’activités cliniques, passaient moins de temps par activité et travaillaient plus d’heures par semaine par rapport aux médecins de toutes les autres régions de la province. Il y avait davantage de similitude entre les régions rurales du nord et du sud qu’entre les régions rurales et urbaines du nord, ce qui suggère qu’il existe une forte composante de ruralité à l’origine de ces observations.
▸ La médecine générale et la médecine de famille étaient les activités cliniques les plus souvent mentionnées, et ce, pour toutes les régions, ce qui n’est pas vraiment surprenant; toutefois, seulement 56,8 % des OP et des MF des régions urbaines du sud disaient que la médecine générale et la médecine familiale faisaient partie de leurs activités cliniques, par rapport à 85,3 % de ceux des régions rurales du nord. Les médecins du nord disaient faire davantage d’enseignement que ceux du sud. Très peu d’OP et de MF du sud mentionnaient qu’ils faisaient aussi des suivis de grossesse et des accouchements, alors qu’à peine 13,0 % de ceux du nord déclaraient faire ce genre de travail.
▸ Plus d’OP et de MF ruraux que d’OP et de MF urbains passaient plus de 50 % de leur temps de pratique comme omnipraticiens ou médecins de famille. Parmi ces médecins, il y avait moins de différences régionales pour ce qui est du pourcentage du temps consacré à la médecine d’urgence, à l’anesthésie, à l’assistance chirurgicale et aux soins palliatifs.
Footnotes
Contributors
Dr Wenghofer, Ms Kam, and Mr Timony contributed to the concept and design of the study and the analysis. Dr Wenghofer and Mr Timony were responsible for data extraction. Dr Wenghofer, Ms Kam, Mr Timony, and Dr Strasser contributed to the analysis and interpretation of the data. All authors have contributed to the writing and revision of the manuscript and have given final approval for publication.
Competing interests
The authors have no competing interests or conflicts to declare
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Backer EL, McIlvain HE, Paulman PM, Ramaekers RC. The characteristics of successful family physicians in rural Nebraska: a qualitative study of physician interviews. J Rural Health. 2006;22(2):189–91. doi: 10.1111/j.1748-0361.2006.00030.x. [DOI] [PubMed] [Google Scholar]
- 2.Beaulieu MD, Rioux M, Rocher G, Samson L, Boucher L. Family practice: professional identity in transition. A case study of family medicine in Canada. Soc Sci Med. 2008;67(7):1153–63. doi: 10.1016/j.socscimed.2008.06.019. Epub 2008 Jul 20. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal D, Gokhale M, Campbell EG, Weissman JS. Preparedness for clinical practice: reports of graduating residents at academic health centers. JAMA. 2001;286(9):1027–34. doi: 10.1001/jama.286.9.1027. [DOI] [PubMed] [Google Scholar]
- 4.Wenghofer EF, Timony PE, Gauthier NJ. ‘Rural’ doesn’t mean ‘uniform’: northern vs southern rural family physicians’ workload and practice structures in Ontario. Rural Remote Health. 2014;14(2):2720. Epub 2014 Jun 24. [PubMed] [Google Scholar]
- 5.Baker E, Schmitz D, Epperly T, Nukui A, Miller CM. Rural Idaho family physicians’ scope of practice. J Rural Health. 2010;26(1):85–9. doi: 10.1111/j.1748-0361.2009.00269.x. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin LM, Rosenblatt RA, Schneeweiss R, Lishner DM, Hart LG. Rural and urban physicians: does the content of their Medicare practices differ? J Rural Health. 1999;15(2):240–51. doi: 10.1111/j.1748-0361.1999.tb00745.x. [DOI] [PubMed] [Google Scholar]
- 7.Grzybowski S, Stoll K, Kornelsen J. The outcomes of perinatal surgical services in rural British Columbia: a population-based study. Can J Rural Med. 2013;18(4):123–9. [PubMed] [Google Scholar]
- 8.Halverson AL, DaRosa DA, Borgstrom DC, Caropreso PR, Hughes TG, Hoyt DB, et al. Evaluation of a blended learning surgical skills course for rural surgeons. Am J Surg. 2014;208(1):136–42. doi: 10.1016/j.amjsurg.2013.12.039. Epub 2014 Apr 5. [DOI] [PubMed] [Google Scholar]
- 9.Hogenbirk J, Wang F, Pong R, Tesson G, Strasser R. Nature of rural medical practice in Canada: an analysis of the 2001 National Family Physician Survey. Sudbury, ON: Centre for Rural and Northern Health Research, Laurentian University; 2004. [Google Scholar]
- 10.Hutten-Czapski P, Pitblado R, Slade S. Short report: scope of family practice in rural and urban settings. Can Fam Physician. 2004;50:1548–50. [PMC free article] [PubMed] [Google Scholar]
- 11.Hutten-Czapski P. Working to the breadth of our licenses. Can J Rural Med. 2013;18(4):119. [PubMed] [Google Scholar]
- 12.Pashen D, Chater A, Murray R, Sheedy V, White C, Eriksson L, et al. The expanding role of the rural generalist in Australia—a systematic review. Canberra, Aust: Australian Primary Health Care Research Institute; 2007. Available from: www.acrrm.org.au/docs/default-source/documents/the-college-at-work/expanding-role-of-rural-generalists.pdf?sfvrsn=8. Accessed 2015 Jul 3. [Google Scholar]
- 13.Probst JC, Moore CG, Baxley EG, Lammie JJ. Rural-urban differences in visits to primary care physicians. Fam Med. 2002;34(8):609–15. [PubMed] [Google Scholar]
- 14.Rabinowitz HK, Paynter NP. The rural vs urban practice decision. JAMA. 2002;287(1):113. [PubMed] [Google Scholar]
- 15.Strasser R, Couper I, Wynn-Jones J, Rourke J, Chater AB, Reid S. Education for rural practice in rural practice. Educ Prim Care. 2016;27(1):10–4. doi: 10.1080/14739879.2015.1128684. Epub 2016 Jan 20. [DOI] [PubMed] [Google Scholar]
- 16.Weeks WB, Yano EM, Rubenstein LV. Primary care practice management in rural and urban Veterans Health Administration settings. J Rural Health. 2002;18(2):298–303. doi: 10.1111/j.1748-0361.2002.tb00890.x. [DOI] [PubMed] [Google Scholar]
- 17.O’Neill T, Peabody MR, Blackburn BE, Peterson LE. Creating the Individual Scope of Practice (I-SOP) scale. J Appl Meas. 2014;15(3):227–39. [PubMed] [Google Scholar]
- 18.Chan B, Schultz S. Supply and utilization of general practitioner and family physician services in Ontario. ICES investigative report. Toronto, ON: Institute for Clinical Evaluative Sciences; 2005. Available from: www.ices.on.ca/~/media/Files/Atlases-Reports/2005/Supply-and-utilization-of-GP-and-FP-services-in-Ontario/Full%20report.ashx. Accessed 2015 May 23. [Google Scholar]
- 19.Tepper J, Schultz S, Rothwell D, Chan B. Physician services in rural and northern Ontario. ICES investigative report. Toronto, ON: Institute for Clinical Evaluative Sciences; 2006. Available from: www.ices.on.ca/~/media/Files/Atlases-Reports/2006/Physicians-services-in-rural-and-northern-Ontario/Full%20report.ashx. Accessed 2015 Jun 5. [Google Scholar]
- 20.Glasser M, Hunsaker M, Sweet K, MacDowell M, Meurer M. A comprehensive medical program responds to rural primary care needs. Acad Med. 2008;83(10):952–61. doi: 10.1097/ACM.0b013e3181850a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simmons PD. Rural medicine: its own specialty? J Rural Health. 2009;25(3):231–2. doi: 10.1111/j.1748-0361.2009.00223_1.x. [DOI] [PubMed] [Google Scholar]
- 22.Smith J, Hays R. Is rural medicine a separate discipline? Aust J Rural Health. 2004;12(2):67–72. doi: 10.1111/j.1038-5282.2004.00556.x. [DOI] [PubMed] [Google Scholar]
- 23.Strasser R, Neusy AJ. Context counts: training health workers in and for rural and remote areas. Bull World Health Organ. 2010;88(10):777–82. doi: 10.2471/BLT.09.072462. Epub 2010 Aug 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tesson G, Curran V, Pong R, Strasser R. Advances in rural medical education in three countries: Canada, the United States and Australia. Educ Health (Abingdon) 2005;18(3):405–15. doi: 10.1080/13576280500289728. [DOI] [PubMed] [Google Scholar]
- 25.Health Canada Health human resources: balancing supply and demand. Health Policy Res. 2004;8:1–48. [Google Scholar]
- 26.Curran V, Rourke J. The role of medical education in the recruitment and retention of rural physicians. Med Teach. 2004;26(3):265–72. doi: 10.1080/0142159042000192055. [DOI] [PubMed] [Google Scholar]
- 27.Habjan S, Kortes-Miller K, Kelley M, Sullivan H, Pisco L. Building capacity in rural health services: the effect of continuing education. In: Kulig J, Williams A, editors. Health in rural Canada. Vancouver, BC: UBC Press; 2012. pp. 118–36. [Google Scholar]
- 28.Tesson G, Pong R, Strasser R. Distributed medical education as a solution to physician maldistribution: the case of the Northern Ontario School of Medicine. Cah Sociol Demogr Med. 2008;48(2):289–306. [PubMed] [Google Scholar]
- 29.Statistics Canada . Postal code conversion file. Ottawa, ON: Statistics Canada; 2013. [PubMed] [Google Scholar]
- 30.Ontario’s LHINs [website] Toronto, ON: Local Health Integration Networks; 2014. Available from: www.lhins.on.ca. Accessed 2016 Jun 14. [Google Scholar]
- 31.Carson DB, Wenghofer E, Timony P, Schoo A, Berggren P, Charters B, et al. Recruitment and retention of professional labour: the health workforce at settlement level. In: Taylor A, Carson DB, Ensign P, Huskey T, Rasmussen R, Saxinger G, editors. Settlements at the edge: remote human settlements in developed nations. Cheltenham, UK: Edward Elgar Publishing; 2016. pp. 320–36. [Google Scholar]
- 32.Wenghofer EF, Timony PE, Pong RW. A closer look at Ontario’s northern and southern rural physician demographics. Rural Remote Health. 2011;11(2):1591. Epub 2011 Mar 15. [PubMed] [Google Scholar]
- 33.Overview of fellowship training [website] Brisbane, Aust: Australian College of Rural and Remote Medicine; 2018. Available from: www.acrrm.org.au/training-towards-fellowship/overview-of-fellowship-training. Accessed 2018 May 15. [Google Scholar]
- 34.Bosco C, Oandasan I. Review of family medicine within rural and remote Canada: education, practice, and policy. Mississauga, ON: College of Family Physicians of Canada; 2016. [Google Scholar]
- 35.Hancock C, Steinbach A, Nesbitt TS, Adler SR, Auerswald CL. Why doctors choose small towns: a developmental model of rural physician recruitment and retention. Soc Sci Med. 2009;69(9):1368–76. doi: 10.1016/j.socscimed.2009.08.002. Epub 2009 Sep 9. [DOI] [PubMed] [Google Scholar]
- 36.Strasser R, Hogenbirk JC, Lewenberg M, Story M, Kevat A. Starting rural, staying rural: how can we strengthen the pathway from rural upbringing to rural practice? Aust J Rural Health. 2010;18(6):242–8. doi: 10.1111/j.1440-1584.2010.01167.x. [DOI] [PubMed] [Google Scholar]
- 37.Wibulpolprasert S. How do we produce and maintain rural generalists in Thailand?. Paper presented at: 2nd World Summit on Rural Generalist Medicine; 2015 Apr 8–9; Montreal, QC. [Google Scholar]
- 38.World Health Organization . Increasing access to health workers in remote and rural areas through improved retention. Geneva, Switz: World Health Organization; 2010. Available from: http://apps.who.int/iris/bitstream/10665/44369/1/9789241564014_eng.pdf. Accessed 2015 Jul 23. [PubMed] [Google Scholar]
- 39.Gosden T, Forland F, Kristiansen IS, Sutton M, Leese B, Giuffrida A, et al. Capitation, salary, fee-for-service and mixed systems of payment: effects on the behaviour of primary care physicians. Cochrane Database Syst Rev. 2000;(3):CD002215. doi: 10.1002/14651858.CD002215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gosden T, Forland F, Kristiansen IS, Sutton M, Leese B, Giuffrida A, et al. Impact of payment method on behaviour of primary care physicians: a systematic review. J Health Serv Res Policy. 2001;6(1):44–55. doi: 10.1258/1355819011927198. [DOI] [PubMed] [Google Scholar]