Abstract
Introduction
In the emergency department (ED), critical events, including death and severe illness, are not uncommon. Critical events involving children, while less frequent, may be especially distressing. Debriefing following a critical event may serve several purposes: review of team performance, education, identification of errors, emotional support, and planning for future events. Debriefing skills and habits learned during training may be carried forward throughout an emergency physician's career. This study evaluates how educators in emergency medicine (EM) view debriefing after pediatric critical events and identifies barriers to use of debriefing in postgraduate training programs.
Methods
In this cross‐sectional observational study, we surveyed program directors (PDs) from EM residency and pediatric emergency medicine (PEM) fellowship programs via e‐mail listserv. A panel of PEM experts and survey methodologists designed the survey, which was reviewed for content validity by an independent panel of EM educators. We obtained data on current debriefing practices following pediatric critical events, PDs’ perceptions of ideal debriefing practices, and barriers to implementation. Data were analyzed using descriptive statistics.
Results
A total of 109 PDs completed the survey (45% overall response rate). All respondents feel that debriefing pediatric critical events is useful. The majority of debriefings are initiated and led by emergency physicians as informal meetings shortly following a critical event. Debriefings are most commonly held following a patient death, although PDs feel that debriefings should also occur for other specific patient scenarios (e.g., child abuse). Barriers to debriefing include timing, scheduling, location, discomfort with debriefing, participant buy‐in, and leader buy‐in.
Conclusions
Program leaders in both EM and PEM believe that debriefing after pediatric critical events is important for training. Barriers to debriefing specific to the ED setting should be explored to optimize the implementation of this practice.
By its nature, the practice of emergency medicine (EM) is unpredictable and often stressful. Critical events—any distressing event that triggers an emotional response so strong it overwhelms the usual coping mechanisms—are not infrequent. Critical incidents involving children may be particularly distressing for medical professionals and laypeople alike.1, 2, 3, 4, 5 Emotional reactions to these events may affect healthcare professionals’ ability to function in their professional roles.6 The healthcare provider has been described as the “second victim” of such events—the patient being the first—highlighting the effects on the well‐being of the provider.7 Emergency physicians must develop strategies to manage their responses to these events to mitigate postevent trauma and the second victim effect.1, 7, 8, 9
While there are well‐described debriefing methodologies, including critical incident stress debriefing or critical incident stress management,10 we define the term “debriefing” broadly here to connote any semistructured meeting held following a critical event for the purposes of review and discussion of team performance, education, identification of errors, emotional response and support, and development of plans for the future. Debriefing has been used successfully in the military, aviation, and other settings to reduce stress following traumatic events.11 Organizations including the American Heart Association and American Academy of Pediatrics recommend debriefing as a means to improve individual and team performance and improve patient safety.12, 13, 14 It can also serve to promote education,15, 16 provide emotional support, and decrease second victim effect.1, 17, 18, 19 Studies in North America, Europe, and Australia have shown that although viewed as useful, debriefing is used infrequently.3, 6, 20, 21
Little is known about how emergency physicians are trained to debrief critical events involving children. One study of pediatric EM (PEM) fellows in the United States revealed little formal training during subspecialty fellowship on leading debriefings.21 Expertise and proficiency in any aspect of medical practice relies on exposure, experience, and opportunities for feedback.22 Therefore, including debriefing in the EM training experience may encourage its use throughout an individual's career and subsequently may reduce the posttraumatic reactions cause by these highly stressful critical events.
The aims of this study were to describe the frequency and current practice of debriefing after pediatric critical events in EM training, gauge the perceptions of educators and educational leaders regarding how critical event debriefing should ideally be used, and identify the barriers to using debriefing after pediatric critical events in EM training programs.
Methods
Study Design
A panel of specialists in PEM, in collaboration with an expert in survey methodology, designed a survey that contained questions about debriefing after critical events involving children. It was reviewed for content validity and response process by a group of subject matter experts from EM, including educators and current and recent past program directors. The survey was revised based those recommendations.
Program leaders from EM training programs in the United States, including PEM fellowship and EM residency programs, were contacted by e‐mail containing a link to the electronic survey (Data Supplement S1, available as supporting information in the online version of record of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1002/aet2.10031/full). PEM fellowship and EM residency programs were chosen as they both train physicians in the management of children in the emergency department (ED). One program leader—either program director or assistant/associate program director—from each training program was asked to respond. E‐mails were sent with permission to the PEM fellowship program directors’ listserv and the Council of Emergency Medicine Residency Directors (CORD) listserv. Two reminders were sent at 2‐week intervals. Participation was voluntary and anonymous. This study was reviewed by the institutional review board at the lead institution and met criteria for exempt status.
Key Outcome Measures
Characteristics of each training program, along with hospital information, were obtained. Information on current practices of debriefing after critical events involving children was collected, including how often debriefings were held; who was responsible for initiating and leading them; the format, timing, location, and participants; the critical events for which they were held; and the goals of the debriefing. Similar information was also obtained about the program director's perceived ideal debriefing after pediatric critical events. Barriers to performing debriefings within the training context were also assessed.
Data Analysis
Current and ideal debriefing practices and barriers to debriefing after pediatric critical events were assessed using descriptive statistics. Data were analyzed using STATA version 14 (2015, Stata Statistical Software: Release 14, StataCorp).
Results
The survey was sent to program directors and assistant program directors from a total of 78 PEM fellowship programs and 165 EM residency programs. Program leaders from 109 training programs responded to the survey for an overall response rate of 45% (55% of all PEM fellowships and 40% of all EM residency programs). Of all respondents, 43 (39.5%) were from PEM fellowship programs and 66 (60.6%) were from EM residency programs.
Program characteristics and hospital characteristics, including program size, type of ED, annual pediatric volume, pediatric trauma center level, and geographic region, are summarized in Table 1.
Table 1.
Program and Hospital Characteristics for EM Training Programs
| PEM Fellowships, 39.5% (n = 43) | EM Residencies, 60.6% (n = 66) | Total | |
|---|---|---|---|
| Types of trainees | |||
| EM residents | 97.7 (42) | 100.0 (66) | 99.1 (108) |
| Pediatric residents | 95.4 (41) | 47.0 (31) | 66.1 (72) |
| Internal medicine residents | 9.3 (4) | 80.3 (53) | 52.3 (57) |
| Family medicine residents | 74.4 (32) | 60.6 (40) | 66.1 (72) |
| PEM fellows | 97.7 (42) | 33.3 (22) | 58.7 (64) |
| Other | 18.6 (8) | 33.3 (22) | 27.5 (30) |
| ED | |||
| Community‐based general | 2.3 (1) | 60.6 (40) | 37.6 (41) |
| University‐based general | 11.6 (5) | 53.0 (35) | 36.7 (40) |
| Community‐based pediatric | 16.3 (7) | 18.2 (12) | 17.4 (19) |
| University‐based pediatric | 81.4 (35) | 31.8 (21) | 51.4 (56) |
| Pediatric trauma center level | |||
| Level I | 88.1 (37) | 70.8 (46) | 77.6 (83) |
| Level II | 7.1 (3) | 18.5 (12) | 14.0 (15) |
| Not a trauma center | 4.8 (2) | 10.8 (7) | 8.4 (9) |
| Annual pediatric visits | |||
| <10,000 | 0.0 (0) | 16.0 (8) | 9.1 (8) |
| 10,000–24,999 | 0.0 (0) | 54.0 (27) | 29.7 (27) |
| 25,000–49,999 | 44.7 (17) | 18.0 (9) | 29.6 (26) |
| 50,000–74,999 | 23.7 (9) | 8.0 (4) | 14.8 (13) |
| >75,000 | 31.6 (12) | 4.0 (2) | 15.9 (14) |
| Region | |||
| Northeast | 36.8 (14) | 31.6 (18) | 33.7 (32) |
| South Atlantic | 13.2 (5) | 17.5 (10) | 15.8 (15) |
| North Central | 23.7 (9) | 26.3 (15) | 25.3 (24) |
| South Central | 13.2 (5) | 5.3 (3) | 8.4 (8) |
| Mountain | 5.3 (2) | 3.5 (2) | 4.2 (4) |
| West | 7.9 (3) | 15.8 (9) | 12.6 (12) |
Data are reported as % (n).
PEM = pediatric emergency medicine.
Current Critical Event Debriefing Practices
Current debriefing practices and beliefs are reported in Figure 1. The majority of program leaders have attended a debriefing. All PEM and EM program directors believe that debriefing after critical events is at least somewhat useful.
Figure 1.

Current use and perceived utility of critical event debriefing after pediatric critical events. (A) Current practice: program leaders’ responses to “Do you hold debriefings after critical events involving children in your emergency department?” (B) Ideal practice: program leaders’ responses to “Do you think debriefing after a critical event is useful?”
The current practices of debriefing after pediatric critical events are shown in Table 2. If held, most debriefings are initiated and attended by the attending emergency physician. Other participants include resident or fellow physicians, nurses, social workers, and other staff. Others reported to attend include medical students, ED technicians, emergency medical services, chaplains, respiratory therapists, registration personnel, secretaries, housekeeping, and anyone who wants to attend. The format is most commonly an informal meeting held in response to a critical event, as opposed to a scheduled meeting in response to a critical event or previously scheduled formal meeting. Most debriefings are located in the ED. The timing of the debriefings are variable, most commonly occurring shortly after the event.
Table 2.
Current Debriefing Practice After Pediatric Critical Events
| Current Practice | |
|---|---|
| Member who initiates debriefing | |
| Emergency physicians | 64.5 (60) |
| Nurses | 30.1 (28) |
| Resident/fellow physicians | 11.8 (11) |
| Social workers | 11.8 (11) |
| Other staff | 16.1 (15) |
| Debriefing leader | |
| Physician team leader | 47.1 (41) |
| Any team member | 20.7 (18) |
| Other staff | 13.8 (12) |
| Social workers | 10.3 (9) |
| Nurses | 8.1 (7) |
| Debriefing attendees | |
| Attending physicians | 88.2 (82) |
| Resident/fellow physicians | 85.0 (79) |
| Nurses | 82.8 (77) |
| Other clinical staff | 59.1 (55) |
| Social workers | 53.8 (50) |
| Other nonclinical staff | 23.7 (22) |
| Debriefing format | |
| Informal meeting in response to critical event | 75.3 (70) |
| Scheduled meeting in response to critical event | 44.1 (41) |
| Previously scheduled formal meeting | 5.4 (5) |
| Other | 7.5 (7) |
| Debriefing timing | |
| Immediately | 23.9 (21) |
| Same shift | 22.7 (20) |
| 1–3 d | 19.3 (17) |
| 4–14 d | 9.1 (8) |
| Previously scheduled meetings | 2.3 (2) |
| Other | 22.7 (20) |
| Debriefing location—ED | 75.3 (64) |
| Critical events | |
| Death of a patient | 68.8 (64) |
| Multitrauma | 40.9 (38) |
| SIDS | 39.8 (37) |
| Significant injury | 38.7 (36) |
| Child abuse | 29.0 (27) |
| Clinical error | 25.8 (24) |
| Debriefing goals | |
| Emotional support | 82.8 (77) |
| Reduce distress | 77.4 (72) |
| Identify systems issues | 55.9 (52) |
| Medical management | 52.7 (49) |
Data are reported as % (n).
SIDS = sudden infant death syndrome.
The pediatric critical events for which debriefing is reportedly used include death of a child, multitrauma, sudden infant death syndrome (SIDS), significant injury, child abuse, and clinical error. Other critical events for which debriefings were held including critical illness or any event that was deemed traumatic by the staff. The reported goals of debriefing following critical events were to provide emotional support, reduce distress, identify systems or process issues that contributed to the event, and discuss medical management (Table 2).
Ideal Debriefing Practices
Program leaders’ perceptions of the ideal practices for debriefing after pediatric critical events are shown in Table 3. The majority of EM training program leaders feel that, in the ideal setting, any team member should be able to initiate a debriefing. Program leaders report that debriefings should ideally be attended by attending physicians, nurses, residents or fellows, other clinical staff, social work, and any other staff who feel they need or want to attend. EM training program leaders feel that debriefings should ideally be held either immediately after the critical event, within the same shift as the event, or 1 to 3 days later. Nearly half of program leaders prefer a meeting scheduled in response the critical event to an informal meeting or previously scheduled formal meeting. Most program leaders report that the meeting should ideally be located in the ED.
Table 3.
Ideal Debriefing Practice After Pediatric Critical Events
| Ideal Practice | |
|---|---|
| Debriefing attendees | |
| Attending physicians | 82.6 (90) |
| Nurses | 82.6 (90) |
| Resident/fellow physicians | 81.8 (89) |
| Other clinical staff | 76.2 (83) |
| Social workers | 70.6 (77) |
| Other nonclinical staff | 54.1 (59) |
| Debriefing format | |
| Scheduled meeting in response to critical event | 49.5 (45) |
| Informal meeting in response to critical event | 36.3 (33) |
| Previously scheduled formal meeting | 7.7 (7) |
| Other | 6.6 (6) |
| Debriefing timing | |
| Immediately | 34.7 (33) |
| Same shift | 27.4 (26) |
| 1–3 d | 32.6 (31) |
| 4–14 d | 2.1 (2) |
| Previously scheduled meetings | 0.0 (0) |
| Other | 3.2 (3) |
| Debriefing location—ED | 67.0 (63) |
| Critical events | |
| SIDS | 84.4 (92) |
| Death of a patient | 79.8 (87) |
| Clinical error | 66.1 (72) |
| Child abuse | 59.6 (65) |
| Significant injury | 56.0 (61) |
| Multi‐trauma | 40.4 (44) |
| Debriefing goals | |
| Emotional support | 84.4 (92) |
| Reduce distress | 82.6 (90) |
| Identify systems issues | 67.0 (73) |
| Medical management | 56.0 (61) |
Data are reported as % (n).
SIDS = sudden infant death syndrome.
The pediatric critical events for which program leaders report that debriefing should ideally be used include SIDS, any death of a child, clinical error, child abuse, significant injury, and multitrauma. They report that the goals of debriefing after pediatric critical events should be to provide emotional support, to reduce distress, to identify systems or process issues that contributed to the event, and to discuss medical management (Table 3).
Barriers to Debriefing
Barriers to debriefing, as reported by educational leaders in EM, are shown in Figure 2. Barriers included timing of debriefing sessions, achieving buy‐in from leaders or participants, scheduling, finding an appropriate space, or discomfort with the process of debriefing. Other responses included “lack of awareness,” “other clinical needs of the department,” “other patients waiting,” and the feeling of “playing catch‐up.”
Figure 2.
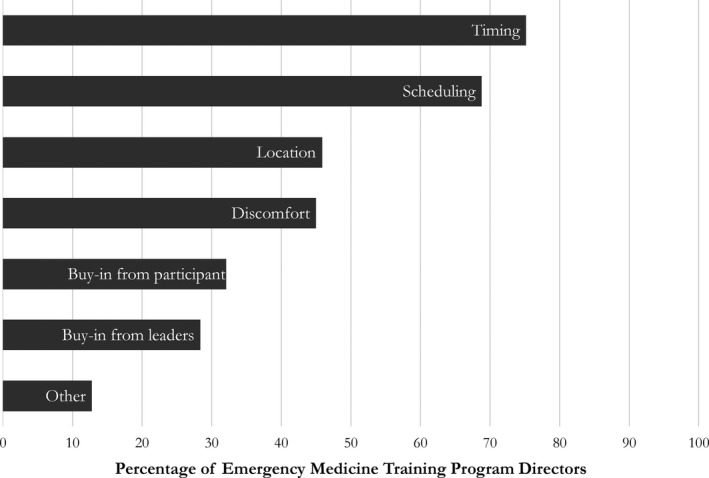
Barriers to debriefing pediatric critical events.
Discussion
Debriefing after a critical event involving a child in the ED provides an important opportunity for physicians and other team members to discuss team performance and medical management, provide education, identify errors, discuss future performance, and buffer the emotional impact of the event on the team.23 Respondents in our study report that emotional support and stress reduction should be included in the goals of critical event debriefing, supporting that which is reported in the literature.1, 17, 23 As a learning experience, attending or leading a debriefing after critical events may help learners in EM to develop skills not only in resuscitation and other clinical skills, but to develop habits such as reflection and introspection, which may increase resilience and decrease burnout.24 Program leaders in EM training programs believe that debriefing after critical events involving children in the ED should be used and should be used more frequently.
The majority of EM training program leaders felt that debriefing should be held shortly following a pediatric critical event. Salas et al.23 describe in their best practices for that debriefings should occur close in time to the event to allow the team members to recall the events and make a link between their own behaviors and outcome. While the inherently unpredictable nature of the ED environment may preclude immediate debriefing, we believe that a formal mechanism for identifying and reporting critical events may allow educators to plan timelier debriefings.
Physicians feel that debriefing is important after medical or trauma resuscitations.3, 20, 21, 25 In the DISCERN program, participants were more likely to debrief for those patients with more intensive interventions, those who were critically ill (including those who did not survive in the ED), and older children.17 Our results indicate that in addition to critically ill children, EM program leaders feel that debriefings should be held for other pediatric events including SIDS, significant injury, child abuse, and clinical errors. These events may be distressing for learners and experienced practitioners alike, and debriefing allows the opportunity to process the complex emotional responses to these stressful occurrences.
Debriefing after pediatric events is used variably by program leaders in EM. While the majority of program leaders report they believe that debriefing a critical event is useful, most actually hold debriefings only sometimes. This gap may reflect the barriers to the use of debriefings. The barriers reported here by program leaders in EM are in keeping with those described in the literature. Healy and Tyrrell6 identified barriers to debriefing to include lack of debriefing guidelines and heavy workloads. These general themes—difficulty balancing debriefing with the needs of a busy ED and difficulty scheduling debriefing at a time when all participants are available—are reflected in our findings. Postgraduate training programs may be able to overcome some of these barriers by using a more structured format for identifying debriefing opportunities and convening debriefing sessions, rather than relying on ad hoc reporting and arrangement. Trainees may then feel empowered to identify opportunities for debriefing and initiate debriefing proceedings. In prior studies, trainees report receiving little formal training in debriefing critical events.21 This may be an opportunity to strengthen residency and fellowship curricula.
Physicians recognize the importance of critical event debriefing and believe that it should occur more often.1 In our study, educational leaders in EM also believe that debriefing is important and underutilized. This represents an important next step to improving education on and use of critical event debriefing. Future efforts should highlight successful examples of debriefing practices founded in evidenced‐based best practices.23 Research should focus on identifying specific methodologies that are most effective and efficient in the ED setting, as well as developing effective curricula for teaching debriefing in medical training and professional development.
Limitations
Cross‐sectional studies are subject to recall bias; program leaders were asked to recall the use of debriefing over an unspecified time period. Social desirability bias may have contributed to overestimation of current debriefing practices as survey respondents were aware that this was a study of debriefing critical events. Only approximately one‐fifth of program leaders reported almost always or always using debriefing and therefore may not be expert enough to determine the goals of debriefing or the critical events for which debriefing should be used. The response rate to our survey was 45%, and respondents may not be representative of all program leaders. Although the survey instructions sought only one response per program, to protect confidentiality we did not control for the possibility of multiple responses from individual programs
Conclusion
Program directors from emergency medicine training programs believe debriefing after pediatric critical events is useful and important. These program leaders feel that debriefing should be held more frequently, should be held soon after a critical event, and should include clinical and nonclinical staff. In addition to cases of critical illness or injury, we have identified other pediatric events—including unexplained death, significant injuries, child abuse, and medical errors—after which debriefing may also help learners process and recover. Interventions to overcome barriers to debriefing of pediatric critical events may increase its use in the ED.
Supporting information
Data Supplement S1. Electronic survey.
AEM Education and Training 2017;1:208–214.
Presented at the Society for Academic Emergency Medicine (SAEM) New England Regional Meeting, Worcester, MA, March 30, 2016; and the SAEM 2016 Annual Meeting, New Orleans, LA, May 13, 2016.
The authors have no relevant financial information or potential conflicts to disclose.
References
- 1. Theophilos T, Magyar J, Babl FE. Debriefing critical incidents in the paediatric emergency department: current practice and perceived needs in Australia and New Zealand. Emerg Med Australas 2009;21:479–83. [DOI] [PubMed] [Google Scholar]
- 2. Healy S, Tyrrell M. Stress in emergency departments: experiences of nurses and doctors. Emerg Nurse 2011;19:31–7. [DOI] [PubMed] [Google Scholar]
- 3. Ireland S, Gilchrist J, Maconochie I. Debriefing after failed paediatric resuscitation: a survey of current UK practice. Emerg Med J 2008;25:328–30. [DOI] [PubMed] [Google Scholar]
- 4. Willebrand M, Sveen J. Injury‐related fear‐avoidance and symptoms of posttraumatic stress in parents of children with burns. Burns 2016;4:414–20. [DOI] [PubMed] [Google Scholar]
- 5. Burns C, Harm NJ. Emergency nurses’ perceptions of critical incidents and stress debriefing. J Emerg Nurs 1993;19:431–6. [PubMed] [Google Scholar]
- 6. Healy S, Tyrrell M. Importance of debriefing following critical incidents. Emerg Nurse 2013;20:32–7. [DOI] [PubMed] [Google Scholar]
- 7. Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320:726–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Garmany JD, Gonzalez F, Ketron M, et al. Implementation of critical incident stress debriefing at the Johnson City Medical Center Emergency Department. Tenn Nurse 1998;61:20–2. [PubMed] [Google Scholar]
- 9. Caine R, Ter‐Bagdasarian L. Early identification and management of critical incident stress. Crit Care Nurse 2003;23:59–65. [PubMed] [Google Scholar]
- 10. Mitchell JT. When disaster strikes.. the critical incident stress debriefing process. JEMS 1983;8:36–9. [PubMed] [Google Scholar]
- 11. Fillion JS, Clements PT, Averill JB, Vigil GJ. Talking as a primary method of peer defusing for military personnel exposed to combat trauma. J Psychosoc Nurs Ment Health Serv 2002;40:40–9. [DOI] [PubMed] [Google Scholar]
- 12. Bhanji F, Mancini ME, Sinz E, et al. Part 16: education, implementation, and teams: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S920–33. [DOI] [PubMed] [Google Scholar]
- 13. Krug SE, Frush K. Patient safety in the pediatric emergency care setting. Pediatrics 2007;120:1367–75. [DOI] [PubMed] [Google Scholar]
- 14. Nolan JP, Soar J, Zideman DA, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation 2010;81:1219–76. [DOI] [PubMed] [Google Scholar]
- 15. Kessler DO, Cheng A, Mullan PC. Debriefing in the emergency department after clinical events: a practical guide. Ann Emerg Med 2015;65:690–8. [DOI] [PubMed] [Google Scholar]
- 16. Mullan PC, Kessler DO, Cheng A, et al. Educational opportunities with postevent debriefing. JAMA 2014;312:2333. [DOI] [PubMed] [Google Scholar]
- 17. Mullan PC, Wuestner E, Kerr TD, Christopher DP, Patel B. Implementation of an in situ qualitative debriefing tool for resuscitations. Resuscitation 2013;84:946–51. [DOI] [PubMed] [Google Scholar]
- 18. Rose S, Bisson J, Churchill R, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database Syst Rev 2002;(2):CD000560. [DOI] [PubMed] [Google Scholar]
- 19. Seys D, Scott S, Wu A, et al. Supporting involved health care professionals (second victims) following an adverse health event: a literature review. Int J Nurs Stud 2013;50:678–87. [DOI] [PubMed] [Google Scholar]
- 20. Sandhu N, Eppich W, Mikrogianakis A, Grant V, Robinson T, Cheng A. Postresuscitation debriefing in the pediatric emergency department: a national needs assessment. CJEM 2014;16:383–92. [PubMed] [Google Scholar]
- 21. Zinns LE, O'Connell KJ, Mullan PC, Ryan LM, Wratney AT. National survey of pediatric emergency medicine fellows on debriefing after medical resuscitations. Pediatr Emerg Care 2015;31:551–4. [DOI] [PubMed] [Google Scholar]
- 22. Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 2004;79(10 Suppl):S70–81. [DOI] [PubMed] [Google Scholar]
- 23. Salas E, Klein C, King H, et al. Debriefing medical teams: 12 evidence‐based best practices and tips. Jt Comm J Qual Patient Saf 2008;34:518–27. [DOI] [PubMed] [Google Scholar]
- 24. Halpern J, Maunder RG, Schwartz B, Gurevich M. Downtime after critical incidents in emergency medical technicians/paramedics. Biomed Res Int 2014;2014:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Berg GM, Hervey AM, Basham‐Saif A, Parsons D, Acuna DL, Lippoldt D. Acceptability and implementation of debriefings after trauma resuscitation. J Trauma Nurs 2014;21:201–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Electronic survey.


