Abstract
Background
Given the increased use of psychoactive substances on the US-Mexico border, a binational study (Tijuana, Mexico-Los Angeles, USA) was conducted to identify the prevalence of substance use in primary care settings.
Objectives
To compare the prevalence and characteristics of patients at risk for substance use disorders in Tijuana and East Los Angeles (LA) community clinics with special attention paid to drug use.
Methods
Design
Observational, cross-sectional, analytical study. Comparison of screening results from patients in Tijuana and LA.
Setting
2 community clinics in LA and 6 in Tijuana.
Participants
2,507 adult patients in LA and 2,890 in Tijuana eligible for WHO Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) screening during March-October 2013.
Measures
WHO ASSIST self-administered on a tablet PC.
Results
Of eligible patients, 96.4% completed the ASSIST in Tijuana and 88.7% in LA (mean 1.34 minutes and 4.20 minutes, respectively). The prevalence of patients with moderate-to-high substance use was higher in LA than Tijuana for each substance: drugs 19.4% vs. 5.7%, alcohol 15.2% vs. 6.5%, tobacco 20.4% vs. 16.2%. LA patients born in Mexico had 2x the odds and LA patients born in the US had 6x the odds of being a moderate-to-high drug user compared to Tijuana patients born in Mexico.
Conclusions
Moderate-to-high drug use is higher in LA than in Tijuana but rates are sufficiently high in both to suggest that screening for drug use (along with alcohol and tobacco use) should be integrated into routine primary care of community clinics in both cities.
INTRODUCTION
The World Health Organization (WHO) has identified substance abuse (excessive use of alcohol, tobacco and drugs) as one of the 20 main risk factors for poor health, morbidity and mortality (WHO, 2009). Therefore identifying strategies to prevent and reduce substance abuse is critical, especially in areas with high rates such as areas along the US-Mexico border (Pan American Health Organization, 2014). These areas include the cities of Los Angeles in the U.S. and Tijuana in Mexico.
Although still of concern, rates of drug use in the city of Tijuana are estimated to be lower than in Los Angeles based on household surveys, and rates are lower in the country of Mexico than in the US. According to Mexico’s most recent National Addiction Survey of 2011 (Instituto Nacional de Psiquiatría Ramón de la Fuente [INPRFM], Instituto Nacional de Salud Pública [INSP], & Secretaría de Salud [SS], 2012), the Mexican national prevalence of drug use among adults aged 12 to 65 years was 1.8% in the past year (3% in men and 0.7% in women), with marijuana being the most commonly used drug (1.2%), followed by cocaine (0.5%) and amphetamine type stimulants (0.2%). The northern border region has the highest prevalence of drug use (2.8%), particularly amphetamine-type stimulants (1.4%) (INPRFM, INSP & SS, 2012). Although Mexico is a country with low drug use compared to other countries in America and Europe (Organization of American States, 2013), the drug use rates have been rising due, among other factors, to the increase in availability of substances and because it is a country of drug production and transit (United Nations Office on Drugs and Crime, 2015).
In the US in 2005–2012, 14.7% of the population aged 12 or older had used any drug in the past year, as compared to 15.4% in the Los Angeles area (Substance Abuse and Mental Health Services Administration [SAMHSA], 2013). In the US, marijuana was the most commonly used drug (7.3%), followed by nonmedical use of psychotherapeutic drugs (2.6%) and cocaine (0.6%). Mexicans, comprise the largest group of immigrants in the US yet foreign-born Latinos have lower rates of substance use than Latinos born in the United States (Alegria et al., 2007; Cook, Alegria, Lin, & Guo, 2009; Perreira et al., 2015).
Despite substantial prevalence rates in both countries, only a minority of users are detected and treated (WHO, 2011). In Mexico, only 9.4% of people who used drugs during the last year received treatment during 2011 (10.3% males and 6.1% females) (INPRFM, INSP, SS, 2012). In the US, among persons with a substance use disorder (SUD) only 10.9% had received SUD treatment at a SUD specialty facility in the past year (SAMHSA, 2013). Barriers to detect drug use include the stigma attached to drug users and the notion held by many lay persons and health professionals that substance use disorders are not medical conditions (Abou-Saleh, 2006).
The WHO emphasizes the detection and treatment of substance use disorders into the care of patients of primary care clinics to reduce the drug abuse problem (Agerwala & McCance-Katz, 2012; Babor & Kadden, 2005; Babor et al., 2007; Cherpitel & Ye, 2008; Goldstein, Whitlock, & DePue, 2004; Humphreys & McLellan, 2010; Pilowsky & Wu, 2012; Shapiro, Coffa, & McCance-Katz, 2013; WHO, 2011). However few studies in the US or Mexico provide reliable estimates of the prevalence of drug use in primary care settings required to implement this strategy (Gelberg et al., 2015; Gryczynski et al., 2014; Lebrun-Harris, Tomoyasu, & Ngo-Metzger, 2014; Lee, Delbanco, Wu, & Gourevitch, 2011; Madras et al., 2009; McNeely et al., 2014a; Roy-Byrne et al., 2014; Saitz et al., 2014; Smith, Schmidt, Allensworth-Davies, & Saitz, 2010). Some information exists regarding the prevalence of substance use along the border for the general household population and emergency room patients, (Borges et al., 2009; Borges et al., 2015; Borges et al., 2011; Cherpitel et al., 2015; Guerrero et al., 2014), SUD specialty treatment centers (Sánchez-Huesca, Arellanez-Hernández, Pérez-Islas, & Rodríguez-Kuri, 2006), or among high risk populations (Chittoor et al., 2013; McDougal et al., 2013; Pitpitan et al., 2013; Servin et al., 2015). However, there is virtually no research on the prevalence of drug use in community health centers (Gelberg et al., 2015) and there are no comparative studies of rates of substance use in primary care setting along the Mexico/U.S border. Therefore, based on the recommendations of the 9th US-Mexico Binational Conference on Drug Demand Reduction-2011(Office of National Drug Control Policy, 2011), we developed a study comparing drug use rates based on screening in community health centers (CHCs) along the US-Mexico border, specifically in the cities of East Los Angeles (LA), US and Tijuana, Mexico, with the expectation of developing similar models of care on both sides of the border. This paper seeks to estimate the rates and correlates of illicit drug misuse, and to compare rates of illicit drug misuse to rates of alcohol and tobacco misuse among patients of CHCs in both countries.
METHODS
This paper is part of a larger study, the “US Binational Quit Using Drugs Intervention Trial”, a randomized controlled trial of screening and brief intervention for risky drug use in adult patients of community health centers of Los Angeles and Tijuana (Gelberg et al., 2015).The study was approved by the UCLA Institutional Review Board and the Ethics Committee of the Mexico National Institute of Psychiatry.
SAMPLING
Clinics
The study Clinics were selected to study substance screening and brief intervention from the border cities of Tijuana and East LA. Both cities had primarily low-income Latino patient populations (California Office of Statewide Health Planning and Development [OSHPD], 2013). The clinics were selected by the following criteria: they included general medical services (i.e., they were primary care centers); were located in at-risk areas for substance use, according to data from the Secretariat of Health of Baja California (INPRFM, INSP & SS, 2012) and data from the Los Angeles County Department of Public Health, Office of Health Assessment and Epidemiology (Los Angeles County Department of Public Health [LACDPH], 2009); were not clinics specializing in addiction treatment; and agreed to participate. Tijuana had thirty CHCs and East Los Angeles had fourteen CHCs (Health Resources and Services Administration [HRSA], 2016; Secretaria de Salud del Estado de Baja California, 2015). Six CHCs were selected in Tijuana and two in East LA. Clinics in Tijuana had fewer patients so more clinics were selected in Tijuana in order to screen similar numbers of patients as in East LA in the allowed screening time. Moreover, given the higher rates of substance use in the communities of East LA (LACDPH, 2009), more clinics had to be selected in Tijuana to obtain an adequate number of risky drug using patients.
Sessions within Clinics
Weekday clinic sessions were selected that had the most patients and research assistants (RAs) available to do screening. Weekend and evening sessions were excluded in both cities because fewer patients attended compared to weekday sessions.
Eligible Patients Completing the ASSIST
Patient sampling took place in LA from March to July, 2013 and in Tijuana from June to October 2013. RAs attempted to pre-screen for eligibility for the ASSIST all adult persons present in the study clinics’ waiting rooms at a selected clinic session before the patients saw their clinicians. Inclusion criteria included: present for a visit for themselves (e.g., not a family member or friend of patient); age 18 or older; spoke English or Spanish. Patients were excluded if they had previously completed the screening for this study. If eligible patients then provided verbal consent, the RA proceeded with interviewer-administered, face-to-face screening questions including age, gender, and pregnancy status. Participation in screening was voluntary and incentives were not provided to the patients.
The patient flow is shown in Figures 1a and 1b. In Tijuana, 96.5% (2,788/2,890) eligible patients completed the ASSIST. In East Los Angeles, 88.8% (2,226/2,507) eligible patients completed the ASSIST. For each city we estimated the additional number that might have been eligible patients but did not complete the screening based on the eligibility rates for known cases (Tijuana: N=96; Los Angeles N=697). Based on these estimates the adjusted response rates were lowered to 93.3% for Tijuana and 69.4% for Los Angeles. The greater reduction for the adjusted rate in Los Angeles is due to the relatively large number of people who declined to give us any screening information (N=1,072).
Figure 1.
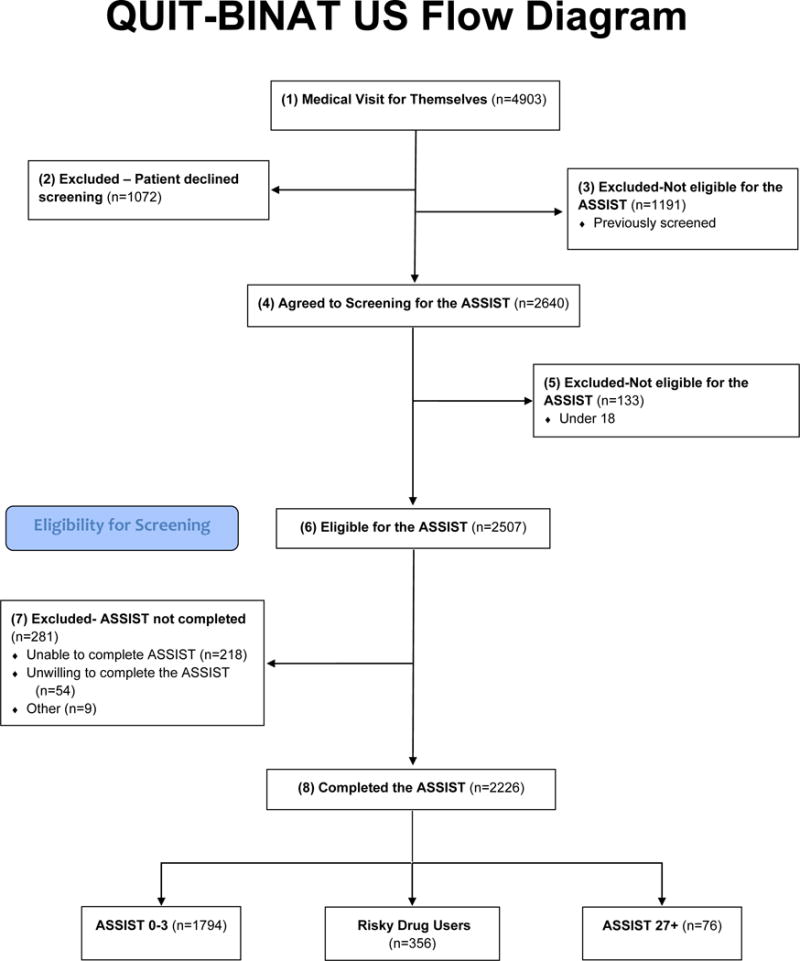
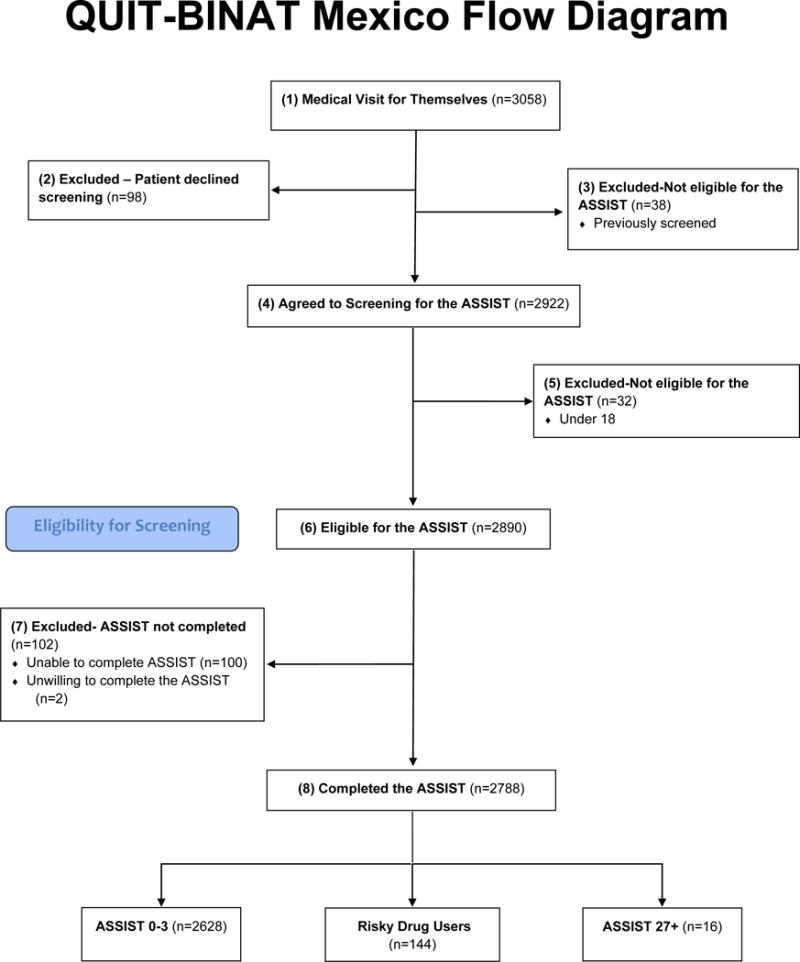
The primary reasons for not completing the ASSIST included: patient refusal to begin or complete the ASSIST although eligible to do so or patients did not have time to complete the ASSIST before being called in from the waiting room to see the clinician. All of the patients in Tijuana completed the ASSIST in Spanish compared to 32.6% of the LA patients. The average time it took patients to complete the ASSIST (starting with the first question on lifetime use, excluding the time it took to read the introductory explanatory text) was higher in Los Angeles (mean 4.2 minutes, SD 6.10) than in Tijuana (mean 1.34 minutes, SD 2.66). Contributing to the shorter ASSIST completion times in Tijuana were the lower prevalence rates of substance use thus limiting the number of questions to be answered compared to East Los Angeles (see Table 1).
Table 1.
Prevalence of drug use among primary care community health center patients, by level of use and city
| DRUG USEa | CITY | |
|---|---|---|
| Los Angeles (n=2226) % |
Tijuana (n=2788) % |
|
| Any drug use | ||
| Lifetime | 44.2*** | 15.1 |
| Past 3 months | 18.5*** | 3.6 |
| Level of drug use | ||
| No or Low useb | 80.6*** | 94.3 |
| Moderate usec | 16.0*** | 5.2 |
| High used | 3.4*** | 0.6 |
| Moderate-to-High Use e | 19.4*** | 5.7 |
| Any injection drug use, lifetime | 3.2* | 1.8 |
| Any injection drug use, past 3 months (%) | 0.8* | 0.3 |
Drug use = use of marijuana, cocaine/crack, methamphetamine and other amphetamines, inhalants, sedatives, hallucinogens, opioids
No or Low Drug Use = ASSIST 0-3 for all drugs
Moderate Drug Use = ASSIST 4-26 for at least one drug, no drug with ASSIST score >=27
High Drug Use = ASSIST >=27 for at least one drug
Moderate-to-High Drug Use = ASSIST 4+ for at least one drug
P<0.05, Chi-square test for differences between cities
P<0.01, Chi-square test for differences between cities
P<0.001, Chi-square test for differences between cities
MEASURES
The WHO Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) was used to identify patients’ risk level of drug, alcohol and tobacco use (Humeniuk et al., 2008; Humeniuk, Dennington, & Ali, 2008; WHO ASSIST Working Group, 2002). The WHO ASSIST was selected because it is brief; designed for use in primary care clinics; is transculturally relevant; and, of particular importance to primary care clinicians, the risk level guides the clinician on whether to administer a brief intervention or evaluate the patient for referral to treatment. The ability of the ASSIST to classify patients based on degree of use has been extensively validated, including the patient self-administered computerized version (Humeniuk, Ali, & WHOAPIS, 2006; Humeniuk et al., 2008; Humeniuk et al., 2008; Humeniuk et al., 2012; WHO ASSIST Working Group, 2002) Based on the ASSIST, patients’ use of each substance category was scored as: no or low use requiring no intervention (score 0-3); moderate use, suggesting clinician brief advice (score 4-26 for drugs and tobacco, 11-26 for alcohol); or high use (at high risk for consequences of drug use) suggesting evaluation and referral for SUD specialty treatment (score 27 and above). Instruments were translated and back-translated and pilot tested for cultural and linguistic sensitivity. Versions of all instruments were subsequently developed in: 1) English, 2) “East Lost Angeles” Spanish, and 3) “Tijuana” Spanish.
Since patients have limited time to complete substance screening in the waiting room before seeing the clinician, time saving and more effective technologies are required. New technologies employing computers have been incorporated into the administration of screening instruments in emergency rooms (Karlsson & Bendtsen, 2005) and primary care settings (Paul et al., 2013). Some have shown increased validity of self-reports of sensitive behaviors through private, self-administered computer-based assessment methods (Moskowitz, 2004). Therefore, we computerized the ASSIST and employed it through patient self-administration on a tablet computer. We employed the same methodology in an earlier study (Baumeister et al., 2014; Gelberg et al., 2015) of risky levels of drug use in Los Angeles clinics and observed the fidelity of the approach.
Patient survey questions were administered on the Electronic Material Management App (EMMA) system, a wireless tablet survey system, utilizing touch screen technology and text-to-speech capability, and providing English and Spanish versions (Singleton et al., 2011). Only a single question and answer set was presented on the tablet screen at one time to simplify the response process for the patient. Consenting patients completed the computerized self-administered touch-screen health-screening questionnaire containing the ASSIST questions and the questions about patient characteristics described in Table 2.
Table 2.
Characteristics of primary care community health center patients screened for drug use with the ASSIST, by city and moderate-to-high level of drug use +.
| CHARACTERISTIC | TOTAL SAMPLE | LOS ANGELES | TIJUANA | Country Comparisons of the Proportion of Moderate-to-High Drug Usea | |||
|---|---|---|---|---|---|---|---|
| Los Angeles | Tijuana | Moderate-to-High Drug Use | Moderate-to-High Drug Use | ||||
| (1) | (2) | (3) | (4) | (5) | (6) | ||
| No | Yes | No | Yes | ||||
| (n=2226) % |
(n=2788) % |
(n=1794) % |
(n=432) % |
(n=2628) % |
(n=160) % |
||
| Gender: | ns | ||||||
|
| |||||||
| Male | 33.0††† | 23.5 | 27.5*** | 55.8 | 21.5*** | 56.3 | |
|
| |||||||
| Female | 67.0 | 76.5 | 72.5 | 44.2 | 78.5 | 43.7 | |
|
| |||||||
| Age Group: | ns | ||||||
| 18-25 | 25.1††† | 21.5 | 24.7** | 26.9 | 20.9*** | 30.6 | |
| 26-34 | 20.9 | 14.3 | 20.2 | 24.1 | 14.0 | 19.4 | |
| 35-45 | 21.1 | 17.9 | 20.5 | 23.6 | 17.5 | 24.4 | |
| 46-65 | 31.4 | 35.1 | 32.9 | 24.8 | 35.7 | 24.4 | |
| >=66 | 1.5 | 11.3 | 1.7 | 0.7 | 11.9 | 1.3 | |
|
| |||||||
| Education (yrs): | *** | ||||||
| 0-6 | 15.2††† | 47.5 | 17.1*** | 7.6 | 48.6*** | 30.0 | |
| 7-9 | 5.7 | 26.9 | 5.7 | 5.6 | 26.4 | 35.6 | |
| >9 | 79.1 | 25.6 | 77.2 | 86.8 | 25.1 | 34.4 | |
|
| |||||||
| Ethnicity: Latino | 92.8 | – | 93.0 | 92.1 | – | – | N/A |
|
| |||||||
| Country of Birth: | N/A | ||||||
| United States | 54.3††† | 0.4 | 48.3*** | 78.9 | 0.4 | 0.6 | |
| Mexico | 37.5 | 99.2 | 42.2 | 17.9 | 99.2 | 99.4 | |
| Other | 8.3 | 0.4 | 9.5 | 3.3 | 0.4 | 0.0 | |
|
| |||||||
| Homeless last night | 2.6††† | 0.3 | 1.8*** | 5.8 | 0.3 | 0.6 | *** |
|
| |||||||
| Pregnant (among women) | 13.7††† | 19.5 | 14.5* | 8.4 | 19.3 | 24.3 | ** |
|
| |||||||
| Chronic Condition: | |||||||
|
| |||||||
| Asthma | 13.8††† | 6.9 | 12.2*** | 20.4 | 6.9 | 7.5 | *** |
|
| |||||||
| Hepatitis | 4.0†† | 2.6 | 2.8*** | 9.3 | 2.4 | 4.4 | ns |
|
| |||||||
| Seizures | 2.9†† | 1.5 | 2.4** | 5.1 | 1.4* | 3.8 | ns |
|
| |||||||
| Cancer | 3.4††† | 1.7 | 3.6 | 2.8 | 1.6 | 2.5 | ns |
|
| |||||||
| Tuberculosis | 3.1 | 2.8 | 3.1 | 3.0 | 2.3*** | 10 | ** |
|
| |||||||
| High Blood Pressure | 28.7††† | 38.3 | 26.8*** | 36.6 | 39.2*** | 23.8 | ** |
|
| |||||||
| Diabetes | 18.7††† | 24.1 | 19. 3 | 16.4 | 24.7** | 15.0 | ns |
|
| |||||||
| HIV/AIDS | 0.8†† | 0.3 | 0.5** | 2.1 | 0.2 | 0.6 | ns |
|
| |||||||
| Any chronic medical condition | 49.4††† | 54.6 | 47.5*** | 57.2 | 55.0 | 48.1 | ns |
N/A: Not applicable
ns: Not significant
Moderate-to-high drug use: ASSIST score >=4 for any of the following: marijuana, cocaine/crack, methamphetamine and other amphetamines, inhalants, sedatives, hallucinogens, opioids
P<0.05,
P<0.01,
P<0.001,
Chi-square tests for difference between cities
P<0.05,
P<0.01,
P<0.001,
ns P>=0.05, Chi-square tests for difference between yes/no moderate-to-high drug use within each city
Country comparisons of demographic characteristics of the proportio of moderate-to-high drug Users in Los Angeles and Tijuana (among the moderate-to-high drug users)
DATA ANALYSIS
The prevalence of different levels of drug use were estimated among patients in each city (LA and Tijuana) (Table 1). We also compared patients from the two cities on demographic characteristics, and compared patients with and without moderate-to-high drug use (ASSIST 4+) in each city and patients with moderate-to-high drug use between cities by means of Chi-square tests for categorical variables and Wilcoxon rank-sum tests for numeric variables (Table 2).
To compare the drug use of Tijuana and Los Angeles patients adjusting for demographic characteristics, multivariate logistic regression models were used (dependent variable 0=not moderate-to-high drug user, 1=moderate-to-high drug user) (Table 3). For these multivariate models, a composite variable was created that combined patient’s clinic city (Tijuana or East Los Angeles) and place of birth (Mexico or United States). Patients were excluded in the following groups because of small numbers: LA patients if they were not born in the US or Mexico; and Tijuana patients if they were not born in Mexico. The model’s goodness-of-fit and the adjustment for nested models were tested. The model controlled for: age, gender, and the composite variable, city–country of birth.
Table 3.
Logistic regressions for moderate-to-high drug useb (ASSIST >=4) among community health center patients
| Variable | Univariate | Multivariatea | Multivariatea (with interaction terms) |
|||
|---|---|---|---|---|---|---|
|
| ||||||
| Column 1 | Column 2 | Column 3 | ||||
|
| ||||||
| N=5,014 | N=4,801 | N=4,801 | ||||
|
| ||||||
| OR | p-value | OR | p-value | OR | p-value | |
| Gender (Male) | 4.02 | <.001 | 4.30 | <.001 | 5.73 | <.001 |
|
| ||||||
| Age | 0.98 | <.001 | 0.98 | <.001 | 0.98 | <.001 |
|
| ||||||
| Education (years) | 1.12 | <.001 | 0.96 | .029 | 1.03 | .136 |
|
| ||||||
| City–Country of Birthc | ||||||
| Tijuana, Mexico born | 1 | 1 | 1 | |||
| LA, Mexico Born | 1.67 | <.001 | 1.64 | .001 | 3.59 | .002 |
| LA, US Born | 6.45 | <.001 | 5.79 | <.001 | 81.67 | <.001 |
|
| ||||||
| Interaction terms: | ||||||
| 1 | ||||||
| Male in LA, Mexico Bornd | 0.96 | .889 | ||||
| Male in LA, US Borne | 0.57 | .009 | ||||
| Education (# years) in LA, Mexico Bornf | 0.91 | <.017 | ||||
| Education (# years) in LA, US Borng | 0.81 | <.001 | ||||
Logistic model included participants with complete responses on the ASSIST who belonged to one of the City-Country of Birth groups included in the table
Dependent variable: having an ASSIST score of 4 or more for at least one drug (moderate-to-high use)
- For LA patients, 8% of patients were excluded for multivariate analyses who were not born in the US or Mexico
- For Tijuana patients, 0.8% of patients were excluded for multivariate analyses who were not born in Mexico
Difference in the effect of being male (ref. female) between patients in LA born in Mexico, and patients in Tijuana
Difference in the effect of being male (ref. female) between patients in LA born in the US, and patients in Tijuana
Difference in the effect of one further year of education between patients in LA born in Mexico, and patients in Tijuana
Difference in the effect of one further year of education between patients in LA born in US, and patients in Tijuana
The final section of the analysis turns to comparisons of the prevalence of moderate to high use of: (1) various drugs (Table 4); (2) combinations of drugs, alcohol and tobacco (Table 4); and (3) combinations of various drugs (poly drug use Table 5).
Table 4.
Prevalence of moderate-to-high usea of drugs, alcohol, and tobacco among primary care community health center patients, by type of substance, and by city
| Substance Used at Moderate-to-High Levela | Los Angeles (n=2226) |
Tijuana (n=2788) |
P value |
|---|---|---|---|
| % | % | ||
| Drugs | 19.4 | 5.7 | *** |
| Marijuana | 12.5 | 4.2 | *** |
| Stimulants: | 7.3 | 3.1 | *** |
| Cocaine/crack | 4.4 | 1.9 | *** |
| Methamphetamine/Amphetamines | 5.7 | 2.4 | *** |
| Inhalants | 1.4 | 0.7 | * |
| Sedatives | 4.6 | 1.5 | *** |
| Hallucinogens | 2.3 | 0.8 | *** |
| Opioids | 4.6 | 1.0 | *** |
| Polydrug use (more than one drug) | 7.6 | 3.1 | *** |
| Alcohol | 15.2 | 6.6 | *** |
| Tobacco | 20.5 | 16.1 | *** |
| Multiple Substances (mutually exclusive groups): | |||
| No substances | 66.0 | 79.7 | *** |
| Drugs only | 6.5 | 1.4 | *** |
| Alcohol only | 4.1 | 2.3 | *** |
| Tobacco only | 7.6 | 10.1 | ** |
| Drugs and alcohol | 2.9 | 0.4 | *** |
| Drugs and tobacco | 4.8 | 2.2 | *** |
| Alcohol and tobacco | 3.0 | 2.2 | |
| Drugs, alcohol, and tobacco | 5.2 | 1.7 | *** |
Moderate-to-High Substance Use: Drugs (ASSIST >=4); Alcohol (ASSIST >=11); Tobacco (ASSIST >=4)
P<0.05, Chi-square test for differences between cities
P<0.01, Chi-square test for differences between cities
P<0.001, Chi-square test for differences between cities
Table 5.
Polydrug use at moderate-to-high levels among community health center patients, by drug type+ and city
| Moderate-to-High Use, Drug Type | CITY | Polydrug-Use (Moderate-to-High Use of Multiple Drugs)a |
|---|---|---|
| % | ||
| Any druga | Los Angeles (n= 432) |
38.9** |
| Tijuana (n= 160 |
54.4 | |
| Marijuana | Los Angeles (n=278) |
46.0** |
| Tijuana (n=117) |
61.5 | |
| Cocaine/crack | Los Angeles (n=97) |
92.8 |
| Tijuana (n=54) |
90.7 | |
| Methamphetamine and other Amphetamines | Los Angeles (n=126) |
73.8 |
| Tijuana (n=67) |
82.1 | |
| Inhalants | Los Angeles (n=31) |
90.3 |
| Tijuana (n=18) |
94.4 | |
| Sedatives | Los Angeles (n=102) |
59.8* |
| Tijuana (n=41) |
80.5 | |
| Hallucinogens | Los Angeles (n=52) |
92.3 |
| Tijuana (n=21) |
100.0 | |
| Opioids | Los Angeles (n=103) |
74.8* |
| Tijuana (n=28) |
92.9 |
Patients who used >1 drug could appear multiple times in the table
Moderate-to-high drug use of at least one other drug (ASSIST >=4)
P<0.05, Chi-square test for categorical variables and Wilcoxon rank-sum tests for continuous variables for differences between cities
P<0.01, Chi-square test for categorical variables and Wilcoxon rank-sum tests for continuous variables for differences between cities
P<0.001, Chi-square test for categorical variables and Wilcoxon rank-sum tests for continuous variables differences between cities
RESULTS
The prevalence of lifetime drug use was much higher in LA (44.2%) than in Tijuana (15.1%) (Table 1). Further, the prevalence of drug use in the past 3 months was higher in LA (18.5%) than Tijuana (3.6%). Levels of drug use according to ASSIST scores were also higher in LA than Tijuana: 16.0% vs. 5.2% for moderate drug users (ASSIST 4-26); 3.4% vs. 0.6% for high drug users (ASSIST 27+); and 19.4% vs. 5.7% for moderate-to-high drug users combined (ASSIST 4+). Lifetime injection drug use was relatively low for patients of both cities, but higher in LA (3.2%) than in Tijuana (1.8%).
Compared to the Tijuana patients, patients in the total LA sample in Table 2 were (column 1 vs. column 2) more likely to be male, younger, and have more years of education. Most LA patients were Latino and nearly 40% were born in Mexico. In Tijuana virtually all patients were born in Mexico. Of 8 possible chronic conditions, LA patients reported having higher rates for five of the conditions but Tijuana patients reported significantly more of the two most prevalent conditions – high blood pressure and diabetes and were more likely to report at least one of the chronic conditions.
We also compared the characteristics of drug users vs. non-users in both countries (Table 2, columns 3 vs. 4 and 5 vs. 6). In both countries, drug users were more likely to be male, younger, and less educated and in LA drug users were more likely than non-users to have been born in the US. However, we found important differences between the two cities as well. In LA, drug users were significantly more likely than non-users to be homeless, not pregnant and to report chronic conditions. In contrast, in Tijuana, drug users were not more likely than non-users to have chronic conditions, or be homeless or pregnant.
Finally, we compared the proportion of all drug users in each country who had particular characteristics (Table 2, column 4 vs. column 6). There were no significant differences in the proportion of drug users between the cities according to gender, age or reporting of any chronic medical condition. However, the proportion of drug users with more education and homeless status was significantly higher in LA than in Tijuana while the proportion of drug users that were pregnant was higher in Tijuana.
Table 3 shows the results of logistic models predicting moderate-to-high drug use (ASSIST 4+), combining the samples from the two cities. In the univariate models (column 1), place of birth was very important. LA patients born in Mexico had nearly twice the odds of being drug users as Tijuana patients, and LA patients born in the US had almost 6 times the odds of being drug users compared to those in Tijuana. Also, males, younger and better educated patients were significantly more likely to be drug users.
In the multivariate model (Table 3, column 2), examining the effects of each independent variable adjusted for all of the others, the results were quite similar with one important exception. The OR for education changed from 1.12 in the univariate model to 0.96 in the multivariate model. This suggests that an additional year of education adjusted for gender, age and city-county of birth actually decreased rather than increased the odds that a patient will be a drug user. In the final multivariate model with interactions (column 3), significant interactions were observed between gender and city-country of birth, and between years of education and city-country of birth. The effect of being male on the odds of being a drug user was significantly higher in Tijuana than among those in LA who were born in the US (p=.009). Also, one further year of education decreased the odds of being a user for patients in LA (Mexico born p=<.017; US born p=<.001) compared to patients in Tijuana.
Table 4 shows that for all types of substances (drugs, alcohol, and tobacco), the prevalence of moderate-to-high use was higher in LA than in Tijuana. In both cities, the most frequently used drugs in the moderate-to-high range were marijuana and stimulants. In LA, the prevalence of moderate-to-high drug use (19.4%) was intermediate between those of alcohol (15.2%) and tobacco (20.5%). In Tijuana, the prevalence of moderate-to-high drug use (5.7%) was only a bit lower than the rates for alcohol (6.6%) and greatly lower than rates for tobacco (16.1%).
Table 4 shows that moderate-to-high drug users in both cities were also likely to also be moderate-to-high alcohol and/or tobacco users. In LA, of 432 patients who were moderate-to-high drug users, two-thirds were poly-substance users: 15.0% were users of both drugs and alcohol at this level, 24.8% users of both drugs and tobacco, and 26.9% were users of all three substances. In Tijuana, of 160 moderate-to-high drug users, 75.0% were poly-substance users: 7.5% were users of both drugs and alcohol, 38.8% users of both drugs and tobacco, and 28.9% were users of all three substances.
Table 5 shows LA patients were twice as likely as Tijuana patients to have polydrug use (7.6% vs. 3.1%). However, among moderate-to-high drug using patients, higher polydrug use rates were found in Tijuana vs. LA (54.4% vs. 38.9%). In both cities nearly all patients who used cocaine/crack, inhalants, and hallucinogens used another drug at moderate-to-high levels, as were most opiate users in Tijuana. Tijuana patients who used marijuana, sedatives, and opiates were more likely to use additional drugs than were patients who used these drugs in LA.
DISCUSSION
To our knowledge, this is the first published paper to compare rates of drug use in primary care patients of CHCs in cities close to the borders of the two countries. Our four key study findings are as follows:
First, rates of drug use were much higher in LA than in Tijuana patients (moderate-to-high drug use was 19% in LA vs. 6% in Tijuana). This was despite the largely Latino ethnic similarity of patients of the East Los Angeles and Tijuana clinics. Drug use rates were especially high for patients born in the US who had 6 times the odds of having moderate-to-high drug use as compared to Tijuana patients born in Mexico; however, higher rates were also found in LA patients born in Mexico who had nearly 2 times the odds of Tijuana patients of using drugs. Thus, Mexico country of birth, a proxy measure of less acculturation in the US, was associated with lower drug use rates.
The differences found in this study are consistent with those reported in other studies, which have identified higher substance use in the U.S. household population than in Mexico. They point out that Mexico-United States migration and acculturation play a key role in drug use (Borges, Medina-Mora, Breslau, & Aguilar-Gaxiola, 2007; Lebrun-Harris et al., 2014; Borges et al., 2009; Borges et al., 2011; Borges et al., 2012; Borges et al., 2015; Cherpitel et al., 2015; Guerrero et al., 2014b). Migration is associated with high stress and exposure to drug-using environments (Dillon, De La Rosa, Sanchez, & Schwartz, 2012; Dillon et al., 2012). Migrants may have higher alcohol and drug use due to social isolation and the stress to which they are subjected to by living far away from the place where they grew up and have their roots (Alegria et al., 2007; Garcia, 2007; Garcia, 2007). Disconnection with their local communities, and separation from their families may predispose Mexican migrants to increase the quantity and frequency of alcohol and illicit drug use or to resume drug use (Ojeda et al., 2009). An environment/cultural effect may exist in rates of drug use among our study’s mostly Latino patient populations, which must be taken into consideration in designing interventions and programs for drug use screening, brief intervention, and prevention. Further research is necessary to determine what cultural factors make the migrant population adopt more similar drug use patterns to those of Americans than those of the country of origin.
Furthermore, clinics in each of the different cities have to worry about different subgroups of drug using patients. In Tijuana drug users were more likely to be pregnant women, less educated, less troubled by homeless status, and more likely to report some chronic conditions (high blood pressure, diabetes) and less likely to report others (hepatitis, cancer, HIV). These findings suggest that interventions to address moderate-to-high drug use may need to be adapted for different subgroups of patients in the two cities, such as low-literacy interventions for less educated males in Tijuana, and interventions that are tailored to the unique needs of homeless patients in LA.
Second, rates of recent moderate-to-high drug use among primary care patients of both countries were high compared to findings from household surveys. Cherpitiel and Ye (2008), found that people who abuse substances were more likely to use emergency and primary health care services than a specialized SUD treatment center, meaning that the user population may be over-represented in community health center settings, compared with the general population, although they do not necessarily visit them for drug-related problems. Community health centers are therefore important sites for identifying those with substance use problems.
Compared to household surveys (SAMHSA, 2013), the rates for drug use in our clinic patient population were higher. In Los Angeles, 45% of primary care patients had used drugs in their lifetime and 19% had used drugs in the past 3 months. While these rates were similar to US general population lifetime use rates (50.5% lifetime use), the rates were much higher than US past month use rates (9.1%), and higher than LA past year use rates (15.4%) (SAMHSA, 2012). In Tijuana, 15% of our study patients had used drugs at least once during their lifetime and 4% had used drugs in the past three months, these figures were considerably higher than those recorded in household surveys. In the northwest region of Mexico (which includes the city of Tijuana and the state of Baja California), 2.9% used drugs in the past year, with marijuana and cocaine being the most commonly used drugs (INPRFM, INSP & SS, 2012). Prevalence of lifetime drug use identified in this study among community health center patients was over twice the rates found in the household survey (the National Survey of Addictions): 15% vs. 7% respectively (Villatoro et al., 2012). Drug use over the past three months in our community health center patients was also considerably higher than use in the past year in the same household survey (3.6% vs 1.8%) (INPRFM, INSP & SS, 2012). We should note that these household data include the population under 18. Given that the drug use rates are higher in our clinic patient population, CHC settings are crucial for the detection, brief intervention and referral of drug use cases. The drugs most commonly used in both cities were marijuana and stimulants (combining cocaine and amphetamines).
Compared to other primary care populations, in the US, the prevalence of moderate-to-high use we found in our CHC patients was higher than rates found in some prior studies (Lebrun-Harris et al., 2014; Lee et al., 2011); similar to rates found in our prior study based on the ASSIST in CHCs in LA; but lower than rates of other studies (Gelberg et al., 2015; Gryczynski et al., 2014; McNeely et al., 2014; Roy-Byrne et al., 2014), perhaps due to differences in the recruitment strategy, sample, definition of drug use, and characteristics of the selected health centers. Nationally, the ASSIST has been used in studies for measuring drug use, but the prevalence rates were not reported from these studies (Saitz et al., 2010; McNeely et al., 2014). Similar contrasts are not available for Mexico since primary care settings have not been studied prior to this.
Third, among moderate-to-high drug users in both countries, polydrug use and polysubstance use was the norm. The majority of moderate-to-high drug users in both countries also used alcohol or tobacco at such risky levels. And, more than one-third of moderate-to-high drug users in LA and more than half in Tijuana also used more than one drug at moderate-to-high levels. Our results suggest that for both countries, clinic-based brief interventions to address drug use might not be able to focus on one drug at a time or on one type of substance at a time, but rather might need to develop strategies to simultaneously address behavior change for multiple drugs and multiple substances (Hall & Prochaska, 2009; Prochaska, Hall, Delucchi, & Hall, 2014).
Fourth, it is possible to conduct patient self-administered screening for substance use utilizing the WHO ASSIST on tablet computers in English and in Spanish in both LA and Tijuana among low-income, primary care patients. Among eligible patients, there were high rates of completion of the ASSIST in both countries. However, when we adjusted the completion rates for those who declined to screen for the ASSIST, the estimated completion rate remains almost the same in Tijuana but drops in East LA. The explanation may lie in hypotheses of a cultural nature. In Mexico, persons may tend to respond positively to survey requests; for example, the last National Addiction Survey had a response rate of 92% for the North West region of Mexico (INPRFM, INSP & SS, 2012). Receiving services at a low fee clinic might lead them to think that answering the survey is part of their obligations and that they are showing their commitment to the institution by agreeing to answer. In the U.S., patients may feel freer to decline to participate in surveys and/or they may be hesitant to participate due to fear of disclosing information related to immigration status. The 2012 National Survey on Drug Use and Health: Summary of National Findings reported a weighted response rate of 73.0% (SAMHSA, 2013), which is comparable to the adjusted response rate found in LA (69.4%) for this study. Further, in LA, seeking agreement to provide screening information was sought by research assistants from UCLA. If permission were sought by persons identified as clinic personnel, the completion rate might have been higher. These hypotheses require future testing.
In our prior work, we also checked for underreporting of drug use and generally found acceptable sensitivity comparing computerized patient reporting on the ASSIST to results of urine drug testing (Gelberg et al., 2015). A recent study also found high test-retest reliability of the patient self-administered computerized version of the ASSIST (McNeely et al., 2014). In general, the patient self-administered computerized screening strategies, adopted in our study are accepted by and easy to use for patients, even for those with different levels of educational attainment (Hahn et al., 2004; Hahn, Choi, Griffith, Yost, & Baker, 2011).
The self-administered version of the WHO ASSIST is a reliable tool that can be used with the Mexican and American populations. We believe that it would not require much modification for it to be applied along the border in “twin” cities. The need for alcohol and drug screening in primary care settings is supported by this study. This study contributes a model that could be used in other parts of the US and Mexico for identifying substance use rates among patients in primary care settings along the border.
Although the two countries have different health systems, they share the problem of drug use. This early detection study also provides some guidance regarding how we should tailor prevention programs on either side of the border (what sort of drug we should orient treatment towards in each country, for example). In any case, for related problems, there should be similar programs for people who cross the borders and may use both country’s health services, which would encourage access to screening and continuity of care.
Additional key study findings were as follows. About half of the drug using patients of both cities had a co-morbid chronic medical condition, suggesting that primary care clinicians will need to address drug use in the context of managing their chronic medical problems. Moderate-to-high drug users’ ages most commonly ranged from age 18 to 64 in both cities, decades of life requiring high productivity, indicating the need to develop programs for these age groups. For both cities combined, male patients had 6 times the odds of being drug users than were female patients, suggesting that primary care clinicians should especially focus on not missing the opportunity to identify and treat drug use among men who have sought ambulatory care since they are generally less likely than women to do so (National Center for Health Statistics, 2013).
The results reveal the influence of the environment in shaping patterns of use. Further research is necessary to determine what cultural factors make the Mexican migrant population adopt drug use patterns more similar to those born in the US, than to those of the country of origin. And it is important to identify key risk and protective factors for drug use in both the US and Mexico, so that the countries can shore up public policies in both border regions. From the perspective of health services provided in Mexico, it is essential to have programs for the early detection of drug use, particularly given the current migration patterns, since recent years have seen a significant increase in return migration from the US to Mexico (Consejo Nacional de Población, 2014).
LIMITATIONS
Study limitations included the following. 1) Self-Report Bias – rates of substance use and other variables were based on patient self-reports. While additional research is needed regarding the extent of under-reporting of drug use by community clinic patients, we did find in a prior study of patients in Los Angeles clinics that the extent of underreporting was limited for most drugs when compared to findings from urine drug testing (Gelberg et al., 2015). 2) Representativeness of participants and clinics sampled - however refusal rates for ASSIST screening within the sampled clinics were comparable to national surveys on drug use for each country (INPRFM, INSP & SS, 2012; SAMSHA, 2013). 3) Generalizability - to other clinics and health care settings in LA and Tijuana and to other cities in the US and Mexico. Future research comparing Los Angeles and Mexico patients’ rates of drug, alcohol, and tobacco use in other types of CHC settings, ambulatory settings, and other medical settings is indicated.
CONCLUSIONS
Rates of drug use are higher than expected in low-income patients of the safety net CHCs in cities close to the US-Mexico border in Los Angeles and Tijuana, and comparable to rates of alcohol use. Routine screening for drug use, along with alcohol and tobacco use, should be integrated into the regular practice of CHCs. Using the patient self-administered ASSIST on touchscreen tablets serves as a feasible model for screening patients for substance use in busy CHCs. This initial study provides evidence to inform future research regarding the usefulness of drug screening in primary care settings and for comparing the results of this screening model in health centers in pairs of sister metropolitan areas at the U.S. - Mexico border. The usefulness of designing policies that promote the implementation of a drug use screening test, which is quick to use and reliable among the population that attends primary care clinics for the timely detection of at-risk drug users has been supported by our findings.
Acknowledgments
Special thank you to Dr. Hendricks Brown and Juan Villamar from the Center for Prevention Implementation Methodology (Ce-PIM) NIDA P30 DA027828. We also appreciate the participation of the National Council Against Addictions (Mexico) through Dr. Mario González Zavala. We are indebted to Dr. Abdolmonem Afifi, Dean Emeritus, UCLA School of Public Health, Professor of Biostatistics & Biomathematics for his careful review and comments on the logistic regression analyses used in this paper.
ROLE OF FUNDING SOURCES
The “US Binational Quit Using Drugs Intervention trial” (3P30DA027828-02S1, 3P30DA027828-02S2) was supported in U.S. by NIDA and the US Office of National Drug Control Policy. In Mexico, funding was received from the US State Department Narcotics Affairs Section (NAS) (SMX53012-GR186). The study was supported in part by Northwestern University’s Center for Prevention Implementation Methodology (Ce-PIM) for Drug Abuse and Sexual Risk Behavior (3P30DA027827), an NIH-funded program, which is supported by the following NIH Institutes: NIDA and OBSSR.
Footnotes
CONTRIBUTORS
All authors contributed to and have approved the final manuscript.
DECLARATION OF INTEREST:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Reference List
- Abou-Saleh MT. Substance use disorders: Recent advances in treatment and models of care. J Psychosom Res. 2006;61(3):305–310. doi: 10.1016/j.jpsychores.2006.06.013. doi:S0022-3999(06)00301-1 [pii];10.1016/j.jpsychores.2006.06.013. [DOI] [PubMed] [Google Scholar]
- Agerwala SM, McCance-Katz EF. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: a brief review. J Psychoactive Drugs. 2012;44(4):307–317. doi: 10.1080/02791072.2012.720169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, et al. Understanding differences in past year psychiatric disorders for Latinos living in the US. Soc Sci Med. 2007;65(2):214–230. doi: 10.1016/j.socscimed.2007.03.026. doi: S0277-9536(07)00141-4 [pii];10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Kadden RM. Screening and interventions for alcohol and drug problems in medical settings: what works? J Trauma. 2005;59(3 Suppl):S80–S87. doi: 10.1097/01.ta.0000174664.88603.21. doi:00005373-200509001-00021 [pii] [DOI] [PubMed] [Google Scholar]
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28(3):7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Baumeister SE, Gelberg L, Leake BD, Yacenda-Murphy J, Vahidi M, Andersen RM. Effect of a primary care based brief intervention trial among risky drug users on health-related quality of life. Drug Alcohol Depend. 2014;142:254–261. doi: 10.1016/j.drugalcdep.2014.06.034. doi: S0376-8716(14)00961-2 [pii];10.1016/j.drugalcdep.2014.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Breslau J, Orozco R, Tancredi DJ, Anderson H, Aguilar-Gaxiola S, et al. A cross-national study on Mexico-US migration, substance use and substance use disorders. Drug Alcohol Depend. 2011;117(1):16–23. doi: 10.1016/j.drugalcdep.2010.12.022. doi: S0376-8716(11)00045-7 [pii];10.1016/j.drugalcdep.2010.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Cherpitel CJ, Orozco R, Zemore SE, Wallisch L, Medina-Mora ME, et al. Substance Use and Cumulative Exposure to American Society: Findings From Both Sides of the US-Mexico Border Region. Am J Public Health. 2016;106(1):119–127. doi: 10.2105/AJPH.2015.302871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Medina-Mora ME, Breslau J, Aguilar-Gaxiola S. The effect of migration to the United States on substance use disorders among returned Mexican migrants and families of migrants. Am J Public Health. 2007;97(10):1847–1851. doi: 10.2105/AJPH.2006.097915. doi: AJPH.2006.097915 [pii];10.2105/AJPH.2006.097915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Medina-Mora ME, Orozco R, Fleiz C, Cherpitel C, Breslau J. The Mexican migration to the United States and substance use in northern Mexico. Addiction. 2009;104(4):603–611. doi: 10.1111/j.1360-0443.2008.02491.x. doi: ADD2491 [pii];10.1111/j.1360-0443.2008.02491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Rafful C, Benjet C, Tancredi DJ, Saito N, Aguilar-Gaxiola S, et al. Mexican immigration to the US and alcohol and drug use opportunities: does it make a difference in alcohol and/or drug use? Drug Alcohol Depend. 2012;125(Suppl 1):S4–11. doi: 10.1016/j.drugalcdep.2012.05.007. doi: S0376-8716(12)00170-6 [pii];10.1016/j.drugalcdep.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Zemore S, Orozco R, Cherpitel CJ, Ye Y, Bond J, et al. Co-Occurrence of Alcohol, Drug Use, DSM-5 Alcohol Use Disorder, and Symptoms of Drug Use Disorder on Both Sides of the U.S.-Mexico Border. Alcohol Clin Exp Res. 2015;39(4):679–687. doi: 10.1111/acer.12672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Office of Statewide Health Planning and Development (OSHPD) Healthcare Information Division: Annual Utilization Report of Primary Care Clinics. U.S.: OSHPD; 2013. (State of California- 2013). [Google Scholar]
- Cherpitel CJ, Ye Y. Drug use and problem drinking associated with primary care and emergency room utilization in the US general population: data from the 2005 national alcohol survey. Drug Alcohol Depend. 2008;97(3):226–230. doi: 10.1016/j.drugalcdep.2008.03.033. doi: S0376-8716(08)00143-9 [pii];10.1016/j.drugalcdep.2008.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Bond J, Zemore SE, Borges G, Greenfield TK. Border effects on DSM-5 alcohol use disorders on both sides of the U.S.-Mexico border. Drug Alcohol Depend. 2015;148:172–179. doi: 10.1016/j.drugalcdep.2015.01.003. doi: S0376-8716(15)00008-3 [pii];10.1016/j.drugalcdep.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chittoor G, Arya R, Farook VS, David R, Puppala S, Resendez RG, et al. Epidemiologic investigation of tuberculosis in a Mexican population from Chihuahua State, Mexico: a pilot study. Tuberculosis (Edinb) 2013;93(Suppl):S71–S77. doi: 10.1016/S1472-9792(13)70014-3. doi: S1472-9792(13)70014-3 [pii];10.1016/S1472-9792(13)70014-3. [DOI] [PubMed] [Google Scholar]
- Consejo Nacional de Población. 20 años de la Encuesta sobre Migración en la frontera Norte de México. México: Consejo Nacional de Población; 2014. Available from: http://www.conapo.gob.mx/work/models/CONAPO/Resource/2460/2/images/EMIF_20.pdf (accessed 13 October 2015) [Google Scholar]
- Cook B, Alegria M, Lin JY, Guo J. Pathways and correlates connecting Latinos’ mental health with exposure to the United States. Am J Public Health. 2009;99(12):2247–2254. doi: 10.2105/AJPH.2008.137091. doi: AJPH.2008.137091 [pii];10.2105/AJPH.2008.137091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon FR, De La Rosa M, Sanchez M, Schwartz SJ. Preimmigration Family Cohesion and Drug/Alcohol Abuse Among Recent Latino Immigrants. Fam J Alex Va. 2012;20(3) doi: 10.1177/1066480712448860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia V. Meeting a binational research challenge: substance abuse among transnational Mexican farmworkers in the United States. J Rural Health. 2007;23(Suppl):61–67. doi: 10.1111/j.1748-0361.2007.00125.x. doi: JRH125 [pii];10.1111/j.1748-0361.2007.00125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelberg L, Andersen RM, Afifi AA, Leake BD, Arangua L, Vahidi M, et al. Project QUIT (Quit Using Drugs Intervention Trial): a randomized controlled trial of a primary care-based multi-component brief intervention to reduce risky drug use. Addiction. 2015;110(11):1777–1790. doi: 10.1111/add.12993. Retrieved from PM:26471159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein MG, Whitlock EP, DePue J. Multiple behavioral risk factor interventions in primary care. Summary of research evidence. Am J Prev Med. 2004;27(2 Suppl):61–79. doi: 10.1016/j.amepre.2004.04.023. S0749379704001035 [pii] [DOI] [PubMed] [Google Scholar]
- Gryczynski J, Mitchell SG, Gonzales A, Moseley A, Peterson TR, Ondersma SJ, et al. A randomized trial of computerized vs. in-person brief intervention for illicit drug use in primary care: Outcomes through 12months. J Subst Abuse Treat. 2014 doi: 10.1016/j.jsat.2014.09.002. doi: S0740-5472(14)00193-7 [pii];10.1016/j.jsat.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Villatoro JA, Kong Y, Gamino MB, Vega WA, Mora ME. Mexicans’ use of illicit drugs in an era of drug reform: National comparative analysis by migrant status. Int J Drug Policy. 2014a doi: 10.1016/j.drugpo.2014.04.006. doi: S0955-3959(14)00082-6 [pii];10.1016/j.drugpo.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Villatoro JA, Kong Y, Gamino MB, Vega WA, Mora ME. Mexicans’ use of illicit drugs in an era of drug reform: National comparative analysis by migrant status. Int J Drug Policy. 2014b doi: 10.1016/j.drugpo.2014.04.006. doi: S0955-3959(14)00082-6 [pii];10.1016/j.drugpo.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn EA, Cella D, Dobrez D, Shiomoto G, Marcus E, Taylor SG, et al. The talking touchscreen: a new approach to outcomes assessment in low literacy. Psychooncology. 2004;13(2):86–95. doi: 10.1002/pon.719. [DOI] [PubMed] [Google Scholar]
- Hahn EA, Choi SW, Griffith JW, Yost KJ, Baker DW. Health literacy assessment using talking touchscreen technology (Health LiTT): a new item response theory-based measure of health literacy. J Health Commun. 2011;16(Suppl 3):150–162. doi: 10.1080/10810730.2011.605434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall SM, Prochaska JJ. Treatment of smokers with co-occurring disorders: emphasis on integration in mental health and addiction treatment settings. Annu Rev Clin Psychol. 2009;5:409–431. doi: 10.1146/annurev.clinpsy.032408.153614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration [HRSA] Find a Health Center US Department of Health and Human Services. U.S.: Health Resources and Services Administration; 2016. Available from: http://findahealthcenter.hrsa.gov/Search_HCC.aspx (accessed 12 Mayo 2015) [Google Scholar]
- Humeniuk R, Ali R, WHOAPIS . Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and pilot brief intervention. Geneva: World Health Organization; 2006. A technical report of phase II findings of the WHO ASSIST Project. [Google Scholar]
- Humeniuk R, Ali R, Babor T, Souza-Formigoni ML, de Lacerda RB, Ling W, et al. A randomized controlled trial of a brief intervention for illicit drugs linked to the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in clients recruited from primary health-care settings in four countries. Addiction. 2012;107(5):957–966. doi: 10.1111/j.1360-0443.2011.03740.x. Retrieved from PM:22126102. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, et al. Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST) Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. doi: ADD2114 [pii];10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Dennington V, Ali R. The effectiveness of a brief intervention for illicit drugs linked to the alcohol, smoking and substance involvement screening test (ASSIST) in primary health care settings A technical report of phase III findings of the WHO ASSIST randomized controlled trial. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- Humphreys K, McLellan AT. Brief Intervention, Treatment, and Recovery Support Services for Americans Who Have Substance Use Disorders: An Overview of Policy in the Obama Administration. Psychological Services. 2010;7:275–284. [Google Scholar]
- Instituto Nacional de Psiquiatría Ramón de la Fuente. Encuestas de Ciudades y Estatales 2005. México: Instituto Nacional de Psiquiatría Ramón de la Fuente; 2006. [Google Scholar]
- Instituto Nacional de Psiquiatría Ramón de la Fuente (INPRFM), Instituto Nacional de Salud Pública (INSP), & Secretaría de Salud (SS) Reporte de Drogas. México, D.F.: Instituto Nacional de Psiquiatría Ramón de la Fuente; Instituto Nacional de Salud Pública; Secretaría de Salud; 2012. Encuesta Nacional de Adiccione 2011. [Google Scholar]
- Karlsson A, Bendtsen P. Acceptability of a computerized alcohol screening and advice routine in an emergency department setting–a patient perspective. Addict Behav. 2005;30(4):767–776. doi: 10.1016/j.addbeh.2004.08.022. doi: S0306-4603(04)00300-4 [pii];10.1016/j.addbeh.2004.08.022. [DOI] [PubMed] [Google Scholar]
- Lebrun-Harris LA, Tomoyasu N, Ngo-Metzger Q. Substance use, risk of dependence, counseling and treatment among adult health center patients. J Health Care Poor Underserved. 2014;25(3):1217–1230. doi: 10.1353/hpu.2014.0130. doi: S1548686914300200 [pii];10.1353/hpu.2014.0130. [DOI] [PubMed] [Google Scholar]
- Lee JD, Delbanco B, Wu E, Gourevitch MN. Substance use prevalence and screening instrument comparisons in urban primary care. Subst Abus. 2011;32(3):128–134. doi: 10.1080/08897077.2011.562732. doi: 933889875 [pii];10.1080/08897077.2011.562732. [DOI] [PubMed] [Google Scholar]
- Los Angeles County Department of Public Health. Key Indicators of Health by Service Planning Area. U.S.: Office of Health Assessment and Epidemiology; 2009. [Google Scholar]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1–3):280–295. doi: 10.1016/j.drugalcdep.2008.08.003. doi: S0376-8716(08)00310-4 [pii];10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDougal L, Strathdee SA, Rangel G, Martinez G, Vera A, Sirotin N, et al. Adverse pregnancy outcomes and sexual violence among female sex workers who inject drugs on the United States-Mexico border. Violence Vict. 2013;28(3):496–512. doi: 10.1891/0886-6708.11-00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Strauss SM, Wright S, Rotrosen J, Khan R, Lee JD, et al. Test-retest reliability of a self-administered alcohol, smoking and substance involvement screening test (ASSIST) in primary care patients. J Subst Abuse Treat. 2014a;47(1):93–101. doi: 10.1016/j.jsat.2014.01.007. doi: S0740-5472(14)00025-7 [pii];10.1016/j.jsat.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Strauss SM, Wright S, Rotrosen J, Khan R, Lee JD, et al. Test-retest reliability of a self-administered Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in primary care patients. J Subst Abuse Treat. 2014b;47(1):93–101. doi: 10.1016/j.jsat.2014.01.007. doi: S0740-5472(14)00025-7 [pii];10.1016/j.jsat.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- Moskowitz JM. Assessment of Cigarette Smoking and Smoking Susceptibility among Youth: Telephone Computer-Assisted Self-Interviews versus Computer-Assisted Telephone Interviews. The Public Opinion Quarterly. 2004;68(4):565–587. doi: 10.2307/3521619. [DOI] [Google Scholar]
- Office of National Drug Control Policy. 9th US-Mexico Binational Conference on Drug Demand Reduction. Mexico, D.F.: 2011. [Google Scholar]
- Ojeda VD, Strathdee SA, Lozada R, Rusch ML, Fraga M, Orozovich P, et al. Associations between migrant status and sexually transmitted infections among female sex workers in Tijuana, Mexico. Sex Transm Infect. 2009;85(6):420–426. doi: 10.1136/sti.2008.032979. doi: sti.2008.032979 [pii];10.1136/sti.2008.032979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization of American States. Drug Problem in the Americas. Washington, DC: Organization of American States; 2013. [Google Scholar]
- Pan American Health Organization. United States-Mexico Border Area. Washington, DC: Pan-American Health Organization; 2014. [Google Scholar]
- Paul CL, Carey M, Yoong SL, D’Este C, Makeham M, Henskens F. Access to chronic disease care in general practice: the acceptability of implementing systematic waiting-room screening using computer-based patient-reported risk status. Br J Gen Pract. 2013;63(614):e620–e626. doi: 10.3399/bjgp13X671605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perreira KM, Gotman N, Isasi CR, Arguelles W, Castaneda SF, Daviglus ML, et al. Mental Health and Exposure to the United States: Key Correlates from the Hispanic Community Health Study of Latinos. J Nerv Ment Dis. 2015;203(9):670–678. doi: 10.1097/NMD.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst Abuse Rehabil. 2012;3(1):25–34. doi: 10.2147/SAR.S30057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitpitan EV, Wagner KD, Goodman-Meza D, Semple SJ, Chavarin C, Strathdee SA, et al. Context matters: the moderating role of bar context in the association between substance use during sex and condom use among male clients of female sex workers in Tijuana, Mexico. AIDS Behav. 2013;17(8):2577–2587. doi: 10.1007/s10461-013-0491-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Hall SE, Delucchi K, Hall SM. Efficacy of initiating tobacco dependence treatment in inpatient psychiatry: a randomized controlled trial. Am J Public Health. 2014;104(8):1557–1565. doi: 10.2105/AJPH.2013.301403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy-Byrne P, Bumgardner K, Krupski A, Dunn C, Ries R, Donovan D, et al. Brief intervention for problem drug use in safety-net primary care settings: a randomized clinical trial. JAMA. 2014;312(5):492–501. doi: 10.1001/jama.2014.7860. doi: 1892249 [pii];10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Alford DP, Bernstein J, Cheng DM, Samet J, Palfai T. Screening and brief intervention for unhealthy drug use in primary care settings: randomized clinical trials are needed. J Addict Med. 2010;4(3):123–130. doi: 10.1097/ADM.0b013e3181db6b67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, et al. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA. 2014;312(5):502–513. doi: 10.1001/jama.2014.7862. doi: 1892250 [pii];10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez-Huesca R, Arellanez-Hernández JL, Pérez-Islas V, Rodríguez-Kuri S. Estudio de la relación entre consumo de drogas y migración a la Frontera Norte de México y Estados Unidos. Salud Mental. 2006;26(1):35–43. [Google Scholar]
- Secretaria de Salud del Estado de Baja California. Ubicaciones de los centros de salud, hospitales y unidades. 2015 Available from: http://www.saludbc.gob.mx/?page_id=365 (accessed 17 October 2015)
- Servin AE, Strathdee S, Munoz FA, Vera A, Rangel G, Silverman JG. Vulnerabilities faced by the children of sex workers in two Mexico-US border cities: a retrospective study on sexual violence, substance use and HIV risk. AIDS Care. 2015;27(1):1–5. doi: 10.1080/09540121.2014.946384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro B, Coffa D, McCance-Katz EF. A primary care approach to substance misuse. Am Fam Physician. 2013;88(2):113–121. doi:d10437 [pii] [PubMed] [Google Scholar]
- Singleton KW, Lan M, Arnold C, Vahidi M, Arangua L, Gelberg L, et al. Wireless data collection of self-administered surveys using tablet computers. AMIA Annu Symp Proc. 2011;2011:1261–1269. [PMC free article] [PubMed] [Google Scholar]
- Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170(13):1155–1160. doi: 10.1001/archinternmed.2010.140. doi: 170/13/1155 [pii];10.1001/archinternmed.2010.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Center for Behavioral Health Statistics and Quality. 2005–2010 National Surveys on Drug Use and Health Substance Use and Mental Disorders in Selected Metropolitan Statistical Areas (MSAs), Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. (Behavioral Health Measures for Los Angeles-Long Beach-Santa Ana MSA). [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. U.S.: Substance Abuse and Mental Health Services Administration (SAMHSA); 2013. [Google Scholar]
- United Nations Office on Drugs and Crime. World Drug Report 2015. Vienna: United Nations Office on Drugs and Crime; 2015. Available from: http://www.unodc.org/documents/wdr2015/World_Drug_Report_2015.pdf (accessed 15th November 2015) [Google Scholar]
- Villatoro JA, Medina-Mora ME, Fleiz C, Moreno M, Robles NO, Bustos M, et al. El consumo de drogas en México: Resultados de la Encuesta Nacional de Adicciones, 2011. Salud Mental. 2012;35(6):447–457. [Google Scholar]
- WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x. doi:185 [pii] [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global Health Risks Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009. [Google Scholar]
- World Health Organization. Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings Mental Health Gap Action Programme (mhGAP) Geneva: World Health Organization; 2011. [PubMed] [Google Scholar]
- Zhang X, Martinez-Donate AP, Nobles J, Hovell MF, Rangel MG, Rhoads NM. Substance Use Across Different Phases of the Migration Process: A Survey of Mexican Migrants Flows. J Immigr Minor Health. 2015 doi: 10.1007/s10903-014-0109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


