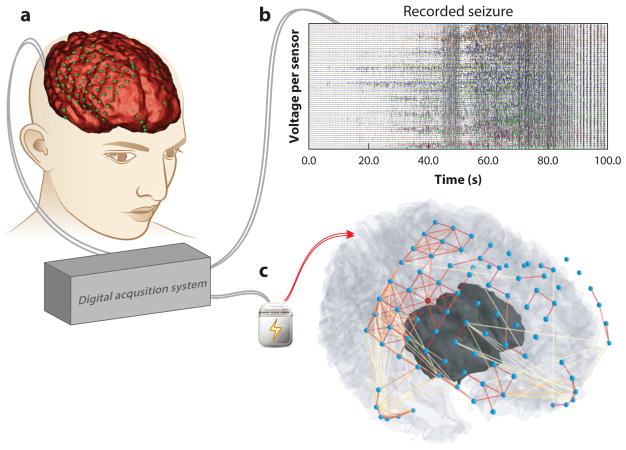
Figure 6.
Clinical translation of network neuroscience tools. Network neuroscience offers a natural framework for improving tools to diagnose and treat brain network disorders. (a) For drug-resistant epilepsy patients, invasive monitoring of brain activity to localize brain tissue where seizures originate and to plan resective surgery is challenging, because the neural processes generating seizures are poorly understood. Epileptic brain signals, electrical fields produced by the firing of neuron populations, are sensed by electrodes that rest on the surface of the brain, beneath the dura, and are recorded by a digital acquisition system. Shown is a three-dimensional reconstruction of a patient’s brain (red ) with electrodes colocalized ( green) to anatomical features. (b) Recorded brain signals are studied by clinical practitioners to characterize spatial and temporal behavior of the patient’s seizure activity. Each line represents a time-varying voltage fluctuation from each electrode sensor. (c) Inferred functional connections from a single time slice during the patient’s recorded seizure demonstrates rich relationships in neural dynamics between brain regions and are not visually evident in panel b (nodes, blue; strong connections, red links; weak connections, yellow links). Functional connectivity patterns demonstrate strong interactions around the brain regions in which seizures begin and weak projections to the brain regions in which seizures spread. Objective tools in network neuroscience can usher in an era of personalized algorithms capable of mapping epileptic network architecture from neural signals and pinpointing implantable neurostimulation devices to specific brain regions for intervention (79, 80, 192).