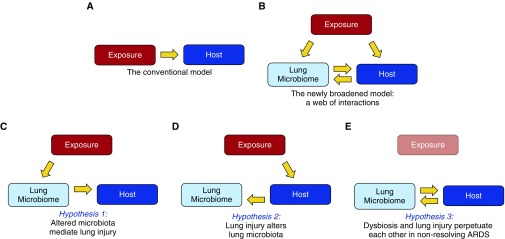
Figure 1.
Broadening our model of acute respiratory distress syndrome (ARDS) pathogenesis. (A) In our conventional understanding of ARDS pathogenesis, a direct or indirect exposure (such as sepsis, pneumonia, or trauma) mediates alveolar inflammation and injury within the host. (B) The discovery of the lung microbiome, and its disruption in ARDS, has broadened our model of pathogenesis, creating a web of associations with undetermined causal relationships. This complexity can be reduced to three key hypotheses. (C) Hypothesis 1: some exposures (such as sepsis [9], hyperoxia, and aspiration) directly alter lung microbiota, mediating alveolar inflammation and injury. (D) Hypothesis 2: lung injury alters the respiratory ecosystem, selectively favoring the outgrowth of select lung bacteria (14, 15). (E) Hypothesis 3: Once lung dysbiosis and lung injury are established, they perpetuate each other, prolonging ARDS even after the provoking exposure is gone (e.g., influenza). Longitudinal human studies, interventional studies with pre- and postintervention sampling, and complementary animal models will be required to test and refine each hypothesis.