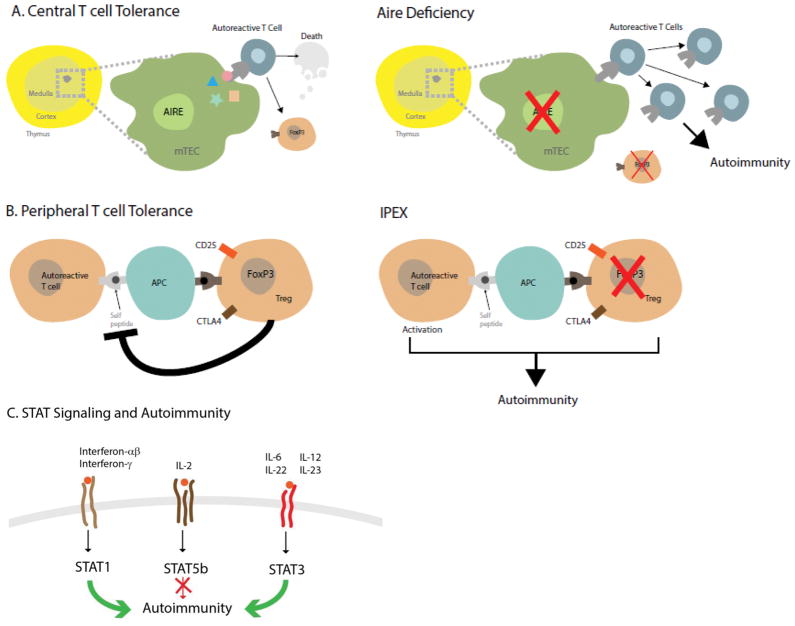
Figure 2. Key Immunoregulatory Pathways Involved in the Pathogenesis of Autoimmune Polyendocrine Syndromes.
Panel A, left illustrates normal central immune tolerance. The autoimmune regulator (AIRE) expressed in medullary thymic epithelial cells (mTEC) promotes expression of tissue-specific antigens (colored star, rectangle, triangle, and circle) which are expressed on the surface. Autoreactive T cells with affinity for self-proteins either die by apoptosis or become forkhead box P3 (FoxP3) expressing T regulatory cells (Tregs). When AIRE is lacking (right panel), autoreactive T cells escape to the general circulation and peripheral lymphoid organs where they can cause autoimmune reactions and the disease APS-1. Lack of Tregs also contribute to autoimmunity. Panel B, left depicts how FoxP3 positive Tregs harness autoreactive T cells by interacting with antigen presenting cells (APCs). FoxP3 mutations (right panel) or mutations in other genes key to the function of Tregs (cytotoxic T lymphocyte antigen 4 (CTLA4), cluster of differentiation 25 (CD25)) remove the inhibition of autoreactive T cells which then cause autoimmunity and immune polyendocrinopathy X-linked (IPEX) and IPEX-like syndromes. Panel C, Signal transducers and activators of transcription (STATs) are transducers of cell surface cytokine signaling (family members depicted at the cell surface). Mutations that lead to a constitutively active form of STAT1 or STAT3 promote autoimmunity (green arrows); loss of function mutations in STAT5b also lead to autoimmunity (red arrow with block). The exact mechanisms need to be further dissected but loss of STAT5b could be due to the improper expression of FOXP3, a known target of STAT5b.