Graphical abstract
Keywords: Composites, Dental materials, Dietary solvents, Flexural properties, Giomers
Abstract
Objective
This study investigated the effect of dietary solvents on flexural strength and modulus of bulk-fill composites.
Materials and methods
One conventional composite (Filtek Z350 [FZ]), two bulk-fill composites (Filtek Bulk-fill [FB] and Tetric N Ceram [TN]) and a bulk-fill giomer (Beautifil-Bulk Restorative [BB]) were evaluated. Specimens (12 × 2 × 2 mm) were fabricated using customized stainless steel molds. Specimens were light-cured, removed from their molds, finished, measured and randomly divided into six groups. The groups (n = 10) were conditioned in the following mediums for 7 days at 37 °C: air (control), artificial saliva (SAGF), distilled water, 0.02 N citric acid, heptane, 50% ethanol–water solution. After conditioning, the specimens were rinsed, blotted dry, measured and subjected to flexural testing using a universal testing machine. Representative SEM images of the intact surfaces were obtained to appraise the degradation mechanism by dietary solvents. Data was subjected to statistical analysis using ANOVA/Tukey’s tests at significance level p < 0.05.
Results
Significant differences in flexural properties were observed between materials and conditioning mediums. The highest flexural properties were usually obtained with conditioning in air (control) or heptane. Exposure to aqueous solutions generally reduced flexural properties of bulk-fill composites.
Conclusion
The effect of dietary solvents on flexural properties of bulk-fill composites was material and medium dependent.
1. Introduction
Dental composite technology had progressed significantly over the past decade (Leprince et al., 2013, Shah and Stansbury, 2014). Despite this, polymerization shrinkage and depth of cure remain a clinical challenge (Deliperi and Bardwell, 2002, Jang et al., 2015, Park et al., 2008). The incremental layering technique had traditionally been used to reduce polymerization shrinkage stresses and to facilitate curing light penetration. Besides being time-consuming to perform, air entrapment, contamination and bond failure can also occur between layers (Jang et al., 2015, Park et al., 2008). Bulk-fill composites were introduced to overcome the need for composite layering and adapting procedures. They allow for the placement of materials in 4–5 mm increments without increasing shrinkage and compromising cure (Jang et al., 2015). The latter is achieved by means of novel resins, special modulators, unique fillers and filler control (Fleming et al., 2008, Lassila et al., 2012, Yap et al., 2016). The mechanical properties of bulk-fill composites have been the subject of some disagreement. While some authors have reported lower mechanical properties than conventional highly-filled composites, others have stated otherwise (El Gezawi et al., 2016, Ilie et al., 2013, Leprince et al., 2014).
Composite restorations are subjected to both physical and chemical degradation intra-orally. In addition to dissolution and softening of the resin matrix, filler damage and de-bonding can also occur ensuing in decreased restoration durability and longevity (Drummond, 2008, Wu et al., 1984). Food simulating liquids (FSLs) are usually used to mimic dietary solvents. They are often used for accelerated aging and testing of dental composites (Krishnan and Yamuna, 1998, Vouvoudi and Sideridou, 2012). Commonly employed FSLs include those listed in the Food and Drug Administration (USA) guidelines (Food and Drug Administration, 1976). Heptane imitates greasy foods like vegetable oils, butter and fatty meats, while citric acid and ethanol solutions mimic certain vegetables, fruits, candies, beverages including alcohol and syrups. Distilled water and artificial saliva are used to replicate the wet oral environment presented by water and saliva (Akova et al., 2006, Vouvoudi and Sideridou, 2012, Yap et al., 2005, Yap et al., 2000b).
FSLs have been found to affect the strength of dental composites in in-vitro studies. Whilst conditioning in ethanol generally weakens dental composites (Krishnan and Yamuna, 1998, Yesilyurt et al., 2009), exposure to heptane was equivocal with authors reporting both increased and decreased strength (Akova et al., 2006, Yap et al., 2000b). These studies were all conducted on conventional materials and few, if any, had determined the impact of food substances on the strength of bulk-fill composites. The latter is clinical meaningful as bulk-fill composites may behave differently from their conventional counterparts considering the variances in filler and resin technology.
The aim of this study was to determine the effect of dietary solvents on flexural strength and modulus of bulk-fill composites. The performance of these materials after conditioning in the various dietary solvents was also compared. The null hypotheses were as follows: (a) Flexural properties of bulk-fill composites are not affected by dietary solvents and (b) Irrespective of conditioning mediums, no significant disparity in flexural properties exists between bulk-fill materials.
2. Materials and methods
2.1. Materials and specimen preparation
The materials evaluated and their technical profiles are presented in Table 1. They included a conventional composite (Filtek Z350 [FZ]), two bulk-fill composites (Filtek Bulk-Fill [FB] and Tetric N ceram Bulk-Fill [TN]) and a bulk-fill giomer (Beautifil Bulk-fill Restorative [BB]). The conventional composite served as a comparison for the bulk-fill materials.
Table 1.
Technical profiles and manufacturers of the materials evaluated.
| Material (Abbreviation) | Manufacturer | Type | Resin | Filler | Filler content % by weight/% by volume |
Lot no. |
|---|---|---|---|---|---|---|
| Filtek Z350 (FZ) [control] |
3 M ESPE, St Paul, MN, USA | Nanohybrid restorative | Bis-GMA Bis-EMA UDMA TEGDMA |
Zirconia/Silica cluster and Silica nanoparticle |
78.5/63.3 | N771467 |
| Filtek Bulk-Fill (FB) |
3 M ESPE, St Paul, MN, USA | Bulk-fill restorative | AUDMA AFM DDDMA UDMA |
Zirconia/Silica cluster, ytterbium trifluoride | 76.5/58.4 | N693019 |
| Tetric N ceram Bulk-Fill (TN) |
Ivoclar, Vivadent Inc., NY, USA | Bulk-fill restorative | Bis-GMA Bis-EMA UDMA |
Barium glass filler, ytterbium fluoride and spherical mixed oxide | 77/55 | S38368 |
| Beautifil-Bulk Restorative (BB) |
SHOFU Inc., Koyoto, Japan | Bulk-fill giomer restorative | Bis-GMA UDMA Bis-MPEPP TEGDMA |
S-PRG based on F-Br-Al-Si glass | 87/74.5 | 051623 |
AUDMA = Aromatic urethane dimethacrylate.
AFM = Addition-fragmentaion monomers.
Bis-EMA = Ethoxylated bisphenol-A-glycidyl methacrylate.
Bis-GMA = Bisphenol-A glycidyl methacrylate.
Bis-MPEPP = Bisphenol-A polyethoxy-dimethacrylate.
DDDMA = 1,12-dodecanediol dimethacrylate.
F-Br-Al-Si = Fluoroboroaluminosiliciate.
S-PRG = Surface modified pre-reacted glass.
TEGDMA = Triethylene glycol dimethacrylate.
UDMA = Urethane dimethacrylate.
*(Abbreviation) depicts the code for study materials.
Sixty beam-shaped specimens (12 × 2 × 2 mm) of each material were fabricated using customized stainless steel molds. The composites were placed in one increment and excess material was removed by compressing the molds between two mylar strips with glass slides. The top surface of the composite specimens were light polymerized with two overlapping irradiation of 10 s each using a LED curing light (Demi Plus, Kerr, CA, USA) with a wave length of 450–470 nm and irradiance of 1330 mW/cm2. The glass slides were removed and the composite specimens were light cured for another 10 s. The mylar strips were subsequently discarded and the composite beams were removed from their molds. Any minor material excess or ‘fins’ were gently removed by fine polishing discs (Sof-Lex, 3M ESPE, USA). The composite specimens were examined for the presence of voids or cracks and any defective specimens were replaced. The final dimensions of the specimens and the parallelism between their opposite surfaces were verified with a digital caliper (Mitutoyo Corporation, Kawaski, Japan).
2.2. Storage mediums and time
The composite specimens were then randomly divided into six groups (n = 10) and conditioned in the following mediums for 7 days at 37 °C: air (control), artificial saliva (SAGF), distilled water, 0.02 N citric acid, heptane, 50% ethanol-water solution. Specimens were kept in sealed containers to minimize evaporation. Composition of artificial saliva (SAGF) used is shown in Table 2 (Gal et al., 2001). The pH of the artificial saliva was adjusted to 6.8 to take after natural saliva when it is released from the salivary ducts (Vouvoudi and Sideridou, 2012).
Table 2.
Composition of the SAGF medium (Gal et al., 2001).
| Components | Concentration (mg L−1) |
|---|---|
| NaCl | 125.6 |
| KCl | 963.9 |
| KSCN | 189.2 |
| KH2PO4 | 654.5 |
| Urea | 200.0 |
| NaSO4·10H2O | 763.2 |
| NH4Cl | 178.0 |
| CaCl2·2H2O | 227.8 |
| NaHCO3 | 630.8 |
2.3. Flexural testing
A three point bending test setup was used to assess the flexural properties of the composites after conditioning in the various mediums. Specimens were rinsed, blotted dry and measured prior to testing. Measurements were taken at two places for length, width and height, and the average of both values was taken to calculate the flexural strength and flexural modulus. The composite specimens were loaded in a universal testing machine (UTM) (Shimadzu Corporation, Kyoto, Japan) with a load cell of 5 KN and crosshead speed of 0.5 mm/min until fracture occurred. Flexural strength, σ, in Megapascals (MPa) was calculated using the following equation:
| (1) |
where
P is the maximum load, in newtons, exerted on the specimens;
L is the distance, in millimeters, between the supports (10 mm);
B is the width, in millimeters, of the specimens measured prior to testing;
H is the height, in millimeters, of the specimens measured prior to testing.
Flexural modulus, E′, in Megapascals (MPa) was calculated using the following equation:
| (2) |
where F/D is the slope, in newtons per millimeter, measured in the straight-line portion of the load-deflection graph. L, B and H had been defined in the flexural strength equation. Flexural modulus was computed and subsequently converted to Gigapascal (GPa).
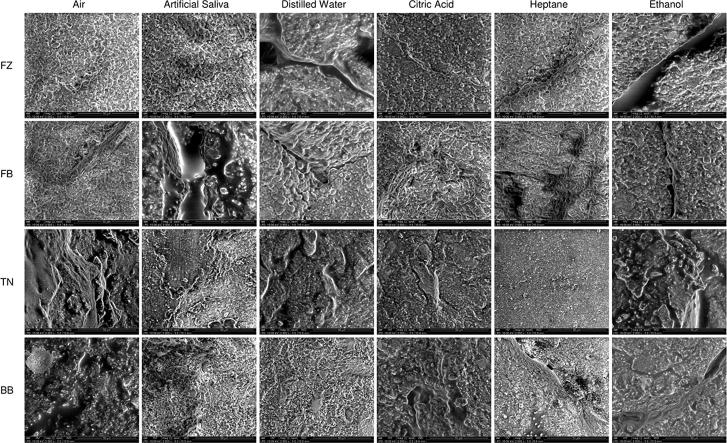
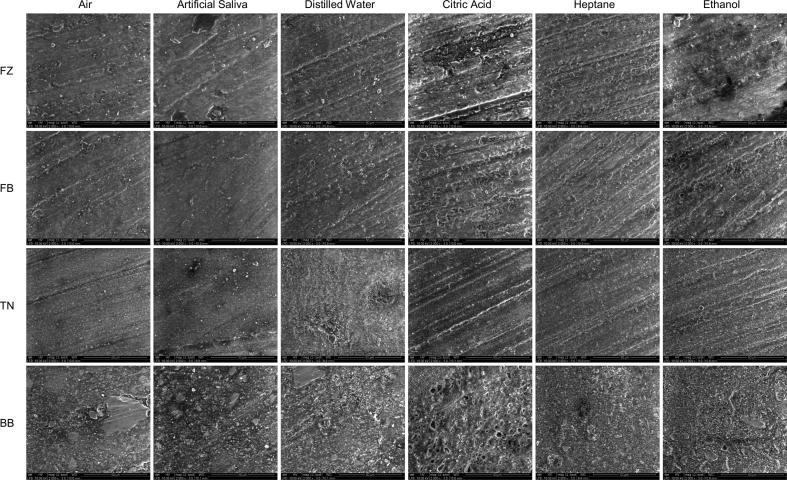
2.4. SEM evaluation
The upper intact surfaces of representative specimens were examined with scanning electron microscopy (SEM) after flexural testing to appraise the degradation mechanisms of the FSLs. Specimens were mounted, gold coated and examined using a FEI Quanta, 250 FEG SEM (Eindhoven, Netherlands) with an accelerating voltage of 10 KV and a working distance of 10 mm at 2000× magnification.
2.5. Statistical analysis
SPSS statistical program (Version 12.0.1, SPSS Inc., Chicago, USA) was used to analyze the data. Normality testing was done using Shapiro-Wilk test. As the test showed normal data distribution, parametric analysis was permissible. Homogeneity of variance was assessed using Levene’s test and equal variances were assumed. The interactions between the independent variables (materials and conditioning mediums) and each of the dependent variables (flexural strength and flexural modulus) were evaluated using two-way ANOVA. One way ANOVA and Tukey’s post hoc tests were then used to determine inter-medium and inter-material differences for flexural strength and modulus. Pearson’s correlation between flexural strength and modulus was conducted at significance level of 0.01. With the exception of correlation, all statistical analyses were carried out at significance level 0.05.
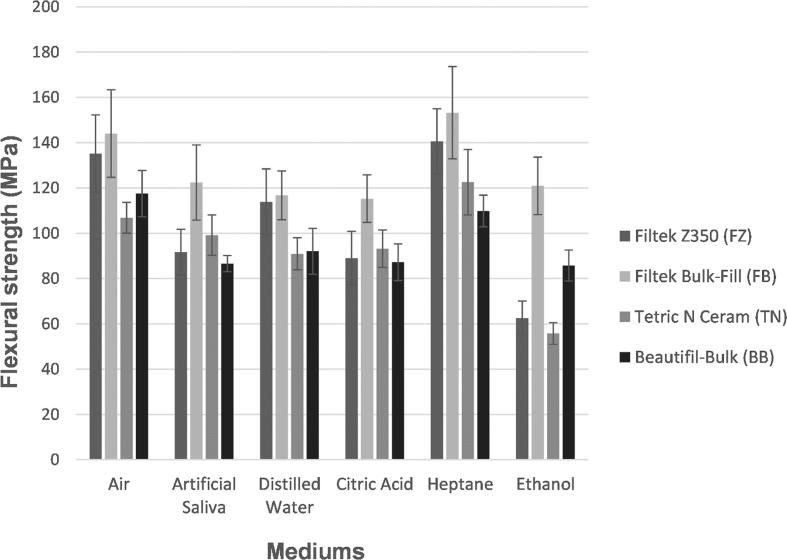
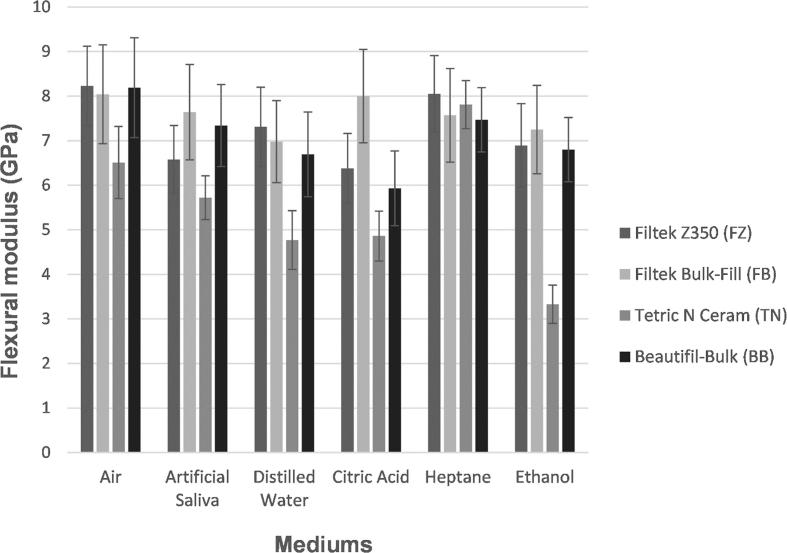
3. Results
Mean flexural strength and modulus for the various materials after conditioning in the different mediums are reflected in Table 3. Fig. 1, Fig. 2 compare the mean flexural strength and modulus of the materials when grouped according to mediums. Results of statistical analysis based on materials are presented in Table 4 whereas enquiry centered on conditioning mediums are shown in Table 5. Two-way ANOVA revealed significant interactions (p < 0.001) between materials and mediums for both flexural strength and modulus. The effects of dietary solvents were therefore material and medium dependent. Correlation between flexural strength and modulus was significant and positive with a correlation coefficient of r = 0.56.
Table 3.
Mean flexural strength (MPa) and modulus (GPa) for the various restorative materials with standard deviations (in parentheses).
| Material/ Medium | Filtek Z350 (FZ) |
Filtek Bulk-Fill (FB) |
Tetric N Ceram (TN) |
Beautifil-Bulk (BB) |
||||
|---|---|---|---|---|---|---|---|---|
| Flexural strength (MPa) | Flexural modulus (GPa) | Flexural strength (MPa) | Flexural modulus (GPa) | Flexural strength (MPa) | Flexural modulus (GPa) | Flexural strength (MPa) | Flexural modulus (GPa) | |
| Air (Control) |
135.20 (17.08) |
8.23 (0.89) |
144.00 (19.32) |
8.04 (1.11) |
106.85 (6.80) |
6.51 (0.81) |
117.53 (10.22) |
8.19 (1.12) |
| Artificial saliva | 91.71 (10.10) |
6.58 (0.76) |
122.39 (16.63) |
7.64 (1.07) |
99.17 (8.89) |
5.72 (0.49) |
86.6 (3.57) |
7.34 (0.92) |
| Distilled water | 113.86 (14.60) |
7.31 (0.89) |
116.75 (10.73) |
6.98 (0.92) |
90.95 (7.06) |
4.77 (0.66) |
92.06 (10.11) |
6.69 (0.95) |
| Citric acid | 89.03 (11.84) |
6.38 (0.78) |
115.26 (10.51) |
8.00 (1.05) |
93.20 (8.23) |
4.86 (0.56) |
87.23 (8.06) |
5.93 (0.84) |
| Heptane | 140.60 (14.43) |
8.05 (0.86) |
153.21 (20.37) |
7.57 (1.05) |
122.55 (14.47) |
7.81 (0.54) |
109.86 (7.03) |
7.47 (0.72) |
| Ethanol | 62.50 (7.56) |
6.89 (0.94) |
120.94 (12.75) |
7.25 (0.99) |
55.77 (4.78) |
3.33 (0.43) |
85.76 (6.86) |
6.80 (0.72) |
Fig. 1.
Mean flexural strength values (MPa) after storage in the different conditioning mediums.
Fig. 2.
Mean flexural modulus values E′ (GPa) after storage in the different conditioning mediums.
Table 4.
Results of statistical analysis for flexural strength and flexural modulus based on materials.a
| Properties | Material | Differences |
|---|---|---|
| Flexural strength | FZ | Heptane, Air (control) > Water > Saliva, Citric acid > Ethanol |
| FB | Heptane, Air (control) > Saliva, Ethanol, Water, Citric acid | |
| TN | Heptane > Air (control), Saliva, Citric acid, Water > Ethanol | |
| Air (control) > Citric acid, Water | ||
| BB | Air (control), Heptane > Water, Citric acid, Saliva, Ethanol | |
| Flexural modulus | FZ | Air (control), Heptane > Ethanol, Saliva, Citric acid |
| FB | No significant difference | |
| TN | Heptane > Air (control) > Saliva > Citric acid, Water > Ethanol | |
| BB | Air (control) > Ethanol, Water, Citric acid | |
| Heptane, Saliva > Citric acid | ||
Abbreviations: FZ, Filtek Z350; FB, Filtek Bulk-Fill; TN, Tetric N Ceram; BB, Beautifil-Bulk.
Results of One way ANOVA and Post Hoc’s Tukey’s test (p < 0.05); > indicates statistical significance.
Table 5.
Results of statistical analysis for flexural strength and flexural modulus based on conditioning mediums.a
| Mediums | Differences |
|
|---|---|---|
| Flexural strength | Flexural modulus | |
| Air | FB, FZ > BB, TN | FZ, BB, FB > TN |
| Artificial saliva | FB > TN, FZ, BB | FB > FZ, TN |
| BB > TN | ||
| Distilled water | FB, FZ > BB, TN | FZ, FB, BB > TN |
| Citric acid | FB > TN, FZ, BB | FB > FZ, BB > TN |
| Heptane | FB, FZ > TN, BB | No significant difference |
| Ethanol 50% | FB > BB, FZ, TN | FB, FZ, BB > TN |
| BB > FZ, TN | ||
Abbreviations: FZ, Filtek Z350; FB, Filtek Bulk-Fill; TN, Tetric N Ceram; BB, Beautifil-Bulk.
Results of One way ANOVA and Post Hoc’s Tukey’s test (p < 0.05); > indicates statistical significance.
With the exception of BB, the highest flexural strength was obtained after conditioning in heptane. For BB, the highest flexural strength was observed with conditioning in air. Flexural strength of FZ, FB and BB after exposure to air and heptane was significantly greater than all other mediums. For TN, flexural strength after conditioning in heptane was significantly higher than the other mediums. Furthermore, flexural strength when stored in air was significantly greater than in citric acid, distilled water and ethanol. Apart from FB, the lowest flexural strength was noted after exposure to ethanol. FB showed the lowest flexural strength after conditioning in citric acid.
For all mediums, FB had the highest flexural strength (Fig. 1). When conditioned in air, distilled water and ethanol, TN had the lowest flexural strength. For artificial saliva, citric acid and heptane, BB was the weakest material. When conditioned in air, distilled water and heptane, FB and FZ was significantly stronger than BB and TN. For the other mediums, FB had significantly higher flexural strength than the other three composites. Conditioning in ethanol also showed BB to be significantly stronger than FZ and TN.
No significant difference in flexural modulus was observed between mediums for FB. Highest flexural modulus was observed after conditioning in air for FZ and BB whereas for TN, heptane showed the highest flexural modulus. The lowest flexural modulus was noted after conditioning in citric acid for FZ and BB while for TN, ethanol presented the lowest flexural modulus. For FZ, conditioning in air and heptane gave significantly higher flexural modulus than all other mediums with the exception of distilled water. There was, however, no significant difference between ethanol, artificial saliva and citric acid. For TN, exposure to ethanol resulted in significantly lower modulus than all other mediums. Flexural modulus of BB after conditioning in citric acid was significantly lower than in air, heptane and artificial saliva.
No significant difference in flexural modulus was observed between materials when conditioned in heptane. When conditioned in air, distilled water and heptane, FZ had the highest flexural modulus. For artificial saliva, citric acid and ethanol, the largest flexural modulus was observed for FB. With the exception of heptane, TN showed the lowest flexural modulus in all mediums (Fig. 2). When exposed to heptane, BB has the lowest flexural modulus. Flexural modulus of TN was significantly lower than all other materials when conditioned in air, distilled water, citric acid and ethanol. As for artificial saliva, TN was significantly less rigid than FB and BB whereas FB was significantly stiffer than FZ and TN. There was no significant difference in flexural modulus between FZ, FB and BB when conditioned in air, distilled water and ethanol. For citric acid, FB was significantly more rigid than all other materials.
The consolidated SEM images are shown in Fig. 3. After conditioning in air and heptane, the surfaces of the materials remained relatively undamaged. When exposed to the different aqueous solutions (i.e. artificial saliva, distilled water, citric acid and ethanol) varying degrees of resin matrix dissolution, filler exposure and dislodgement were observed. With the exception of FB, the degradation outcomes were largely more prominent with ethanol.
Fig. 3.
SEM images of the intact surfaces of specimens after conditioning in the various dietary solvents.
4. Discussion
This study investigated the effect of dietary solvents on flexural strength and modulus of bulk-fill composites. As flexural properties were both material and conditioning medium dependent, the null hypotheses were rejected. The composite materials were conditioned continuously in the various FSLs for 7 days at 37 °C prior to flexural testing. This exposure duration might be considered somewhat long since restorations usually come into contact with foods and liquids for only a short time and sporadically in vivo. Results may possibly embellish the effects of food substances and liquids in vivo. Continuous exposure can occur in vivo since chemicals are absorbed by adherent debris (such as calculus or food particles) at the margins or grooves of restorations (Akova et al., 2006, Yap et al., 2000b). Correlation between flexural strength and flexural modulus was significant and positive (r = 0.56). An increase in flexural strength was thus associated with increased stiffness.
Flexural testing plays an important role in characterizing dental composites and allows for the determination of both flexural strength and modulus (International Organization for Standardization, 2000). While flexural strength signifies the highest stress experienced by the composites before they fail, flexural modulus represents their stiffness. Flexural testing results in complex tensions stemming from the integration of compression, shear and tensile stresses (dos Santos et al., 2012). Different clinical situations necessitates the use of composites with dissimilar flexural strength and modulus (Anusavice, 2003, Rodrigues et al., 2007, Yap et al., 2002). In Class I, II, III and IV cavities, composites should have high flexural strength and modulus to minimize fracture and deformation under occlusal loading. For Class V cavities, composites with low flexural modulus are more desirable since they can flex with the teeth when occlusally loaded, decreasing stresses along the adhesive interface and probability of debonding (Pontes et al., 2013, Yap et al., 2002).
ISO 4049 flexural test specimens are typically 25 mm long (International Organization for Standardization, 2000). These elongated composite specimens are technically challenging to fabricate and require the use of several overlapping light irradiation owing to the relatively smaller light exit windows of most curing tips (dos Santos et al., 2012). As the mesio-distal widths of molars are usually around 11 mm, the ISO recommended length is also not really clinically appropriate. The use of mini-flexural test specimens (12 mm × 2 mm × 2 mm) had been validated by Yap and Teoh (2003). Significant and positive correlations for flexural strength and modulus were observed between the mini- and ISO flexural tests. Besides being more clinically relevant, the mini-flexural test specimens have the merit of decreased fabrication time and material usage.
According to the ISO standards, composite materials should have a minimum flexural strength of 80 MPa (International Organization for Standardization, 2000). With the exception of FZ and TN after conditioning in ethanol, all composites evaluated achieved higher flexural strengths irrespective of conditioning mediums. For all composites, conditioning in heptane and air (control) imparted significantly higher flexural strengths than the other mediums. Findings were consistent with SEM observations corroborated those of Yap et al. based on ISO flexural specimens (Yap et al., 2000b). Heptane, a water insoluble hydrocarbon, may possibly inhibit silica and the other fillers from leaching out. This also explains the higher flexural strength of specimens conditioned in air when compared to those in aqueous solutions (Yap et al., 2000a). Conversely, Akova and co-workers reported decreased flexural strength and hardness after conditioning in heptane (Akova et al., 2006). Their study was, however, conducted on bis-acryl resin provisional materials and not on composite resins. With the exception of the bulk-fill giomer BB, the flexural strength of all composites was higher when conditioned in heptane than in air. Appraisal of the fractured specimens was also carried out with SEM but was uneventful and did not reveal any specific modes of failure between materials and mediums.
Apart from FB, conditioning in ethanol generally resulted in the lowest flexural strength. All the composites evaluated were BisGMA-based with the exception of FB. Since ethanol has a solubility index that is similar to that of BisGMA, it increases dental composite disintegration (El-Safty et al., 2012). This was evidenced by the resin matrix dissolution, filler exposure and degradation observed with SEM after conditioning in ethanol. The lower susceptibility of FB to degradation by ethanol can be attributed to its use of monomers other than BisGMA. FB is based on urethane dimethacrylate (UDMA) and also contained aromatic urethane dimethacrylate (AUDMA) and addition fragmentation monomers (AFM) for moderating stiffness of its polymer matrix. This may also explain the higher flexural strength of FB in all mediums when compared to the other materials including the conventional composite FZ. The flexural strength of FZ was significantly higher than the other bulk-fill composites when conditioned in air, distilled water and heptane. Leprince and co-workers also reported lower flexural properties of most bulk-fill composites when compared to highly filled conventional ones and cautioned against the use of bulk-fill composites for restorations under high occlusal load (Leprince et al., 2014). Nonetheless, no significant difference in flexural properties was generally observed between conventional and bulk-fill materials when conditioned in ethanol, citric acid and artificial saliva. Findings reinforce the need for more material and medium specific mechanical evaluations before definitive conclusions can be made.
When conditioned in heptane, no significant difference in flexural modulus was observed between materials. The lowest modulus was observed after exposure to ethanol for TN and citric acid for FZ and BB. The decrease in rigidity of TN can again be explained by the softening effect of ethanol on the resin matrix. Weak intraoral acids such as citric acid have been found to damage the inorganic fillers in composites (Akova et al., 2006). The giomer bulk-fill composite BB may be particularly prone owing to the susceptibility of their ‘pre-reacted’ fluorosilicate glass fillers to acid degradation (Kooi et al., 2012). Dietary habits of patients must therefore be considered during composite selection to enhance restoration longevity. The flexural modulus of TN was generally the lowest regardless of mediums. This can be attributed to its relatively lower filler volume (55% versus 58.4–74.5%) when compared to the other composites. Results supported that of El-Safty and co-workers who found a significant positive correlation between modulus and filler loading (El-Safty et al., 2012). No significant difference in flexural modulus was observed between conditioning mediums for FB. The rigidity of FB was thus impartial to conditioning mediums.
There were some limitations with our study. Firstly, the conditioning period was only 7 days and may be extended to determine the longer term effects of dietary solvents on flexural properties (Krishnan and Yamuna, 1998, Vouvoudi and Sideridou, 2012). Since dental composites are visco-elastic in nature, the static flexural tests performed cannot provide much information on material structure. Dynamic testing could be conducted to determine both elastic and viscous properties of the composites. Dynamic mechanical analysis can be implemented using wide variations of frequencies, displacements and temperatures to simulate the range of forces and temperatures in vivo (Jacobsen and Darr, 1997). Unlike the current static test, dynamic testing is non-destructive and allows for the re-testing of specimens over extended time periods.
5. Conclusion
Within the confines of the current study, the effect of dietary solvents on flexural strength and modulus of bulk-fill composites were both material and medium dependent. The highest flexural properties were usually obtained with conditioning in air (control) or heptane. Exposure to aqueous solutions including artificial saliva generally reduced flexural properties of bulk-fill composites. With the exception of the UDMA-based bulk-fill composite (FB), ethanol significantly reduced the flexural properties of BisGMA-based conventional and bulk-fill composites. Dietary habits of patients must be taken into consideration when selecting composites for stress-bearing restorations.
Conflict of interests
None.
Acknowledgements
This work was supported by research grant (PG320-2016A) Faculty of Dentistry, University of Malaya. The authors would like to thank 3M-EPSE, Shofu Asia and Ivoclar Vivadent Inc. for their material support.
Footnotes
Peer review under responsibility of King Saud University.
References
- Akova T., Ozkomur A., Uysal H. Effect of food-simulating liquids on the mechanical properties of provisional restorative materials. Dent. Mater. 2006;22:1130–1134. doi: 10.1016/j.dental.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Anusavice K.J. Mechanical properties of dental materials. In: Anusavice K.J., Phillips R.W., editors. Phillip’s Science of Dental Materials. Saunders; 2003. pp. 73–101. [Google Scholar]
- Deliperi S., Bardwell D.N. An alternative method to reduce polymerization shrinkage in direct posterior composite restorations. J. Am. Dent. Assoc. 2002;133:1387–1398. doi: 10.14219/jada.archive.2002.0055. [DOI] [PubMed] [Google Scholar]
- dos Santos S.G., Moyses M.R., Alcantara C.E.P., Ribeiro J.C.R., Ribeiro J.G.R. Flexural strength of a composite resin light cured with different exposure modes and immersed in ethanol or distilled water media. J. Conserv. Dent. 2012;15:333–336. doi: 10.4103/0972-0707.101891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond J.L. Degradation, fatigue, and failure of resin dental composite materials. J. Dent. Res. 2008;87:710–719. doi: 10.1177/154405910808700802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Safty S., Akhtar R., Silikas N., Watts D.C. Nanomechanical properties of dental resin-composites. Dent. Mater. 2012;28:1292–1300. doi: 10.1016/j.dental.2012.09.007. [DOI] [PubMed] [Google Scholar]
- El Gezawi M., Kaisarly D., Al-Saleh H., ArRejaie A., Al-Harbi F., Kunzelmann K. Degradation potential of bulk versus incrementally applied and indirect composites: color, microhardness, and surface deterioration. Oper. Dent. 2016;41:195–208. doi: 10.2341/15-195-L. [DOI] [PubMed] [Google Scholar]
- Fleming G.J.P., Awan M., Cooper P.R., Sloan A.J. The potential of a resin-composite to be cured to a 4 mm depth. Dent. Mater. 2008;24:522–529. doi: 10.1016/j.dental.2007.05.016. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration . FDA; Washington, DC: 1976. FDA Guidelines for Chemistry and Technology Requirements of Indirect Additive Petitions. [Google Scholar]
- Gal J.Y., Fovet Y., Adib-Yadzi M. About a synthetic saliva for in vitro studies. Talanta. 2001;53:1103–1115. doi: 10.1016/s0039-9140(00)00618-4. [DOI] [PubMed] [Google Scholar]
- Ilie N., Bucuta S., Draenert M. Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Oper. Dent. 2013;38:618–625. doi: 10.2341/12-395-L. [DOI] [PubMed] [Google Scholar]
- International Organization for Standardization . third ed. Internatonal Organization for Standardization; Genève, Switzerland: 2000. ISO 4049: Dentistry–Polymer-Based Filling, Restorative and Luting Materials. [Google Scholar]
- Jacobsen P.H., Darr A.H. Static and dynamic moduli of composite restorative materials. J. Oral Rehabil. 1997;24:265–273. doi: 10.1046/j.1365-2842.1997.d01-288.x. [DOI] [PubMed] [Google Scholar]
- Jang J.H., Park S.H., Hwang I.N. Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper. Dent. 2015;40:172–180. doi: 10.2341/13-307-L. [DOI] [PubMed] [Google Scholar]
- Kooi T.J.M., Tan Q.Z., Yap A.U., Guo W., Tay K.J., Soh M.S. Effects of food-simulating liquids on surface properties of giomer restoratives. Oper. Dent. 2012;37:665–671. doi: 10.2341/11-419-L. [DOI] [PubMed] [Google Scholar]
- Krishnan V.K., Yamuna V. Aging studies of a radiopaque light-cured dental composite in food-simulating liquids. J. Appl. Polym. Sci. 1998;69:1153–1158. [Google Scholar]
- Lassila L.V.J., Nagas E., Vallittu P.K., Garoushi S. Translucency of flowable bulk-filling composites of various thicknesses. Chin. J. Dent. Res. 2012;15:31–35. [PubMed] [Google Scholar]
- Leprince J.G., Palin W.M., Hadis M.A., Devaux J., Leloup G. Progress in dimethacrylate-based dental composite technology and curing efficiency. Dent. Mater. 2013;29:139–156. doi: 10.1016/j.dental.2012.11.005. [DOI] [PubMed] [Google Scholar]
- Leprince J.G., Palin W.M., Vanacker J., Sabbagh J., Devaux J., Leloup G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014;42:993–1000. doi: 10.1016/j.jdent.2014.05.009. [DOI] [PubMed] [Google Scholar]
- Park J., Chang J., Ferracane J., Lee I.B. How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dent. Mater. 2008;24:1501–1505. doi: 10.1016/j.dental.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Pontes L.F., Alves E.B., Alves B.P., Ballester R.Y., Dias C.G.B.T., Silva C.M. Mechanical properties of nanofilled and microhybrid composites cured by different light polymerization modes. Gen. Dent. 2013;61:30–33. [PubMed] [Google Scholar]
- Rodrigues S.A.J., Zanchi C.H., Carvalho R.V., Demarco F.F. Flexural strength and modulus of elasticity of different types of resin-based composites. Braz. Oral Res. 2007;21:16–21. doi: 10.1590/s1806-83242007000100003. [DOI] [PubMed] [Google Scholar]
- Shah P.K., Stansbury J.W. Role of filler and functional group conversion in the evolution of properties in polymeric dental restoratives. Dent. Mater. 2014;30:586–593. doi: 10.1016/j.dental.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vouvoudi E.C., Sideridou I.D. Dynamic mechanical properties of dental nanofilled light-cured resin composites: effect of food-simulating liquids. J. Mech. Behav. Biomed. Mater. 2012;10:87–96. doi: 10.1016/j.jmbbm.2012.02.007. [DOI] [PubMed] [Google Scholar]
- Wu W., Toth E.E., Moffa J.F., Ellison J.A. Subsurface damage layer of in vivo worn dental composite restorations. J. Dent. Res. 1984;63:675–680. doi: 10.1177/00220345840630051401. [DOI] [PubMed] [Google Scholar]
- Yap A.U., Chandra S., Chung S., Lim C. Changes in flexural properties of composite restoratives after aging in water. Oper. Dent. 2002;27:468–474. [PubMed] [Google Scholar]
- Yap A.U., Lim L., Yang T., Ali A., Chung S. Influence of dietary solvents on strength of nanofill and ormocer composites. Oper. Dent. 2005;30:129–133. [PubMed] [Google Scholar]
- Yap A.U., Low J.S., Ong L. Effect of food-simulating liquids on surface characteristics of composite and polyacid-modified. Oper. Dent. 2000;25:170–176. [PubMed] [Google Scholar]
- Yap A.U., Pandya M., Toh W.S. Depth of cure of contemporary bulk-fill resin-based composites. Dent. Mater. J. 2016;35:503–510. doi: 10.4012/dmj.2015-402. [DOI] [PubMed] [Google Scholar]
- Yap A.U., Tan D.T.T., Goh B.K.C., Kuah H.G., Goh M. Effect of food-simulating liquids on the flexural strength of composite and polyacid-modified composite restoratives. Oper. Dent. 2000;25:202–208. [PubMed] [Google Scholar]
- Yap A.U., Teoh S.H. Comparison of flexural properties of composite restoratives using the iso and mini-flexural tests. J. Oral Rehabil. 2003;30:171–177. doi: 10.1046/j.1365-2842.2003.01004.x. [DOI] [PubMed] [Google Scholar]
- Yesilyurt C., Yoldas O., Altintas S.H., Kusgoz A. Effects of food-simulating liquids on the mechanical properties of a silorane-based dental composite. Dent. Mater. J. 2009;28:362–367. doi: 10.4012/dmj.28.362. [DOI] [PubMed] [Google Scholar]