Abstract
This report presents a young woman with psychotic symptoms that were highly suspicious of schizophrenia. Previous attempts of antidepressant therapy of mood symptoms had been ineffective. However, she also presented with discrete signs of an underlying neurological condition, and as a part of the diagnostic workup, neuroimaging revealed ventriculomegaly. She was diagnosed with obstructive hydrocephalus and experienced full remission of psychotic symptoms after neurosurgical intervention with a ventriculoperitoneal shunt. This atypical presentation of obstructive hydrocephalus underlines the importance of neuroimaging in psychiatric differential diagnostics. Otherwise, this young woman had been diagnosed with schizophrenia, instead of organic delusional disorder secondary to a neurological condition, with possible irreversible damage to brain tissue as a consequence.
Keywords: psychiatry, psychotic disorders (incl schizophrenia), hydrocephalus, neuroimaging
Background
In hydrocephalus, cerebrospinal fluid (CSF) accumulates in the brain’s ventricular system. Most cases of hydrocephalus in adults are normal-pressure hydrocephalus (NPH), where the intracranial pressure is normal and there is communication between all parts of the ventricular system. Another type of hydrocephalus is obstructive hydrocephalus caused by obstruction of the CSF flow at some point from production to resorption, which leads to dilation and elevated pressure in the ventricular system before the obstruction. This obstruction is typically caused by cysts or tumours closing narrow passages to the CSF as Foramen of Monro or the Aqueduct of Sylvius. Hydrocephalus commonly presents with a triad of symptoms: cognitive impairment, urinary incontinence and gait disturbance.1 No exact figures for the prevalence of hydrocephalus in adults exist, but it is estimated to affect 2–3 in 100 000 individuals and that NPH is present in 0.5%–1.5% of individuals above 60 years.2 Besides cognitive impairment, other neuropsychiatric symptoms as anxiety or depression are common in hydrocephalus, but predominant psychotic symptoms are not a typical manifestation of this condition.1 The symptoms of hydrocephalus are considered potentially reversible if the condition is treated before it results in permanent damage to the surrounding brain tissue.3 An organic aetiology of mental disturbances is most common in elderly, but can, even though seldom, also be present in younger individuals.4
This case report illustrates why a proper workup is paramount for psychiatric differential diagnostics, even though history and psychopathology are highly suggestive of schizophrenia.
Case presentation
A 22-year-old woman, with a history of depressive symptoms, was acutely admitted to a psychiatric emergency ward because of suicidal ideation and self-harm.
At admission, she described experiences of both auditive and visual hallucinations. In the following days, she also described the experience of depersonalisation and derealisation. Neurological examination at the time of admission did not give rise to any suspicion of neurological disease, and there was no history of physical illness.
Four months earlier, she had been referred to our outpatient clinic with suicidal thoughts and treated with three different antidepressants (sertraline, duloxetine and paroxetine) on suspicion of major depressive disorder, but without any remarkable effect. On one occasion, during this treatment, she had described what seemed to be internal auditive hallucinations with experience of both noise and voices.
She was described as generally intelligent and well functioning despite a moderate but continuous use of cannabis during her high school years. After high school, she studied archaeology at the university for 1 year before dropping out because of cognitive difficulties—at that time considered to be a part of a depressive episode. There was no current history of substance abuse in any form.
The combination of hallucinations and perceptual disturbances, along with the mood symptoms, was considered highly suspicious for developing schizophrenia, and further investigations was initiated during admission to the psychiatric emergency ward.
Investigations
The diagnostic workup included observation during admission and a semistructured diagnostic interview (Present State Examination5) to characterise psychopathology.
During the diagnostic interview, many different symptoms were found to be present: anxiety, obsessive symptoms, perceptual disturbances, disturbances of thought, hallucinations and delusions. The clinical impression to the interviewer was an intelligent and cooperative woman with appropriate grooming, but also a tormented woman with subtle disorientation and remarkable psychomotor retardation (speech and facial expression). She described a free-floating form of anxiety, obsessions and compulsions regarding checking and cleaning, the latter not ego dystonic. Perceptual disturbances were present as visual disturbance of her image in mirrors, and as derealisation and depersonalisation. The experience of derealisation and depersonalisation was described as ‘dreaming while awake’, as if the surroundings were in slow motion and unreal and as a loss of feelings. Hallucinations were present in all modalities of perception: verbal and non-verbal internal auditive hallucinations, unformed visual hallucinations of flashes and shadows, tactile hallucinations as the sense of touch, olfactory hallucinations of rotten flesh (without any accompanying delusional explanation) and somatic hallucinations of feeling like a robot and foreignness to her arm. Thought disturbances were experienced in different forms: as insertion of thoughts about pending catastrophes and suicide, as audible thoughts and as a broadcast of thoughts. At occasions, she had experienced her legs, speech and acts of self-mutilation as under foreign control. Delusional beliefs were of persecutory and depressive nature. The persecutory delusions were centred around fear of poisoning from food and of a murderous plot including snipers ready to shoot her when going outside. The interviewer also noticed signs of cognitive impairment as she had word-finding difficulty and disorientation. No formal psychometric rating of cognitive symptoms was applied.
Even though many of the psychopathologies mentioned above are typical for schizophrenia (pseudo-obsessions and first-rank symptoms), several other symptoms were suggestive of an organic aetiology: unformed visual together with olfactory hallucinations, subtle disorientation, word-finding difficulty and persistent headache. Because of the patient’s neurological symptoms, she was referred to further neurological evaluation including neuroimaging (CT scan and MRI of the head). There were no symptoms of urinary incontinence in the medical history. However, detailed neurological examination revealed insecure gait and coordination problems, but no sign of paralysis. She was referred directly to neurosurgical intervention on the basis of her symptoms and evident ventriculomegaly, without further neurological investigations (ie, lumbar puncture).
Differential diagnosis
Due to the predominant psychotic symptoms, and their nature, the possible differential diagnoses at this point was either organic mental disorders or (primary) psychotic disorders, when considering that there was no history of recent substance use.
Treatment
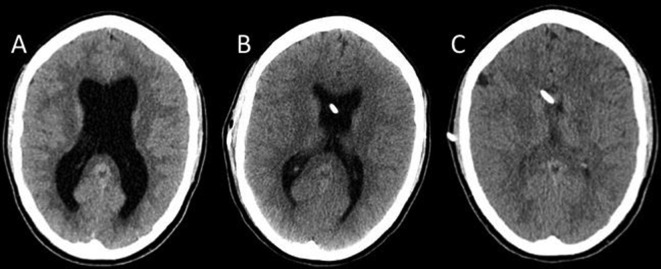
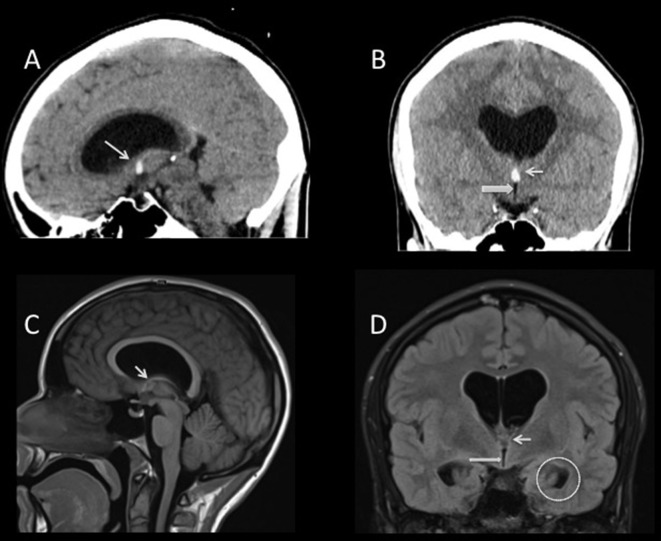
Initially, the patient was treated with antipsychotics (olanzapine and aripiprazole) for her psychotic symptoms. After CT and MRI of the head had shown ventriculomegaly (figures 1A and 2), the patient was referred to the neurosurgical department for further evaluation. Here the diagnosis of obstructive hydrocephalus was established on the basis of neuroimaging, showing dilation of the lateral ventricles, together with a small colloid cyst in the roof of the third ventricle immediately adjacent to the Foramen of Monro and normal calibre of the third ventricle (figure 2). This was deemed the most probable cause of this condition, and the patient was found a candidate for surgery with a ventriculoperitoneal shunt (VPS) (figure 1 B and C).
Figure 1.
Non-contrast enhanced CT scan. Images in transverse plane at the level of the lateral ventricles obtained before ventriculoperitoneal shunt (VPS). (A) Ventriculomegaly. (B and C) Increasing regression of ventriculomegaly 1 week (B) and 1 year (C) after placement of VPS, respectively. VPS catheter is seen in (B) and (C).
Figure 2.
Non-contrast enhanced CT scan in sagittal (A) and coronal (B) plane shows ventriculomegaly of the lateral ventricles and normal calibre of the third ventricle (broad arrow). A small hyperdense colloid cyst is seen adjacent to the Foramen of Monro (thin arrow). Same findings are shown on MRI—fluid-attenuated inversion recovery (FLAIR) T1 weighted (C) and FLAIR T2 weighted (D). In (D), bilateral dilatation of the temporal horns is shown (circled on the left side). No interstitial oedema was present.
Outcome and follow-up
After insertion of the VPS, there were no longer signs of gait disturbances. During further evaluation at the psychiatric department, she showed none of the prior psychopathologies, and therefore her antipsychotic treatment was gradually reduced until she was discharged 18 days after surgery without any antipsychotic medication.
After discharge from the psychiatric department, the patient has been followed up in a psychiatric outpatient clinic and has within the last 17 months not had any relapse of psychotic symptoms. However, depressive and cognitive symptoms occur in periods, and she is still treated with antidepressant medications (paroxetine and mirtazapine). At follow-ups in the neurosurgical department, no signs of urinary symptoms or gait disturbances have been found.
Discussion
Psychoses with organic aetiology can mimic practically any mental illness and are typically characterised by the presence of cognitive impairment, neurological soft signs and hallucinations across all sensory modalities, but without delusional content.4 In contrast, schizophrenia is a psychotic syndrome with many distinct features: Prominent delusions (typically systemised, with impossible content and with accompanying hallucinations), disturbances of thought and speech and negative symptoms as anhedonia and avolition.
In this case, the patient presented many symptoms typical to schizophrenia as pseudo-obsessions and first-rank symptoms, but also several symptoms not typical to schizophrenia as olfactory hallucinations and subtle disorientation. The presence of a persistent headache lead to subacute CT scan of the head which visualised the probable cause of her symptoms: a colloid cyst adjacent to Foramen of Monro, causing obstructive hydrocephalus with dilation of lateral ventricles. Many reports of psychotic or psychiatric symptoms in patients with hydrocephalus are from patients with NPH. A Brazilian survey of patients with NPH found that 25 of 35 (71%) had psychiatric symptoms (depression, anxiety, psychosis).6 However, psychotic symptoms have also been reported in several cases of obstructive hydrocephalus: Roberts et al 7 found five cases with schizophrenia-like psychoses, presenting with symptoms as delusions, auditive hallucinations or social withdrawal, which were later diagnosed with obstructive hydrocephalus on the basis of Sylvian aqueduct stenosis. Other cases have been reported where patients with obstructive hydrocephalus on the basis of colloid cysts around the third ventricle presented with different psychiatric symptoms as hypomania,8 depressive symptoms,9 10 anxiety attacks11 and delusions.10 11 All cases experienced relief from symptoms on surgical intervention by either shunt or removal of cyst.8–11 Dilation of the lateral ventricles has the potential to affect several brain regions hypothesised to be involved in psychiatric conditions, especially frontal lobes, temporal lobes and limbic areas. However, the exact connection from compression of brain tissue to neuropsychiatric symptoms is not known.12
We cannot be sure that the remission of psychotic symptoms, in this case, was solely due to the surgical procedure, but the coincidence in time strongly favours this intervention as the cause of remission. Antipsychotic treatment could play a role in remission of her symptoms, but as there so far has not been any relapse of these, this is not the most likely cause. The possibility exists that the neurological symptoms could have been present at admission, but overlooked by the interviewing physician.
Danish guidelines for diagnosis and treatment of schizophrenia recommends structured diagnostic interview as the cornerstone of the diagnostic process in first episode psychosis (FEP). This interview must be complemented with general somatic and neurological examination, as physical, neurological and other psychiatric conditions can present as psychotic disorders, for example, delirium, hyperthyroidism, encephalitis or intoxication.13 These guidelines also mention that electroencephalogram and CT scan of the head should be considered in FEP, even though neurological symptoms are absent.13 This recommendation of neuroimaging in FEP has been subject to debate, as a subsequent review of neuroimaging in patients with FEP found the prevalence of possible significant findings in this population to be very low (0.6%–3.3%) and that neuroimaging therefore should be reserved for late onset of psychosis, or in situations with neurological symptoms, as it would not lead to surgical action in most cases.14
In conclusion, this case illustrates the relevance of thorough somatic and neurological examination, including neuroimaging, in patients with psychosis, as underlying neuropathological conditions easily can be missed.
Learning points.
Systematic and thorough differential diagnostics is essential in psychiatry to exclude organic causes for mental disturbances.
Psychiatric patients should undergo a routine neurological investigation to rule out possible coexisting neurological disorders.
Neurological examination of the psychiatric patient should include cranial nerve examination, strength, reflexes, sensation, coordination, Romberg test and gait to capture pathology relevant to organic conditions.
Neuroimaging is mandatory at some point in schizophrenia diagnostics.
Footnotes
Contributors: MH has drafted the manuscript. PH has conducted the psychopathological interview. WK has produced the images and other radiological details and LH was responsible for the psychopharmacological treatment. All authors are responsible for the critical revision of the manuscript and its intellectual content.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Fritsch MJ, Kehler U, Meier U. Normal pressure hydrocephalus: pathophysiology, diagnosis, treatment. Stuttgart: Thieme, 2014:6–56. [Google Scholar]
- 2. Brean A, Eide PK. The epidemiology of hydrocephalus Rigamonti D, Adult hydrocephalus. Cambridge: Cambridge University Press, 2014:57–62. [Google Scholar]
- 3. David AS, Lishman WA. Lishman’s organic psychiatry: a textbook of neuropsychiatry. 4th edn: NJWiley-Blackwell, 2009. [Google Scholar]
- 4. Jansson L, Nordgaard J. The psychiatric interview for differential diagnosis. Switzerland: Springer, 2016. [Google Scholar]
- 5. World Health Organization. Schedules for clinical assessment in neuropsychiatry, version 2.1. division of mental health: Geneva Present State Examination, 1998. [Google Scholar]
- 6. Oliveira MF, Oliveira JR, Rotta JM, et al. . Psychiatric symptoms are present in most of the patients with idiopathic normal pressure hydrocephalus. Arq Neuropsiquiatr 2014;72:435–8. 10.1590/0004-282X20140047 [DOI] [PubMed] [Google Scholar]
- 7. Roberts JK, Trimble MR, Robertson M. Schizophrenic psychosis associated with aqueduct stenosis in adults. J Neurol Neurosurg Psychiatry 1983;46:892–8. 10.1136/jnnp.46.10.892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Javed Q, Dutta A. Third ventricular colloid cyst and organic hypomania. Prog Neurol Psychiatry 2014;18:18–20. 10.1002/pnp.355 [DOI] [Google Scholar]
- 9. Jones AM. Psychiatric presentation of a third ventricular colloid cyst in a mentally handicapped woman. Br J Psychiatry 1993;163:677–8. 10.1192/bjp.163.5.677 [DOI] [PubMed] [Google Scholar]
- 10. Upadhyaya AK, Sud PD. Psychiatric presentation of third ventricular colloid cyst. A case report. Br J Psychiatry 1988;152:567–9. 10.1192/bjp.152.4.567 [DOI] [PubMed] [Google Scholar]
- 11. Lobosky JM, Vangilder JC, Damasio AR. Behavioural manifestations of third ventricular colloid cysts. J Neurol Neurosurg Psychiatry 1984;47:1075–80. 10.1136/jnnp.47.10.1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lawrence JE, Nadarajah R, Treger TD, et al. . Neuropsychiatric Manifestations of Colloid Cysts: a review of the literature. Psychiatr Danub 2015;27(Suppl 1):S315–20. [PubMed] [Google Scholar]
- 13. Referenceprogram for skizofreni [Reference programme for Schizophrenia]. Copenhagen: Danish Health Authority, 2004. http://www.sst.dk/~/media/B4266C94C73246B5BB3E645B61917BE4.ashx [Google Scholar]
- 14. Ebdrup BH, Lublin H, Akeson P, et al. . [Patients with first-episode psychosis should not be scanned routinely]. Ugeskr Laeger 2011;173:484–9. [PubMed] [Google Scholar]