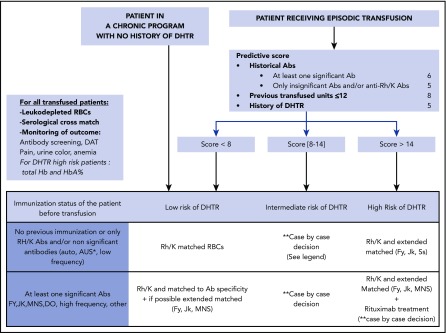
Figure 1.
Recommended transfusion guidelines for patients with SCD. All transfused patients with SCD should receive serologically crossmatch-compatible leukodepleted RBCs and be monitored carefully by performing regular antibody screening tests including DAT and checking for pain, urine color, and signs of anemia. Total Hb and HbA% measurements (Figure 2) are recommended for patients at high risk of DHTR. Patients on a chronic transfusion protocol are considered low-risk DHTR. For patients receiving episodic transfusions, 3 criteria, assigned different point values based on statistical analysis,48 are considered DHTR risk factors: (1) History of RBC immunization. A point value of 6 is given if the patient has a history of at least 1 clinically significant antibody (other than anti-Rh or anti-K) classically known to be involved in transfusion reactions, such as anti-Jkb, Fya, S, HrS. A point value of 5 is given if the patient has a history of only anti-Rh/-K and/or antibodies considered not clinically (clin) significant (eg, autoantibodies or nonspecific antibodies [Ab’s]). Thus, a patient who has an anti-Rh plus an anti-Jkb is given a point value of 6 (and not 6 + 5). (2) Cumulative transfusions of 12 units or less. (3) A previous DHTR. By adding the point values, a DHTR risk score is calculated and transfusion is tailored accordingly. Patients with a score of <8 are considered low risk. Patients transfused episodically who have a low risk of DHTR are transfused with Rh (D, C, E, c, e) and K matched RBCs, which is extended to Fy, Jk, and Ss only if the patient has developed antibodies against any one of these antigens. *AUS, antibody with unknown specificity. **Patients who score between 8 and 14 have an intermediate risk. For such patients, the extent of matching should be based on their DHTR history and number of previous transfusions; those with no history of DHTR who have been transfused only a few times are considered at a lower risk similar to low-risk patients, but they should still be monitored closely. However, for patients with intermediate DHTR risk who have a history of DHTRs and few transfusions in the past (≤12), we generally consider them high risk, and they receive extended matched RBCs (Fy, Jk, Ss). Patients with a score of >14 are considered at high DHTR risk. Episodically transfused patients with a high risk of DHTR (based on the predictive score) always receive extended matched RBCs (Fy, Jk, Ss). Prophylactic rituximab use should be considered for patients with a history of alloantibodies and severe DHTR.