Abstract
Background
Atherosclerotic cardiovascular disease (ASCVD) and cancer are among the leading causes of economic burden, morbidity, and mortality in the United States. We aimed to quantify the overall impact of cardiovascular modifiable risk factor (CRF) profile on healthcare expenditures among those with and without ASCVD and/or cancer.
Methods and Results
The 2012–2013 Medical Expenditure Panel Survey, a nationally representative adult sample (≥40 years), was utilized for the study. Variables included ASCVD, CRF (hypertension, diabetes mellitus, hypercholesterolemia, smoking, physical activity and/or obesity), and cancer (all). Two‐part econometric models analyzed cost data. Medical Expenditure Panel Survey participants (n=27 275, 59±9 years, 52% female) were studied and 14% had cancer, translating to 25.6 million US adults over 40 years of age. A higher prevalence of ASCVD was noted in those with versus without cancer (25% versus 14%). Absence of ASCVD and a more favorable CRF profile were associated with significantly lower expenditures across the spectrum of cancer diagnosis. Among cancer patients, the adjusted mean annual cost for those with and without ASCVD were $10 852 (95% confidence interval [8917, 12 788]) and $6436 (95% confidence interval [5531, 7342]). Among cancer patients without ASCVD, adjusted annual healthcare expenditures among those with optimal versus poor CRF profile were $4782 and $7256.
Conclusions
In a nationally representative US adult population, absence of ASCVD and a favorable CRF profile were associated with significantly lower medical expenditure among cancer patients. This provides estimates to continue better cardiovascular management and prevention practices, while contextualizing the burden of cancer.
Keywords: cancer, cardiovascular disease risk factors, cost
Subject Categories: Cardiovascular Disease, Lifestyle, Epidemiology, Risk Factors
Clinical Perspective
What Is New?
In this study, we noted a higher prevalence of atherosclerotic cardiovascular disease as well as poor cardiovascular disease risk profile among cancer survivors.
Absence of atherosclerotic cardiovascular disease and presence of optimal cardiovascular risk profile among cancer survivors was associated with a significantly lower overall medical expenditure and resource utilization, including prescription medications, hospitalizations, emergency department, and outpatient visits.
What Are the Clinical Implications?
These results support population healthcare models emphasizing prevention of atherosclerotic cardiovascular disease and improvement of cardiovascular risk factor profiles to favorably impact the rising burden of healthcare expenditures among cancer survivors.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) and cancer are among the leading causes of economic burden, morbidity, and mortality in the United States.1 Nearly half of all deaths in the United States can be attributed to either cancer or ASCVD. The annual direct and indirect cost of ASCVD and cancer in the United States is an estimated $844.4 billion dollars, which is projected to double by 2030.2, 3, 4 In addition to an aging population, a growing number of cancer survivors are expected to increase from 15.5 to 20 million over the next decade, and in whom ASCVD is one of the most common causes of non–cancer‐related deaths.5, 6
An emerging paradigm, which continues to evolve, is the inextricable link between ASCVD and cancer through common modifiable risk factors such as tobacco use, obesity, diabetes mellitus, diet quality, and physical activity. A scientific statement from 2004 endorsed by the American Heart Association, American Cancer Society, and American Diabetes Association called for more collaborative and effective preventive healthcare strategies by targeting these shared risk factors.7 Cancer survivorship begins at the time of diagnosis, and many face increased healthcare expenditures compared with individuals without a history of cancer, which can lead to a reduced use of preventive services and preventive medications.8, 9, 10 Although there are some reports highlighting optimal cardiovascular risk factor (CRF) profile in middle age being associated with reduced cardiovascular costs later in life, the impact of ASCVD and global CRF on healthcare costs and resource utilization among cancer survivors is not well described.11, 12
The goal of this study was to detail the healthcare costs for cancer patients across the spectrum of ASCVD status and varying modifiable CRF profiles in a nationally representative population. We hypothesized that a favorable CRF profile will be associated with significantly lower direct healthcare expenditure and resource utilization in cancer survivors.
Methods
Design
The Medical Expenditure Panel Survey (MEPS) data sets and codebooks used for this study are available to the public, and can be accessed on the Agency for Healthcare Research and Quality website at: https://meps.ahrq.gov/mepsweb/.13 We conducted a retrospective study that utilized data from the MEPS, 2012 and 2013. The MEPS, led by the Agency for Healthcare Research and Quality, is a set of large‐scale, national survey about individuals and families, their medical providers, and their employers. The Household Component of the MEPS collects data about health services used, their frequency and cost, charges, source of payment, income, employment, as well as ample data on insurance used by and available to US workers.13 The MEPS respondents are enrolled for 2 years of data collection, with a new panel beginning each year. The sampling frame for the MEPS‐Household Component is drawn from respondents to the National Health Interview Survey and the design of the MEPS‐ Household Component survey includes sampling weights, stratification, and clustering. The MEPS sampling weights incorporate adjustment for the complex sample design and reflect survey nonresponse and population totals from the Current Population Survey.13
In order to increase the study's population, we merged 2012 and 2013 data, and used (from the MEPS Household Component) the full‐year consolidated data files and medical conditions files. The full‐year consolidated data files include most demographics on a person‐level, while the medical conditions files include each diagnosis a person has, which after being transcribed verbatim at each survey, are translated into International Classification of Diseases, 9th Edition, Clinical Modification (ICD‐9‐CM) by professional coders. MEPS also allows categorization by Clinical Classification Software, a tool from Healthcare Cost and Utilization Project that groups ICD‐9‐CM codes into meaningful clinical categories.14 All files were linked together in order to determine accurate results for each individual. Since MEPS information is publically available, de‐identified data‐files, it was exempt from institutional review board review.15
Participants
Initially, 75 402 individuals were surveyed between 2012 and 2013. We limited our study population to US adults ≥40 years of age (because of the low prevalence of established ASCVD among adults aged 18–39 years), who had a positive sampling weight (to best estimate nationally representative results), and a body mass index≥18.5 kg/m2 (given that they often represent a sicker patient population), reaching a study population of 25 275 noninstitutionalized individuals.
Study Variables
Individuals in the study population were classified into our outcome variables based on presence of either a prior diagnosis (ascertained by ICD‐9‐CM or Clinical Classification Software codes, Table S1), or self‐report for any of the following: ASCVD (coronary artery disease, cerebrovascular disease, or peripheral artery disease), any cancer, and CRFs (hypertension, diabetes mellitus, hypercholesterolemia, lack of physical exercise [defined as not participating in moderate‐vigorous physical activity, ≥30 minutes, ≥5 times per week], smoking and/or obesity [body mass index ≥30 kg/m2, a constructed variable using self‐reported weight and height]). For CRFs, based on the presence of the individual risk factors, survey participants were profiled as “Poor” (≥4 CRFs), “Average” (3–2 CRFs), or “Optimal” (0–1 CRFs).
Outcome variables: expenditures and resource utilization
Total annual direct medical expenditures were calculated for each person. Data for this variable included expenditures from all payer groups and out‐of‐pocket spending, including information from hospitalizations, prescribed medications, outpatient visits (hospital outpatient visits and office‐based visits), emergency department (ED) visits, and other expenditures (dental visits, vision aid, home health care, and other medical supplies). In a similar fashion, resource utilization analysis assessed the total number of outpatient and ED visits, number of hospitalizations and number of prescription medications purchases/refills each surveyed individual incurred. All expenditures were adjusted to 2013 US dollars by use of the gross domestic product .16
Covariates
Other variables included in the study were age (grouped in 40–54, 55–64, 65–74, and ≥75), sex, family income (grouped in Poor/Near poor [<125% of the 2012 federal poverty level], Low/Middle Income [125% to <400% federal poverty level], and High Income [≥400% federal poverty level]), race/ethnicity, employment, insurance type, education, geographical region, and modified Charlson Comorbidity Index (without cardiovascular components).
Statistical Analysis
For comparison of demographic characteristics in our sample, χ2 tests were performed.17 Because of the right‐skewedness of expenditures data (i.e. most expenditures are seen in only a small proportion of the population), 2‐part models were utilized to study expenditures.18 Two‐part models are often used to model healthcare expenditures, and are the product of (1) the probability that any given individual had any expenditures; and (2) their mean expenditures.19 The first part of the model consists of a probabilistic regression model (probit), which estimates the probability of zero versus positive expenditures. Contingent upon having a positive annual healthcare expenditure, a generalized linear model (glm) with gamma distribution and a logarithmic‐link function estimates the average expenditure per capita19, 20; we determined the distribution of the glm using the modified Park Test.21 For resource utilization, unadjusted and adjusted logistic regression models were utilized. Unadjusted means and proportions were calculated, adjusting for the survey design and sampling weight. For all statistical analyses, P<0.05 was considered statistically significant. All analyses were carried out using Stata®, version 13.1 (StataCorp, LP, College Station, TX). Total and Marginal expenditures were estimated using the “margins” command after the 2‐part models.19 All analyses took into consideration the MEPS complex survey design.
Results
Population Characteristics
The final study population consisted of 27 275 participants ≥40 years of age (59±9 years, 52% female), which translates to ≈141.6 million US adults; demographic information is presented in Table 1. Overall, 14% had cancer, translating to 25.6 million of the noninstitutionalized adult population in the United States. Those with cancer were more likely to be older, female, have ASCVD, have poor CRF profile, and a higher burden of comorbid conditions. In the total study population with cancer, 1434 (26.7%) had optimal, 2361 (50.6%) had average, and 1126 (22.7%) had poor CRF profile, translating to 6.8, 12.9, and 5.8 million individuals in the United States, respectively.
Table 1.
Baseline Characteristics From Adults ≥40 Years of Age, With and Without Cancer, From the MEPS Survey 2012–2013
| All | Cancer | No Cancer | P Value | |
|---|---|---|---|---|
| Sample (N) | 27 275 | 3951 | 23 324 | |
| Weighted sample | 141 619 336 | 25 610 059 | 116 009 277 | |
| Age strata, n (weighted %) (y) | <0.001 | |||
| 40–54 | 14 418 (42.4) | 963 (18.2) | 13 455 (47.7) | |
| 55–64 | 8152 (27.2) | 1076 (24.8) | 7076 (27.7) | |
| 65–74 | 4937 (17.6) | 1203 (28.5) | 3734 (15.2) | |
| ≥75 | 3366 (12.8) | 1157 (28.4) | 2209 (9.4) | |
| Sex, n (weighted %) | <0.001 | |||
| Female | 39 365 (52.2) | 2913 (54.9) | 36 452 (51.6) | |
| Male | 36 037 (47.8) | 2008 (45.1) | 34 029 (48.4) | |
| Race/ethnicity, n (weighted %) | <0.001 | |||
| Non‐Hispanic white | 27 747 (70.9) | 3390 (87.3) | 24 357 (67.2) | |
| Non‐Hispanic black | 15 646 (10.9) | 690 (5.5) | 14 956 (12.1) | |
| Non‐Hispanic Asian | 5410 (4.9) | 151 (1.5) | 5259 (5.6) | |
| Non‐Hispanic other/multiple | 2219 (1.9) | 74 (1.1) | 2145 (2.1) | |
| Hispanic | 24 380 (11.5) | 616 (4.6) | 23 764 (13.0) | |
| Atherosclerotic cardiovascular disease, n (weighted %) | <0.001 | |||
| Non‐ASCVD | 70 395 (84.3) | 3738 (74.9) | 66 657 (86.4) | |
| ASCVD | 5007 (15.7) | 1183 (25.1) | 3824 (13.6) | |
| CRF profile, n (weighted %) | <0.001 | |||
| Optimal | 48 893 (36.0) | 1434 (26.7) | 47 459 (38.0) | |
| Average | 20 121 (45.8) | 2361 (50.6) | 17 760 (44.7) | |
| Poor | 6388 (18.2) | 1126 (22.7) | 5262 (17.2) | |
| Education, n (weighted %) | <0.001 | |||
| <High School | 33 722 (13.9) | 890 (11.9) | 32 832 (14.3) | |
| GED or high school diploma | 29 967 (56.0) | 2683 (55.4) | 27 284 (56.2) | |
| >College | 11 550 (30.1) | 1343 (32.8) | 10 207 (29.5) | |
| Insurance status, n (weighted %) | <0.001 | |||
| Private | 37 641 (67.1) | 2963 (66.7) | 34 678 (67.2) | |
| Public only | 24 128 (21.5) | 1639 (29.1) | 22 489 (19.8) | |
| Uninsured | 13 633 (11.4) | 319 (4.2) | 13 314 (12.9) | |
| Region, n (weighted %) | <0.001 | |||
| Northeast | 12 254 (18.3) | 796 (17.2) | 11 458 (18.6) | |
| Midwest | 13 810 (21.8) | 1066 (23.3) | 12 744 (21.5) | |
| South | 28 178 (37.3) | 1861 (36.9) | 26 317 (37.4) | |
| West | 21 160 (22.5) | 1198 (22.6) | 19 962 (22.5) | |
| Family income, n (weighted %) | <0.001 | |||
| Poor | 18 124 (10.3) | 757 (8.3) | 17 367 (10.7) | |
| Near poor | 5033 (4.3) | 285 (4.9) | 4748 (4.2) | |
| Low income | 13 111 (12.8) | 722 (13.8) | 12 389 (12.6) | |
| Middle income | 20 719 (28.7) | 1386 (26.5) | 19 333 (29.1) | |
| High income | 18 415 (44.0) | 1771 (46.4) | 16 644 (43.4) | |
| Modified Charlson Comorbidity Indexa, n (weighted %) | <0.001 | |||
| 0 | 67 098 (83.8) | 2976 (62.1) | 64 122 (88.6) | |
| 1 | 6737 (10.9) | 576 (11.5) | 6161 (10.8) | |
| ≥2 | 1567 (5.3) | 1369 (26.4) | 198 (0.6) |
ASCVD indicates atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor; GED, general equivalency diploma; MEP, Medical Expenditure Panel.
Charlson Comorbidity Index without Cardiovascular components.
Healthcare Expenditures
Average per‐capita healthcare expenditures estimated using univariate and multivariate models by CRF profile, cancer, and ASCVD status are shown in Table 2. Presence of cancer was associated with increased overall healthcare expenditures compared with those without cancer across the spectrum of ASCVD status and CRF profile. Cancer participants without ASCVD and a poor CRF profile had a mean annual expenditure of $11 191 compared with $8116 among those with an optimal CRF profile (Table 2, model 1). Additional adjustments for covariates including demographics, socioeconomic factors, insurance, and comorbid conditions continued to show a robust association with $7256 (95% confidence interval [CI], 5245–9266) versus $4782 (95% CI, 3764–5800) mean annual expenditure of cancer participants without ASCVD and with poor CRF versus optimal CRF profiles, respectively (Table 2, model 3). Highest adjusted marginal total healthcare expenditure of $10 852 (95% CI, 8917–12 788) was observed in those with both cancer and ASCVD. In a sensitivity analysis, we additionally added an interaction between presence of cancer diagnosis and ASCVD/NON‐ASCVD CRF Profiles, with it being nonsignificant (P>0.1), thus proving that a cancer diagnosis would not influence our results, and similar trends should be expected. Figure details levels of specific expenditures (hospitalizations, ED visits, prescription drugs, office‐based visits, and other) according to CRF profile, ASCVD, and cancer status. Adjusting for covariates including demographics, insurance, socioeconomic status, as well as comorbid conditions, individuals with cancer in the absence of ASCVD and with a poor CRF profile spent an annual average of $2207 on hospitalizations and $1969 on prescription medications compared with $1194 and $624 for cancer individuals with optimal CRF profile, respectively.
Table 2.
Total Costs by Cancer, ASCVD, and CRF Profile
| ASCVD | No ASCVD | |||
|---|---|---|---|---|
| CRF Profile | ||||
| Poor | Average | Optimal | ||
| Expenditure (95% CI) | Expenditure (95% CI) | Expenditure (95% CI) | Expenditure (95% CI) | |
| Model 1 | ||||
| Cancer | $15 906 (14 335, 17 477) | $11 191 (9137, 13 244) | $9129 (8087, 10 171) | $8116 (5608, 10 623) |
| No cancer | $11 556 (10 608, 12 503) | $7842 (7039, 8644) | $4413 (4123, 4703) | $2697 (2477, 2918) |
| Model 2 | ||||
| Cancer | $14 001 (11 773, 16 228) | $9639 (7486, 11 793) | $6712 (5849, 7574) | $6309 (4380, 8238) |
| No cancer | $9972 (8630, 11 313) | $7034 (6132, 7936) | $3698 (3447, 3948) | $2446 (2237, 2655) |
| Model 3 | ||||
| Cancer | $10 852 (8917, 12 788) | $7256 (5245, 9266) | $5306 (4715, 5896) | $4782 (3764, 5800) |
| No cancer | $9443 (8316, 10 569) | $6790 (6009, 7572) | $3954 (3691, 4218) | $2841 (2542, 3140) |
Model 1: unadjusted. Model 2: adjusted for age, sex, socioeconomic status, race/ethnicity, insurance type, and geographical region. Model 3: adjusted for “model 2” plus Modified Charlson Comorbidity Index (without cardiovascular components). ASCVD indicates atherosclerotic cardiovascular disease; CI, confidence interval; CRF, cardiovascular risk factor.
Figure 1.
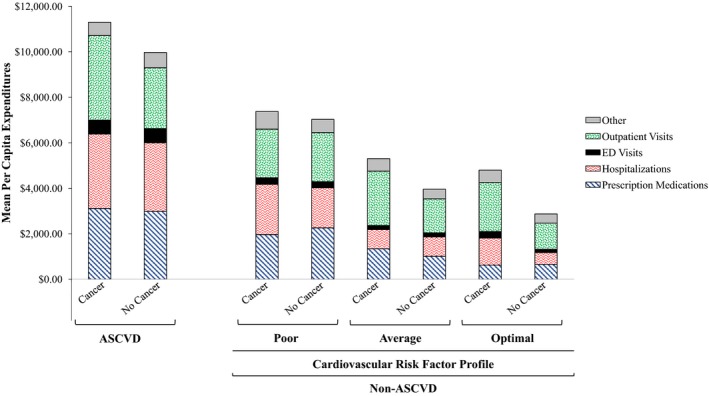
Mean per capita healthcare expenditures by ASCVD, cardiovascular risk factor profile, and cancer status. ASCVD indicates atherosclerotic cardiovascular disease; ED, emergency department. Weighted and adjusted for age, sex, socioeconomic status, race/ethnicity, insurance type, geographic region, modified Charlson Comorbidity Index (without Cardiovascular components), and modifiable risk factors (only ASCVD).
Healthcare Resource Utilization
Table 3 summarizes healthcare utilization rates across cancer and ASCVD status as well as CRF profile categories. Overall, favorable CRF profile and the absence of ASCVD were associated with significantly less use of healthcare resources among individuals with cancer. Among cancer participants without ASCVD, those with optimal versus poor CRF profile were less likely to have an ED visit (10.3% versus 22.6%) or any hospitalization (7.3% versus 15.1%). After adjusting for key covariates, among individuals with cancer but without ASCVD, those with optimal CRF profile had 72% lower odds of being hospitalized (odds ratio, 0.28 [95% CI, 0.15–0.53]), 67% lower odds of having an ED visit (odds ratio, 0.33 [95% CI, 0.27–0.41]), 61% lower odds of outpatient visit (odds ratio, 0.39 [95% CI, 0.17–0.89]), and 89% lower odds of purchasing/refilling a prescription medication (odds ratio, 0.11 [95% CI, 0.09–0.12]) compared with those with poor CRF profile.
Table 3.
Resource Utilization Stratified by ASCVD, Cancer, and CRF Profile
| ASCVD | No ASCVD | |||
|---|---|---|---|---|
| CRF Profile | ||||
| Poor | Average | Optimal | ||
| Hospitalizations | ||||
| Proportion with any hospitalization | ||||
| Cancer | 0.2791 | 0.1509 | 0.1155 | 0.0731 |
| No cancer | 0.1991 | 0.1019 | 0.0593 | 0.025 |
| Average hospitalizations | ||||
| Cancer | 1.43 | 1.36 | 1.28 | 1.27 |
| No cancer | 1.42 | 1.4 | 1.19 | 1.15 |
| OR for any hospitalization | ||||
| Cancer | ||||
| Unadjusted | Ref | 0.46 (0.40, 0.53) | 0.34 (0.29, 0.39) | 0.20 (0.13, 0.32) |
| Adjusteda | Ref | 0.53 (0.40, 0.70) | 0.43 (0.42, 0.44) | 0.28 (0.15, 0.53) |
| No cancer | ||||
| Unadjusted | Ref | 0.46 (0.38, 0.55) | 0.25 (0.17, 0.38) | 0.10 (0.08, 0.14) |
| Adjusteda | Ref | 0.53 (0.45, 0.64) | 0.34 (0.23, 0.51) | 0.16 (0.13, 0.20) |
| ED | ||||
| Proportion with any ED visits | ||||
| Cancer | 0.3091 | 0.2257 | 0.1708 | 0.1027 |
| No cancer | 0.2634 | 0.1721 | 0.1215 | 0.0717 |
| Average ED visits | ||||
| Cancer | 1.66 | 1.31 | 1.44 | 1.5 |
| No cancer | 1.58 | 1.52 | 1.36 | 1.27 |
| OR for any ED visits | ||||
| Cancer | ||||
| Unadjusted | Ref | 0.65 (0.49, 0.87) | 0.46 (0.20, 1.05) | 0.26 (0.19, 0.34) |
| Adjusted | Ref | 0.72 (0.51, 1.01) | 0.55 (0.25, 1.20) | 0.33 (0.27, 0.41) |
| No cancer | ||||
| Unadjusted | Ref | 0.58 (0.42, 0.81) | 0.39 (0.20, 0.73) | 0.22 (0.16, 0.29) |
| Adjusteda | Ref | 0.58 (0.45, 0.75) | 0.44 (0.25, 0.77) | 0.26 (0.20, 0.35) |
| Outpatient visits | ||||
| Proportion with any outpatient visits | ||||
| Cancer | 0.9759 | 0.9588 | 0.9542 | 0.911 |
| No cancer | 0.9188 | 0.9026 | 0.7956 | 0.6837 |
| Average outpatient visits | ||||
| Cancer | 18.02 | 13.4 | 13.56 | 11.04 |
| No cancer | 12.7 | 10.53 | 8.13 | 6.95 |
| OR for any outpatient visits | ||||
| Cancer | ||||
| Unadjusted | Ref | 0.58 (0.16, 2.12) | 0.52 (0.25, 1.08) | 0.25 (0.14, 0.47) |
| Adjusteda | Ref | 0.68 (0.11, 4.16) | 0.70 (0.45, 1.09) | 0.39 (0.17, 0.89) |
| No cancer | ||||
| Unadjusted | Ref | 0.82 (0.79, 0.85) | 0.34 (0.28, 0.42) | 0.19 (0.17, 0.22) |
| Adjusteda | Ref | 0.98 (0.76, 1.25) | 0.45 (0.31, 0.66) | 0.27 (0.22, 0.32) |
| Prescription medications | ||||
| Proportion with any purchase/refills | ||||
| Cancer | 0.9792 | 0.9732 | 0.9473 | 0.7788 |
| No cancer | 0.9391 | 0.937 | 0.7734 | 0.5385 |
| Average purchase/refills | ||||
| Cancer | 42.22 | 40.18 | 23.85 | 13.55 |
| No cancer | 39.27 | 35.21 | 18.42 | 9.72 |
| OR for any purchase/refills | ||||
| Cancer | ||||
| Unadjusted | Ref | 0.77 (0.48, 1.24) | 0.38 (0.18, 0.80) | 0.07 (0.06, 0.09) |
| Adjusteda | Ref | 0.92 (0.55, 1.54) | 0.51 (0.25, 1.07) | 0.11 (0.09, 0.12) |
| No cancer | ||||
| Unadjusted | Ref | 0.97 (0.45, 2.06) | 0.22 (0.17, 0.29) | 0.08 (0.05, 0.11) |
| Adjusteda | Ref | 1.27 (0.71, 2.27) | 0.32 (0.26, 0.38) | 0.12 (0.08, 0.18) |
Odds ratios are presented as: OR (95% CI). ASCVD indicates atherosclerotic cardiovascular disease; CI, confidence interval; CRF, cardiovascular risk factor; ED, emergency department; OR, odds ratio.
Adjusted for age, sex, socioeconomic status, race/ethnicity, insurance type, geographical region, and Modified Charlson Comorbidity Index (without cardiovascular components).
Discussion
Previous studies have evaluated the financial burden associated with cancer survivorship4, 8, 10, 22, 23; however, to the authors' knowledge, this is the first attempt to contextualize the economic impact of ASCVD and CRF profiles on cancer survivors in a contemporary national representative sample of the US population. We found a higher prevalence of ASCVD (25% versus 14%) and lower likelihood of an optimal CRF profile (27% versus 38%) among cancer survivors compared with those without cancer. Additionally, we found significantly reduced healthcare utilization and expenditures among cancer survivors without ASCVD, and especially among those with optimal CRF profile.
Our results are consistent with prior reports highlighting the increased burden of ASCVD and CRF in cancer survivors.5, 24, 25, 26 Several contributing factors to this observation include common risk factors, rapidly growing survivorship population with the majority over the age of 65, and potentially cardiotoxic effects from cancer therapies themselves.6, 24, 27 Many of the major shared risk factors between cancer and ASCVD are incorporated into the American Heart Association's “Strategic Impact Goals for 2020,” which introduced the Life's Simple 7 (smoking status, physical activity, eating pattern, body weight, blood cholesterol, blood glucose, and blood pressure) as a population‐level health‐promotion strategy that has been shown to improve overall cardiovascular outcomes.28, 29 Additionally, adherence to more components in American Heart Association's Life's Simple 7 appears to be associated with a lower risk of incident cancer even when smoking was removed from the score.30 In a large retrospective cohort, adherence to cancer guidelines for obesity, physical activity, and diet were associated with a reduction of cancer and ASCVD mortality.31 Optimal management of cancer survivors involves increased awareness of worse oncological and cardiovascular outcomes in individuals with ASCVD and CRF, and early recognition and aggressive management of shared risk factors. As noted in our study (Figure), presence of ASCVD and poor risk profile in absence of ASCVD was not only associated with much higher subspecific absolute costs, but also a significant proportion of costs (30%) were related to hospitalizations. On the other hand, among cancer patients in absence of a diagnosis of ASCVD, among patients with average and optimal CRF, hospitalizations contributed to nearly 15% of overall expenditures, with a major proportion (≈40%) of all costs related to outpatient visits. These findings support the focus of current healthcare reforms for value‐based health care, emphasizing an integrated population health on lowering overall healthcare costs by shifting care from hospital‐based services to ambulatory. Our results provide cost estimates for potential cost savings by incorporating preventive strategies of modifiable CRF for cancer survivors to mitigate progression to ASCVD and reduce the associated comorbid cost burden.32
Study Limitations
Several limitations should be noted. First, we could not break down cost by type or stage of cancer, or whether active treatment for cancer was being delivered. Cancer survivors were defined as any individual who has ever been diagnosed with cancer regardless of duration as previously described.6 Second, the MEPS data only capture a fraction of total national health expenditures for cancer patients. For example, nursing home expenditures attributable to cancer are excluded.33 Cancer patients with advanced disease were likely not able to participate in the survey, further underestimating cancer costs. The true burden of cancer goes beyond medical costs and includes lost productivity, stress, mental health, costs for travel and child care, and costs incurred by caretakers.34 Other analyses have reported an underestimation of total medical expenditures from MEPS data, which all suggest our results are a conservative estimate for the burden of modifiable CRF on cancer patients as well as the estimated savings from prevention strategies,33, 35, 36 therefore strengthening our findings. Third, because cancer, ASCVD, and modifiable CRF were self‐reported, there is likely an underrepresentation of the true national prevalence, as has previously been described.37, 38 The prevalence of ASCVD in this study was lower than previous national estimates (15.7% versus 36%), in part because we excluded hypertension, as it was included in the CRF profile.2 Fourth, lack of information on dietary habits did not allow us to include this important modifiable risk factor. Additionally, because of the lack of clinical factors (blood pressure, fasting blood glucose, and total cholesterol), we were not able to calculate American Heart Association's ideal health cardiovascular status (Life's Simple 7). Fifth, there is a risk of residual confounding from unmeasured characteristics that could affect our study outcomes, despite our best attempts to comprehensively control for the most importantly observed contributing variables. Lastly, the results only apply to the noninstitutionalized adult US population.
Conclusions
From a contemporary nationally representative population, we found that the absence of ASCVD and a favorable cardiovascular risk factor profile among cancer survivors was associated with significantly lower healthcare expenditure and resource utilization. These results provide robust estimates for potential healthcare savings as preemptive strategies continue to become integrated into new healthcare delivery models, for increased awareness and prevention of ASCVD, and improvement in cardiovascular risk factor profiles among those with and without diagnosed cancer.
Disclosures
Dr Nasir is on the advisory board for Quest Diagnostics and consultant for Regeneron. Dr Blankstein is on the advisory board for Amgen Inc, is a consultant to EKOS Corporation, and receives research support from Amgen Inc and Gilead Inc. Dr Desai and Dr Spatz are supported by grant K12 HS023000‐01 from the Agency for Healthcare Research and Quality. Dr Desai receives research funding from the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are used for public reporting and support from Johnson & Johnson and Medtronic, through Yale University, to develop methods of clinical trial data sharing. Dr Spatz receives research funding from the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are used for public reporting. The remaining authors have no disclosures to report.
Supporting information
Table S1. ICD‐9‐CM Codes, MEPS 2012–2013
(J Am Heart Assoc. 2018;7:e007874 DOI: 10.1161/JAHA.117.007874.)29686026
References
- 1. Xu J, Murphy SL, Kochanek KD, Bastian BA. Deaths: final data for 2013. Natl Vital Stat Rep. 2016;64:1–119. [PubMed] [Google Scholar]
- 2. Writing Group M , Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; American Heart Association Statistics C and Stroke Statistics S . Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 3. Bloom DE, Cafiero E, Jané‐Llopis E, Abrahams‐Gessel S, Bloom LR, Fathima S, Feigl AB, Gaziano T, Hamandi A, Mowafi M. The global economic burden of noncommunicable diseases. Geneva: Economic Forum; 2011. [Google Scholar]
- 4. Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the US: estimates, projections, and future research. Cancer Epidemiol Biomarkers Prev. 2011;20:2006–2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Armenian SH, Xu L, Ky B, Sun C, Farol LT, Pal SK, Douglas PS, Bhatia S, Chao C. Cardiovascular disease among survivors of adult‐onset cancer: a community‐based retrospective cohort study. J Clin Oncol. 2016;34:1122–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30. [DOI] [PubMed] [Google Scholar]
- 7. Eyre H, Kahn R, Robertson RM, Clark NG, Doyle C, Hong Y, Gansler T, Glynn T, Smith RA, Taubert K, Thun MJ; American Cancer S, American Diabetes A, American Heart A . Preventing cancer, cardiovascular disease, and diabetes: a common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. Circulation. 2004;109:3244–3255. [DOI] [PubMed] [Google Scholar]
- 8. Guy GP Jr, Ekwueme DU, Yabroff KR, Dowling EC, Li C, Rodriguez JL, de Moor JS, Virgo KS. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31:3749–3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rezayatmand R, Pavlova M, Groot W. The impact of out‐of‐pocket payments on prevention and health‐related lifestyle: a systematic literature review. Eur J Public Health. 2013;23:74–79. [DOI] [PubMed] [Google Scholar]
- 10. Guy GP Jr, Yabroff KR, Ekwueme DU, Virgo KS, Han X, Banegas MP, Soni A, Zheng Z, Chawla N, Geiger AM. Healthcare expenditure burden among non‐elderly cancer survivors, 2008–2012. Am J Prev Med. 2015;49:S489–S497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daviglus ML, Liu K, Greenland P, Dyer AR, Garside DB, Manheim L, Lowe LP, Rodin M, Lubitz J, Stamler J. Benefit of a favorable cardiovascular risk‐factor profile in middle age with respect to Medicare costs. N Engl J Med. 1998;339:1122–1129. [DOI] [PubMed] [Google Scholar]
- 12. Willis BL, DeFina LF, Bachmann JM, Franzini L, Shay CM, Gao A, Leonard D, Berry JD. Association of ideal cardiovascular health and long‐term healthcare costs. Am J Prev Med. 2015;49:678–685. [DOI] [PubMed] [Google Scholar]
- 13. Medical Expenditure Panel Survey. Available at: http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. Accessed August 21, 2009.
- 14. HCUP . Clinical Classification Software. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed March 6, 2017.
- 15. IRB Exemption. Available at: http://www.hhs.gov/ohrp/regulations-and-policy/decision-trees/. Accessed February 16, 2016.
- 16. MEPS Price Index. Available at: http://meps.ahrq.gov/about_meps/Price_Index.shtml. Accessed May 8, 2016.
- 17. Ozieh MN, Dismuke CE, Lynch CP, Egede LE. Medical care expenditures associated with chronic kidney disease in adults with diabetes: United States 2011. Diabetes Res Clin Pract. 2015;109:185–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mihaylova B, Briggs A, O'Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20:897–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Belloti F, Deb P, Manning WG, Norton EC. twopm: two‐part models. Stata J. 2015;15:3–20. [Google Scholar]
- 20. Hardin J, HIilbe J. Generalized Linear Models and Extensions. 2nd ed College Station, TX: StataCorp LP, Stata Press; 2007. [Google Scholar]
- 21. Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. [DOI] [PubMed] [Google Scholar]
- 22. Banegas MP, Guy GP Jr, de Moor JS, Ekwueme DU, Virgo KS, Kent EE, Nutt S, Zheng Z, Rechis R, Yabroff KR. For working‐age cancer survivors, medical debt and bankruptcy create financial hardships. Health Aff (Millwood). 2016;35:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zheng Z, Yabroff KR, Guy GP Jr, Han X, Li C, Banegas MP, Ekwueme DU, Jemal A. Annual medical expenditure and productivity loss among colorectal, female breast, and prostate cancer survivors in the United States. J Natl Cancer Inst. 2016;108:djv382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Johnson CB, Davis MK, Law A, Sulpher J. Shared risk factors for cardiovascular disease and cancer: implications for preventive health and clinical care in oncology patients. Can J Cardiol. 2016;32:900–907. [DOI] [PubMed] [Google Scholar]
- 25. Vijayvergia N, Denlinger CS. Lifestyle factors in cancer survivorship: where we are and where we are headed. J Pers Med. 2015;5:243–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Weaver KE, Foraker RE, Alfano CM, Rowland JH, Arora NK, Bellizzi KM, Hamilton AS, Oakley‐Girvan I, Keel G, Aziz NM. Cardiovascular risk factors among long‐term survivors of breast, prostate, colorectal, and gynecologic cancers: a gap in survivorship care? J Cancer Surviv. 2013;7:253–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shelburne N, Adhikari B, Brell J, Davis M, Desvigne‐Nickens P, Freedman A, Minasian L, Force T, Remick SC. Cancer treatment—related cardiotoxicity: current state of knowledge and future research priorities. J Natl Cancer Inst. 2014;106:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD, Investigators AS. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all‐cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rasmussen‐Torvik LJ, Shay CM, Abramson JG, Friedrich CA, Nettleton JA, Prizment AE, Folsom AR. Ideal cardiovascular health is inversely associated with incident cancer: the Atherosclerosis Risk In Communities study. Circulation. 2013;127:1270–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McCullough ML, Patel AV, Kushi LH, Patel R, Willett WC, Doyle C, Thun MJ, Gapstur SM. Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all‐cause mortality. Cancer Epidemiol Biomarkers Prev. 2011;20:1089–1097. [DOI] [PubMed] [Google Scholar]
- 32. Barac A, Murtagh G, Carver JR, Chen MH, Freeman AM, Herrmann J, Iliescu C, Ky B, Mayer EL, Okwuosa TM, Plana JC, Ryan TD, Rzeszut AK, Douglas PS. Cardiovascular health of patients with cancer and cancer survivors. J Am Coll Cardiol. 2015;65:2739–2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sing M, Banthin JS, Selden TM, Cowan CA, Keehan SP. Reconciling medical expenditure estimates from the MEPS and NHEA, 2002. Health Care Financ Rev. 2006;28:25–40. [PMC free article] [PubMed] [Google Scholar]
- 34. Yabroff KR, Davis WW, Lamont EB, Fahey A, Topor M, Brown ML, Warren JL. Patient time costs associated with cancer care. J Natl Cancer Inst. 2007;99:14–23. [DOI] [PubMed] [Google Scholar]
- 35. Aizcorbe A, Liebman E, Pack S, Cutler DM, Chernew ME, Rosen AB. Measuring health care costs of individuals with employer‐sponsored health insurance in the U.S.: a comparison of survey and claims data. Stat J IAOS. 2012;28:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Trogdon JG, Murphy LB, Khavjou OA, Li R, Maylahn CM, Tangka FK, Nurmagambetov TA, Ekwueme DU, Nwaise I, Chapman DP, Orenstein D. Costs of chronic diseases at the state level: the chronic disease cost calculator. Prev Chronic Dis. 2015;12:E140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Edwards WS, Winn DM, Kurlantzick V, Sheridan S, Berk ML, Retchin S, Collins JG. Evaluation of National Health Interview Survey diagnostic reporting. Vital Health Stat 2. 1994: 1–116. [PubMed] [Google Scholar]
- 38. Dominguez FJ, Lawrence C, Halpern EF, Drohan B, Grinstein G, Black DM, Smith BL, Gadd MA, Specht M, Kopans DB, Moore RH, Hughes SS, Roche CA, Hughes KS. Accuracy of self‐reported personal history of cancer in an outpatient breast center. J Genet Couns. 2007;16:341–345. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. ICD‐9‐CM Codes, MEPS 2012–2013


