Abstract
The aim of this study was to determine complication rates and possible risk factors of expert-performed endotracheal intubation (ETI) in patients with trauma, in both the prehospital setting and the emergency department. We also investigated how the occurrence of ETI-related complications affected the survival of trauma patients. This single-center retrospective observational study included all injured patients who underwent anesthesiologist-performed ETI from 2007 to 2017. ETI-related complications were defined as hypoxemia, unrecognized esophageal intubation, regurgitation, cardiac arrest, ETI failure rescued by emergency surgical airway, dental trauma, cuff leak, and mainstem bronchus intubation. Of the 537 patients included, 23.5% experienced at least one complication. Multivariable logistic regression analysis revealed that low Glasgow Coma Scale Score (adjusted odds ratio [AOR], 0.93; 95% confidence interval [CI], 0.88–0.98), elevated heart rate (AOR, 1.01; 95% CI, 1.00–1.02), and three or more ETI attempts (AOR, 15.71; 95% CI, 3.37–73.2) were independent predictors of ETI-related complications. We also found that ETI-related complications decreased the likelihood of survival of trauma patients (AOR, 0.60; 95% CI, 0.38–0.95), independently of age, male sex, Injury Severity Score, Glasgow Coma Scale Score, and off-hours presentation. Our results suggest that airway management in trauma patients carries a very high risk; this finding has implications for the practice of airway management in injured patients.
1. Introduction
Traumatic injury is the leading cause of death and disability among young people and places a tremendous economic burden on society [1, 2]. Early and appropriate airway management is a vital lifesaving measure in severely injured patients [3] because airway compromise is a significant cause of poor outcomes in this population [4]. Trauma patients have a very high risk of hemodynamic instability, restlessness, inadequate evaluation, and the need for cervical spine protection, all of which contribute to difficult ETI [5–9]. Ideally, this challenging procedure should be delegated to a skilled laryngoscopist who performs ETI frequently, such as an anesthesiologist. To better understand the risks of trauma airway management, it is important to clarify the incidence and associated factors of expert-performed ETI-related complications. However, past studies have not fully provided this information.
Previous studies have reported that trauma ETI can cause life-threating complications, including aspiration, misplacement of the endotracheal tube, hypoxemia, the need for an emergency surgical airway, and circulatory collapse [8, 9]. However, the degree to which these complications affect the outcomes of trauma patients is not well understood.
In our hospital emergency department (ED), airway management in severe trauma patients is primarily the responsibility of anesthesiologists. Our facility also runs a prehospital emergency medical unit staffed by the same anesthesiologists. This unique clinical arrangement allows us to investigate the incidence and possible risk factors of ETI-related complications in trauma patients treated in both the prehospital setting and the ED by laryngoscopists with “expert” status, as recently defined by Breckwoldt et al. [10]. Using our trauma and quality assurance database, we also investigated how the occurrence of ETI-related complications affected the survival of trauma patients.
2. Materials and Methods
2.1. Ethical Approval and Consent to Participate
The study was approved by the Ethics Committee of Ohta Nishinouchi Hospital (no. 6_H27) on May 15, 2015. The committee waived the need for informed consent because the study was nonrandomized and assessed the clinical outcomes of routine practices.
2.2. Study Design and Setting
This retrospective observational study was conducted at a community hospital in a provincial Japanese city located approximately 200 km north of Tokyo. The hospital serves both as a teaching facility and as a referral medical center for a population of 538,000 inhabitants within an area of 2400 km2. Annually, the hospital receives > 5500 ambulances and > 1200 trauma patients with injuries of varying severity. At the hospital, the primary responsibility for airway management in severe trauma patients lies with ED physicians with a background in anesthesiology. The hospital also runs a prehospital emergency medical unit (doctor-car system) consisting of a trained ambulance driver, a nurse, and a senior physician whose specialty is anesthesiology. This physician-delivery system is dispatched to the scene in response to a request by the regional medical control center.
Anesthesiologists must have a minimum of 4 years of clinical experience before they are allowed to work in the ED or the prehospital emergency medical unit. Each anesthesiologist performs approximately 300 ETIs per year in the operating room. Operating room cases cover the full spectrum of difficult airway situations, including head and neck surgery, pediatric anesthesia, and differential lung ventilation.
2.3. Participants and Data Sources
This study included all trauma patients who underwent emergency ETI in either the prehospital or the ED setting from January 1, 2007, to January 1, 2017. The exclusion criteria were as follows: patients who received ongoing cardiopulmonary resuscitation at initial contact, patients who received a surgical airway as an initial intubation attempt, and patients who were transported to our hospital from other facilities. In Japan, paramedics are not permitted to perform ETI except in cases of cardiopulmonary arrest. Therefore, this study did not include trauma patients who received ETI performed by paramedics. The data were collected from a trauma and quality assurance electronic database, medical records, and nursing records. Our facility maintains a rigorous peer-review process to ensure the quality of our trauma practice. Life-threatening ETI-associated complications, such as cardiac arrest after an ETI attempt, failed intubation salvaged by emergency surgical airway, and esophageal intubation with delayed recognition, occurring in either the prehospital or ED setting, are peer-reviewed, confirmed by experienced anesthesiologists, and recorded in the quality assurance database.
The database also records injury severity according to the Abbreviated Injury Scale (AIS) for each body region [11], the Injury Severity Score (ISS) [12], the Revised Trauma Score (RTS) [13], and the probability of survival (Ps), which is based on the Trauma and Injury Severity Scores method [14, 15]. These parameters were scored without delay by one of the authors (KS). Comorbidity was described using the Charlson comorbidity index [16].
Our department uses a structured medical record that includes the patient's age, sex, initial vital signs, time from the emergency call to scene arrival, time from scene departure to the ED, past medical history, detailed history of the present condition, physical examination, laboratory data, radiological findings, final diagnosis, patient disposition, and any complications. As specified in the guidelines of several professional anesthesiology societies [17, 18], our department mandates documentation of the details of airway difficulty in the medical record to provide relevant information on ETI-related complications. All physicians who participate in the management of trauma patients are required to complete the form immediately; an ED director at our hospital (KS) checks all medical records at the earliest possible opportunity to verify the completeness and reliability of the data. Nursing records include information on the laryngoscopist, the number of ETI attempts, the medication used to facilitate ETI, and the patient's vital signs before and after ETI attempts. The ETI procedure and the choice of drugs to facilitate ETI are at the discretion of the participating anesthesiologist. A standard operating procedure for ETI [19], such as unified equipment set-up, pre-ETI assessment, and postintubation care with end-tidal CO2 detection, has not yet been established in our facility. Correct endotracheal tube placement is verified based on clinical findings, such as tube fogging, chest rise, and auscultation, with secondary confirmation by capnometry performed at the discretion of the attending physician. In our ED, a chest X-ray or computed tomography scan is routinely performed after tube placement to detect mainstem bronchus intubation. For consistency with our own studies and those of other researchers [20, 21], off hours were defined as the period from 6:01 PM to 8:00 AM on weekdays plus the entire weekend.
2.4. Definition of Endotracheal Intubation-Related Complications
ETI-associated complications were defined as hypoxemia, esophageal intubation with delayed recognition, cardiac arrest immediately after ETI attempt, recorded regurgitation, ETI failure rescued by emergency surgical airway, dental trauma, cuff leak requiring intubation, or mainstem bronchus intubation. Hypoxemia was defined as a decline in pulse oximetry saturation > 10% from baseline during ETI attempts, not resulting from esophageal intubation [21–24]. Esophageal intubation with delayed recognition was defined as misplacement of the endotracheal tube in the upper esophagus or hypopharynx, with time elapsed and desaturation (> 10% decline in pulse oximetry saturation) also recorded [21–24]. Recorded regurgitation was defined as the immediate peri-induction regurgitation of gastric contents at the glottis opening or in the endotracheal tube, clearly documented in the ED or nursing records [21–24]. Cardiac arrest immediately after an ETI attempt included asystole, bradycardia, or dysrhythmia in a patient without a measurable blood pressure and requiring cardiopulmonary resuscitation during or immediately after the ETI attempt [21–24]. If ETI was impossible after anesthesia induction and a salvage surgical technique was required, then the event was classified as ETI failure rescued by emergency surgical airway [21, 25]. Previous studies have included hemodynamic parameters, such as hypertension and hypotension, in the definition of ETI-related complications [22–24]. However, we chose to exclude hemodynamic data because hemodynamic perturbations resulting from ETI are difficult to distinguish from those arising from underlying trauma-based etiologies [26, 27].
2.5. Objectives of the Study
The main objective of the study was to clarify the incidence and possible risk factors of ETI-related complications in patients with trauma. The secondary aim was to assess how ETI-related complications affect the survival of trauma patients.
2.6. Statistical Analysis
To achieve the study goals, we first evaluated differences in the baseline clinical characteristics of trauma patients who experienced ETI-related complications versus those who did not. Differences in continuous variables were compared with Student's t-test or Mann–Whitney U-test for normally and non-normally distributed data, respectively, after applying the Shapiro–Wilk test for normality. Differences in categorical variables were compared with a chi-squared test followed by residual analysis.
Next, univariable and multivariable logistic regression models were established to detect independent risk factors for ETI-related complications. Imbalanced characteristics between patients with versus without ETI-related complications (variables with P < 0.15 in Table 2; see Results), such as the location in which ETI was performed, use of rapid-sequence intubation technique, patient sex, ISS, GCS, heart rate, pulse oximetry saturation, and need for three or more ETI attempts, were included as independent variables in the logistic regressions.
Table 2.
Demographic characteristics of trauma patients, according to occurrence of ETI-related complications.
| Number of ETI-related complications | |||
|---|---|---|---|
| ≥ 1 (n =126) | 0 (n =411) | P value | |
| Age, years | 59 (32–74) | 60 (37–73) | 0.864 |
| Male, n (%) | 80 (63.5) | 291 (70.8) | 0.121 |
| Etiology of trauma, n (%) | 0.499 | ||
| Blunt injury | 102 (81.0) | 327 (79.6) | |
| Penetrating injury | 7 (5.6) | 25 (6.1) | |
| Burn | 17 (13.5) | 59 (14.4) | |
| Anatomic parameters | |||
| AIS | |||
| Head or neck | 3 (0–5) | 2 (0–5) | 0.036 |
| Face | 0 (0–1) | 0 (0–1) | 0.288 |
| Chest | 3 (0–4) | 3 (0–4) | 0.665 |
| Abdomen or pelvic contents | 0 (0–2) | 0 (0–2) | 0.526 |
| Extremities or pelvic girdle | 2 (0–3) | 1 (0–3) | 0.870 |
| External | 0 (0–0) | 0 (0–0) | 0.679 |
| ISS | 36 (25–45) | 29 (22–42) | 0.005 |
| Physiological parameters | |||
| GCS | 8 (3–12) | 12 (6–14) | < 0.001 |
| Initial recorded vital signs | |||
| Systolic blood pressure, mmHg (mean [SD]) | 126 (41) | 125 (40) | 0.916 |
| Heart rate, beats/min | 101 (85–120) | 92 (78–116) | 0.011 |
| Shock index | 0.8 (0.6–1.1) | 0.8 (0.6–1.0) | 0.267 |
| Respiratory rate, breaths/min | 24 (20–30) | 22 (18–30) | 0.072 |
| Pulse oximetry saturation, % | 100 (95–100) | 100 (98–100) | 0.128 |
| RTS | 5.9 (4.2–6.9) | 6.5 (5.1–7.8) | < 0.001 |
| Ps, % | 59.0 (18.8–85.4) | 80.9 (40.4–95.0) | < 0.001 |
| Charlson comorbidity index | 0 (0–1) | 0 (0–1) | 0.579 |
| Off-hours presentationa, n (%) | 76 (60.3) | 246 (59.9) | 0.926 |
| Emergency operation, n (%) | 54 (42.9) | 204 (49.6) | 0.183 |
| Prehospital ETI | 43 (34.1) | 94 (22.9) | 0.011 |
| Prehospital times | |||
| From emergency call to scene arrival, min | 9 (7–13) | 10 (7–13) | 0.877 |
| From scene arrival to departure, min | 12 (7–19) | 12 (7–21) | 0.96 |
| From scene departure to hospital arrival, min | 12 (8–22) | 14 (8–24) | 0.473 |
| Total prehospital time, min | 37 (27–57) | 38 (27–59) | 0.652 |
| Characteristics of ETI | |||
| Three or more ETI attempts | 12 (9.5) | 2 (0.5) | < 0.001 |
| ETI method | 0.005 | ||
| Without medication | 45 (35.7)∗ | 90 (21.9)∗∗ | |
| Sedative/analgesic only | 28 (22.2) | 80 (19.5) | |
| Paralytic agent only | 9 (7.1) | 31 (7.5) | |
| Rapid sequence intubation technique | 44 (34.9)∗∗ | 210 (51.1)∗ | |
| Hospital length of stay, days | 42 (12–63) | 43 (19–79) | 0.550 |
Data are expressed as the median (interquartile range) unless otherwise indicated.
AIS: Abbreviated Injury Scale, ED: emergency department, ETI: endotracheal intubation, GCS: Glasgow Coma Scale Score, ISS: Injury Severity Score, Ps: probability of survival, RTS: Revised Trauma Score, SD: standard deviation.
a6:01 PM to 8:00 AM on weekdays plus all weekend hours.
∗ Adjusted standardized residual > 1.96, ∗∗ adjusted standardized residual < −1.96.
Finally, to clarify whether ETI-related complications decreased the survival of injured patients independently of age, sex, ISS, GCS, and off-hours admission, additional logistic regression models were constructed. A set of these variables was chosen a priori based on previous information [12, 28–30] and biological plausibility.
In all logistic regression models, a variance inflation factor was used to detect multicollinearity. The models' goodness of fit and discrimination ability were confirmed with the Hosmer–Lemeshow test and the c statistic, respectively. All statistical analyses were performed with SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA). A P value < 0.05 was considered statistically significant.
3. Results
During the 120-month study period, 12,705 trauma patients were brought to the ED, of whom 794 required ETI in the prehospital or ED setting (Figure 1). Of these, we excluded 223 patients who received ongoing cardiopulmonary resuscitation, 30 patients who were transported from other facilities, and four patients who underwent initial airway management by emergency surgery. The remaining 537 patients were included in the analysis. Of these patients, 137 (25.5%) received ETI in a prehospital setting and 400 (74.5%) in the ED (Figure 1). Complete records were available for all patients and no data were missing from the analyses.
Figure 1.
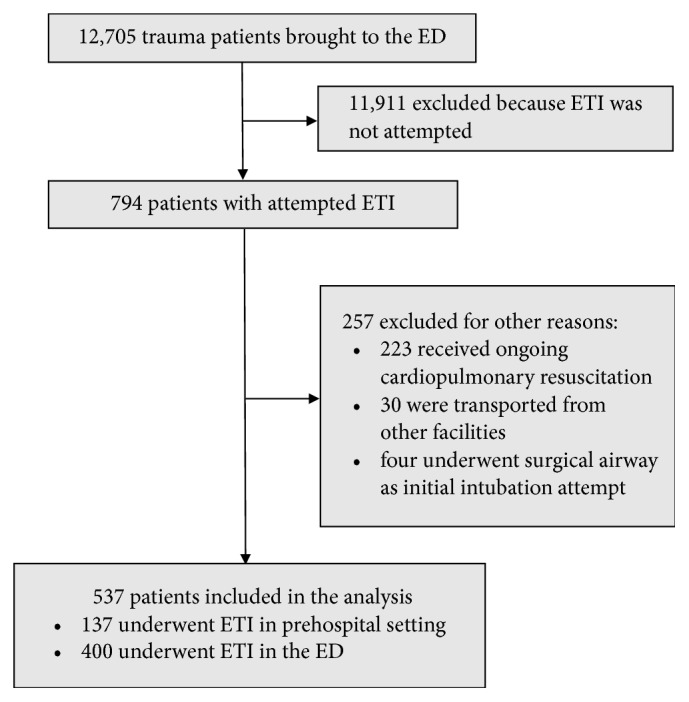
Flow chart showing the selection process for injured patients who underwent ETI in prehospital or emergency department setting. ED emergency department, ETI endotracheal intubation.
3.1. Incidence of Endotracheal Intubation-Related Complications
Table 1 shows details of ETI-related airway complications in prehospital and ED settings. Overall, 23.5% of the study population experienced at least one ETI-associated complication, of which mainstem bronchus intubation was the most common.
Table 1.
Details of airway-related complications in injured patients who underwent ETI in prehospital or emergency department setting.
| N = 537 | n (%) |
|---|---|
| At least one complication | 126 (23.5) |
| Hypoxemia | 25 (4.7) |
| Esophageal intubation with delayed recognition | 9 (1.7) |
| Cardiac arrest immediately after ETI attempt | 17 (3.2) |
| Recorded regurgitation | 27 (5.0) |
| ETI failure rescued by emergency surgical airway | 7 (1.3) |
| Dental trauma | 8 (1.5) |
| Cuff leak requiring reintubation | 5 (0.9) |
| Mainstem bronchus intubation | 46 (8.6) |
Data are expressed as n (%). ETI: endotracheal intubation.
3.2. Possible Risk Factors for Endotracheal Intubation-Related Complications
Table 2 compares the clinical demographics of patients who experienced ETI-related complications versus those who did not. Patients who experienced ETI-related complications were more likely to have higher scores for anatomic severity scales (ISS, P = 0.005; AIS head or neck, P = 0.036), lower scores for physiological severity scales (GCS, P < 0.001; RTS, P < 0.001), and higher heart rate (P = 0.011) than those without complications. The occurrence of ETI-related complications was significantly higher in the prehospital setting (crude OR, 1.75; 95% CI, 1.13–2.70; P = 0.011) and in patients who needed three or more ETI attempts (crude OR, 21.53; 95% CI, 4.75–97.6; P < 0.001). Rapid-sequence intubation technique was used in 34.9% of patients who experienced airway complications and in 51.1% of patients who did not.
Imbalanced characteristics (variables in Table 2 with P < 0.15) were entered into a multivariable model, which revealed that the independent predictors of ETI-related complications in injured patients were GCS (adjusted odds ratio [AOR], 0.93; 95% confidence interval [CI], 0.88–0.98; P = 0.009), heart rate (AOR, 1.01; 95% CI, 1.00–1.02; P = 0.023), and three or more ETI attempts (AOR, 15.71; 95% CI, 3.37–73.2; P < 0.001) (Table 3). The Hosmer–Lemeshow test verified the good fit of this model (P = 0.139); the c statistic for this logistic model was 0.704, suggesting acceptable discrimination. The use of rapid-sequence intubation technique was associated with a lower risk of airway-related complications on crude analysis (crude OR, 0.51; 95% CI, 0.34–0.78; P = 0.002). A similar association remained on adjusted analysis, although it did not reach statistical significance (AOR, 0.67; 95% CI, 0.41–1.08; P = 0.099).
Table 3.
Logistic regression models for occurrence of airway-related complications in injured patients.
| Univariable analysis | Multivariable analysis a | |||
|---|---|---|---|---|
| Crude OR (95% CI) | P value | AOR (95% CI) | P value | |
| Prehospital ETI | 1.75 (1.13–2.70) | 0.011 | 0.99 (0.58–1.66) | 0.955 |
| Male | 0.72 (0.47–1.09) | 0.121 | 0.64 (0.41–1.01) | 0.053 |
| Rapid-sequence intubation | 0.51 (0.34–0.78) | 0.002 | 0.67 (0.41–1.08) | 0.099 |
| AIS head or neck | 1.10 (1.00–1.21) | 0.041 | - | - |
| ISS | 1.02 (1.01–1.03) | 0.002 | 1.01 (1.00–1.02) | 0.161 |
| GCS | 0.90 (0.86–0.95) | < 0.001 | 0.93 (0.88–0.98) | 0.009 |
| RTS | 0.82 (0.73–0.92) | 0.001 | - | - |
| Ps | 0.33 (0.18–0.58) | < 0.001 | - | - |
| Heart rate | 1.01 (1.00–1.02) | 0.022 | 1.01 (1.00–1.02) | 0.023 |
| Respiratory rate | 1.01 (0.99–1.03) | 0.230 | 1.01 (0.99–1.04) | 0.203 |
| Three or more ETI attempts | 21.53 (4.75–97.6) | < 0.001 | 15.71 (3.37–73.2) | < 0.001 |
| Pulse oximetry saturation | 1.00 (0.99–1.00) | 0.389 | 1.00 (0.99–1.01) | 0.733 |
AIS: Abbreviated Injury Scale, AOR: adjusted odds ratio, CI: confidence interval, ED: emergency department, ETI: endotracheal intubation, GCS: Glasgow Coma Scale Score, ISS: Injury Severity Score, OR: odds ratio, Ps: probability of survival, RTS: Revised Trauma Score.
aAdjustment for all variables included in the table. The patient group that did not experience ETI-related complication was the reference set.
Good fit was verified with the Hosmer–Lemeshow test (P = 0.139). The c statistic for the model was 0.704. “AIS head or neck” was not used as an explanatory variable because of its strong correlation with GCS. RTS is a weighted physiological scoring system consisting of the GCS, systolic blood pressure, and respiratory rate. Therefore, RTS was not included as an explanatory variable in this model. Ps was not included because it is calculated from ISS, RTS, and age.
3.3. Endotracheal Intubation-Related Complications Independently Worsened the Survival of Trauma Patients
A second multivariable logistic regression analysis showed that ETI-related complications decreased the likelihood of survival of trauma patients (AOR, 0.60; 95% CI, 0.38–0.95; P = 0.030), independently of age, male sex, ISS, GCS, and off-hours presentation (Table 4). The Hosmer–Lemeshow test verified the good fit of this model (P = 0.161); the c statistic for this logistic model was 0.784, suggesting acceptable discrimination.
Table 4.
Logistic regression models of factors associated with survival in trauma patients who received ETI in the prehospital setting or ED.
| Univariable analysis | Multivariable analysis a | ||||
|---|---|---|---|---|---|
| Crude OR (95% CI) | P value | AOR (95% CI) | P value | ||
| ETI-related adverse events | 0.46 (0.31–0.69) | < 0.001 | 0.60 (0.38–0.95) | 0.030 | |
| Age | 0.98 (0.97–0.99) | < 0.001 | 0.98 (0.97–0.98) | < 0.001 | |
| Male | 1.06 (0.73–1.55) | 0.744 | 0.95 (0.61–1.47) | 0.814 | |
| ISS | 0.95 (0.94–0.97) | < 0.001 | 0.96 (0.95–0.97) | < 0.001 | |
| GCS | 1.18 (1.13–1.23) | < 0.001 | 1.16 (1.10–1.21) | < 0.001 | |
| Off-hoursb presentation | 0.87 (0.61–1.24) | 0.439 | 0.74 (0.49–1.13) | 0.160 | |
ETI-related complications independently worsened the survival of trauma patients.
AOR: adjusted odds ratio, CI: confidence interval, ED: emergency department, ETI: endotracheal intubation, GCS: Glasgow Coma Scale Score, ISS: Injury Severity Score, OR: odds ratio.
aAdjustment for all variables included in the table. Good fit was verified with the Hosmer–Lemeshow test (P = 0.161). The c statistic for the model was 0.784.
b6:01 PM to 8:00 AM on weekdays plus all weekend hours.
4. Discussion
In this study of trauma patients who underwent expert-performed ETI for airway compromise, severe complications were common and were associated with low GCS, elevated heart rate, and the need for three or more ETI attempts. We also found that ETI-related complications decreased the likelihood of survival of trauma patients, independently of age, sex, anatomic severity, and physiological severity.
Our data showed that even laryngoscopists with expert status [10] may frequently be confronted with severe ETI-related complications in both the prehospital and ED settings. Our results suggest that trauma airway management carries a very high risk; therefore, our findings serve as a caution to healthcare professionals involved in this procedure. Although this study did not directly address this issue, we believe that the experience of the laryngoscopist should be considered when performing ETI in injured patients. Previous studies have indicated that prehospital ETI performed by paramedics with limited experience results in twice the rate of esophageal intubation as ETI performed by experienced physicians [31–34]. Reported overall prehospital ETI success rates in patients with trauma are 68% for paramedics [31] and 99.3% for trauma anesthesiologists [9]. This ETI success rate for anesthesiologists was comparable with our data (98.7% success rate). A previous study [35] and a recent meta-analysis [36] also showed that the provider's degree of ETI experience significantly influenced the outcomes of injured patients. In addition, Paal et al. [37] and the Scandinavian Society for Anaesthesiology and Intensive Care Medicine [38] recommend that ETI in high risk populations should be delegated to skilled laryngoscopists.
We also found that low GCS, elevated heart rate, and multiple ETI attempts were potential risk factors for ETI-related complications. Higher heart rate and lower GCS may reflect the lower physiological reserve of injured patients, which predisposes them to airway-related complications. Our findings highlight the need for care providers to be especially vigilant in treating such patients.
Consistent with previous reports [23, 24, 27], repeated attempts at laryngoscopy were associated with ETI-related complications in our trauma cohort. This finding supports the use of strategies to limit the number of laryngoscopy attempts and maximize first-pass laryngoscopy success when performing ETI, such as optimal positioning and use of airway management adjuncts (e.g., gum elastic bougie or video laryngoscopy) [23].
Crude analysis in the present study showed that the use of rapid-sequence intubation technique was associated with a lower risk of airway-related complications in injured patients. A similar association remained after adjustment for injury and physiological severity, although it did not reach statistical significance. Previous studies have documented the associations between the use of rapid-sequence intubation and high ETI success rates [22, 39–41] and low complication rates [42]. Our data corroborate these findings and expand them to include a different patient population and practice setting. Along with the existing literature, our findings support the current practice guideline [43, 44], which recommends rapid-sequence intubation as the initial method of emergency airway management in most trauma patients.
Finally, we found that ETI-related complications decreased the likelihood of survival of trauma patients, independently of anatomic severity and physiological reserve, in both the prehospital setting and the ED. Therefore, all healthcare professionals should be aware that any airway-related complication increases the risk of further harm in trauma patients. Although this study was unable to confirm the hypothesis, it is possible that a considerable proportion of observed complications might have been avoided. Jaber et al. [45] recently reported that the introduction of an “intubation bundle,” including preoxygenation, rapid-sequence intubation, and capnography to verify correct tube placement, significantly decreased the number of ETI-related complications in critically ill patients. In many Japanese EDs, including our own, procedural preferences for ETI vary greatly [46] and a standardized procedure is lacking. To reduce ETI-related complications, a standard operating procedure [19] for ETI in trauma patients should be implemented (e.g., unified equipment set-up, rapid-sequence intubation, and postintubation care with end-tidal CO2 detection) in both the prehospital setting and ED. We believe that implementing standardized procedures will improve the outcomes of trauma patients.
4.1. Limitations and Strengths
This study had three major limitations. First, its retrospective nature may have increased the risk of bias, including self-reporting and diagnostic biases. Despite the use of structured medical records and a quality assurance database that captured all severe ETI-related complications occurring in both prehospital and ED settings, ETI complications may have been missed, underestimated, or misclassified.
Second, although multivariable logistic regression analysis indicated that GCS, heart rate, and the need for three or more ETI attempts were potential risk factors for ETI-related complications, there may have been other, unknown confounders for ETI-related complications, as can occur in any observational study. For example, board certification in anesthesiology of the operators and the use of a video laryngoscope [47, 48] or capnometry [49] may have affected the rate of ETI success and ETI-related complications. However, our database did not record these variables. There were also substantial differences in characteristics between patients who experienced airway-related complications and those who did not. Although we rigorously adjusted for these differences to detect independent predictors of airway-related complications, there remains a risk of incomplete adjustment. For example, ISS has been shown to underestimate multiple severe injuries within the same body region [50]. It might have been useful to use the new ISS (the sum of squares of the three most severe injuries, regardless of the body regions injured) [51] instead of the ISS; however, we did not record this variable.
Third, while our ED is typical of a Japanese teaching hospital, as with any single-center study, it may not be possible to extrapolate our findings to other medical institutions, especially those in other countries.
Despite these limitations, this study also had several strengths. First, our study clarified the incidence and risk factors for ETI-related complications in trauma patients when expert laryngoscopists performed ETI in the ED and prehospital settings. Our hospital's anesthesiologists have long been in charge of trauma airway management in both locations. To the best of our knowledge, past studies have not provided such information. Second, because we used structured ED records and our department has a rigorous peer-review process supervised by its director, there were no missing data. We therefore believe that our study provides an accurate depiction of advanced airway management by expert laryngoscopists in trauma patients in prehospital and ED settings.
5. Conclusion
In this study of trauma patients who underwent expert-performed ETI for airway compromise, severe ETI-related adverse events were common and were associated with low GCS, elevated heart rate, and repeated ETI attempts. The occurrence of these airway-related complications decreased the likelihood of survival of injured patients, independently of anatomic severity and physiological reserve. These data have implications for the practice of airway management in trauma patients in the prehospital setting and ED.
Acknowledgments
The authors wish to thank their colleagues at Ohta Nishinouchi Hospital for data acquisition. They also thank Nozomi Ono, M.D. (Department of Psychiatry, Hoshigaoka Hospital, Koriyama, Japan), for assistance in reviewing the manuscript and Anne M. O'Rourke, Ph.D., and Rebecca Tollefson, D.V.M., from Edanz Group (http://www.edanzediting.com/ac) for editing drafts of this manuscript.
Data Availability
All data relevant to the study are included in this published article. Further datasets analyzed during the study are available from the corresponding author on reasonable request.
Disclosure
The current affiliation of Takeyasu Kakamu is Section of Environment and Radiation, International Agency for Research on Cancer, 150 Cours Albert Thomas, 69372 Lyon CEDEX 08, France.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- 1.Corso P., Finkelstein E., Miller T., Fiebelkorn I., Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Injury Prevention. 2006;12(4):212–218. doi: 10.1136/ip.2005.010983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thornhill S., Teasdale G. M., Murray G. D., McEwen J., Roy C. W., Penny K. I. Disability in young people and adults one year after head injury: prospective cohort study. British Medical Journal. 2000;320(7250):1631–1635. doi: 10.1136/bmj.320.7250.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lockey D. J., Healey B., Crewdson K., Chalk G., Weaver A. E., Davies G. E. Advanced airway management is necessary in prehospital trauma patients. British Journal of Anaesthesia. 2015;114(4):657–662. doi: 10.1093/bja/aeu412. [DOI] [PubMed] [Google Scholar]
- 4.Esposito T. J., Sanddal N. D., Dean J. M., Hansen J. D., Reynolds S. A., Battan K. Analysis of preventable pediatric trauma deaths and inappropriate trauma care in Montana. Journal of Trauma. 1999;47(2):243–253. doi: 10.1097/00005373-199908000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Von Elm E., Schoettker P., Henzi I., Osterwalder J., Walder B. Pre-hospital tracheal intubation in patients with traumatic brain injury: Systematic review of current evidence. British Journal of Anaesthesia. 2009;103(3):371–386. doi: 10.1093/bja/aep202. [DOI] [PubMed] [Google Scholar]
- 6.Bushra J. S., McNeil B., Wald D. A., Schwell A., Karras D. J. A Comparison of Trauma Intubations Managed by Anesthesiologists and Emergency Physicians. Academic Emergency Medicine. 2004;11(1):66–70. doi: 10.1197/j.aem.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Ono Y., Yokoyama H., Matsumoto A., Kumada Y., Shinohara K., Tase C. Surgical airways for trauma patients in an emergency surgical setting: 11 years' experience at a teaching hospital in Japan. Journal of Anesthesia & Clinical Research. 2013;27(6):832–837. doi: 10.1007/s00540-013-1640-6. [DOI] [PubMed] [Google Scholar]
- 8.Lockey D. J., Coats T., Parr M. J. A. Aspiration in severe trauma: A prospective study. Anaesthesia. 1999;54(11):1097–1098. doi: 10.1046/j.1365-2044.1999.00754.x. [DOI] [PubMed] [Google Scholar]
- 9.Lockey D., Crewdson K., Weaver A., Davies G. Observational study of the success rates of intubation and failed intubation airway rescue techniques in 7256 attempted intubations of trauma patients by pre-hospital physicians. British Journal of Anaesthesia. 2014;113(2):220–225. doi: 10.1093/bja/aeu227. [DOI] [PubMed] [Google Scholar]
- 10.Breckwoldt J., Klemstein S., Brunne B., Schnitzer L., Arntz H.-R., Mochmann H.-C. Expertise in prehospital endotracheal intubation by emergency medicine physicians-Comparing 'proficient performers' and 'experts'. Resuscitation. 2012;83(4):434–439. doi: 10.1016/j.resuscitation.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Committee on Medical Aspects of Automotive Safety. Rating the severity of tissue damage: I. The abbreviated scale. JAMA. 1971;215:277–280. doi: 10.1001/jama.1971.03180150059012. [DOI] [PubMed] [Google Scholar]
- 12.Baker S. P., O'Neill B., Haddon W., Jr., Long W. B. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. The Journal of Trauma and Acute Care Surgery. 1974;14(3):187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Champion H. R., Sacco W. J., Copes W. S., Gann D. S., Gennarelli T. A., Flanagan M. E. A revision of the trauma score. Journal of Trauma - Injury Infection and Critical Care. 1989;29(5):623–629. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Boyd C. R., Tolson M. A., Copes W. S. Evaluating trauma care: The TRISS method. Journal of Trauma - Injury Infection and Critical Care. 1987;27(4):370–378. doi: 10.1097/00005373-198704000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Champion H. R., Copes W. S., Sacco W. J., et al. The major trauma outcome study: Establishing national norms for trauma care. Journal of Trauma - Injury Infection and Critical Care. 1990;30(11):1356–1365. doi: 10.1097/00005373-199011000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Charlson M. E., Pompei P., Ales K. L., MacKenzie C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Japanese Society of Anesthesiologistsm. JSA airway management guideline 2014: to improve the safety of induction of anesthesia. Journal of Anesthesia & Clinical Research. 2014;28(4):482–493. doi: 10.1007/s00540-014-1844-4. [DOI] [PubMed] [Google Scholar]
- 18.Apfelbaum J. L., Hagberg C. A., Caplan R. A., et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251–270. doi: 10.1097/aln.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 19.Sherren P. B., Tricklebank S., Glover G. Development of a standard operating procedure and checklist for rapid sequence induction in the critically ill. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2014;22(41) doi: 10.1186/s13049-014-0041-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Helling T. S., Nelson P. M., Shook J. W., Lainhart K., Kintigh D. The presence of in-house attending trauma surgeons does not improve management or outcome of critically injured patients. Journal of Trauma. 2003;55(1):20–25. doi: 10.1097/01.TA.0000071621.39088.7B. [DOI] [PubMed] [Google Scholar]
- 21.Ono Y., Sugiyama T., Chida Y., et al. Association between off-hour presentation and endotracheal-intubation-related adverse events in trauma patients with a predicted difficult airway: A historical cohort study at a community emergency department in Japan. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2016;24(1):p. 106. doi: 10.1186/s13049-016-0296-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walls R. M., Brown C. A., III, Bair A. E., Pallin D. J. Emergency airway management: a multi-center report of 8937 Emergency Department intubations. The Journal of Emergency Medicine. 2011;41(4):347–354. doi: 10.1016/j.jemermed.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 23.Hasegawa K., Shigemitsu K., Hagiwara Y., et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Annals of Emergency Medicine. 2012;60(6):749–e2. doi: 10.1016/j.annemergmed.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Mort T. C. Emergency Tracheal Intubation: Complications Associated with Repeated Laryngoscopic Attempts. Anesthesia & Analgesia. 2004;99:607–613. doi: 10.1213/01.ANE.0000122825.04923.15. [DOI] [PubMed] [Google Scholar]
- 25.Cook T. M., Woodall N., Harper J., Benger J. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. British Journal of Anaesthesia. 2011;106(5):632–642. doi: 10.1093/bja/aer059. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt U. H., Kumwilaisak K., Bittner E., George E., Hess D. Effects of supervision by attending anesthesiologists on complications of emergency tracheal intubation. Anesthesiology. 2008;109(6):973–977. doi: 10.1097/ALN.0b013e31818ddb90. [DOI] [PubMed] [Google Scholar]
- 27.Martin L. D., Mhyre J. M., Shanks A. M., Tremper K. K., Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011;114(1):42–48. doi: 10.1097/ALN.0b013e318201c415. [DOI] [PubMed] [Google Scholar]
- 28.Bergeron E., Rossignol M., Osler T., Clas D., Lavoie A. Improving the TRISS Methodology by Restructuring Age Categories and Adding Comorbidities. Journal of Trauma - Injury Infection and Critical Care. 2004;56(4):760–767. doi: 10.1097/01.TA.0000119199.52226.C0. [DOI] [PubMed] [Google Scholar]
- 29.Zhu Z., Shang X., Qi P., Ma S. Sex-based differences in outcomes after severe injury: An analysis of blunt trauma patients in China. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2017;25(1):p. 47. doi: 10.1186/s13049-017-0389-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bell C. M., Redelmeier D. A. Mortality among patients admitted to hospitals on weekends as compared with weekdays. The New England Journal of Medicine. 2001;345(9):663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 31.Cobas M. A., De La Peña M. A., Manning R., Candiotti K., Varon A. J. Prehospital intubations and mortality: A level 1 trauma center perspective. Anesthesia & Analgesia. 2009;109(2):489–493. doi: 10.1213/ane.0b013e3181aa3063. [DOI] [PubMed] [Google Scholar]
- 32.Timmermann A., Russo S. G., Eich C., et al. The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians. Anesthesia & Analgesia. 2007;104(3):619–623. doi: 10.1213/01.ane.0000253523.80050.e9. [DOI] [PubMed] [Google Scholar]
- 33.Jemmett M. E., Kendal K. M., Fourre M. W., Burton J. H. Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting. Acad Emerg Med. 2003;10:961–965. doi: 10.1111/j.1553-2712.2003.tb00652.x. [DOI] [PubMed] [Google Scholar]
- 34.Katz S. H., Falk J. L. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Annals of Emergency Medicine. 2001;37(1):32–37. doi: 10.1067/mem.2001.112098. [DOI] [PubMed] [Google Scholar]
- 35.Wang H. E., Peitzman A. B., Cassidy L. D., Adelson P. D., Yealy D. M. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Annals of Emergency Medicine. 2004;44(5):439–450. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 36.Bossers S. M., Schwarte L. A., Loer S. A., Twisk J. W. R., Boer C., Schober P. Experience in prehospital endotracheal intubation significantly influences mortality of patients with severe traumatic brain injury: A systematic review and meta-analysis. PLoS ONE. 2015;10(10) doi: 10.1371/journal.pone.0141034.e0141034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paal P., Herff H., Mitterlechner T., et al. Anaesthesia in prehospital emergencies and in the emergency room. Resuscitation. 2010;81(2):148–154. doi: 10.1016/j.resuscitation.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 38.Berlac P., Hyldmo P. K., Kongstad P. Pre-hospital airway management: guidelines from a task force from the Scandinavian Society for Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiologica Scandinavica. 2008;52(7):897–907. doi: 10.1111/j.1399-6576.2008.01673.x. [DOI] [PubMed] [Google Scholar]
- 39.Bozeman W. P., Kleiner D. M., Huggett V. A comparison of rapid-sequence intubation and etomidate-only intubation in the prehospital air medical setting. Prehospital Emergency Care. 2006;10(1):8–13. doi: 10.1080/10903120500366854. [DOI] [PubMed] [Google Scholar]
- 40.Kim C., Kang H. G., Lim T. H., Choi B. Y., Shin Y.-J., Choi H. J. What factors affect the success rate of the first attempt at endotracheal intubation in emergency departments? Emergency Medicine Journal. 2013;30(11):888–892. doi: 10.1136/emermed-2012-201708. [DOI] [PubMed] [Google Scholar]
- 41.Okubo M., Gibo K., Hagiwara Y., Nakayama Y., Hasegawa K. The effectiveness of rapid sequence intubation (RSI) versus non-RSI in emergency department: an analysis of multicenter prospective observational study. International Journal of Emergency Medicine. 2017;10(1) doi: 10.1186/s12245-017-0129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li J., Murphy-Lavoie H., Bugas C., Martinez J., Preston C. Complications of emergency intubation with and without paralysis. The American Journal of Emergency Medicine. 1999;17(2):141–144. doi: 10.1016/S0735-6757(99)90046-3. [DOI] [PubMed] [Google Scholar]
- 43.Dunham M. C., Barraco R. D., Clark D. E., et al. Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury. The Journal of Trauma: Injury, Infection, and Critical Care. 2003;55(1):162–179. doi: 10.1097/01.ta.0000083335.93868.2c. [DOI] [PubMed] [Google Scholar]
- 44.Mayglothling J., Duane T. M., Gibbs M., et al. Emergency tracheal intubation immediately following traumatic injury: an eastern association for the surgery of trauma practice management guideline. The Journal of Trauma and Acute Care Surgery. 2012;73(5):S333–S340. doi: 10.1097/ta.0b013e31827018a5. [DOI] [PubMed] [Google Scholar]
- 45.Jaber S., Jung B., Corne P., et al. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Intensive Care Medicine. 2010;36(2):248–255. doi: 10.1007/s00134-009-1717-8. [DOI] [PubMed] [Google Scholar]
- 46.Hasegawa K., Hagiwara Y., Chiba T., et al. Emergency airway management in Japan: Interim analysis of a multi-center prospective observational study. Resuscitation. 2012;83(4):428–433. doi: 10.1016/j.resuscitation.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 47.Sakles J. C., Mosier J., Chiu S., Cosentino M., Kalin L. A comparison of the C-MAC video laryngoscope to the macintosh direct laryngoscope for intubation in the emergency department. Annals of Emergency Medicine. 2012;60(6):739–748. doi: 10.1016/j.annemergmed.2012.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aziz M. F., Dillman D., Fu R., Brambrink A. M. Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology. 2012;116(3):629–636. doi: 10.1097/aln.0b013e318246ea34. [DOI] [PubMed] [Google Scholar]
- 49.Silvestri S., Ralls G. A., Krauss B., et al. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Annals of Emergency Medicine. 2005;45(5):497–503. doi: 10.1016/j.annemergmed.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 50.Smith B. P., Goldberg A. J., Gaughan J. P., Seamon M. J. A comparison of Injury Severity Score and New Injury Severity Score after penetrating trauma: A prospective analysis. Journal of Trauma and Acute Care Surgery. 2015;79(2):269–274. doi: 10.1097/TA.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 51.Osler T., Baker S. P., Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. Journal of Trauma - Injury Infection and Critical Care. 1997;43(6):922–926. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in this published article. Further datasets analyzed during the study are available from the corresponding author on reasonable request.


