Abstract
[Purpose] To investigate the effect of vitamin D supplementation on rehabilitation outcomes and balance in patients having hemiplegia due to ischemic stroke. [Subjects and Methods] Vitamin D levels of 132 patients hospitalized for hemiplegia rehabilitation due to ischemic stroke were tested. Consequently, 86/132 patients had low vitamin D levels, 72 of which met the inclusion criteria and were included in the study. Patients were divided into two groups: Group A (injected with 300,000 IU vitamin D), and Group B (injected intramuscularly with saline). Each patient was tested at the baseline and at the third month using the Brunnstrom recovery staging, functional ambulation scale, modified Barthel index, and Berg balance scale. The findings were compared between the groups. [Results] By the end of the third month, The Berg balance scale results and modified Barthel index scores significantly differed between the two groups, whereas Brunnstrom recovery staging and functional ambulation scale test results did not. [Conclusion] This study found that vitamin D administration increased the activity levels and accelerated balance recovery but did not significantly affect ambulation or motor recovery. These results warrant confirmation by longer follow-up studies with a larger number of participants.
Key words: Vitamin D, Hemiplegia, Rehabilitation and balance outcomes
INTRODUCTION
Strokes are one of the most common causes of disability in the world, and the most common occurrence after stroke is hemiplegia. In hemiplegic patients, vitamin D deficiency is a common health problem1, 2). Immobility, old age, and the resulting reduced dietary intake, decreased exposure to daylight, reduced production capacity of the skin, reduced absorption from the intestines, and kidney hydroxylation have been identified as its causes3, 4).
Low vitamin D levels increase the risk of ischemic stroke1). Maintaining vitamin D at normal levels reportedly reduces stroke risk and improves balance and muscle function in lower extremities1, 2). Thus, in this context, our study investigating the role of vitamin D supplementation in the management of patients having hemiplegia due to ischemic stroke is significant. Herein, we aimed to investigate the effect of vitamin D supplementation on rehabilitation outcomes and balance in hemiplegic patients with vitamin D deficiency.
SUBJECTS AND METHODS
The study was a randomized, double-blind, placebo-controlled study and included 132 patients with hemiplegia due to ischemic stroke who were hospitalized for neurological rehabilitation between September 2014 and March 2015 in Erenkoy Physical Therapy and Rehabilitation Hospital Of these patients, 86/132 had low D vitamin levels (winter season measurement, <30 ng/ml), and 72 of these 86 patients met the inclusion criteria (stated below). Patients were divided into two groups: the vitamin D-injected group (Group A) and the saline-injected control group (Group B).
The inclusion criteria were hospitalization for hemiplegia rehabilitation, no history of cerebrovascular disease, ischemic etiology of stroke, and a gap of at least 2 months having passed since the last stroke. The exclusion criteria were as follows: having an end-stage disease (cancer) or a disease other than stroke that may affect balance or ambulation (e.g., multiple sclerosis, Parkinson’s disease, or pelvic and lower limb surgery), constrain sun exposure (e.g., vitiligo and psoriasis), or affect vitamin D levels (e.g., chronic renal failure and celiac disease).
Data pertaining to the following clinical features were recorded by data entry staff without specifying group information: sociodemographic data, Brunnstrom recovery staging (BRS), functional ambulation scale (FAS), modified Barthel index (MBI) scores, Berg balance scale (BBS), and vitamin D levels. All patients provided written informed consent. Ethics committee approval was obtained from Yeditepe University Medical Faculty (Approval number: 0197/2012) before the study proceeded. The study has been reported as per the CONSORT 2010 guidelines.
At the beginning of the study, patients in Group A were injected intramuscularly with 300,000 IU vitamin D in 2 ml of liquid and those in Group B were injected intramuscularly with 2 ml of physiological saline. Each patient was assessed by an independent physiatrist with the BRS test for motor evaluation, FAS for ambulation, MBI for mobility and daily life activities, and BBS for balance on the day of being included in the study and 3 months after this date.
Measurement of 25 (OH) vitamin D3 was performed with an RIA CT kit (BioSource Europe SA, Nivelles, Belgium) using a radioimmunoassay method. A 25 (OH) vitamin D3 level >30 ng/ml was considered normal. Patients were only admitted during the fall–winter period (from September to February) to prevent the effects of seasonal differences on vitamin D levels.
The Berg Balance Scale is a 14-item assessment tool used to evaluate the balance and fall risk. Each item is scored between 0 (minimum) and 4 (maximum). Higher scores indicate better balance5, 6). The MBI comprises 10 items relating to daily activities and mobility. Scoring depends on whether the patient gets help while performing these functions. The highest score (100) indicates that the person is completely physically independent while performing these functions, whereas the minimum score (0) indicates complete dependence. Patients are assessed at five levels7). The FAS comprises six stages. Stage 5 shows independent ambulation, while Stage 0 shows non-functional ambulation8). Brunnstrom Recovery Staging assesses the level of motor function in hemiplegic patients. Healing stages are classified into six; on Stage 1, flaccidity is present and no movements of the part can be initiated, whereas Stage 6 shows normal function9).
Statistical analyses were done with the use of with SPSS version 20.0 for Windows (SPSS Inc., Chicago, IL, USA) package program. In addition to descriptive statistical methods, group comparisons of non-normally distributed variables were done using independent t-test. A p value <0.05 was considered statistically significant.
Patient grouping information and measurement results were collected by the data entry staff after the third-month evaluation was completed.
The sample size was determined by the power analysis method. No secondary analysis was performed. A simple randomization method was used in this study. Patients considered eligible to participate in the study were listed; the patients who had an odd a sequence number were taken into one group, and the others were taken into the other group. Sequence randomization was performed by a service nurse who was given information only about the grouping, without detailed knowledge of the study content. The service nurse prepared the injection only with the knowledge of the group the individual belonged to, and another nurse who did not have group information injected the prepared injections. The data records of the participants were kept by data entry staff that had no information about the contents of the study. After the patient evaluations were completed, the participants’ grouping information was reported to the data entry staff by the relevant nurse.
RESULTS
Thirty-six patients were randomly assigned to each group. Three patients from Group A and two from Group B were transferred to other hospitals due to other health problems. The planned injection was given to 33 patients from Group A and 34 patients from Group B. We excluded two patients in Group A and one patient in Group B from the study due to not participating in the follow-up (Fig. 1).
Fig. 1.
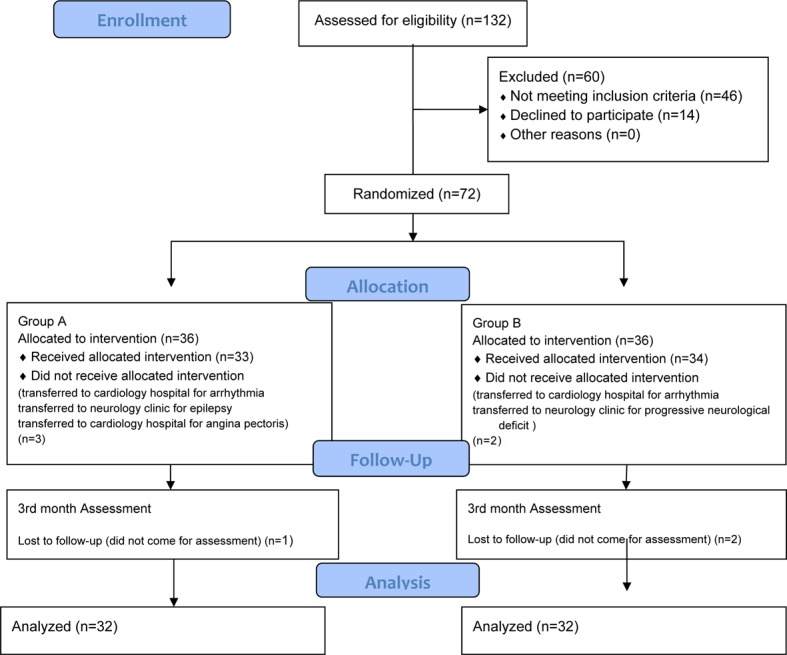
CONSORT 2010 flow diagram of the study.
The study was conducted between September 2014 and March 2015. Each patient was rehabilitated for 3 months after the injection, and rehabilitation and balance evaluations were made at the end of the third month. Basic demographic and clinical data are shown in Table 1.
Table 1. Basic demographic and clinical data.
| Group A n=32 | Group B n=32 | |
| Age (year) | 69.84 ± 10.09 | 66.930 ± 10.053 |
| Gender | ||
| Female | 15 (46.8%) | 14 (43.8%) |
| Male | 17 (53.2%) | 18 (56.2%) |
| Duration after stroke (months) | 4.78 ± 1.86 | 4.28 ± 1.09 |
| Vitamin D (ng/ml) | 13.93 ± 4.58 | 16.06 ± 5.60 |
| PTH (ng/l) | 60.17± 22.83 | 56.18 ± 29.76 |
| ALP (IU/l) | 209.16 ± 67.44 | 197.53 ± 40.96 |
| Ca (mmol/l) | 8.99 ± 0.45 | 8.94 ± 0.43 |
| P (mmol/l) | 3.48 ± 0.51 | 3.38 ± 0.75 |
The continuous variables are expressed as mean ± standard error of mean (SEM); the categorical variables are expressed as numbers (n) and percentage (%).
Comparisons of the rehabilitation outcomes and balance are shown in Table 2. During the baseline and third months, the results of the BRS for the upper extremity, hand, and lower extremity evaluations did not statistically significantly differ between Groups A and B. Although MBI did not significantly differ (p=0.148) between the two groups at the beginning of the study, by the end of the 3rd month, a statistically significant difference was evident (p<0.001). The baseline (p=0.817) and third-month statistics (p=0.018) of the FAS did not significantly differ between the groups. Although there was no statistically significant difference between the two groups at the beginning of the (p=0.436), there was a statistically significant difference between them by the end of the third month (p<0.001).
Table 2. Comparison of rehabilitation outcomes and balance between groups A and B.
| Group A (mean ± SD) | Group B (mean ± SD) | p | |
| BRS upper extremity Baseline | 1.91 ± 0.86 | 1.66 ± 0.65 | 0.194 |
| BRS upper extremity 3rd month | 2.25 ± 0.92 | 1.84 ± 0.81 | 0.065 |
| BRS lower extremity Baseline | 3.09 ± 0.99 | 3.34 ± 5.28 | 0.794 |
| BRS lower extremity 3rd month | 3.59 ± 0.87 | 3.12 ± 0.79 | 0.028 |
| BRS hand Baseline | 1.28 ± 0.58 | 1.34 ± 0.48 | 0.641 |
| BRS hand 3rd month | 1.62 ± 0.66 | 1.69 ± 0.78 | 0.731 |
| MBI Baseline | 40.96 ± 24.58 | 32.5 ± 21.51 | 0.148 |
| MBI 3rd month | 59.18 ± 22.15 | 41.87 ± 20.42 | 0.002 |
| FAS Baseline | 0.97 ± 1.18 | 0.91 ± 0.96 | 0.817 |
| FAS 3rd month | 2.34 ± 1.31 | 1.60 ± 1.16 | 0.018 |
| BBT Baseline | 21.84 ± 16.17 | 18.88 ± 14.07 | 0.436 |
| BBT 3rd month | 38.72 ± 14.14 | 24.75 ± 14.76 | 0.000 |
BRS: Brunnstrom Recovery Staging; MBI: Modified Barthel Index; FAS: Functional Ambulation Scale; BBS: Berg balance scale. p<0.05 was significant.
DISCUSSION
The treatment of vitamin D deficiency is quite easy, inexpensive, and safe. Vitamin D levels in elderly have been associated with decreased muscle strength, balance, and physical performance. As the majority of the hemiplegic patients are elderly, a specific investigation on this topic focusing on the elderly was warranted10, 11). In this study, we investigated the association of vitamin D administration with balance and rehabilitation outcomes in ischemic hemiplegic patients and found that vitamin D administration improved the mobility and daily life activities with accelerated balance recovery. Our study is the first double-blind, randomized controlled study carried out in this regard.
The effect of calcium plus D vitamin administration on ischemic stroke outcomes was previously investigated by Gupta et al12). In acute phase evaluations, decreases in disability and mortality were found among some other improvements. Another study assessed if there was a correlation between stroke patients’ vitamin D levels and age, duration of illness, and functional independence scale scores and found no correlation13). Based on rehabilitation outcome evaluations in this study, although no improvement in the BRS assessment and FAS outcomes was observed after vitamin D supplementation, a significant improvement was observed in the MBI scores (in terms of daily living activities and mobility) and BBS scores.
In post-stroke hemiplegic patients, vitamin D supplementation has been shown to increase muscle strength, thus reducing falls and associated fractures14). Our findings support the notion that reduced falling and the associated reduction of fractures are not only related to increased muscle strength but may also be related to the effect of vitamin D on maintaining body balance.
Several studies have examined the relationship between vitamin D levels and balance. However, to our knowledge, our study is the first to investigate this relationship in patients having hemiplegia due to ischemic stroke. Some of the previous studies have reported a positive contribution of vitamin D to balance10, 15) whereas some reported no such effect of vitamin D16). In a study of healthy middle-aged subjects, no correlation was found between vitamin D and balance17). A study on osteoporotic patients found that balance scores were significant in patients with low vitamin D levels18). In a systematic review and meta-analysis conducted to investigate the effect of vitamin D supplementation on balance in elderly individuals, vitamin D supplementation of 800–1,000 IU per day was found to have beneficial effects on balance1). In a study conducted in women aged >60 years, balance control was found to be better in patients with 25 (OH) vitamin D levels above 50 nmol/l than in those with the levels <50 nmol/l2). Unlike some previous studies, in our study, we did not investigate the relationship between balance and direct vitamin D levels; we instead investigated how balance scores changed with vitamin D supplementation in patients with vitamin D deficiency; consequently, those who received vitamin D supplementation showed more improvement than those who did not receive supplementation. There are some hypotheses on the mechanism, by which vitamin D is effective on balance17, 18). Although the underlying mechanisms of several effects of vitamin D on balance and neuromuscular functions are still not fully understood, it is believed to be associated with the muscle cells that regulate the muscle membrane phospholipid metabolism and the flow of calcium19,20,21).
The relationship between vitamin D and the quality of life has been investigated for different diseases in previous studies. In a cross-sectional study of 350 patients with hip fractures, Di Monaco et al. found a significant correlation between vitamin D and the Barthel index scores, which was used as a functional improvement indicator22). Another study revealed a correlation between low vitamin D levels in elderly patients who needed home care and decreased activities of daily living23). In the present study, MBI and FAS were used to evaluate the daily activities, mobility, and ambulation status of the patients, and the association between these and vitamin D supplementation was investigated. We found better MBI scores after vitamin D supplementation in hemiplegic patients. There was no significant association between FAS values with vitamin D supplementation in hemiplegic patients. Previous studies have investigated the relationships of vitamin D levels with the quality of life and ambulation. In a study, 236 patients aged ≥65 years with hemiplegia were monitored for 2 years, and a correlation of vitamin D levels with Barthel index scores and muscle strength of the non-hemiplegic side was observed14). In a retrospective study, Yalbuzdağ et al.24) examined 120 stroke patients after rehabilitation and identified a relationship between changes in the Functional Independence Measure Mobility score of patients and vitamin D. However, there was no relationship identified between FAS values and vitamin D levels. Our findings were consistent with these findings of Yalbuzdağ et al.24) on the relationship of vitamin D levels with the quality of life and ambulation ability. There were significant improvements in activities of daily living after vitamin D supplementation; however, no significant improvements in ambulation were observed.
The most important limitation of this study is that a generalization cannot be made due to the small number of patients included. Another limitation is that the follow-up period of the patients was limited to 3 months. A long-term comparison of results can give a broader perspective.
In conclusion, this study supports that vitamin D supplementation has positive effects on the improvement of balance and activities of daily living in patients having hemiplegia due to ischemic stroke who have low levels of vitamin D. However, the effects on motor healing and ambulation could not be clearly demonstrated.
Conflict of interest
None
REFERENCES
- 1.Sun Q, Pan A, Hu FB, et al. : 25-Hydroxyvitamin D levels and the risk of stroke: a prospective study and meta-analysis. Stroke, 2012, 43: 1470–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akdeniz S, Hepguler S, Öztürk C, et al. : The relation between vitamin D and postural balance according to clinical tests and tetrax posturography. J Phys Ther Sci, 2016, 28: 1272–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dukas L, Schacht E, Mazor Z, et al. : Treatment with alfacalcidol in elderly people significantly decreases the high risk of falls associated with a low creatinine clearance of <65 ml/min. Osteoporos Int, 2005, 16: 198–203. [DOI] [PubMed] [Google Scholar]
- 4.Linnebur SA, Vondracek SF, Vande Griend JP, et al. : Prevalence of vitamin D insufficiency in elderly ambulatory outpatients in Denver, Colorado. Am J Geriatr Pharmacother, 2007, 5: 1–8. [DOI] [PubMed] [Google Scholar]
- 5.Blum L, Korner-Bitensky N: Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther, 2008, 88: 559–566. [DOI] [PubMed] [Google Scholar]
- 6.Berg K, Wood-Dauphinee S, Williams JI: The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med, 1995, 27: 27–36. [PubMed] [Google Scholar]
- 7.Shah S, Vanclay F, Cooper B: Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol, 1989, 42: 703–709. [DOI] [PubMed] [Google Scholar]
- 8.Holden MK, Gill KM, Magliozzi MR, et al. : Clinical gait assessment in the neurologically impaired. Reliability and meaningfulness. Phys Ther, 1984, 64: 35–40. [DOI] [PubMed] [Google Scholar]
- 9.Brunnstrom S: Motor testing procedures in hemiplegia: based on sequential recovery stages. Phys Ther, 1966, 46: 357–375. [DOI] [PubMed] [Google Scholar]
- 10.Gloth FM, 3rd, Smith CE, Hollis BW, et al. : Functional improvement with vitamin D replenishment in a cohort of frail, vitamin D-deficient older people. J Am Geriatr Soc, 1995, 43: 1269–1271. [DOI] [PubMed] [Google Scholar]
- 11.Wicherts IS, van Schoor NM, Boeke AJ, et al. : Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab, 2007, 92: 2058–2065. [DOI] [PubMed] [Google Scholar]
- 12.Gupta A, Prabhakar S, Modi M, et al. : Effect of Vitamin D and calcium supplementation on ischaemic stroke outcome: a randomised controlled open-label trial. Int J Clin Pract, 2016, 70: 764–770. [DOI] [PubMed] [Google Scholar]
- 13.Ozdemir O, Samut G, Kutsal YG: Are vitamin D levels of the patients with stroke always associated with their functional status? Turk J Osteoporos, 2011, 17: 54–59. [Google Scholar]
- 14.Sato Y, Asoh T, Kondo I, et al. : Vitamin D deficiency and risk of hip fractures among disabled elderly stroke patients. Stroke, 2001, 32: 1673–1677. [DOI] [PubMed] [Google Scholar]
- 15.Muir SW, Montero-Odasso M: Effect of vitamin D supplementation on muscle strength, gait and balance in older adults: a systematic review and meta-analysis. J Am Geriatr Soc, 2011, 59: 2291–2300. [DOI] [PubMed] [Google Scholar]
- 16.Qutubuddin A, Cifu DX, Adler RA, et al. : A pilot study of vitamin D and balance characteristics in middle-aged, healthy individuals. PM R, 2010, 2: 23–26. [DOI] [PubMed] [Google Scholar]
- 17.Gerdhem P, Ringsberg K A M, Obrant KJ, et al. : Association between 25-hydroxy vitamin D levels, physical activity, muscle strength and fractures in the prospective population-based OPRA Study of Elderly Women. Osteoporos Int, 2005, 16: 1425–1431. [DOI] [PubMed] [Google Scholar]
- 18.Korkmaz N, Tutoğlu A, Korkmaz I, et al. : The relationships among vitamin D Level, balance, muscle strength, and quality of life in postmenopausal patients with osteoporosis. J Phys Ther Sci, 2014, 26: 1521–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pérez-López FR: Vitamin D and its implications for musculoskeletal health in women: an update. Maturitas, 2007, 58: 117–137. [DOI] [PubMed] [Google Scholar]
- 20.Ceglia L: Vitamin D and its role in skeletal muscle. Curr Opin Clin Nutr Metab Care, 2009, 12: 628–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. : Effect of vitamin D on falls: a meta-analysis. JAMA, 2004, 291: 1999–2006. [DOI] [PubMed] [Google Scholar]
- 22.Di Monaco M, Vallero F, Di Monaco R: Serum levels of 25-hydroxyvitamin D and functional recovery after hip fracture. Arch Phys Med Rehabil, 2005, 86: 64–68. [DOI] [PubMed] [Google Scholar]
- 23.Nakamura K, Nishiwaki T, Ueno K, et al. : Serum 25-hydroxyvitamin D levels and activities of daily living in noninstitutionalized elderly Japanese requiring care. J Bone Miner Metab, 2005, 23: 488–494. [DOI] [PubMed] [Google Scholar]
- 24.Yalbuzdag SA, Sarifakioglu B, Afsar SI, et al. : Is 25(OH)D associated with cognitive impairment and functional improvement in stroke? a retrospective clinical study. J Stroke Cerebrovasc Dis, 2015, 24: 1479–1486. [DOI] [PubMed] [Google Scholar]


