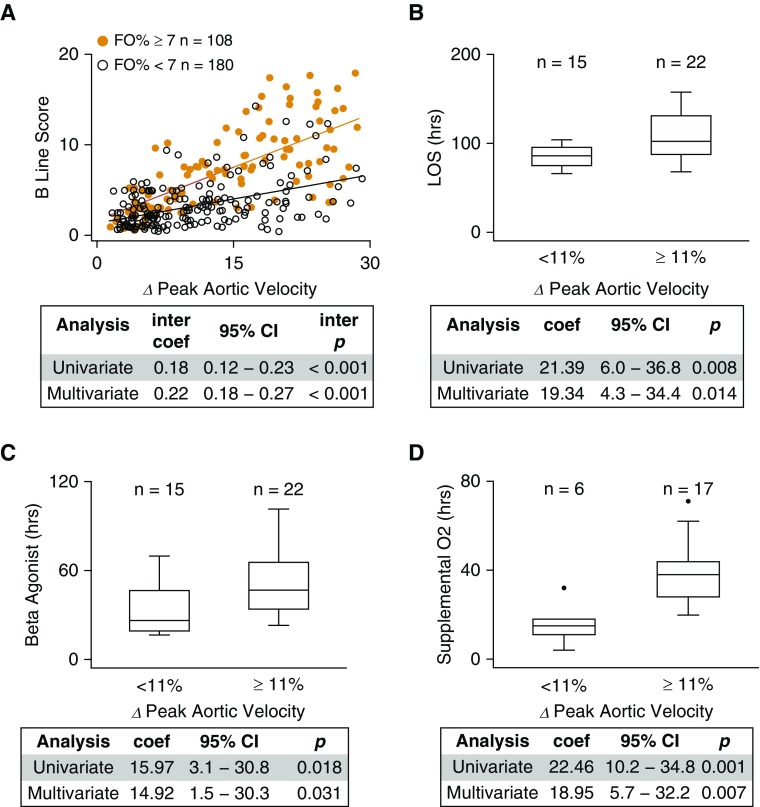
Figure 4.
Interaction between fluid overload and intrapleural pressure is associated with evidence of increased extravascular lung water. (A) For individuals with rhinovirus-triggered asthma exacerbation (n = 61 individuals with 288 measurements), as percent variation in peak aortic velocity over the respiratory cycle (∆ peak aortic velocity %) increased, those individuals with clinically meaningful fluid overloaded (fluid overload percent [FO%] ≥ 7, orange; n = 108 observations) were significantly more likely to exhibit ultrasound signs of extravascular lung water (B-lines) compared with individuals with FO% less than 7 (black; n = 180 observations). The linear regression interaction coefficient (inter coef), 95% confidence interval (CI), and interaction P (inter p) value are shown (multivariable analysis adjusted for age, weight, time from hospital admission to ultrasound measurements, and acute asthma severity score at the time of ultrasound measurements). The combination of clinically meaningful fluid overload (FO% ≥ 7) and high respiratory variation in peak aortic velocity (≥11%) was significantly associated with (B) longer length of stay (LOS), (C) longer duration of β-agonist therapy, and (D) longer duration of supplemental oxygen when compared with patients who had clinically meaningful fluid overload but low respiratory variation in peak aortic velocity. Box-plots split datasets into quartiles, with outliers represented by solid circles. The regression coefficient (coef), 95% CI, and P value are shown (multivariable analysis adjusted for age, sex, race, composite asthma severity index score, initial serum bicarbonate, and acute asthma severity score).