Abstract
Aortic stiffness during cardiac contraction is defined by the rigidity of the aorta and the elastic resistance to deformation. Recent studies suggest that aortic stiffness may be associated with changes in cholesterol efflux in endothelial cells. This alteration in cholesterol efflux may directly affect endothelial function, extracellular matrix composition, and vascular smooth muscle cell function and behavior. These pathological changes favor an aortic stiffness phenotype. Among all of the proteins participating in the cholesterol efflux process, ATP binding cassette transporter A1 (ABCA1) appears to be the main contributor to arterial stiffness changes in terms of structural and cellular function. ABCA1 is also associated with vascular inflammation mediators implicated in aortic stiffness. The goal of this mini review is to provide a conceptual hypothesis of the recent advancements in the understanding of ABCA1 in cholesterol efflux and its role and association in the development of aortic stiffness, with a particular emphasis on the potential mechanisms and pathways involved.
Keywords: aortic stiffness, cholesterol efflux, reverse cholesterol transport, ATP-binding cassette transporters
1. Introduction
Arterial stiffness develops from a complex interaction between stable and dynamic changes involving structural and cellular elements of the vessel wall. Aortic stiffness is a consequence of pathophysiological alterations involving endothelial cells, vascular smooth muscle cells (VSMCs), extracellular matrix (ECM), inflammatory responses, and other functional elements [1]. The aorta not only serves as a conduit for blood to reach peripheral tissues, but also regulates systolic blood pressure and maintains diastolic blood pressure by its elastic properties (Windkessel effect) [2]. Normal compliance and contractility of the aorta help in damping the fluctuation in blood pressure over the cardiac cycle and assist in the maintenance of organ perfusion during diastole. Vessel compliance is considered to be related to the composition of the ECM—particularly collagens and elastin [3]. VSMCs provide an active tension component within the aorta contributing to its contractility properties [4]. The endothelium also modulates aortic stiffness due to its capacity to modulate smooth muscle tone. Dedifferentiated VSMCs synthesize large amounts of ECM proteins and matrix-modifying enzymes and are therefore proposed to be a significant regulator of ECM remodeling and arterial stiffness [5,6].
A stiffened aorta, as a consequence of fractures of the elastic lamina, replacement of elastin by collagens, local inflammation, VSMC infiltration, necrosis, and calcification, opposes systolic distention. When this occurs, hemodynamic factors require a greater amount of force to accommodate the stroke volume, which leads to an increase in systolic blood pressure and a decrease in diastolic blood pressure, and therefore high pulse pressure. The increase in systolic blood pressure and velocity can result in an increase in left ventricular afterload and increased sheer stress to vessels. Meanwhile, a decrease in diastolic blood pressure causes decreased perfusion in both the peripheral and coronary circulations. It is well recognized that aortic stiffness precedes future systemic hypertension and amplifies the pathogenesis of hypertension by changing the pressure oscillations and pulsatile shear stress throughout the cardiovascular system [7,8,9]. Additionally, aortic stiffness is believed to be the earliest detectable manifestations of adverse structural and functional changes within the aortic wall [10]. Aortic stiffness is recognized as an independent predictor of left ventricular diastolic dysfunction and heart failure with preserved ejection fraction [11,12,13], as well as cardiovascular events and mortality [14,15].
Aortic stiffness, as well as high-density lipoprotein (HDL), particularly its activity in cholesterol efflux, are associated with cardiovascular risk factors such as hypertension [16], metabolic syndrome [17,18], and coronary artery disease [19]. Cholesterol efflux affects endothelial cells, ECM composition, and VSMC function and behavior [20,21], suggesting an intimacy between arterial stiffness and the cholesterol efflux in cardiovascular diseases.
2. Potential Mechanisms of Aortic Stiffness and Cholesterol Efflux
Increasing evidence supports the potential role of cholesterol efflux in aortic stiffness. Apolipoprotein (Apo) A1 is the major protein component of HDL and is essential for HDL biogenesis and function. Recent studies report that HDL-3 cholesterol and Apo B/Apo A1 ratio are associated with arterial stiffness [22,23]. Oxidized low-density lipoprotein (LDL) exhibits potentially atherogenic actions, including the transformation of macrophages to foam cells. Previous reports demonstrate that oxidized LDL decreases cholesterol efflux from endothelial cell membranes, which in turn leads to endothelial cell stiffening, changes in cellular force generation, and network formation [24,25]. These factors contribute to the arterial stiffness.
The cholesterol efflux pathway is thought to also play a key role in HDL anti-atherogenic pathways [26,27]. Indeed, the capacity of cholesterol efflux has been shown to be inversely associated with intima-media thickness [28]. However, this relationship is independent of HDL cholesterol levels, suggesting that cholesterol efflux may contribute to the process of aortic stiffening via other possible mechanisms.
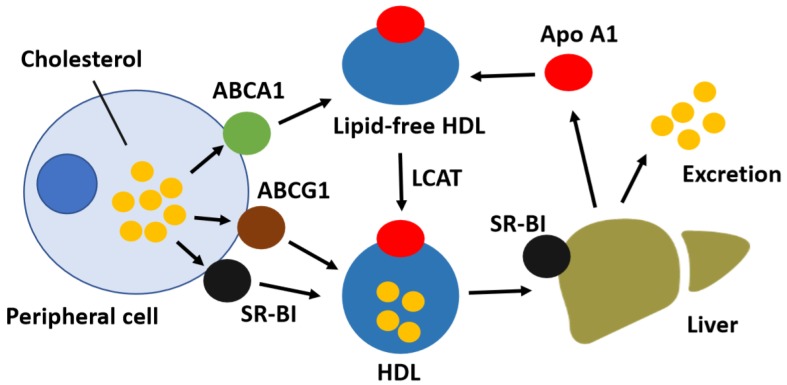
Reverse cholesterol transport is a complex multistep process. The initial and critical step, by which free cholesterol is exported from peripheral cells and subsequently transferred to HDL particles, is known as cholesterol efflux [29]. Increased cholesterol efflux prevents subsequent cardiac events by initiating the removal of excessive peripheral cholesterol for transport to the liver and subsequent removal [30]. Multiple proteins affect the rate and capacity of cholesterol efflux, including membrane transporters, mitochondrial enzymes, and Apo E [31,32]. In addition, enzymes involved in lipid storage and oxidation pathways affect the cholesterol efflux capacity by changing the intracellular cholesterol pool size. Extracellular lipid acceptors such as Apo A1 or HDL also impact the rate at which free cholesterol and phospholipids are transported from the cells [33]. Three cholesterol transporters, namely the ATP binding cassette transporter (ABC) A1, ABCG1, and scavenger receptor BI (SR-BI), are best characterized as primary mediators of cholesterol efflux (Figure 1) [34]. ABCA1 facilitates the efflux of free cholesterol to lipid-free Apo A1 in the plasma [35]; ABCG1 and SR-BI mediate free cholesterol efflux to mature HDL [36].
Figure 1.
Schematic diagram of reverse cholesterol transport. Lipid-poor Apolipoprotein (Apo) A1 acquires free cholesterol from peripheral cells via ATP binding cassette transporter (ABC) A1, whereas the ABCG1 and scavenger receptor BI (SR-BI) transporters facilitate cholesterol efflux to high-density lipoprotein (HDL) particles. Free cholesterol is esterified to cholesteryl esters within nascent HDL particles by lecithin-cholesterol acyltransferase (LCAT), thereby generating mature HDL. The liver selectively takes up HDL-associated cholesteryl esters via SR-BI and excretes HDL-derived cholesterol into the bile as free cholesterol or as bile acids after conversion.
Transgenic animals with endothelial-specific overexpression of either ABCA1 or ABCG1 have been found to have enhanced cholesterol efflux, attenuated endothelial dysfunction, and reduced diet-induced aortic lesions [37,38]. Both ABCG1 and SR-BI are associated with endothelial nitric oxide synthase (eNOS) activity and endothelium-dependent vasorelaxation [39,40]. Interestingly, specific chemical inhibition of these transporters did not alter cholesterol efflux in cultured human aortic endothelial cells [41]. However, increased expressions of ABCA1 and ABCG1 were observed in aortic endothelial cells under shear stress [42], thus suggesting the participation of these transporters in reverse cholesterol transport only under simulated in vivo conditions. Another possibility is that other membrane or plasma proteins may also facilitate the cholesterol transporters in enhancing cholesterol efflux. Moreover, reduced function of ABCA1 might not only lead to cholesterol deposition in macrophages, but also contribute the dysfunctional changes of other cell types and inflammation in the arterial wall [43]. ABCA1 has been implicated in promoting the engulfment of apoptotic cells [44] and the release of prostaglandin into endothelial cells [45], resulting in anti-stiffening and anti-atherogenic effects through vasodilation as well as the inhibition of the expression of adhesion molecules, platelet aggregation, and monocyte adhesion [46]. Both ABCA1 and ABCG1 play beneficial roles in suppressing the oxidative burst and preserving the viability of macrophages following exposure to oxidized phospholipids [47].
In addition, a series of clinical trials report that angiotensin and fibroblast growth factor (FGF)-21 are associated with arterial stiffness. These tissue factors increase VSMC contraction, growth, and proliferation, as well as promoting cytoskeletal structural changes [48,49,50]. On the other hand, animal studies reveal that FGF-21 deletion aggravates diabetes-induced aortic remodeling and inflammation in type 1 diabetic mice [51] and Apo E(−/−) mice [52]; the blockage of endogenous angiotensin remarkably enhances contents of lipids and macrophages and decreases contents of VSMCs and collagens in aortic lesions in Apo E(−/−) mice [53]. As suggested by studies showing that angiotensin and FGF-21 enhance cholesterol efflux by upregulating ABCA1 and/or ABCG1 in macrophages [54,55], angiotensin and FGF-21 could act as compensatory mechanisms against arterial stiffness by enhancing cholesterol efflux. A proposed hypothesis is that ABCA1 and/or ABCG1-dependant cholesterol efflux may serve as mediators of arterial stiffness. However, further studies are warranted to elucidate this hypothesis.
The participation of cholesterol transporters in transient aortic stiffening is implicated by the application of intralipids. Intralipid is a fat emulsion of predominantly unsaturated fatty acids (UFAs) for intravenous administration. A number of studies suggest a close relationship between UFAs and cholesterol efflux [56,57,58,59]. Dose-dependent effects of UFAs on inhibiting cholesterol efflux from mouse macrophages by downregulating ABCA1 mRNA [56] and/or increasing degradation of ABCA1 protein [57,59] have been observed in in vitro studies. Indeed, the overexpression of either Apo A1 or ABCA1 can result in an increase in cholesterol efflux and a decrease in fatty acid synthesis [60]. Moreover, high-rate infusions of intralipid increase systemic vascular resistance as well as reduce vascular compliance in both humans and animals [61,62,63]. These data raise the possibility that cholesterol efflux may contribute to aortic stiffness via its interaction with fatty acid metabolism. However, other mechanisms, such as the suppression of eNOS activity and NO production by fatty acids, may be involved in vessel stiffening [64,65]. The effects of cholesterol efflux on arterial stiffness are further supported by a study revealing that cyclooxygenase-2 (COX-2) inhibition reduces arterial stiffness in hypertensive animals. This is achieved by diminishing vascular collagen deposition, normalizing altered elastin structure, and decreasing connective tissue growth factor gene expression [66]. An inhibitory effect of Apo A1 on COX-2 expression has also been observed [67,68]. Cholesterol efflux plays a role in the protection of aortic stiffness development by enhancing endothelial function, as well as inhibiting VSMC proliferation and inflammatory response.
Interestingly, changes of hemodynamic features related to or caused by aortic stiffness may also have an impact on functional cholesterol efflux. Recently, reduced cholesterol efflux capacity was observed in a minipig model of non-ischemic heart failure sustained by high-rate left ventricle pacing [69]. In hypertensive patients, the levels of cholesterol transporters were negatively associated with mean blood pressure, and the reduction of these transporters could be reversed by anti-hypertensive therapy [70]. Peroxisome proliferator-activating receptor gamma (PPARγ)-liver X receptor (LXR)-ABCA1 pathways are one of the key pathways in cholesterol efflux in macrophages [71]. It has been reported that PPARγ expression decreases in the lung vascular tissue in patients with pulmonary hypertension. It is likely that high fluid shear stress decreases PPARγ expression in vitro [72], and potentially impairs cholesterol efflux from macrophages. Studies in aortic endothelial cells subjected to laminar shear flow conditions demonstrate the upregulation of LXRα expression and the induction of transporter genes ABCA1 and ABCG1 [42,69].
3. The Role of ABCA1 in Pulse Wave Velocity
As the major cell-surface transporter in HDL-mediated cholesterol efflux, ABCA1 has been demonstrated to be associated with pulse wave velocity (PWV) in clinical studies. PWV is a frequently used surrogate marker of aortic stiffness and has been proposed to predict the risk of future cardiovascular disease events and total mortality [73]. ABCA1 gene mutation carriers are characterized by increased intima-media thickness [74,75], while ABCA1-dependent cholesterol efflux is inversely correlated with PWV in healthy subjects [76].
4. The Role of ABCA1 in Influencing Cellular Phenotypes
The importance of regulatory pathways in ABCA1 expression is critical in the regulation of VSMC differentiation, that is, a switch from a VSMC phenotype to a contractile synthetic form [77,78]. Apo A1 functions as the primary protein component of HDL and regulates the levels of ABCA1 by reducing the rate of ABCA1 protein degradation [79]. A marked variability in Apo A1 binding and Apo A1-mediated cholesterol efflux has been observed across different VSMC phenotypes, which exhibit different levels of contractility and rates of synthesis of ECM components including collagens, elastin, proteoglycans, cadherins, and integrins that regulate the stiffness of vessels [5,80,81]. Apo E upregulates ABCA1 expression [82], and is associated with the VSMC proliferation and the expressions of aortic stiffness-dependent ECM genes, such as collagen-I, fibronectin, and lysyl oxidase [83,84]. Recently, Castiglioni et al. demonstrated that HDL-3 counteracts VSMC phenotypic changes, increases VSMC markers, and decreases inflammation-associated markers after cholesterol-loading if a functional ABCA1 transporter is present [85]. A potential role of ABCA1 in aortic stiffness is suggested by its involvement in the regulation of VSMCs.
5. ABCA1 as an Anti-Inflammatory Receptor
Recent studies suggest that ABCA1 can function as an anti-inflammatory receptor to suppress the expression of inflammatory factors. ABCA1-deficient mice have increased inflammatory cell infiltration in the vessel wall and blood circulation [86]. ABCA1-mutation carriers exhibit a pro-inflammatory state as indicated by elevated levels of circulating inflammatory cytokines [87]. Interleukin (IL)-1β secretion is impaired by inhibitors of ABCA1 [88,89], while the interaction of Apo A1 with ABCA1-expressing macrophages suppresses the induction of the inflammatory cytokines IL-1β, IL-6, and tumor necrosis factor (TNF)-α [90]. IL-1β is reported to be responsible for the secretion and activation of matrix metalloproteinases (MMPs) 2 and 9 [91,92], while TNF-α inhibition improves endothelial function and reduces aortic stiffness [93,94]. MMPs are a family of over 20 enzymes that are capable of modifying all components of the ECM. MMPs participate in tissue development, remodeling, and repair, as well as atherosclerosis [95]. Of note, MMPs 2 and 9 are proposed to be the key elastolytic enzymes in ECM degradation [96]. It is reported that ABCA1 gene polymorphisms are associated with dyslipidemia and the production of some inflammatory cytokines including IL-6 and C-reactive protein (CRP) [97]. Moreover, one report suggests that the transcription levels of ABCA1 in Chinese populations are negatively associated with plasma CRP [98]. It is known that CRP promotes vascular inflammation and is found to be associated with aortic stiffness [99,100]. Furthermore, the nuclear receptors LXR and PPARγ, which are the key regulators of ABCA1 expression, have been documented to repress the inflammatory activity of MMP 2 and MMP 9 [101,102,103,104,105]. Therefore, it is hypothesized that ABCA1 may inhibit aortic stiffness by its anti-inflammatory properties.
6. Conclusions
There are several factors that are mechanistic in arterial stiffness related to cholesterol transport, such as endothelial dysfunction and inflammation. Clinical conditions such as hypertension, diabetes, dyslipidemia, and insulin resistance can contribute to bidirectional processes involved in the initiation and progression of arterial stiffening. Cholesterol efflux is associated with a number of structural and cellular changes that are associated with aortic stiffness. Hence, both the direct and indirect effects of cholesterol efflux are likely significant in understanding aortic stiffness development and pathophysiology.
Acknowledgments
Shutan Liao is funded under an NHMRC Development Grant.
Author Contributions
Conceptualization, S.L. and C.M.; Writing-Original Draft Preparation, S.L.; Writing-Review & Editing, C.M.
Conflicts of Interest
There are no conflicts of interest.
References
- 1.Park S., Lakatta E.G. Role of inflammation in the pathogenesis of arterial stiffness. Yonsei Med. J. 2012;53:258–261. doi: 10.3349/ymj.2012.53.2.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Belz G.G. Elastic properties and Windkessel function of the human aorta. Cardiovasc. Drugs Ther. 1995;9:73–83. doi: 10.1007/BF00877747. [DOI] [PubMed] [Google Scholar]
- 3.Wagenseil J.E., Mecham R.P. Vascular extracellular matrix and arterial mechanics. Physiol. Rev. 2009;89:957–989. doi: 10.1152/physrev.00041.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuna B.G., Bakker E.N., VanBavel E. Smooth muscle biomechanics and plasticity: Relevance for vascular calibre and remodelling. Basic Clin. Pharmacol. Toxicol. 2012;110:35–41. doi: 10.1111/j.1742-7843.2011.00794.x. [DOI] [PubMed] [Google Scholar]
- 5.Owens G.K., Kumar M.S., Wamhoff B.R. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol. Rev. 2004;84:767–801. doi: 10.1152/physrev.00041.2003. [DOI] [PubMed] [Google Scholar]
- 6.Saphirstein R.J., Morgan K.G. The contribution of vascular smooth muscle to aortic stiffness across length scales. Microcirculation. 2014;21:201–207. doi: 10.1111/micc.12101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Safar M.E., Nilsson P.M., Blacher J., Mimran A. Pulse pressure, arterial stiffness, and end-organ damage. Curr. Hypertens. Rep. 2012;14:339–344. doi: 10.1007/s11906-012-0272-9. [DOI] [PubMed] [Google Scholar]
- 8.Laurent S., Alivon M., Beaussier H., Boutouyrie P. Aortic stiffness as a tissue biomarker for predicting future cardiovascular events in asymptomatic hypertensive subjects. Ann. Med. 2012;44:S93–S97. doi: 10.3109/07853890.2011.653398. [DOI] [PubMed] [Google Scholar]
- 9.Kaess B.M., Rong J., Larson M.G., Hamburg N.M., Vita J.A., Levy D., Benjamin E.J., Vasan R.S., Mitchell G.F. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA. 2012;308:875–881. doi: 10.1001/2012.jama.10503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavalcante J.L., Lima J.A., Redheuil A., Al-Mallah M.H. Aortic stiffness: Current understanding and future directions. J. Am. Coll. Cardiol. 2011;57:1511–1522. doi: 10.1016/j.jacc.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 11.Chow B., Rabkin S.W. The relationship between arterial stiffness and heart failure with preserved ejection fraction: A systemic meta-analysis. Heart Fail. Rev. 2015;20:291–303. doi: 10.1007/s10741-015-9471-1. [DOI] [PubMed] [Google Scholar]
- 12.Chung C.M., Chu C.M., Chang S.T., Cheng H.W., Yang T.Y., Wan P.C., Pan K.L., Lin Y.S., Hsu J.T. Quantification of aortic stiffness to predict the degree of left ventricular diastolic function. Am. J. Med. Sci. 2010;340:468–473. doi: 10.1097/MAJ.0b013e3181f0142c. [DOI] [PubMed] [Google Scholar]
- 13.Quinaglia T., Bensalah M.Z., Bollache E., Kachenoura N., Soulat G., Boutouyrie P., Laurent S., Mousseaux E. Differential impact of local and regional aortic stiffness on left ventricular remodeling: A cardiovascular magnetic resonance study. J. Hypertens. 2018;36:552–559. doi: 10.1097/HJH.0000000000001597. [DOI] [PubMed] [Google Scholar]
- 14.Vlachopoulos C., Aznaouridis K., Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010;55:1318–1327. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell G.F., Hwang S.J., Vasan R.S., Larson M.G., Pencina M.J., Hamburg N.M., Vita J.A., Levy D., Benjamin E.J. Arterial stiffness and cardiovascular events: The Framingham Heart Study. Circulation. 2010;121:505–511. doi: 10.1161/CIRCULATIONAHA.109.886655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yin R.X., Wu D.F., Aung L.H., Yan T.T., Cao X.L., Long X.J., Miao L., Liu W.Y., Zhang L., Li M. Several lipid-related gene polymorphisms interact with overweight/obesity to modulate blood pressure levels. Int. J. Mol. Sci. 2012;13:12062–12081. doi: 10.3390/ijms130912062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gall J., Frisdal E., Bittar R., Le Goff W., Bruckert E., Lesnik P., Guerin M., Giral P. Association of Cholesterol Efflux Capacity With Clinical Features of Metabolic Syndrome: Relevance to Atherosclerosis. J. Am. Heart Assoc. 2016;5 doi: 10.1161/JAHA.116.004808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lucero D., Sviridov D., Freeman L., Lopez G.I., Fassio E., Remaley A.T., Schreier L. Increased cholesterol efflux capacity in metabolic syndrome: Relation with qualitative alterations in HDL and LCAT. Atherosclerosis. 2015;242:236–242. doi: 10.1016/j.atherosclerosis.2015.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Liu C., Zhang Y., Ding D., Li X., Yang Y., Li Q., Zheng Y., Wang D., Ling W. Cholesterol efflux capacity is an independent predictor of all-cause and cardiovascular mortality in patients with coronary artery disease: A prospective cohort study. Atherosclerosis. 2016;249:116–124. doi: 10.1016/j.atherosclerosis.2015.10.111. [DOI] [PubMed] [Google Scholar]
- 20.Prosser H.C., Ng M.K., Bursill C.A. The role of cholesterol efflux in mechanisms of endothelial protection by HDL. Curr. Opin. Lipidol. 2012;23:182–189. doi: 10.1097/MOL.0b013e328352c4dd. [DOI] [PubMed] [Google Scholar]
- 21.Dubland J.A., Francis G.A. So Much Cholesterol: The unrecognized importance of smooth muscle cells in atherosclerotic foam cell formation. Curr. Opin. Lipidol. 2016;27:155–161. doi: 10.1097/MOL.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 22.Wang F., Wang X., Ye P., Cao R., Zhang Y., Qi Y., Zhao D. High-density lipoprotein 3 cholesterol is a predictive factor for arterial stiffness: A community-based 4.8-year prospective study. Lipids Health Dis. 2018;17:5. doi: 10.1186/s12944-017-0650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim M.K., Ahn C.W., Kang S., Ha J.Y., Baek H., Park J.S., Kim K.R. Association between Apolipoprotein B/Apolipoprotein A-1 and arterial stiffness in metabolic syndrome. Clin. Chim. Acta. 2014;437:115–119. doi: 10.1016/j.cca.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Byfield F.J., Tikku S., Rothblat G.H., Gooch K.J., Levitan I. OxLDL increases endothelial stiffness, force generation, and network formation. J. Lipid Res. 2006;47:715–723. doi: 10.1194/jlr.M500439-JLR200. [DOI] [PubMed] [Google Scholar]
- 25.Shentu T.P., Titushkin I., Singh D.K., Gooch K.J., Subbaiah P.V., Cho M., Levitan I. oxLDL-induced decrease in lipid order of membrane domains is inversely correlated with endothelial stiffness and network formation. Am. J. Physiol. Cell Physiol. 2010;299:C218–C229. doi: 10.1152/ajpcell.00383.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cuchel M., Rader D.J. Macrophage reverse cholesterol transport: Key to the regression of atherosclerosis? Circulation. 2006;113:2548–2555. doi: 10.1161/CIRCULATIONAHA.104.475715. [DOI] [PubMed] [Google Scholar]
- 27.Osorio J. Vascular disease: Cholesterol-efflux capacity might be the key to the protective effects of HDL. Nat. Rev. Cardiol. 2011;8:122. doi: 10.1038/nrcardio.2011.9. [DOI] [PubMed] [Google Scholar]
- 28.Khera A.V., Cuchel M., de la Llera-Moya M., Rodrigues A., Burke M.F., Jafri K., French B.C., Phillips J.A., Mucksavage M.L., Wilensky R.L., et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N. Engl. J. Med. 2011;364:127–135. doi: 10.1056/NEJMoa1001689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Favari E., Chroni A., Tietge U.J., Zanotti I., Escola-Gil J.C., Bernini F. Cholesterol efflux and reverse cholesterol transport. Handb. Exp. Pharmacol. 2015;224:181–206. doi: 10.1007/978-3-319-09665-0_4. [DOI] [PubMed] [Google Scholar]
- 30.Hutchins P.M., Heinecke J.W. Cholesterol efflux capacity, macrophage reverse cholesterol transport and cardioprotective HDL. Curr. Opin. Lipidol. 2015;26:388–393. doi: 10.1097/MOL.0000000000000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schmitz G., Langmann T. Transcriptional regulatory networks in lipid metabolism control ABCA1 expression. Biochim. Biophys. Acta. 2005;1735:1–19. doi: 10.1016/j.bbalip.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 32.Yancey P.G., Bortnick A.E., Kellner-Weibel G., de la Llera-Moya M., Phillips M.C., Rothblat G.H. Importance of different pathways of cellular cholesterol efflux. Arterioscler. Thromb. Vasc. Biol. 2003;23:712–719. doi: 10.1161/01.ATV.0000057572.97137.DD. [DOI] [PubMed] [Google Scholar]
- 33.Fournier N., Paul J.L., Atger V., Cogny A., Soni T., de la Llera-Moya M., Rothblat G., Moatti N. HDL phospholipid content and composition as a major factor determining cholesterol efflux capacity from Fu5AH cells to human serum. Arterioscler. Thromb. Vasc. Biol. 1997;17:2685–2691. doi: 10.1161/01.ATV.17.11.2685. [DOI] [PubMed] [Google Scholar]
- 34.Fu Y. Rate-limiting factors of cholesterol efflux in reverse cholesterol transport: Acceptors and donors. Clin. Exp. Pharmacol. Physiol. 2010;37:703–709. doi: 10.1111/j.1440-1681.2010.05386.x. [DOI] [PubMed] [Google Scholar]
- 35.Kennedy M.A., Barrera G.C., Nakamura K., Baldan A., Tarr P., Fishbein M.C., Frank J., Francone O.L., Edwards P.A. ABCG1 has a critical role in mediating cholesterol efflux to HDL and preventing cellular lipid accumulation. Cell Metab. 2005;1:121–131. doi: 10.1016/j.cmet.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 36.Yancey P.G., de la Llera-Moya M., Swarnakar S., Monzo P., Klein S.M., Connelly M.A., Johnson W.J., Williams D.L., Rothblat G.H. High density lipoprotein phospholipid composition is a major determinant of the bi-directional flux and net movement of cellular free cholesterol mediated by scavenger receptor BI. J. Biol. Chem. 2000;275:36596–36604. doi: 10.1074/jbc.M006924200. [DOI] [PubMed] [Google Scholar]
- 37.Vaisman B.L., Demosky S.J., Stonik J.A., Ghias M., Knapper C.L., Sampson M.L., Dai C., Levine S.J., Remaley A.T. Endothelial expression of human ABCA1 in mice increases plasma HDL cholesterol and reduces diet-induced atherosclerosis. J. Lipid Res. 2012;53:158–167. doi: 10.1194/jlr.M018713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Munch G., Bultmann A., Li Z., Holthoff H.P., Ullrich J., Wagner S., Ungerer M. Overexpression of ABCG1 protein attenuates arteriosclerosis and endothelial dysfunction in atherosclerotic rabbits. Heart Int. 2012;7:e12. doi: 10.4081/hi.2012.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yuhanna I.S., Zhu Y., Cox B.E., Hahner L.D., Osborne-Lawrence S., Lu P., Marcel Y.L., Anderson R.G., Mendelsohn M.E., Hobbs H.H., et al. High-density lipoprotein binding to scavenger receptor-BI activates endothelial nitric oxide synthase. Nat. Med. 2001;7:853–857. doi: 10.1038/89986. [DOI] [PubMed] [Google Scholar]
- 40.Westerterp M., Koetsveld J., Yu S., Han S., Li R., Goldberg I.J., Welch C.L., Tall A.R. Increased atherosclerosis in mice with vascular ATP-binding cassette transporter G1 deficiency—Brief report. Arterioscler. Thromb. Vasc. Biol. 2010;30:2103–2105. doi: 10.1161/ATVBAHA.110.212985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O’Connell B.J., Denis M., Genest J. Cellular physiology of cholesterol efflux in vascular endothelial cells. Circulation. 2004;110:2881–2888. doi: 10.1161/01.CIR.0000146333.20727.2B. [DOI] [PubMed] [Google Scholar]
- 42.Zhu M., Fu Y., Hou Y., Wang N., Guan Y., Tang C., Shyy J.Y., Zhu Y. Laminar shear stress regulates liver X receptor in vascular endothelial cells. Arterioscler. Thromb. Vasc. Biol. 2008;28:527–533. doi: 10.1161/ATVBAHA.107.143487. [DOI] [PubMed] [Google Scholar]
- 43.Yin K., Liao D.F., Tang C.K. ATP-binding membrane cassette transporter A1 (ABCA1): A possible link between inflammation and reverse cholesterol transport. Mol. Med. 2010;16:438–449. doi: 10.2119/molmed.2010-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hamon Y., Broccardo C., Chambenoit O., Luciani M.F., Toti F., Chaslin S., Freyssinet J.M., Devaux P.F., McNeish J., Marguet D., et al. ABC1 promotes engulfment of apoptotic cells and transbilayer redistribution of phosphatidylserine. Nat. Cell Biol. 2000;2:399–406. doi: 10.1038/35017029. [DOI] [PubMed] [Google Scholar]
- 45.Liu D., Ji L., Tong X., Pan B., Han J.Y., Huang Y., Chen Y.E., Pennathur S., Zhang Y., Zheng L. Human apolipoprotein A-I induces cyclooxygenase-2 expression and prostaglandin I-2 release in endothelial cells through ATP-binding cassette transporter A1. Am. J. Physiol. Cell Physiol. 2011;301:C739–C748. doi: 10.1152/ajpcell.00055.2011. [DOI] [PubMed] [Google Scholar]
- 46.Schror K., Hohlfeld T. Mechanisms of anti-ischemic action of prostaglandin E1 in peripheral arterial occlusive disease. VASA. 2004;33:119–124. doi: 10.1024/0301-1526.33.3.119. [DOI] [PubMed] [Google Scholar]
- 47.Yvan-Charvet L., Pagler T.A., Seimon T.A., Thorp E., Welch C.L., Witztum J.L., Tabas I., Tall A.R. ABCA1 and ABCG1 protect against oxidative stress-induced macrophage apoptosis during efferocytosis. Circ. Res. 2010;106:1861–1869. doi: 10.1161/CIRCRESAHA.110.217281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sohn S.I., Kim C.J. Modulation of renin-angiotensin system and arterial stiffness: Evidence from clinical trials. Curr. Hypertens. Rev. 2014;10:37–40. doi: 10.2174/157340211001141111160311. [DOI] [PubMed] [Google Scholar]
- 49.Yang S.J., Hong H.C., Choi H.Y., Yoo H.J., Cho G.J., Hwang T.G., Baik S.H., Choi D.S., Kim S.M., Choi K.M. Effects of a three-month combined exercise programme on fibroblast growth factor 21 and fetuin-A levels and arterial stiffness in obese women. Clin. Endocrinol. 2011;75:464–469. doi: 10.1111/j.1365-2265.2011.04078.x. [DOI] [PubMed] [Google Scholar]
- 50.Ulu S.M., Yuksel S., Altuntas A., Kacar E., Ahsen A., Altug A., Celik S., Sezer M.T. Associations between serum hepcidin level, FGF-21 level and oxidative stress with arterial stiffness in CAPD patients. Int. Urol. Nephrol. 2014;46:2409–2414. doi: 10.1007/s11255-014-0753-7. [DOI] [PubMed] [Google Scholar]
- 51.Yan X., Chen J., Zhang C., Zeng J., Zhou S., Zhang Z., Lu X., Chen J., Feng W., Li X., et al. Fibroblast growth factor 21 deletion aggravates diabetes-induced pathogenic changes in the aorta in type 1 diabetic mice. Cardiovasc. Diabetol. 2015;14:77. doi: 10.1186/s12933-015-0241-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lin Z., Pan X., Wu F., Ye D., Zhang Y., Wang Y., Jin L., Lian Q., Huang Y., Ding H., et al. Fibroblast growth factor 21 prevents atherosclerosis by suppression of hepatic sterol regulatory element-binding protein-2 and induction of adiponectin in mice. Circulation. 2015;131:1861–1871. doi: 10.1161/CIRCULATIONAHA.115.015308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yang J., Yang X., Meng X., Dong M., Guo T., Kong J., Zhang K., Zhang Y., Zhang C. Endogenous activated angiotensin-(1-7) plays a protective effect against atherosclerotic plaques unstability in high fat diet fed ApoE knockout mice. Int. J. Cardiol. 2015;184:645–652. doi: 10.1016/j.ijcard.2015.03.059. [DOI] [PubMed] [Google Scholar]
- 54.Liang B., Wang X., Bian Y., Yang H., Liu M., Bai R., Yang Z., Xiao C. Angiotensin-(1-7) upregulates expression of adenosine triphosphate-binding cassette transporter A1 and adenosine triphosphate-binding cassette transporter G1 through the Mas receptor through the liver X receptor alpha signalling pathway in THP-1 macrophages treated with angiotensin-II. Clin. Exp. Pharmacol. Physiol. 2014;41:1023–1030. doi: 10.1111/1440-1681.12312. [DOI] [PubMed] [Google Scholar]
- 55.Lin X.L., He X.L., Zeng J.F., Zhang H., Zhao Y., Tan J.K., Wang Z. FGF21 increases cholesterol efflux by upregulating ABCA1 through the ERK1/2-PPARγ -LXRalpha pathway in THP1 macrophage-derived foam cells. DNA Cell Biol. 2014;33:514–521. doi: 10.1089/dna.2013.2290. [DOI] [PubMed] [Google Scholar]
- 56.Uehara Y., Engel T., Li Z., Goepfert C., Rust S., Zhou X., Langer C., Schachtrup C., Wiekowski J., Lorkowski S., et al. Polyunsaturated fatty acids and acetoacetate downregulate the expression of the ATP-binding cassette transporter A1. Diabetes. 2002;51:2922–2928. doi: 10.2337/diabetes.51.10.2922. [DOI] [PubMed] [Google Scholar]
- 57.Wang Y., Oram J.F. Unsaturated fatty acids inhibit cholesterol efflux from macrophages by increasing degradation of ATP-binding cassette transporter A1. J. Biol. Chem. 2002;277:5692–5697. doi: 10.1074/jbc.M109977200. [DOI] [PubMed] [Google Scholar]
- 58.Zhang J., Kris-Etherton P.M., Thompson J.T., Hannon D.B., Gillies P.J., Heuvel J.P. Alpha-linolenic acid increases cholesterol efflux in macrophage-derived foam cells by decreasing stearoyl CoA desaturase 1 expression: Evidence for a farnesoid-X-receptor mechanism of action. J. Nutr. Biochem. 2012;23:400–409. doi: 10.1016/j.jnutbio.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 59.Wang Y., Oram J.F. Unsaturated fatty acids phosphorylate and destabilize ABCA1 through a protein kinase C delta pathway. J. Lipid Res. 2007;48:1062–1068. doi: 10.1194/jlr.M600437-JLR200. [DOI] [PubMed] [Google Scholar]
- 60.Ma D., Liu W., Wang Y. ApoA-I or ABCA1 expression suppresses fatty acid synthesis by reducing 27-hydroxycholesterol levels. Biochimie. 2014;103:101–108. doi: 10.1016/j.biochi.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 61.Stojiljkovic M.P., Zhang D., Lopes H.F., Lee C.G., Goodfriend T.L., Egan B.M. Hemodynamic effects of lipids in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2001;280:R1674–R1679. doi: 10.1152/ajpregu.2001.280.6.R1674. [DOI] [PubMed] [Google Scholar]
- 62.Udelsmann A., Melo Mde S. Hemodynamic changes with high infusion rates of lipid emulsion. Experimental study in swine. Acta Cir. Bras. 2015;30:720–726. doi: 10.1590/S0102-865020150110000001. [DOI] [PubMed] [Google Scholar]
- 63.Royse C., Royse A. The cardiovascular effects of intralipid as a rescue therapy for non-fatal bupivacaine toxicity. J. Perioper. Sci. 2014;1:1–6. [Google Scholar]
- 64.Davda R.K., Stepniakowski K.T., Lu G., Ullian M.E., Goodfriend T.L., Egan B.M. Oleic acid inhibits endothelial nitric oxide synthase by a protein kinase C-independent mechanism. Hypertension. 1995;26:764–770. doi: 10.1161/01.HYP.26.5.764. [DOI] [PubMed] [Google Scholar]
- 65.Steinberg H.O., Paradisi G., Hook G., Crowder K., Cronin J., Baron A.D. Free fatty acid elevation impairs insulin-mediated vasodilation and nitric oxide production. Diabetes. 2000;49:1231–1238. doi: 10.2337/diabetes.49.7.1231. [DOI] [PubMed] [Google Scholar]
- 66.Avendano M.S., Martinez-Revelles S., Aguado A., Simoes M.R., Gonzalez-Amor M., Palacios R., Guillem-Llobat P., Vassallo D.V., Vila L., Garcia-Puig J., et al. Role of COX-2-derived PGE2 on vascular stiffness and function in hypertension. Br. J. Pharmacol. 2016;173:1541–1555. doi: 10.1111/bph.13457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang W., Shi X., Yuan Y., Zhu H., Zhou W., Huang H., Feng M. Inhibitory effect of apolipoprotein A-I on matrix metalloproteinase-2 expression in vivo and in vitro. Acta Biochim. Biophys. Sin. 2013;45:194–202. doi: 10.1093/abbs/gms121. [DOI] [PubMed] [Google Scholar]
- 68.Mao J., Liu W., Wang Y. Apolipoprotein A-I expression suppresses COX-2 expression by reducing reactive oxygen species in hepatocytes. Biochem. Biophys. Res. Commun. 2014;454:359–363. doi: 10.1016/j.bbrc.2014.10.094. [DOI] [PubMed] [Google Scholar]
- 69.Bigazzi F., Adorni M.P., Puntoni M., Sbrana F., Lionetti V., Pino B.D., Favari E., Recchia F.A., Bernini F., Sampietro T. Analysis of Serum Cholesterol Efflux Capacity in a Minipig Model of Nonischemic Heart Failure. J. Atheroscler. Thromb. 2017;24:853–862. doi: 10.5551/jat.37101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xu M., Zhou H., Gu Q., Li C. The expression of ATP-binding cassette transporters in hypertensive patients. Hypertens. Res. 2009;32:455–461. doi: 10.1038/hr.2009.46. [DOI] [PubMed] [Google Scholar]
- 71.Chawla A., Boisvert W.A., Lee C.H., Laffitte B.A., Barak Y., Joseph S.B., Liao D., Nagy L., Edwards P.A., Curtiss L.K., et al. A PPARγ -LXR-ABCA1 pathway in macrophages is involved in cholesterol efflux and atherogenesis. Mol. Cell. 2001;7:161–171. doi: 10.1016/S1097-2765(01)00164-2. [DOI] [PubMed] [Google Scholar]
- 72.Ameshima S., Golpon H., Cool C.D., Chan D., Vandivier R.W., Gardai S.J., Wick M., Nemenoff R.A., Geraci M.W., Voelkel N.F. Peroxisome proliferator-activated receptor gamma (PPARγ) expression is decreased in pulmonary hypertension and affects endothelial cell growth. Circ. Res. 2003;92:1162–1169. doi: 10.1161/01.RES.0000073585.50092.14. [DOI] [PubMed] [Google Scholar]
- 73.Ben-Shlomo Y., Spears M., Boustred C., May M., Anderson S.G., Benjamin E.J., Boutouyrie P., Cameron J., Chen C.H., Cruickshank J.K., et al. Aortic pulse wave velocity improves cardiovascular event prediction: An individual participant meta-analysis of prospective observational data from 17,635 subjects. J. Am. Coll. Cardiol. 2014;63:636–646. doi: 10.1016/j.jacc.2013.09.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bochem A.E., van Wijk D.F., Holleboom A.G., Duivenvoorden R., Motazacker M.M., Dallinga-Thie G.M., de Groot E., Kastelein J.J., Nederveen A.J., Hovingh G.K., et al. ABCA1 mutation carriers with low high-density lipoprotein cholesterol are characterized by a larger atherosclerotic burden. Eur. Heart J. 2013;34:286–291. doi: 10.1093/eurheartj/ehs376. [DOI] [PubMed] [Google Scholar]
- 75.van Dam M.J., de Groot E., Clee S.M., Hovingh G.K., Roelants R., Brooks-Wilson A., Zwinderman A.H., Smit A.J., Smelt A.H., Groen A.K., et al. Association between increased arterial-wall thickness and impairment in ABCA1-driven cholesterol efflux: An observational study. Lancet. 2002;359:37–42. doi: 10.1016/S0140-6736(02)07277-X. [DOI] [PubMed] [Google Scholar]
- 76.Favari E., Ronda N., Adorni M.P., Zimetti F., Salvi P., Manfredini M., Bernini F., Borghi C., Cicero A.F. ABCA1-dependent serum cholesterol efflux capacity inversely correlates with pulse wave velocity in healthy subjects. J. Lipid Res. 2013;54:238–243. doi: 10.1194/jlr.P030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mourmoura E., Vasilaki A., Giannoukas A., Michalodimitrakis E., Pavlidis P., Tsezou A. Evidence of deregulated cholesterol efflux in abdominal aortic aneurysm. Acta Histochem. 2016;118:97–108. doi: 10.1016/j.acthis.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 78.Lacolley P., Regnault V., Segers P., Laurent S. Vascular Smooth Muscle Cells and Arterial Stiffening: Relevance in Development, Aging, and Disease. Physiol. Rev. 2017;97:1555–1617. doi: 10.1152/physrev.00003.2017. [DOI] [PubMed] [Google Scholar]
- 79.Martinez L.O., Agerholm-Larsen B., Wang N., Chen W., Tall A.R. Phosphorylation of a pest sequence in ABCA1 promotes calpain degradation and is reversed by ApoA-I. J. Biol. Chem. 2003;278:37368–37374. doi: 10.1074/jbc.M307161200. [DOI] [PubMed] [Google Scholar]
- 80.Francis G.A., Tsujita M., Terry T.L. Apolipoprotein AI efficiently binds to and mediates cholesterol and phospholipid efflux from human but not rat aortic smooth muscle cells. Biochemistry. 1999;38:16315–16322. doi: 10.1021/bi991742b. [DOI] [PubMed] [Google Scholar]
- 81.Choi H.Y., Rahmani M., Wong B.W., Allahverdian S., McManus B.M., Pickering J.G., Chan T., Francis G.A. ATP-binding cassette transporter A1 expression and apolipoprotein A-I binding are impaired in intima-type arterial smooth muscle cells. Circulation. 2009;119:3223–3231. doi: 10.1161/CIRCULATIONAHA.108.841130. [DOI] [PubMed] [Google Scholar]
- 82.Zhao Y., Chen X., Yang H., Zhou L., Okoro E.U., Guo Z. A novel function of apolipoprotein E: Upregulation of ATP-binding cassette transporter A1 expression. PLoS ONE. 2011;6:e21453. doi: 10.1371/journal.pone.0021453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kothapalli D., Liu S.L., Bae Y.H., Monslow J., Xu T., Hawthorne E.A., Byfield F.J., Castagnino P., Rao S., Rader D.J., et al. Cardiovascular protection by ApoE and ApoE-HDL linked to suppression of ECM gene expression and arterial stiffening. Cell Rep. 2012;2:1259–1271. doi: 10.1016/j.celrep.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Reddick R.L., Zhang S.H., Maeda N. Atherosclerosis in mice lacking Apo E. Evaluation of lesional development and progression. Arterioscler. Thromb. 1994;14:141–147. doi: 10.1161/01.ATV.14.1.141. [DOI] [PubMed] [Google Scholar]
- 85.Castiglioni S., Monti M., Arnaboldi L., Canavesi M., Ainis Buscherini G., Calabresi L., Corsini A., Bellosta S. ABCA1 and HDL3 are required to modulate smooth muscle cells phenotypic switch after cholesterol loading. Atherosclerosis. 2017;266:8–15. doi: 10.1016/j.atherosclerosis.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 86.Aiello R.J., Brees D., Francone O.L. ABCA1-deficient mice: Insights into the role of monocyte lipid efflux in HDL formation and inflammation. Arterioscler. Thromb. Vasc. Biol. 2003;23:972–980. doi: 10.1161/01.ATV.0000054661.21499.FB. [DOI] [PubMed] [Google Scholar]
- 87.Bochem A.E., van der Valk F.M., Tolani S., Stroes E.S., Westerterp M., Tall A.R. Increased Systemic and Plaque Inflammation in ABCA1 Mutation Carriers With Attenuation by Statins. Arterioscler. Thromb. Vasc. Biol. 2015;35:1663–1669. doi: 10.1161/ATVBAHA.114.304959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hamon Y., Luciani M.F., Becq F., Verrier B., Rubartelli A., Chimini G. Interleukin-1β secretion is impaired by inhibitors of the Atp binding cassette transporter, ABC1. Blood. 1997;90:2911–2915. [PubMed] [Google Scholar]
- 89.Zhou X., Engel T., Goepfert C., Erren M., Assmann G., von Eckardstein A. The ATP binding cassette transporter A1 contributes to the secretion of interleukin 1β from macrophages but not from monocytes. Biochem. Biophys. Res. Commun. 2002;291:598–604. doi: 10.1006/bbrc.2002.6473. [DOI] [PubMed] [Google Scholar]
- 90.Tang C., Liu Y., Kessler P.S., Vaughan A.M., Oram J.F. The macrophage cholesterol exporter ABCA1 functions as an anti-inflammatory receptor. J. Biol. Chem. 2009;284:32336–32343. doi: 10.1074/jbc.M109.047472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mountain D.J., Singh M., Menon B., Singh K. Interleukin-1β increases expression and activity of matrix metalloproteinase-2 in cardiac microvascular endothelial cells: Role of PKCalpha/beta1 and MAPKs. Am. J. Physiol. Cell Physiol. 2007;292:C867–C875. doi: 10.1152/ajpcell.00161.2006. [DOI] [PubMed] [Google Scholar]
- 92.Ruhul Amin A.R., Senga T., Oo M.L., Thant A.A., Hamaguchi M. Secretion of matrix metalloproteinase-9 by the proinflammatory cytokine, IL-1beta: A role for the dual signalling pathways, Akt and Erk. Genes Cells. 2003;8:515–523. doi: 10.1046/j.1365-2443.2003.00652.x. [DOI] [PubMed] [Google Scholar]
- 93.Maki-Petaja K.M., Elkhawad M., Cheriyan J., Joshi F.R., Ostor A.J., Hall F.C., Rudd J.H., Wilkinson I.B. Anti-tumor necrosis factor-alpha therapy reduces aortic inflammation and stiffness in patients with rheumatoid arthritis. Circulation. 2012;126:2473–2480. doi: 10.1161/CIRCULATIONAHA.112.120410. [DOI] [PubMed] [Google Scholar]
- 94.Moreau K.L., Deane K.D., Meditz A.L., Kohrt W.M. Tumor necrosis factor-α inhibition improves endothelial function and decreases arterial stiffness in estrogen-deficient postmenopausal women. Atherosclerosis. 2013;230:390–396. doi: 10.1016/j.atherosclerosis.2013.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sternlicht M.D., Werb Z. How matrix metalloproteinases regulate cell behavior. Annu. Rev. Cell Dev. Biol. 2001;17:463–516. doi: 10.1146/annurev.cellbio.17.1.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Van Doren S.R. Matrix metalloproteinase interactions with collagen and elastin. Matrix Biol. 2015;44–46:224–231. doi: 10.1016/j.matbio.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Babashamsi M.M., Halalkhor S., Moradi Firouzjah H., Parsian H., Jalali S.F., Babashamsi M. Association of ATP-Binding Cassette Transporter A1 (ABCA1)-565 C/T Gene Polymorphism with Hypoalphalipoproteinemia and Serum Lipids, IL-6 and CRP Levels. Avicenna J. Med. Biotechnol. 2017;9:38–43. [PMC free article] [PubMed] [Google Scholar]
- 98.Li C., Guo R., Lou J., Zhou H. The transcription levels of ABCA1, ABCG1 and SR-BI are negatively associated with plasma CRP in Chinese populations with various risk factors for atherosclerosis. Inflammation. 2012;35:1641–1648. doi: 10.1007/s10753-012-9479-9. [DOI] [PubMed] [Google Scholar]
- 99.Mattace-Raso F.U., van der Cammen T.J., van der Meer I.M., Schalekamp M.A., Asmar R., Hofman A., Witteman J.C. C-reactive protein and arterial stiffness in older adults: The Rotterdam Study. Atherosclerosis. 2004;176:111–116. doi: 10.1016/j.atherosclerosis.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 100.Nagano M., Nakamura M., Sato K., Tanaka F., Segawa T., Hiramori K. Association between serum C-reactive protein levels and pulse wave velocity: A population-based cross-sectional study in a general population. Atherosclerosis. 2005;180:189–195. doi: 10.1016/j.atherosclerosis.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 101.Castrillo A., Joseph S.B., Marathe C., Mangelsdorf D.J., Tontonoz P. Liver X receptor-dependent repression of matrix metalloproteinase-9 expression in macrophages. J. Biol. Chem. 2003;278:10443–10449. doi: 10.1074/jbc.M213071200. [DOI] [PubMed] [Google Scholar]
- 102.Jiang C., Ting A.T., Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998;391:82–86. doi: 10.1038/34184. [DOI] [PubMed] [Google Scholar]
- 103.Marx N., Sukhova G., Murphy C., Libby P., Plutzky J. Macrophages in human atheroma contain PPARγ: Differentiation-dependent peroxisomal proliferator-activated receptor gamma(PPARγ) expression and reduction of MMP-9 activity through PPARγ activation in mononuclear phagocytes in vitro. Am. J. Pathol. 1998;153:17–23. doi: 10.1016/S0002-9440(10)65540-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Laragione T., Gulko P.S. Liver X receptor regulates rheumatoid arthritis fibroblast-like synoviocyte invasiveness, matrix metalloproteinase 2 activation, interleukin-6 and CXCL10. Mol. Med. 2012;18:1009–1017. doi: 10.2119/molmed.2012.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ham S.A., Lee H., Hwang J.S., Kang E.S., Yoo T., Paek K.S., Do J.T., Park C., Oh J.W., Kim J.H., et al. Activation of peroxisome proliferator-activated receptor delta inhibits angiotensin II-induced activation of matrix metalloproteinase-2 in vascular smooth muscle cells. J. Vasc. Res. 2014;51:221–230. doi: 10.1159/000365250. [DOI] [PubMed] [Google Scholar]