Abstract
Rationale:
Reversible splenial lesion syndrome (RESLES) is a reversible condition with an excellent prognosis in most patients. The clinical features include altered states of consciousness, delirium, headache, and seizures, but no callosal disconnection syndromes have been described in RESLES.
Patient concerns:
We presented a 57-year-old patient with alien hand syndrome, autotopagnosia, gait disorders, and left ideomotor apraxia after blood transfusion. The brain magnetic resonance imaging (MRI) showed a few regions with high signal intensity in the genu, body, and splenium of the right corpus callosum on diffusion weighted images. Cerebrovascular examination was unremarkable.
Diagnoses:
He was diagnosed with RESLES and callosal disconnection syndrome.
Interventions:
The patient received symptomatic and supportive treatment in our hospital.
Outcomes:
He recovered to baseline on following up of 6 months and abnormalities on brain MRI completely disappeared.
Lessons:
Neurologists should be aware of the symptoms of callosal disconnection syndrome in RESLES. In addition, caution should be taken when transfusing blood products in patients with gastrointestinal bleeding.
Keywords: alien hand syndrome, callosal disconnection syndrome, reversible splenial lesion syndrome
1. Introduction
Reversible splenial lesion syndrome (RESLES) is characterized by reversible lesion in the splenium of corpus callosum (SCC) with a perfect prognosis in most condition. RESLES is related to various causes, including seizures, encephalitis/ encephalopathy, metabolic disturbances, cerebral edema, and antiepileptic drug withdrawal.[1] The pathogenesis is still unclear. Most studies suggested cellular fluid regulation abnormalities and myelin edema induced by changes in salt homeostasis in RESLES.[2] The manifestation is nonspecific, including altered states of consciousness, delirium, headache, and seizures.[3] Specifically, callosal disconnection syndromes in RESLES has received little attention.[1] We report a rare case of RESLES following blood transfusion presented with callosal disconnection syndrome.
2. Case report
This patient was a 57-year-old right-handed traffic policeman with a history of diabetes mellitus and hypertension. He was first admitted to a local hospital due to urgent hematochezia and upper abdominal discomfort. Emergency gastroscopy proved duodenal ulcer bleeding. After blood transfusion, he presented paraphasia, walking instability, and loss of bimanual coordination, characterized by the left hand performing opposite movements to the right hand. He also complained that his left hand did not belong to him but to someone else. More importantly, the patient showed loss of coordination as well as mirror movements between the lower limbs. For instance, he had difficulty going to the toilet by himself, because when his right leg moved forward, his left leg moved back at the same time. This phenomenon disappeared gradually and then mirror movements appeared. Sometime when his right leg moved forward, his left leg did the same action. Two weeks later, he was admitted to our hospital because he suffered from anesthesia of the left side of his body.
On examination, the patient was alert and oriented. There was only mildly dysarthric speech. Hypesthesia of his left side of body and face was observed. His motor strength and tone were both normal. But deep-tendon reflexes in all extremities reduced symmetrically and frontal lobe releasing signs such as reflexive grasping were absent. Other general physical examinations were all within normal limits. The brain magnetic resonance imaging (MRI) showed a few regions with low signal intensity in the genu, body, and splenium of the right corpus callosum on the T1-weighted image and high signal intensity in the same area on diffusion-weighted images (DWI), T2-weighted, and fluid attenuated inversion recovery (FLAIR) images (Fig. 1). Computed tomographic angiography of the cerebral vessels did not show any obvious stenosis in cerebral arteries. Our patient got 23 and 12 scores in the Mini-mental State Examination and Montreal Cognitive Assessment, respectively. No positive results were found in Line bisection tasks, Letter cancellation, Star test, Line cancellation, and Copy a daisy. During neuropsychological test, when he used his right hand to move toy bricks, the left hand would interfere by taking them back (the intermanual conflict). Our patient exhibited difficulties in naming the left fingers as well as pointing to named parts of the body with his left hand, especially in the nonvisual condition, on the test of body identification by the method of Nagumo and Yamadori.[4] The accuracy of naming the fingers with eyes closed and with hand behind body was 40%/30% (left fingers) as well as 80%/90% (right fingers), respectively. Correct rate of pointing to the named body parts with the left hand and the right hand was 86% and 100%, respectively. In addition, he performed the test of praxia, including verbal commands, imitation, pantomime to visual presentation of objects, and object use by the method of Lausberg et al.[5] Our patient showed prominently left hand ideomotor apraxia, such as brushing teeth and combing his hair, which was worse on verbal commands and pantomime to object use to visual object presentation, while improved on imitation and actual object use. Types of errors included spatial errors, hand position errors, and hand shape errors. He received symptomatic and supportive treatment in our hospital. After 6 months of hospital discharge, our patient improved apparently and could drive a car by himself. These abnormalities on brain MRI completely disappeared.
Figure 1.
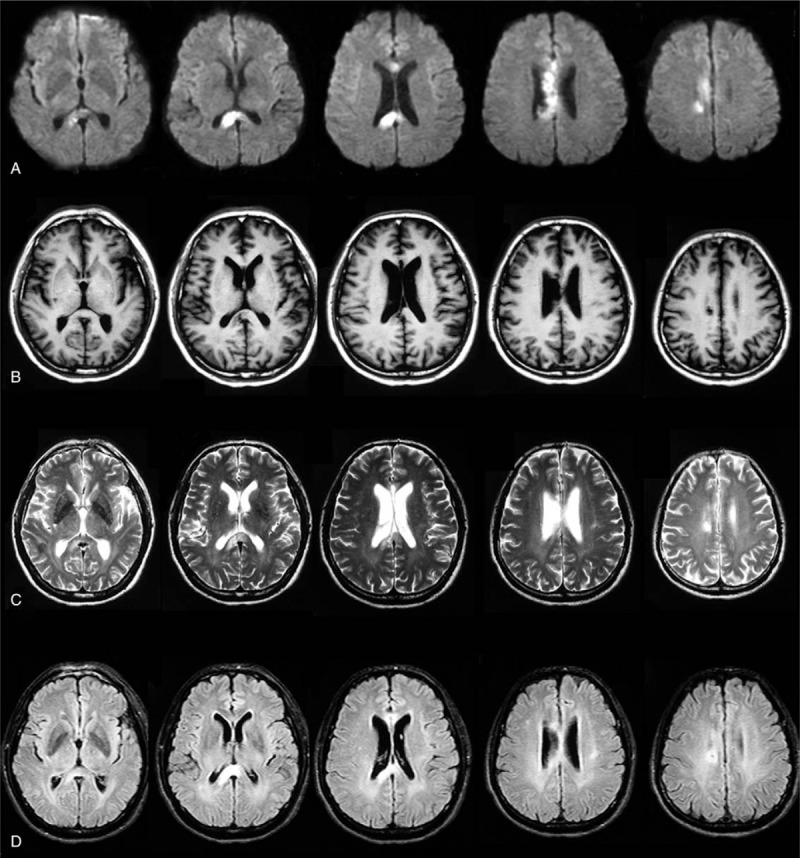
The brain MRI showed a few regions with low signal intensity in the genu, body, and splenium of the right corpus callosum on the T1-weighted image (B) and high signal intensity in the same area on diffusion-weighted images (DWI) (A), T2-weighted (C), and FLAIR images (D).
3. Discussion
Callosal disconnection syndrome is characterized by the impairment of interhemispheric transfer of information due to the disruptions of corpus callosal fibers. The most common symptoms of this syndrome are left alien hand syndrome, intermanual conflict, left tactile anomia, left ideomotor apraxia, and left agraphia.[4] Our patient presented several features of callosal disconnection syndrome, including alien hand syndrome, autotopagnosia, gait disorders, and left ideomotor apraxia, with no evidence of alexia, apraphia, and hemispatial neglect. Thus, he met the criteria for callosal disconnection syndrome. Furthermore, as Garcia-Monco et al[1] mentioned in their review, our patient could also be diagnosed with RESLES.
As to the etiology of RESLES, our patient did not have any trauma history, seizures, infection, metabolic disturbances, drug use, or withdrawal other than blood transfusion. Although blood transfusions may be lifesaving, but they inherit their own risks.[6,7] Several inflammatory complication of transfusion could occur, which involve inflammatory responses and mediators, especially cytokines, chemokines, and the like.[8] Thus, we speculate that RESLES might be caused by some other pathways activated by blood transfusion. RESLES in the setting of only blood transfusion remains unclear. Uygur Kucukseymen et al[9] revealed a case of RESLES associated with intravenous immunoglobulin (IVIG) treatment. They suggested that IVIG therapy could result in reversible corpus callosum splenial (CCS) lesions with encephalopathy and possibly result from cytotoxic edema and/or cerebral arterial vasospasm. Cevallos and Berman[10] have also reported a case of posterior reversible encephalopathy syndrome (PRES) secondary to blood transfusion. They suggested that rapid correction of hemoglobin and hematocrit could increase blood viscosity and influence cerebral autoregulation leading to the release of inflammatory cytokines.[10] We speculate that blood transfusion and IVIG share similar mechanism, which could both produce release of inflammatory cytokines, arterial vasospasm, and cytotoxic edema. So, our case also provides evidence to support possible role of blood transfusion in RESLES.
4. Conclusion
Neurologists should be aware of the symptoms of callosal disconnection syndrome in RESLES. In addition, caution should be taken when transfusing blood products in patients with gastrointestinal bleeding.
Acknowledgment
The authors thank Dr. Ying Jin from the Department of Neurology, Beijing Hospital.
Author contributions
Conceptualization: Hai-Bo Chen.
Data curation: Xin-Xin Ma.
Writing – original draft: Xin-Xin Ma.
Writing – review & editing: Wen Su, Hai-Bo Chen.
Footnotes
Abbreviations: CCS = corpus callosum splenial, DWI = diffusion-weighted images, FLAIR = fluid attenuated inversion recovery, IVIG = intravenous immunoglobulin, MRI = magnetic resonance imaging, PRES = posterior reversible encephalopathy syndrome, RESLES = reversible splenial lesion syndrome.
The patient and his son agreed with the publication of this study.
The authors have no conflicts of interest to declare.
References
- [1].Garcia-Monco JC, Cortina IE, Ferreira E, et al. Reversible splenial lesion syndrome (RESLES): what's in a name? J Neuroimaging 2011;21:e1–4. [DOI] [PubMed] [Google Scholar]
- [2].Garcia-Monco JC, Martinez A, Brochado AP, et al. Isolated and reversible lesions of the corpus callosum: a distinct entity. J Neuroimaging 2010;20:1–2. [DOI] [PubMed] [Google Scholar]
- [3].Dong K, Zhang Q, Ding J, et al. Mild encephalopathy with a reversible splenial lesion mimicking transient ischemic attack: a case report. Medicine (Baltimore) 2016;95:e5258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Nagumo T, Yamadori A. Callosal disconnection syndrome and knowledge of the body: a case of left hand isolation from the body schema with names. J Neurol Neurosurg Psychiatry 1995;59:548–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lausberg H, Cruz RF, Kita S, et al. Pantomime to visual presentation of objects: left hand dyspraxia in patients with complete callosotomy. Brain 2003;126:343–60. [DOI] [PubMed] [Google Scholar]
- [6].Oge T, Kilic CH, Kilic GS. Economic impact of blood transfusions: balancing cost and benefits. Eurasian J Med 2014;46:47–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sahu S, Hemlata, Verma A. Adverse events related to blood transfusion. Indian J Anaesth 2014;58:543–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Garraud O, Sut C, Haddad A, et al. Transfusion-associated hazards: a revisit of their presentation. Transfus Clin Biol 2018;25:118–35. [DOI] [PubMed] [Google Scholar]
- [9].Uygur Kucukseymen E, Yuksel B, Genc F, et al. Reversible splenial lesion syndrome after intravenous immunoglobulin treatment for Guillain-Barre syndrome. Clin Neuropharmacol 2017;40:224–5. [DOI] [PubMed] [Google Scholar]
- [10].Cevallos CA, Berman BS. Posterior reversible encephalopathy syndrome after blood transfusion. J Neurol Sci 2016;367:245–6. [DOI] [PubMed] [Google Scholar]


