Abstract
Background: Integration of momentary contextual and psychosocial factors within self-management feedback may provide more specific, engaging, and personalized targets for problem solving.
Methods: Forty-four youth ages 13–19 with type 1 diabetes (T1D) were provided a Bluetooth meter and completed the 30-day protocol. Participants were randomized to “app + meter” or “meter-only” groups. App + meter participants completed mealtime and bedtime assessment each day. Assessments focused on psychosocial and contextual information relevant for self-management. Graphical feedback integrated self-monitored blood glucose (SMBG), insulin, and Bluetooth-transmitted blood glucose data with the psychosocial and contextual data. App + meter participants completed an interview to identify data patterns.
Results: The median number of momentary assessments per participant was 80.0 (range 32–120) with 2.60 per day. By 2 weeks participants had an average of 40.77 (SD 12.23) assessments. Dose–response analyses indicated that the number of app assessments submitted were significantly related to higher mean daily SMBG (r = −0.44, P < 0.05) and to lower% missed mealtime SMBG (r = −0.47, P < 0.01). Number of feedback viewing sessions was also significantly related to a lower% missed mealtime SMBG (r = −0.44, P < 0.05). Controlling for baseline variables, mixed-effects analyses did not indicate group × time differences in mean daily SMBG. Engagement analyses resulted in three trajectory groups distinguished by assessment frequencies and rates of decline. Engagement group membership was significantly related to gender, mean daily SMBG, and HbA1c values.
Conclusions: Momentary assessment combined with device data provided a feasible means to provide novel personalized biobehavioral feedback for adolescents with T1D. A 2-week protocol provided sufficient data for self-management problem identification. In addition to feedback, more intensive intervention may need to be integrated for those patients with the lowest self-management at baseline.
Keywords: : Ecological momentary assessment, Feedback, Type 1 diabetes, Adolescent, Engagement, Mobile health
Introduction
Successful self-management of type 1 diabetes (T1D) requires many daily tasks that need to be carried out at mealtimes, often in social contexts, and are influenced by psychosocial issues, such as negative effect, stress, and stigma.1–3 In diabetes, identification of problems with self-management would typically take place surrounding review of data from devices, such as continuous glucose monitors, blood glucose (BG) meters, and insulin pumps. However, currently, identification of problems with self-management relies not only on accurate and actionable device data, but also relies on inferences and patient recall regarding the context of that data. Cognitive processes important for retrospective identification of problems, such as pattern recognition and causal inference, are often based on incomplete or inaccurate recall of experiences, behaviors, and events.4 Dependence on patient recall and awareness may lead to identification of self-management targets for change that are simply most recent, are emotionally salient but rarely occur, and/or are not correlated with self-management.5–7 Greater accuracy and specificity regarding which psychosocial barriers occur, their quantitative relationship to self-management tasks, and their frequency and timing could reduce effort focused on irrelevant or unquantified factors.
With the ubiquitous use of mobile technologies, it is now feasible to utilize methods that more proximally assess psychosocial, contextually relevant, and time-varying factors that influence health behaviors.8 Ecological momentary assessment (EMA) often utilizes mobile technologies to either unobtrusively obtain relevant data without participant effort or obtain self-reported data that are proximal in time and context to self-management events, such as meals. The EMA method has been used widely in health behavior research and has identified novel, modifiable, and more specific correlates of health behaviors, such as affect and risk of smoking lapses,9 social context and physical activity,10 situational stress and asthma symptoms,11 and time of day and day of the week, in relation to binge–purge behaviors.12
Data that are potentially most relevant for diabetes momentary studies includes factors that are (1) time varying, (2) contextually relevant, (3) habitual or frequent enough to warrant assessment, (4) hypothesized to provide novel insights into self-management and/or BG patterns, and (5) provide modifiable targets for intervention. Daily diary studies have been conducted associating mood or distress with diabetes self-management,13–16 but few momentary assessment studies have been conducted in diabetes. Diabetes EMA studies have reported that social context and social desirability were relevant to lower BG monitoring in adolescents,17 momentary increases in negative emotion were related to an increased likelihood of restricting mealtime insulin in adults with symptoms of eating disorders,18 and morning times have been related to worse self-management in adolescents compared with other times of the day.19
In addition to gathering momentary data for basic behavioral science, there is potential for this type of data to enhance self-management problem solving. In particular, it may be useful to provide guidance during the problem identification stage of problem solving. Personalized feedback is considered a fundamental aspect of behavior change that has often been used to create problem awareness, communicate risk, and guide behavior change.20,21 Much feedback in diabetes is digital in nature. However, engagement with health behavior technologies in general are often suboptimal.22–24 The development of viable momentary data systems with personalized feedback may support improved engagement with digital interventions through more relevant, timely, and specific feedback for patients. In diabetes, few feedback systems integrate psychosocial, behavioral, and biological data.25 To the extent that biobehavioral feedback provides meaningful and actionable insights, it may be a novel and useful component of diabetes problem-solving systems.26,27
Thus, to improve the relevance and specificity of patient data used to inform self-management problem identification, we developed a mobile application called MyDay to assess contextual, psychosocial, and self-management factors in a momentary fashion and integrate that data with BG values from meters for biobehavioral feedback. The overall aim of this study was to provide initial support for the feasibility and utility of the approach. In addition, we sought to identify short-term impact of the mobile app use on self-monitored blood glucose (SMBG), and identify mobile app engagement patterns and their relation to youth behaviors and characteristics.
Methods
Study design and participants
Participants were recruited from a regional diabetes clinic in an academic medical center in Nashville, Tennessee. Youth were eligible for the study if they (1) were patients in the pediatric diabetes clinic over the age of 12 years, (2) had been diagnosed with T1D for at least 6 months, (3) were able to speak and read English, (4) owned a working Android or iOS smartphone, and (5) were willing to use a Bluetooth BG meter during the study. Recruitment took place through flyers in the clinic, from a list of patients who previously expressed interest in research participation and clinician referral.
Procedures
At baseline, all participants were randomized to either the MyDay app condition or a meter-only condition on a 2:1 ratio, respectively. Adolescents and young adults completed baseline questionnaires and parents or young adults provided clinical and demographic information. All participants were asked to bring in their current meter(s), which were uploaded to provide prebaseline data for group by time SMBG comparisons. The iHealth® Bluetooth meter was explained and demonstrated. Participants were required to demonstrate use of the meter. One month of test strips were provided (180 strips) and participants kept the meter after the study. Participants were then monitored for a period of 3 days to ensure that the meter was used successfully. If no meter data were submitted, the participant and/or parents were contacted for troubleshooting. All participants were compensated $60 for completion of the study. Meter-only participants completed baseline measures and provided Bluetooth SMBG data.
For app + meter participants, four assessments were scheduled per day corresponding to mealtimes (breakfast, lunch, dinner) and bedtime for 30 days for a maximum of 120 assessments per participant (90 mealtime and 30 bedtime assessments). Each of the 90 mealtime mobile assessment notifications were individually automatically scheduled based on participant reports of likely mealtimes during the study period. Investigators instructed participants to submit mealtime assessments regardless of whether they ate a meal. Ad hoc snacks could also be entered into the app. Bedtime and snacks were not used for biobehavioral feedback because SMBG and insulin administration could not always be expected at those times. Data could be entered for that day at any time until midnight.
Five text messages (SMS) were also sent per week as prompts to orient users to the app and feedback. Twenty SMS messages were created and all app participants received all messages at the same times (no more than one per day). An example of SMS messages included “Remember to check in with MyDay app at your mealtimes even if you don't eat!” and “What time of day is your best or worst for taking care of diabetes? The MyDay app can help you find that out.”
At baseline, the MyDay app was demonstrated in-person and through a video. Adolescents were asked to demonstrate use of the app to submit an assessment. App + meter participants were paid an additional $40 (in addition to the base of $60) if they achieved 80% success in completing MyDay assessments for up to $100 total compensation. At 14 days into the 30-day protocol, these participants were contacted to complete a brief structured data-guided telephone interview. Participants were sent a pdf of their feedback on the day of the interview, which was then used to guide the discussion of feedback. The University Institutional Review Board approved the study. All adolescents, young adults, and a parent (for minors) completed informed assent or consent before study procedures commenced.
MyDay mobile application features
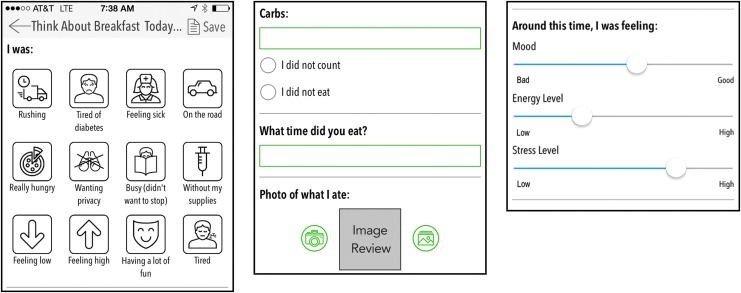
The MyDay app was developed on iOS and Android platforms by an interdisciplinary team of diabetes researchers, clinicians, software developers, user interface designers, and youth with T1D. The software allowed flexible creation of data collection content, format, and timing. Question response options include Likert type, check boxes, sliders, icons, text, numeric, and digital photo uploads. Figure 1 shows examples of assessment interfaces. The system consisted of the native app supported by a Ruby on Rails (v4.1) backend PostgreSQL database. In-app notifications were scheduled for each individual. All communications were handled through a secure socket layer. Users were able to take photos of meals and store them in the app gallery.
FIG. 1.
Examples of assessment screens.
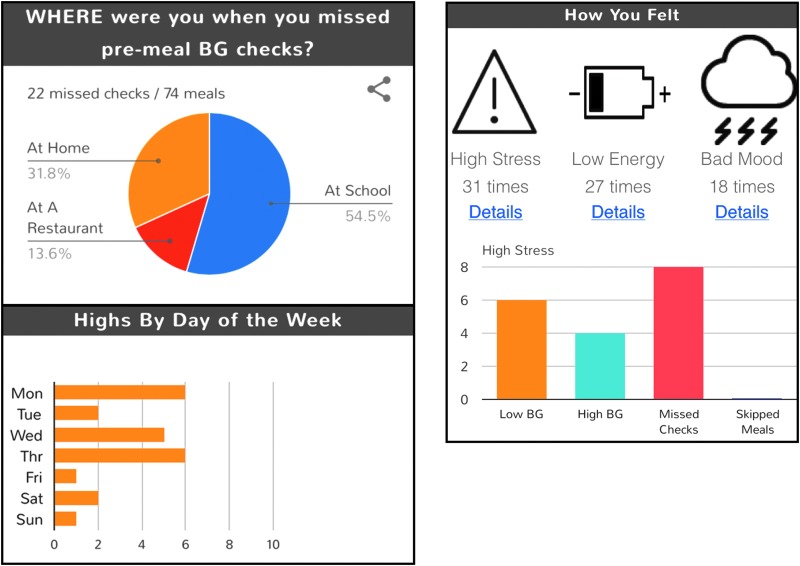
Biobehavioral feedback graphs were generated in MyDay that integrated BG values and self-management tasks, such as SMBG and insulin bolus administration, with momentary psychosocial and contextual data. Feedback was updated automatically with each assessment, could be viewed an unlimited number of times through the main navigation menu and could be shared with others through standard sharing options (MMS, email, social media). Domains of feedback were: Good News, mealtime BG checks, Lows, mealtime Insulin, Highs, Carbohydrates, Missed Meals, App use, and Logbook. Examples of feedback are shown in Figure 2. Good news was the only conditionally provided feedback and showed text that reinforced minimum criteria for adequate self-management endorsed by clinical team members (endocrinologists/nurse practitioner). For example, if a participant had an average daily SMBG of over three they would receive a message “You checked your blood sugar at least three times per day each day this week!”
FIG. 2.
Examples of graphical feedback.
Measures
Baseline questionnaires
Three questionnaires were administered to adolescents at baseline. The Self-Care Inventory–Revised (SCI-R),28,29 includes 15 items that assess the frequency of a range of self-management behaviors for the previous 2 months. The measure is frequently used in behavioral diabetes research and has established reliability and criterion validity with HbA1c.29,30 The barriers to diabetes adherence (BDA),31 questionnaire contains 21 items that assess five domains of psychosocial barriers to self-management (social support, time pressures and planning, parental autonomy support, stress/burn out, and stigma). The measure has established internal consistency and criterion validity with HbA1c.31 The Diabetes Adherence Problem-Solving Questionnaire (DAPS-Q) has 13 items that assess the use of problem-solving steps for diabetes self-management. The measure has demonstrated internal consistency and criterion validity with HbA1c.32 The HbA1c test results were obtained from the medical record and limited to the 4 months before or on the baseline date.
Data-guided interview
At 14 days the app + meter participants took part in a structured phone interview conducted by a master's-level researcher. The purpose of the interview was to identify self-management patterns in the biobehavioral feedback and generate possible causal inferences for the patterns. The day of their scheduled interview youth received a digital pdf of their current feedback graphs. The structured interview protocol took 20–30 min. All participants received the same structured questions. As they viewed feedback graphs the adolescent was asked, “Do you see a pattern?” and if yes, “Why do you think that pattern is happening?” and “Were you aware of that pattern already?”
Meter-based and momentary self-reported self-management
The source of SMBG and BG data was obtained from the iHealth Bluetooth meter provided to all participants. Mealtime SMBG (yes/no + value) from the meter was paired with reported mealtimes for the app + meter group for feedback. Missed mealtime SMBG was defined as BG values not present in the meter up to 1 h before and 15 min after the mealtime reported. The 15-min postmeal window was added when it was noted during pilot testing that youth may report eating “now” but the meal could be delayed. This was utilized to reduce overestimates of missed SMBG in feedback. Mealtime insulin boluses (yes/no) and carbohydrate counts were collected through self-report through the app. MyDay updated feedback whenever a new assessment was submitted.
Momentary psychosocial, contextual, and time-based factors
Each participant could submit three meal assessments per day (breakfast, lunch, dinner) for a total maximum of 90 mealtime assessments over 30 days. Momentary assessment items were included based on documented or hypothesized relationships with diabetes self-management and the appropriateness for EMA. Factors thought to vary over relatively shorter periods of time, such as social context or location, are most appropriate for EMA. The psychosocial variables of stress, fatigue, and mood were each assessed using an interactive “slider,” which moved between two poles (low stress–high stress, low energy–high energy, good mood–bad mood). Those variables were coded with a range of 0–100 (Fig. 1). Location and social context were assessed using check boxes. Binary icon buttons were presented for contextual barriers to self-management, such as “rushing”, “on the road”, and “hungry”. Time of the submitted assessments and day of the week were automatically coded by the software.
Statistical methods
Descriptive statistics were generated for sample characteristics and EMA assessments using SPSS (v 24). All analyses were carried out per-protocol.
To assess impact of the meter and app on SMBG, data were analyzed using between- and within-group analyses. For between-group analyses, data were analyzed by three 2-week phases: prebaseline obtained from personal meters, the first 2 weeks before the data-guided interview, and the last 2 weeks. Group by time daily SMBG were analyzed using mixed-effects modeling with STATA (v14) controlling for baseline HbA1c and prebaseline SMBG frequency. Dose–response analyses were carried out using nonparametric bivariate Pearson correlations between app use and SMBG frequency.
To identify potential subgroups of engagement, group-based trajectory analyses were performed using Proc Traj (SAS, v9.4).33 Trajectory solutions were evaluated by significance between clusters and the Bayesian Information Criterion (BIC) and Aikake Information Criterion (AIC) values. Participant demographics, clinical characteristics, and baseline measures were then related to trajectories using either Pearson chi-square or Kruskal–Wallis tests. The app database captured only page views that contained multiple feedback graphs, so the feedback was analyzed by aggregating feedback page views into “viewing sessions”. A viewing session could contain any number of specific page views, but was separated in time from another session by at least 15 min. Results were reported in accordance with the CREMAS adapted STROBE checklist for EMA studies.34
Results
Table 1 shows characteristics of the sample. The sample ranged in age from 13 to 19 years. Three app + meter subjects dropped out due to competing demands (vacation, football camp). One app + meter subject was eliminated from analyses due to lack of app entries and nonresponse to the interview invitation resulting in 30 app + meter and 14 meter-only participants.
Table 1.
Participant Characteristics
| Mean (SD) or% | All n = 44 | App + Meter n = 30 | Meter-only n = 14 |
|---|---|---|---|
| Age (years) | 15.33 (1.67) | 15.42 (1.54) | 15.14 (1.96) |
| Female | 53.33% | 51.61% | 57.14% |
| Race | |||
| White | 86.67% | 90.32% | 78.57% |
| African American | 4.44% | 0% | 14.29% |
| Mixed race | 8.89% | 9.68% | 7.14% |
| Hispanic | 2.22% | 0% | 7.14% |
| Income | |||
| Less than $50,000 | 26.67% | 16.13% | 50.00% |
| $50,000–$100,000 | 31.11% | 38.71% | 14.29% |
| Over $100,000 | 28.89% | 35.49% | 14.29% |
| Declined | 13.33% | 9.68% | 21.43% |
| Duration of diabetes (years) | 5.83 (4.00) | 5.89 (4.30) | 5.68 (3.38) |
| Uses insulin pump | 68.89% | 74.19% | 57.14% |
| Baseline HbA1c (%) | 8.56 (1.88) | 8.00 (1.16) | 9.81 (2.53) |
App use
The median number of assessments completed per participant over 30 days was 80.00 (mean 77.00, SD 29.10, range 32–120). The median number of assessments per day was 2.60 (mean 2.53; SD 1.03; range 0.60–4.00, mode 3). Week-by-week the average daily assessments gradually declined and ranged from 3.12 in week 1 (SD 0.87) to 2.10 in week 4 (SD 1.31). At the time of the data-guided interview (2 weeks), there was an average of 40.77 (SD 12.23) assessments per participant. There was 0.59% missing location and 1.44% missing social context data. Stress had 25.73% missing data, whereas fatigue and mood had 3.14% and 2.10% missing data, respectively. Carbohydrate counts had 69.34% missing data for app entries reporting a meal and thus were excluded from analyses.
Of the 2310 total assessments submitted, 1851 (80.1%) were submitted at a mealtime. Average percent (SD) of submitted assessments per mealtime and bedtime were as follows: breakfast 69.3% (SD 23.6), lunch 67.2% (SD 24.9), dinner 62.3% (SD 27.7), and bedtime 49.3% (SD 31.9). Of the mealtime assessments, 79.5% (n = 1472) reported meals and 20.5% (n = 379) reported skipped meals. At 30 days there was an average of 61.7 (SD 20.8, range 26–90) assessments per participant with reported meals. Most assessments were completed shortly after a meal with the longest delay associated with lunchtime. The median delay in submitted assessments at breakfast was 0.47 hour, at lunch was 1.88 hours, and at dinner was 0.54 hour. A total of 12 (0.82%) assessments were submitted before the reported mealtime.
The number of feedback viewing sessions per participant was 12.0 (Median; IQR = 7–22, Range 4–128) with 4.00, 2.50, 3.00, and 1.50 viewing sessions for weeks 1–4, respectively. Twelve subjects (40%) shared their feedback at least once with another person.
Association of app use with SMBG
To document short-term changes in the number of SMBG per day, mixed-effects models analyzing the fixed effects of group, time, and group by time interaction were conducted. Random effects were the individual participants. For this analysis, data were aggregated into 2-week phases: prebaseline, first 2 weeks, and second 2 weeks. Data collected from personal meters were used for prebaseline data. Controlling for baseline HbA1c and prebaseline SMBG, there were significant differences in group (F, 35.48, P < 0.001), time (F, 14.60, P < 0.001), but not group by time (F, 1.06, ns).
To estimate within-group dose–response relationships, number of app data assessments submitted, and number of feedback viewing sessions were correlated to mean daily SMBG and percent missed mealtime SMBG. The Pearson correlation between app assessments and mean daily SMBG was r = 0.44 (P < 0.05) and between app assessments and missed mealtime SMBG was r = −0.47 (P < 0.01). We were able to include missed mealtime SMBG here because only the app + meter group monitored mealtimes. The relationship between feedback viewing sessions and daily SMBG was r = 0.32 (ns) and between feedback viewing and missed mealtime SMBG was −0.44 (P < 0.05).
Engagement trajectories and correlates
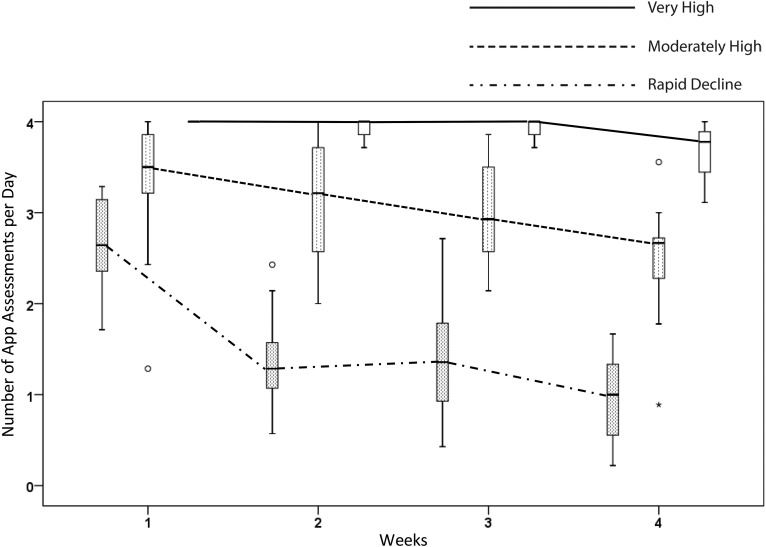
Two metrics of engagement were analyzed: number of daily app assessments submitted and feedback viewing sessions per week. The two metrics were correlated 0.45 (P < 0.01). Using assessments submitted, a three-trajectory solution best fit the data (BIC: −156.4 to −148.1; AIC: 152.5 to −141.1). Figure 3 shows trajectories of assessments completed by week. One trajectory represented 20% of app users that completed nearly every assessment over the 30-day protocol (Labeled: Very High Engagement). Another trajectory, represented by 40% of the group, started out fairly high (over three assessments per day) and declined marginally (Labeled: Consistently Moderate Engagement). The third trajectory, represented by 40% of the group, started at a moderate level (2.7 assessments per day) and declined relatively quickly to one assessment per day. (Labeled: Rapidly Declining Engagement).
FIG. 3.
Group trajectories of average daily assessments by week.
Trajectory membership was associated with HbA1c (Chi2, 7.12, P = 0.028), average daily SMBG (Chi2, 10.51, P = 0.005), and gender (Chi2, 7.00, P = 0.032). Correlates of trajectory group membership are shown in Table 2. Post hoc analyses indicated that the group differences were driven by levels of those variables in the rapidly declining engagement group compared with the other two groups. Age, insulin pump use, % BG in-range (defined as 70–150 mg/dL), and the baseline measures DAPS-Q, SCI-R, or BDA were not significantly related to engagement patterns.
Table 2.
Correlates of Engagement Trajectory Group Membership
| Consistently high (n = 6) | Consistently moderate (n = 12) | Rapidly declining (n = 12) | Pearson Chi2 or Kruskal–Wallis (P) | |
|---|---|---|---|---|
| HbA1c | 6.60 | 7.80 | 8.55 | 7.12* |
| Daily SMBG | 4.09 | 4.63 | 2.20 | 10.51** |
| % BG in range | 37.67 | 33.52 | 25.27 | 3.42 |
| % On pump | 83.3 | 83.3 | 58.3 | 2.30 |
| % Female | 83.3 | 66.7 | 25.0 | 6.90* |
| Age | 16.00 | 15.00 | 15.50 | 2.02 |
| Diabetes problem solving | 4.08 | 3.73 | 3.80 | 0.71 |
| Self-management | 3.63 | 3.63 | 3.57 | 0.347 |
| Barriers to diabetes adherence | 1.83 | 1.47 | 1.83 | 1.94 |
Medians are reported unless otherwise noted. Post hoc tests of group differences indicated the rapidly declining group was significantly different than the other two groups.
P < 0.05.
P < 0.01.
Analysis of feedback viewing sessions resulted in a single trajectory group. Attempts to fit more than one pattern resulted in considerably worsening fit (BIC: −367.8 to −327.6; AIC: −365.7 to −322.7).
Discussion
This study is one of the first to integrate momentary assessment data within integrative biobehavioral patient feedback.35,36 A primary purpose for the study was to demonstrate feasibility of the assessment and feedback system and protocol. However, the results are representative of several issues facing the use of diabetes self-monitoring and feedback systems in basic research, clinical research, and clinical practice.
Digital health behavior research has documented a common use pattern characterized by moderate-to-high engagement at baseline with steady decline over time.22 Adherence to momentary assessment protocols in children and adolescents has also been characterized as suboptimal.37 A broad range of momentary assessment schedules have been utilized in research with varying levels of participant burden depending on the nature of the phenomenon, but typically have been shorter in duration and/or less intensive than the ambitious 30-day protocol tested in this study.38,39 The momentary assessment protocol tested in this study provided sufficient data for self-management problem identification with ∼41 assessments per participant at 2 weeks.
Several behavioral components likely played a role in supporting engagement. Financial incentives were provided for general participation and also based on a predetermined criterion for assessment submission frequency. Additionally, SMS prompts oriented participants to the app and to feedback. Finally, the system provided feedback on topics that were likely new to most adolescents such as missed BG checks by mealtime or location. Despite incentives for assessments, prompts, and potential novelty, carbohydrate counts were particularly challenging for adolescents. Carbohydrate counting is arguably one of the most difficult diabetes self-management tasks due to the social nature of meals and the precision needed for accurate estimation.40,41 To obtain carbohydrate data, even for short-term research protocols, a multifaceted approach may be necessary with supplementary education, digital estimation tools, and/or salient incentives specific to counting carbohydrates. Less obtrusive assessment of mealtimes in general and carbohydrates specifically are needed. Innovative methods, including automated estimation of nutrients through photos, are still not feasible but may provide a viable option for future research.42,43 Bedtime was also associated with relatively more missing data compared with mealtimes. Given that bedtime may pose risk for inadequate self-management for some adolescents, examination of barriers specific to that time of day, such as fatigue, and more precisely timed prompts will be important moving forward.
Patterns of app assessments showed three group-based trajectories of engagement distinguished by their overall levels and rates of decline. The groups did not have differences in self-reported self-care, psychosocial barriers to self-management or lower self-management problem-solving skills at baseline. The trajectory groups were differentiated by differences primarily between the rapid decline group versus the very high and moderately high groups. The rapidly declining engagement group had higher baseline HbA1c, lower average SMBG, and fewer females. The two groups who submitted assessments at high levels across the 30 days may have shown high engagement due to responsiveness to the prompts and incentives, would complete research or self-management tasks based on social desirability, and/or may have had a greater need to demonstrate self-management competence.44 These and other more specific hypotheses regarding individual differences should be explored in future digital health engagement research.
The engagement results are representative of a broad issue in behavioral technology design and research related to addressing the unique characteristics of those patients most in need of behavioral support. The individuals who had the worst glycemic control at baseline and were least engaged in their self-management were those also least engaged in or adherent to the research protocol. The sample included individuals who were not in good control or were completing suboptimal rates of SMBG, but the system did not successfully engage them in behavioral self-monitoring and feedback. A wide range of factors, such as socioeconomic status, diabetes distress, and/or family conflict issues have been associated with suboptimal self-management in adolescents.45–47 It may be that these factors were associated with higher baseline HbA1c and to the rapidly declining engagement pattern. Self-monitoring and feedback systems are not generally designed to address, and are unlikely to reduce, many of those potential barriers. However, assessment of more broad factors is important to move forward in our ability to understand and predict trajectories of engagement with behavioral diabetes technologies.
Analysis of engagement with the graphical feedback showed an overall moderate level with decline over time and variability in frequency. Feedback of viewing sessions ranged from just a few to over 100. While it is difficult to directly compare this result with other studies, there is some evidence that adolescents only infrequently use diabetes device software and interact with feedback.48,49 No clear subgroup patterns of engagement with the feedback emerged. The lack of subgroup differentiation for feedback viewing may be related to the fact that submission of assessments was incentivized and feedback viewing was not. Feedback viewing may be more driven by intrinsic motivations such as self-exploration, whereas rote or quantitative metrics of success such as assessment submissions are relatively more driven by extrinsic rewards.50 Inclusion of strategies related to intrinsic and developmentally salient motivations to view feedback, such as a process of self-exploration and promotion of positive communications around data sharing could be feasibly integrated into forthcoming iterations of the feedback system.51,52
EMA has only infrequently been the source of behavioral feedback, but has promise in stimulating causal inferences and personal self-management narratives.35,36,53 In addition to using momentary data, the feedback in this system incorporated desirable attributes, such as immediacy, novelty, and personal relevance.27 Despite these features, app use did not result in differential group by time changes in SMBG. Within-group dose–response analyses indicated that app assessments and mean daily SMBG were positively related and app assessments and frequency of feedback viewing sessions were positively related to improved rates of mealtime SMBG. More specific data and insights are needed to understand how the feedback was used and when they were used in relation to self-management.
Self-monitoring and feedback are considered an important foundation for behavior change, but their impact alone or outside of a multicomponent intervention varies considerably across studies.26,54,55 The current system used a new free-standing assessment and feedback system. We envision a role for stand-alone systems, such as this as part of basic and clinical research, but hypothesize that the best interventional use of self-monitoring and feedback is within cyclical goal-focused problem-solving cycles. A behavioral goal-focused strategy for assessment would reduce burden and possibly extend the feasible duration of data collection. Better precision and specificity in the implementation of technology-mediated health behavior systems will provide a better understanding of how to engage individuals in their health data and feedback.56 For example, examination of the timing of feedback views in relation to subsequent self-management tasks could result in more impactful feedback and effective contextually relevant communications to enhance engagement and facilitate self-management decision making.57 Maximizing the impact of behavioral feedback will likely involve the provision of just-in-time communications based on clinically relevant data thresholds.58
Despite utilization of advanced assessment and feedback methods, the study had limitations. The nature of momentary assessment and need for reduced burden and efficiency led to assessment of psychosocial constructs based on single items. Smartphone-based momentary assessment of constructs, such as mood, have been utilized successfully in previous studies,59,60 but psychometric evaluations are lacking. Momentary assessment research must find a balance between lengthy validated self-report questionnaires and more feasible momentary methods. Related to the nature of the intensive assessment and burden, the goal is to continue to integrate the most unobtrusive methods as possible. Momentary data collection was used in this study in a broad, intensive, and exploratory manner. In this pilot study we did not incorporate unobtrusive sources of data for two variables: insulin dosing data and location. Passive data from devices and GPS from mobile phones will be utilized moving forward. Finally, the randomized small sample resulted in unequal variables across groups at baseline.
Although some relevant behaviors, experiences, and processes may feasibly tap into existing big data or use passive data streams,61–63 there are a number of behaviors and subjective experiences that will continue to need self-report for the foreseeable future. For basic EMA research purposes, not focused on changing behavior, off-setting response burden for successful engagement may be a matter of finding the best short-term extrinsic incentive levels and schedules to obtain intensive individual data. Ultimately, obtaining data in an ongoing unobtrusive manner to identify modifiable conditions under which optimal and suboptimal self-management occurs for each individual will be a milestone from which researchers, clinicians, and patients will benefit. Achieving that milestone requires larger studies with the ability to seamlessly integrate diabetes device data and development of robust algorithms to automate detection of relevant behavioral patterns. However, there are costs and benefits to utilizing completely unobtrusive or “passive” data sources. When no effort or attention is needed from participants to collect data about themselves, any potential benefits of self-monitoring due to increased self-awareness at the time of assessment will also decrease.
Self-monitoring and feedback in diabetes is a daily fact of life. Data and devices related to glucose measurement and administration require patient input and attention, provide feedback regarding BG trends, and are used for adjustments and compensatory actions. The system and methods developed for this research advance our ability to more proximally and specifically assess and address psychosocial and contextual correlates of self-management in T1D. The method has potential for the advancement of patient reported outcomes in clinical care, the development of personalized risk profiles in chronic illness, and the integration of contextual risk factors in closed loop diabetes systems. Momentary assessment has the potential to provide novel insights and direct problem solving and self-management improvement efforts more efficiently. The examination and conceptualization of engagement with digital health behavior systems is relatively new.56,64 Identification of engagement subgroups will improve the ability of clinical research to address attrition threats to internal validity. The group-based engagement analyses utilized in this study, provided a useful initial approach to identifying subgroups and correlates of those subgroups using quantitative metrics.
Acknowledgments
The authors wish to thank the families who participated in this research and the MyDay software developers: Robert McClellan, Logan Buchanan, Edward Dean, and Dr. Yu Sun.
This study was funded through grants from the National Institutes of Health (DP3 DK097706 and UL1 TR000445). Part of these results was submitted as a poster presentation to the American Diabetes Association meeting in 2016.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Hilliard ME, Yi-Frazier JP, Hessler D, et al. : Stress and A1c Among People with Diabetes Across the Lifespan. Curr Diab Rep 2016;16:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schabert J, Browne JL, Mosely K, Speight J: Social stigma in diabetes: a framework to understand a growing problem for an increasing epidemic. Patient 2013;6:1–10 [DOI] [PubMed] [Google Scholar]
- 3.Young-Hyman D, de Groot M, Hill-Briggs F, et al. : Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care 2016;39:2126–2140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shiffman S, Stone AA, Hufford MR: Ecological momentary assessment. Ann Rev Clin Psychol 2008;4:1–32 [DOI] [PubMed] [Google Scholar]
- 5.Healy AF, Havas DA, Parker JT: Comparing serial position effects in semantic and episodic memory using reconstruction of order tasks. J Mem Lang 2000;42:147–167 [Google Scholar]
- 6.LaBar KS, Cabeza R: Cognitive neuroscience of emotional memory. Nat Rev Neurosci 2006;7:54. [DOI] [PubMed] [Google Scholar]
- 7.Duke DC, Harris MA: Executive function, adherence, and glycemic control in adolescents with type 1 diabetes: a literature review. Curr Diab Rep 2014;14:532. [DOI] [PubMed] [Google Scholar]
- 8.Shiffman S: Conceptualizing analyses of ecological momentary assessment data. Nicotine Tob Res 2014;16 Suppl 2:S76–S87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roberts ME, Bidwell LC, Colby SM, Gwaltney CJ: With others or alone? Adolescent individual differences in the context of smoking lapses. Health Psychol 2015;34:1066–1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunton GF, Liao Y, Intille S, et al. : Momentary assessment of contextual influences on affective response during physical activity. Health Psychol 2015;34:1145–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunton G, Dzubur E, Li M, et al. : Momentary assessment of psychosocial stressors, context, and asthma symptoms in hispanic adolescents. Behav Modif 2016;40:257–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smyth JM, Wonderlich SA, Sliwinski MJ, et al. : Ecological momentary assessment of affect, stress, and binge-purge behaviors: day of week and time of day effects in the natural environment. Int J Eat Disord 2009;42:429–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baucom KJ, Queen TL, Wiebe DJ, et al. : Depressive symptoms, daily stress, and adherence in late adolescents with type 1 diabetes. Health Psychol 2015;34:522–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skaff MM, Mullan JT, Almeida DM, et al. : Daily negative mood affects fasting glucose in type 2 diabetes. Health Psychol 2009;28:265–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Queen TL, Butner J, Wiebe DJ, Berg CA: A micro-developmental view of parental well-being in families coping with chronic illness. J Fam Psychol 2016;30:843–853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lansing AH, Berg CA, Butner J, Wiebe DJ: Self-control, daily negative affect, and blood glucose control in adolescents with type 1 diabetes. Health Psychol 2016. http://doi.org/10.1037/hea0000325 [DOI] [PMC free article] [PubMed]
- 17.Borus JS, Blood E, Volkening LK, et al. : Momentary assessment of social context and glucose monitoring adherence in adolescents with type 1 diabetes. J Adolesc Health 2013;52:578–583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merwin RM, Dmitrieva NO, Honeycutt LK, et al. : Momentary predictors of insulin restriction among adults with type 1 diabetes and eating disorder symptomatology. Diabetes Care 2015;38:2025–2032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mulvaney SA, Rothman RL, Dietrich MS, et al. : Using mobile phones to measure adolescent diabetes adherence. Health Psychol 2012;31:43–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riper H, van Straten A, Keuken M, et al. : Curbing problem drinking with personalized-feedback interventions: a meta-analysis. Am J Prev Med 2009;36:247–255 [DOI] [PubMed] [Google Scholar]
- 21.Wing RR, Phelan S: Long-term weight loss maintenance. Am J Clin Nutr 2005;82:222S–225S [DOI] [PubMed] [Google Scholar]
- 22.Eysenbach G: The law of attrition. J Med Internet Res 2005;7:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kohl LF, Crutzen R, de Vries NK: Online prevention aimed at lifestyle behaviors: a systematic review of reviews. J Med Internet Res 2013;15:e146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maher CA, Lewis LK, Ferrar K, et al. : Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res 2014;16:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kovatchev BP, Mendosa P, Anderson S, et al. : Effect of automated bio-behavioral feedback on the control of type 1 diabetes. Diabetes Care 2011;34:302–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kluger AN, DeNisi A: The effects of feedback interventions on performance: a historical review, a meta-analysis, and a preliminary feedback intervention theory. Psychol Bull 1996;119:254–284 [Google Scholar]
- 27.Polonsky WH, Fisher L: When does personalized feedback make a difference? A narrative review of recent findings and their implications for promoting better diabetes self-care. Curr Diab Rep 2015;15:50. [DOI] [PubMed] [Google Scholar]
- 28.La Greca AM: Manual for the Self-Care Inventory. Coral Gables, FL: 2004 [Google Scholar]
- 29.Weinger K, Butler HA, Welch GW, La Greca AM: Measuring diabetes self-care: a psychometric analysis of the self-care inventory-revised with adults. Diabetes Care 2005;28:1346–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewin AB, LaGreca AM, Geffken GR, et al. : Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: the Self-Care Inventory (SCI). J Pediatr Psychol 2009;34:999–1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mulvaney SA, Hood KK, Schlundt DG, et al. : Development and initial validation of the barriers to diabetes adherence measure for adolescents. Diabetes Res Clin Pract 2011;94:77–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mulvaney SA, Jaser SS, Rothman RL, et al. : Development and validation of the diabetes adolescent problem solving questionnaire. Patient Educ Couns 2014;97:96–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nagin DS: Analyzing development trajectories: a semiparametic, group-based approach. Psychol Methods 1999;4:139–157 [Google Scholar]
- 34.Liao Y, Skelton K, Dunton G, Bruening M: A systematic review of methods and procedures used in ecological momentary assessments of diet and physical activity research in youth: an adapted STROBE checklist for reporting EMA studies (CREMAS). J Med Internet Res 2016;18:e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Snippe E, Simons CJ, Hartmann JA, et al. : Change in daily life behaviors and depression: within-person and between-person associations. Health Psychol 2016;35:433–441 [DOI] [PubMed] [Google Scholar]
- 36.van der Krieke L, Blaauw FJ, Emerencia AC, et al. : Temporal dynamics of health and well-being: a crowdsourcing approach to momentary assessments and automated generation of personalized feedback. Psychosom Med 2017;79:213–223 [DOI] [PubMed] [Google Scholar]
- 37.Wen CKF, Schneider S, Stone AA, Spruijt-Metz D: Compliance with mobile ecological momentary assessment protocols in children and adolescents: a systematic review and meta-analysis. J Med Internet Res 2017;19:e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bruening M, van Woerden I, Todd M, et al. : A Mobile Ecological Momentary Assessment Tool (devilSPARC) for Nutrition and Physical Activity Behaviors in College Students: A Validation Study. J Med Internet Res 2016;18:e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brannon EE, Cushing CC, Crick CJ, Mitchell TB: The promise of wearable sensors and ecological momentary assessment measures for dynamical systems modeling in adolescents: a feasibility and acceptability study. Transl Behav Med 2016;6:558–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehta SN, Volkening LK, Anderson BJ, et al. : Dietary behaviors predict glycemic control in youth with type 1 diabetes. Diabetes Care 2008;31:1318–1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ahola AJ, Mäkimattila S, Saraheimo M, et al. : Many patients with type 1 diabetes estimate their prandial insulin needs inappropriately. J Diabetes 2010;2:194–202 [DOI] [PubMed] [Google Scholar]
- 42.Stumbo PJ: New technology in dietary assessment: a review of digital methods in improving food record accuracy. Proc Nutr Soc 2013;72:70–76 [DOI] [PubMed] [Google Scholar]
- 43.Liu YC, Chen CH, Lee CW, et al. : Design and usability evaluation of user-centered and visual-based aids for dietary food measurement on mobile devices in a randomized controlled trial. J Biomed Inform 2016;64:122–130 [DOI] [PubMed] [Google Scholar]
- 44.Deci E, Ryan R: Intrinsic Motivation and Self-Determination in Human Behavior. New York: Plenum Press, 1985 [Google Scholar]
- 45.Hilliard ME, Guilfoyle SM, Dolan LM, Hood KK: Prediction of adolescents' glycemic control 1 year after diabetes-specific family conflict: the mediating role of blood glucose monitoring adherence. Arch Pediatr Adolesc Med 2011;165:624–629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Iturralde E, Weissberg-Benchell J, Hood KK: Avoidant coping and diabetes-related distress: pathways to adolescents' Type 1 diabetes outcomes. Health Psychol 2017;36:236–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hassan K, Loar R, Anderson BJ, Heptulla RA: The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. J Pediatr 2006;149:526–531 [DOI] [PubMed] [Google Scholar]
- 48.Vaala SE, Hood KK, Laffel L, et al. : Use of commonly available technologies for diabetes information and self-management among adolescents with type 1 diabetes and their parents: a web-based survey study. Interactive J Med Res 2015;4:e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wong JC, Neinstein AB, Spindler M, Adi S: A minority of patients with type 1 diabetes routinely downloads and retrospectively reviews device data. Diabetes Technol Ther 2015;17:555–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cerasoli CP, Nicklin JM, Ford MT: Intrinsic motivation and extrinsic incentives jointly predict performance: a 40-year meta-analysis. Psychol Bull 2014;140:980–1008 [DOI] [PubMed] [Google Scholar]
- 51.Ryan RM, Deci EL: Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78 [DOI] [PubMed] [Google Scholar]
- 52.Vaala SE, Lee JM, Hood KK, Mulvaney SA: Sharing and helping: predictors of adolescents' willingness to share diabetes personal health information with peers. J Am Med Inform Assoc 2018;25:135–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kwasnicka D, Dombrowski SU, White M, Sniehotta FF: Data-prompted interviews: using individual ecological data to stimulate narratives and explore meanings. Health Psychol 2015;34:1191–1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hartmann JA, Wichers M, Menne-Lothmann C, et al. : Experience sampling-based personalized feedback and positive affect: a randomized controlled trial in depressed patients. PLoS One 2015;10:e0128095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jakicic JM, Davis KK, Rogers RJ, et al. : Effect of wearable technology combined with a lifestyle intervention on long-term weight loss: the IDEA randomized clinical trial. JAMA 2016;316:1161–1171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yardley L, Spring BJ, Riper H, et al. : Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med 2016;51:833–842 [DOI] [PubMed] [Google Scholar]
- 57.Rus HM, Cameron LD: Health communication in social media: message features predicting user engagement on diabetes-related facebook pages. Ann Behav Med 2016;50:678–689 [DOI] [PubMed] [Google Scholar]
- 58.Nahum-Shani I, Smith SN, Spring BJ, et al. : Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med 2016:1–17. doi: 10.1007/s12160-016-9830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thornorarinsdottir H, Kessing LV, Faurholt-Jepsen M: Smartphone-based self-assessment of stress in healthy adult individuals: a systematic review. J Med Internet Res 2017;19:e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vinci C, Li L, Wu C, et al. : The association of positive emotion and first smoking lapse: an ecological momentary assessment study. Health Psychol 2017;36:1038–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Asselbergs J, Ruwaard J, Ejdys M, et al. : Mobile phone-based unobtrusive ecological momentary assessment of day-to-day mood: an explorative study. J Med Internet Res 2016;18:e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Canzian L, Musolesi M: Trajectories of depression: unobtrusive monitoring of depressive states by means of smartphone mobility traces analysis. Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing: ACM; 2015:1293–1304 [Google Scholar]
- 63.Gimpel H, Regal C, Schmidt M: myStress: unobtrusive Smartphone-Based Stress Detection. 23th European Conference on Information Systems (ECIS 2015). Münster, Germany; 2015:1–13 [Google Scholar]
- 64.Perski O, Blandford A, West R, Michie S: Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Transl Behav Med 2016;7:254–267 [DOI] [PMC free article] [PubMed] [Google Scholar]