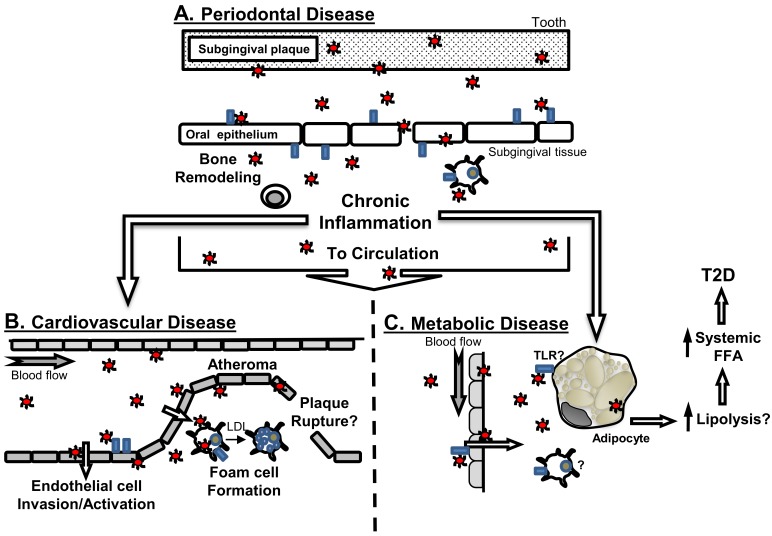
Figure 1.
Connections of periodontal disease to systemic diseases and implication of TLRs. (A) Periodontal disease is an oral disease whereby bacteria such as P. gingivalis (red circles) interact with oral epithelial cells in part through TLRs (blue rectangles). This initial host interaction participates in the generation of chronic local inflammation, and promotes immune cell recruitment to affected gingival tissues. P. gingivalis and other periodontal disease-associated bacteria have been detected in blood, and thus can transition from the oral cavity via the circulation, or potentially via translocation within immune cells that could migrate from the oral environment, to localize at distant sites, and influence; (B) cardiovascular disease, or (C) metabolic disease (hypothetical model). Animal modeling supports that P. gingivalis can accelerate atherosclerosis, and this is in part mediated by activities of TLRs, at the vascular endothelium or as part of bacterial interaction with macrophages to promote foam cell formation. The resultant inflammation may further promote development of increasing vascular plaque complexity associated with atherosclerosis. As a consequence of bacteremia, P. gingivalis may gain access to adipose tissue and interact with adipocytes either directly, or indirectly via inflammatory cells and/or chronic inflammatory cues sensed by adipose tissue. Through these direct or indirect strategies, adipocytes would elevate lipolysis, that would contribute to increased systemic levels of free fatty acids (FFA) to promotes insulin resistance and ultimately lead to the development of T2D. The contribution of TLRs to oral infection-influenced adipocyte dysfunction is unknown.