Fig. 1. Protective and harmful innate immune responses to trauma.
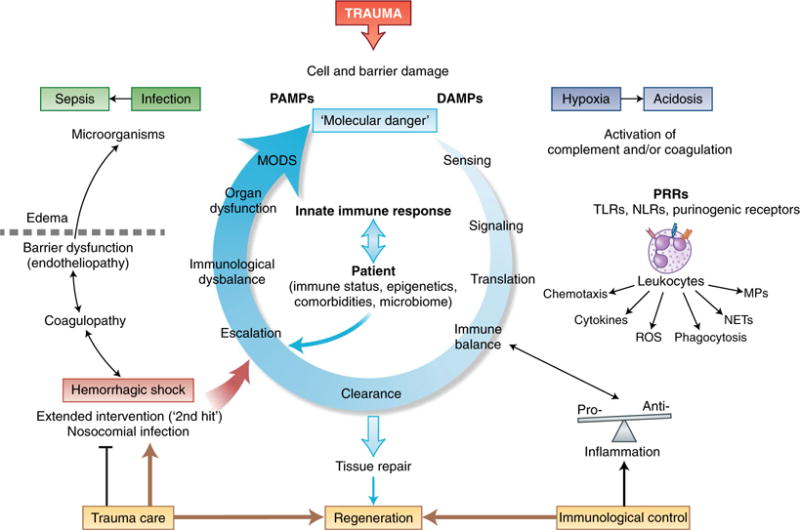
Trauma leads to the damage of external and Internal barriers and thus exposes the Immune system to DAMPs and PAMPs. Molecular danger signals and the destruction of local barriers are sensed by the complement and the coagulation systems and induce intracellular signaling in leukocytes via PRRs, which leads to translation into an instantaneous cellular immune response. Ideally, a balanced pro-inflammatory and anti-inflammatory reaction leads to rapid clearance of debris and the induction of effective tissue repair and regeneration; adverse events can be caused by individual factors of the patient or aggravated tissue damage after hemorrhage, nosocomial infection or extended surgical intervention. Escalation of the innate immune response in the form of coagulopathy and excessive inflammation leads to barrier disturbance, edema formation and compromised innate defense against invading microorganisms. Such changes can aggravate hypoxic conditions, the accumulation of metabolites and bacterial invasion, all of which can ‘feed in’ more DAMPs and PAMPs and thus generate a vicious cycle of the innate immune response. This eventually results in organ dysfunction and systemic infection, which emphasizes the importance of damage-adjusted trauma-care principles as well as control of the balance of the immune system, particularly in the acute phase after injury. MPs, microparticles.
