We report a case of a 45-year-old male who underwent a right lobectomy for metastatic liver tumors from colorectal cancer. Nine years after surgery, the patient had obstructive jaundice (total bilirubin - 19.1 mg/dL and direct bilirubin - 14.6 mg/dL). Magnetic resonance imaging showed a high-intensity mass at the porta hepatis on diffusion-weighted images. Three-dimensional magnetic resonance cholangiopancreatography and true fast imaging with steady precession showed that the B2, B3, and B4 segments were displaced [Figure 1a–c]. A malignant hilar biliary obstruction caused by recurrence of liver metastasis was diagnosed.
Figure 1.

(a) A diffusion-weighted magnetic resonance imaging showed a high-intensity mass at the porta hepatis. (b) True fast imaging with steady precession showed a high-intensity mass at the porta hepatis and left lobe of liver had hepatomegaly in compensatory. (c) Three-dimensional magnetic resonance cholangiopancreatography showed the B2, B3, and B4 segments were displaced
Endoscopic ultrasound-guided biliary drainage (EUS-BD) was performed because the duodenum was deformed due to operation and a duodenoscope could not reach the papilla of Vater. EUS showed the B2 and B3 dilatation and tumor at the porta hepatis [Figure 2a]. At first, the B2 segment was punctured [Figure 2b and 2c] because the liver volume of Segment 2 (55% [1089 mL] of total liver volume) was larger than Segment 3 (35% [693 mL]). A self-expanding metal stent ([SEMS] Zilver 635®, 8-mm, 6-French, Cook Medical, Bloomington, USA) was placed in the stricture site [Video 1 and Figure 2b and 2c]. Because there was a high risk of transesophageal and transmediastinal puncture, hepaticogastrostomy (HGS) was not performed.
Figure 2.
(a) Endoscopic ultrasound showed the dilation of B2 segment and B3 segment due to the recurrence of liver metastasis at the porta hepatis. (b) The B2 segment was punctured under endoscopic ultrasound guidance, and cholangiography showed a dilation of B2. (c) A self-expanding metal stent was placed in the stricture site
Five days after the first procedure, serum bilirubin level was not enough to improve (total bilirubin - 9.8 mg/dL). EUS showed the dilation of the B3 [Figure 3a], and the B3 was punctured transgastrically [Figure 3b]. An SEMS was placed in the stricture site of B3 using stent-in-stent technique [Figure 3c]. Because of the transgastric puncture, HGS was performed using a 7-French plastic stent to secure an access route at the time of reintervention [Video 2 and Figure 4a]. Five days after the second procedure, serum bilirubin level was improved (total bilirubin - 3.2 mg/dL). There were no procedural complications. Stent dysfunction did not occur before the patient died of cancer (during 128 days) [Figure 4b].
Figure 3.
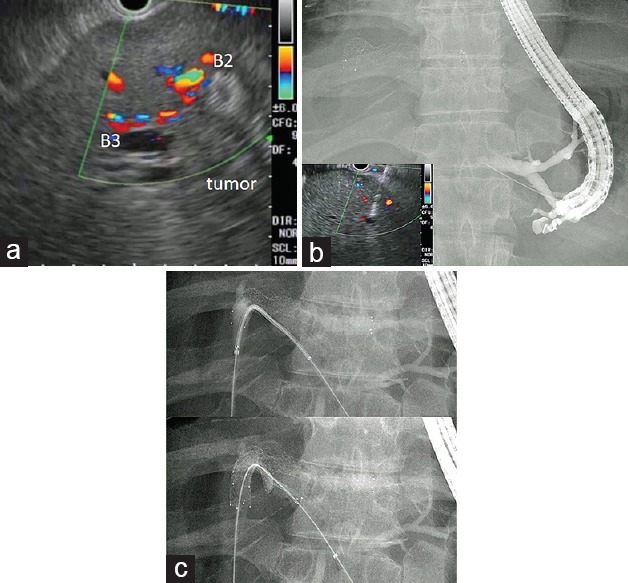
(a) Endoscopic ultrasound showed the dilation of B3 segment due to the recurrence of liver metastasis at the porta hepatis and a SEMS of B2 segment. (b) The B3 segment was punctured under endoscopic ultrasound guidance, and cholangiography showed a dilation of B3. (c) A self-expanding metal stent was placed in the stricture site using stent-in-stent technique
Figure 4.
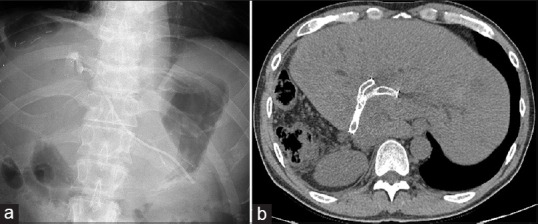
(a) After 3 months of procedures, there was no stent dislocation. (b) After 3 months of procedure, computed tomography showed self-expanding metal stents and no dilation of B2 and B3
DISCUSSION AND CONCLUSION
In patients in whom a transpapillary biliary drainage is difficult, percutaneous transhepatic biliary drainage (PTBD) will be an effective procedure. However, the PTBD will be difficult to perform for B2 segment and compromise the quality of life of patients, especially in case of multiple PTBD was needed like this patient's condition.
In recent years, EUS-BD has been actively performed, and EUS-guided antegrade-biliary-stenting (EUS-AS) has also been reported to be an effective procedure.[1,2,3] Moreover, EUS-HGS combined with AS was reported to safely and effectively avoid adverse events associated with EUS-HGS.[2] Sometimes, EUS-BD is challenging in patients with malignant hilar biliary obstruction. However, EUS-AS using the stent-in-stent technique and HGS may be a useful procedure for the treatment of malignant hilar biliary obstruction (B2 and B3 was displaced) that is difficult to manage by transpapillary procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.eusjournal.com
REFERENCES
- 1.Nguyen-Tang T, Binmoeller KF, Sanchez-Yague A, et al. Endoscopic ultrasound (EUS)-guided transhepatic anterograde self-expandable metal stent (SEMS) placement across malignant biliary obstruction. Endoscopy. 2010;42:232–6. doi: 10.1055/s-0029-1243858. [DOI] [PubMed] [Google Scholar]
- 2.Ogura T, Masuda D, Imoto A, et al. EUS-guided hepaticogastrostomy combined with fine-gauge antegrade stenting: A pilot study. Endoscopy. 2014;46:416–21. doi: 10.1055/s-0034-1365020. [DOI] [PubMed] [Google Scholar]
- 3.Dhir V, Artifon EL, Gupta K, et al. Multicenter study on endoscopic ultrasound-guided expandable biliary metal stent placement: Choice of access route, direction of stent insertion, and drainage route. Dig Endosc. 2014;26:430–5. doi: 10.1111/den.12153. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


