Abstract
Objectives
This analysis estimates the whole‐of‐system direct costs for people living with dementia in residential care by using a broad health and social care provision perspective and compares it to people without dementia living in residential care.
Methods
Data were collected from 541 individuals living permanently in 17 care facilities across Australia. The annual cost of health and residential care was determined by using individual resource use data and reported by the dementia status of the individuals.
Results
The average annual whole‐of‐system cost for people living with dementia in residential care was approximately AU$88 000 (US$ 67 100) per person in 2016. The cost of residential care constituted 93% of the total costs. The direct health care costs were comprised mainly of hospital admissions (48%), pharmaceuticals (31%) and out‐of‐hospital attendances (15%). While total costs were not significantly different between those with and without dementia, the cost of residential care was significantly higher and the cost of health care was significantly lower for people living with dementia.
Conclusion
This study provides the first estimate of the whole‐of‐system costs of providing health and residential care for people living with dementia in residential aged care in Australia using individual level health and social care data. This predominantly bottom‐up cost estimate indicates the high cost associated with caring for people with dementia living permanently in residential care, which is underestimated when limited cost perspectives or top‐down, population costing approaches are taken.
Keywords: Australia, cost, dementia, health care utilisation, residential aged care
Key points.
The annual health and residential care costs for people with dementia in residential care is AU$88 000 per person in 2016.
93% of the costs are attributable to residential care.
Health care costs were lower and residential care costs higher for people with dementia compared to those without.
The health and residential care costs are substantial and high compared to previous estimates using limited cost perspectives or top‐down approaches.
1. INTRODUCTION
The worldwide prevalence of dementia in 2010 was estimated to be 35.6 million and is projected to increase to 115.4 million by 2050.1 This is accompanied by an increasing demand for residential aged care (ie, nursing homes or long‐term institutional care). In 2009, an average of 1.4% of gross domestic product was spent on public funding of long‐term care in OECD countries and is estimated to double by 2050.2
In Australia, over half of the permanent residents living in residential aged care are likely to have dementia.3 People with dementia are also likely to have increased health care needs, comorbidities, and hospitalisations.4, 5, 6, 7
Within the context of an ageing population, it is critical to ascertain the cost of providing long‐term care for people with dementia. Several studies have estimated this with large variations in the costing approach, perspective, setting, and location.8, 9 Most commonly, studies use a predominantly macro or top‐down approach or use a mixture of macrocosting and microcosting (bottom‐up) approaches.10, 11, 12, 13, 14 Top‐down approaches provide an overarching view but with lower precision,15 and it is generally only feasible to determine resource use and costs for those with a formal diagnosis of dementia. However, dementia in a residential care setting often remains undiagnosed—approximately half or more of dementia cases in residential care are undetected.16, 17 In addition, various costing estimates use different perspectives and are conducted in community or mixed settings. A recent Alzheimer's Australia report used a cost of illness approach and estimated costs directly attributable to dementia.14 In recent reviews of the cost of dementia,8, 9 the majority of studies used a societal perspective but only 6 were conducted exclusively in residential care settings. Most existing estimates of cost of dementia are in North American or European countries.10, 14
In Australia, previous studies have estimated the costs of dementia care by using a top‐down approach10 or from a consumer contribution (out‐of‐pocket) perspective.14 However, the true cost of providing residential care for people living with dementia in Australia is currently unknown. This study using a predominantly microcosting approach aims to provide a detailed assessment of the whole‐of‐system costs of people living with dementia in residential aged care from a health and residential care provision perspective. A secondary aim was to compare the costs for people with and without dementia in this setting.
2. METHODS
2.1. Participants
This analysis is part of the INSPIRED (Investigating Services Provided in the Residential Care Environment for Dementia) study that aimed to determine and compare quality of life, quality of care and utilisation of health care resources, and costs of individuals living in residential care facilities that provide alternative models of care for people with cognitive impairment and dementia. The study enrolled 541 participants, residing for 12 months or longer in 17 facilities managed by 5 not‐for‐profit care providers across 4 Australian states (7 facilities in South Australia, 5 in New South Wales, 3 in Western Australia, and 2 in Queensland). Facilities known to be dementia specific or having a high proportion of residents with dementia were intentionally approached for recruitment. Although approached, no for‐profit providers agreed to participate. Individuals in palliative care and those who had complex medical issues that would impede participation were excluded. Data on demographic and social characteristics, health and function, care provision, quality of care and quality of life were collected from participants and/or carers (for participants with significant cognitive impairment), and formal care staff at a single time point between January 2015 and February 2016. Retrospective health care utilisation data were sourced from Commonwealth and state data custodians for the 12 months prior to participant data collection. Human research ethics approval was obtained from the Flinders University Social and Behavioural ethics committee and all relevant custodians of health care data.
2.2. Dementia status
Dementia was defined as either a diagnosis of dementia from medical records or cognitive impairment based on the Psychogeriatric Assessment Scales‐Cognitive Impairment Scale (PAS‐Cog with a score of ≥5). The PAS‐Cog is routinely used for Australian government assessments in residential care. It measures cognitive impairment on a scale from 0 to 21 with higher scores indicating severe cognitive impairment.18 Almost 20% (N = 103) of study participants had a PAS‐Cog score, indicative of probable dementia but no diagnosis recorded.
2.3. Resource use and cost data
A broad health and residential care provision perspective was used for the costs. This perspective included the majority of the all‐cause cost to the government and to individuals living with dementia but did not include private health insurance costs. All costs were reported in Australian dollars (AU$) after adjusting to 2016 prices by applying the health sector specific price deflator.19 Costing methods followed standard Australian guidelines.20 Additional out‐of‐pocket costs were incorporated as detailed below. Key cost estimates were converted to 2016 US$ (AU$1 = US$0.7617).21
2.3.1. Residential care costs
The user fee component of residential care costs was determined as 85% of the Australian single person age pension that is charged to all users of residential care in Australia. Government funding was determined based on the levels of funding received by the care providers based on the Aged Care Funding Instrument (ACFI). The ACFI provides funding based on core individual care needs in the domains of daily living, behaviour, and complex health care.22 For this analysis, the basic subsidy rates for the period ending June 2016 were applied to the levels of care need across the 3 domains to calculate government funding of residential care costs. The user paid fees and ACFI‐based subsidy together are recommended for calculating residential care costs in Australia20 and comprise 85% of the revenue received by residential care facilities.23
2.3.2. Health care utilisation and costs
Health care utilisation included out‐of‐hospital service use, hospital admissions and emergency service use, and pharmaceutical use. The utilisation measures for each of these along with their source and costing methodology are presented in Table 1. Linked Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS) data were not complete; 16% did not provide valid consent (ie, proxy consent not accepted as valid consent by data custodian) to obtain this data. However, a sensitivity analysis (not tabulated) of out‐of‐hospital medical services using data from only those who provided full consent did not alter the estimates across these health care components or total costs. The impact on pharmaceutical use data was negligible as the primary data source for pharmaceutical use was pharmacy records (Table 1). Hence, no imputation was made and complete case analysis was conducted.
Table 1.
Health care utilisation measures and costing methodology
| Health Care Utilisation Components | Categories/definitions | Source of Data, Measure | Calculation |
|---|---|---|---|
| Out‐of‐hospital services | Medical attendances, diagnostic, imaging, and investigation procedures, pathology services, and therapeutic procedures | Commonwealth Medicare Benefits Schedule (MBS)a, number of services | Provider charged fees for each item code applied as per the Medicare Benefits Schedule (MBS)a |
| Hospital admissions | Day and overnight hospital admissions | State custodians of hospital data, number of admissions | Admissions grouped into Australian Refined Diagnosis Related Groups (AR‐DRGs)b and Round 18 (2013‐2014)c cost weights applied |
| Emergency presentations | Emergency presentations not leading to admissions | State custodians of emergency department data, number of presentations | Presentations grouped into Urgency Related Groups (URGs) and Round 18 (2013‐2014)c cost weights applied |
| Pharmaceutical use | Medications | Supplying pharmacies of respective facilities (supplemented by data from medication charts and PBS), number of unique medications | Dispensed Price for Maximum Quantity (DPMQ)d from the Pharmaceutical Benefits Scheme (PBS)e applied by PBS item codes |
Abbreviations: DPMQ, Dispensed Price for Maximum Quantity; MBS, Medicare Benefits Schedule; PBS, Pharmaceutical Benefits Scheme.
The MBS is a listing of all medical services provided under the Medicare programme of the Australian government.24
Australian Consortium for Classification Development.25
Independent Hospital Pricing Authority.26
The DPMQ incorporates cost of drugs, dispensing costs and out of pocket contributions.
Department of Health.27
2.4. Analysis
Demographic, social, health, and facility characteristics were compared by dementia status and P‐values calculated by using t‐tests or chi‐squared tests as appropriate. Proportions of participants who accessed services, the mean number of services accessed, and the mean annual costs were reported by dementia status, and differences were compared using t‐tests. Statistical significance was considered at P‐value < 0.05. The proportion of mean costs for each cost component were displayed graphically. The influence of outliers of costs were examined; only 1 outlier was found in hospital admissions costs and was assessed to be a genuine outlier based on a review of the service use items. Excluding this outlier did not change the statistically significant difference in health care costs between participants with and without dementia. Medians were also compared using the Wilcoxon‐Mann‐Whitney test to exclude the effect of outliers.
3. RESULTS
A total of 1323 individuals were assessed for eligibility, 901 were eligible and 541 consented to participate in the study. Four of the 17 participating facilities were located outside of major cities, and the mean facility size was 83 beds. Fourteen facilities reported having a dementia‐specific unit or wing. Overall, 84% of the participants had dementia based either on medical diagnosis or cognitive assessment score, mean age was 85 years, approximately 75% were female, and they had on average 3.6 comorbidities in addition to dementia (Table 2). People with dementia had significantly worse activities of daily living (Modified Barthel index), neuropsychiatric symptom scores and fewer weekly social interactions than those without dementia. A smaller proportion of people with dementia lived in a large facility and more were married.
Table 2.
Characteristics of the INSPIRED study participants by dementia status
| Characteristic | Dementiaa (n = 453) | No Dementia (n = 88) | P‐value |
|---|---|---|---|
| Age, mean (SD) | 85.4 (8.6) | 85.8 (8.3) | 0.693 |
| Female, n (%) | 339 (74.8) | 64 (72.7) | 0.678 |
| Currently married, n (%) | 125 (27.7) | 12 (13.6) | 0.006 |
| Barthel index, mean (SD) | 35.8 (31.6) | 63.8 (29.2) | <0.001 |
| Number of comorbidities, mean (SD) | 3.6 (1.4) | 3.9 (1.4) | 0.05 |
| Neuropsychiatric inventory, mean (SD) | 9.0 (6.5) | 4.4 (4.0) | <0.001 |
| Resided in a large facility, n (%) | 230 (50.8) | 58 (65.9) | 0.009 |
| Resided in a regional location, n (%) | 104 (23.0) | 17 (19.3) | 0.453 |
| Weekly social interaction with family and friends, n (%) | 308 (68.9) | 70 (80.5) | 0.030 |
A diagnosis of dementia or PAS‐Cog ≥ 5.
Overall, the characteristics of the INSPIRED study sample were similar to the broader Australian national population living permanently in residential aged care in terms of age, marital status, and ACFI‐based care needs. However, there were more female, more people living in facilities in major cities, and a higher proportion living in medium and large sized facilities (Table S1 in the Supporting Information).
The majority of participants with dementia had high level of care need across all 3 ACFI domains (56‐76%; Table 3). A greater proportion of those with dementia had high levels of need for activities of daily living and behaviour compared to those without dementia. The 2 groups were similar in the complex health care domain. The levels of need translated to an overall annual basic cost of providing residential care of approximately $82 300 (US$62 700) for those with dementia and $73 200 (US$55 700) for those without dementia (Table 4), a statistically significant difference of about AU$9100 (US$7000) annually per person.
Table 3.
Care needs of INSPIRED study participants (n = 538) as assessed by the ACFI domains by dementia status
| ACFI Domains | Levels | Dementia n (%) | No Dementia n (%) |
|---|---|---|---|
| Activities of daily living | Nil | 0 (0) | 0 (0) |
| Low | 37 (8) | 23 (26) | |
| Medium | 138 (31) | 29 (33) | |
| High | 275 (61) | 36 (41) | |
| Behaviour | Nil | 5 (1) | 13 (15) |
| Low | 21 (5) | 23 (26) | |
| Medium | 83 (18) | 21 (24) | |
| High | 341 (76) | 31 (35) | |
| Complex health care | Nil | 9 (2) | 2 (2) |
| Low | 56 (12) | 12 (14) | |
| Medium | 134 (30) | 21 (24) | |
| High | 251 (56) | 53 (60) |
Table 4.
Annual resource use and costs per person (2016 Australian dollars) by dementia status
| Cost components | % (n) Accessed Services | Mean (95%CI) Number of Services | Mean (95% CI) Annual Cost in AU$ | |||
|---|---|---|---|---|---|---|
| Dementia | No Dementia | Dementia | No Dementia | Dementia | No Dementia | |
| Residential care costs | ‐ | ‐ | ‐ | ‐ | 82 316a (81 087, 83 546)*** | 73 166 (69 796, 76 537) |
| Total out of hospital | ‐ | ‐ | ‐ | ‐ | 2874 (2691, 3057)*** | 4873 (4200, 5545) |
| General practitioner attendances | 73 (327)* | 84 (74) | 13.5 (12.3, 14.7)*** | 20.6 (16.9, 24.2) | 806 (732, 880)*** | 1292 (1076, 1508) |
| Specialist attendances | 17 (78)*** | 51 (45) | 0.4 (0.3, 0.5)*** | 2.0 (1.1, 2.9) | 51 (34, 67)** | 236 (105, 367) |
| Other attendances | 24 (106)*** | 55 (48) | 0.8 (0.5, 1.1) | 2.0 (0.8, 3.2) | 26 (18, 34)** | 69 (42, 97) |
| Total attendances | 73 (330)** | 86 (76) | 14.7 (13.4, 16.0)*** | 24.6 (20.4, 28.7) | 883 (800, 964)*** | 1597 (1307, 1887) |
| Diagnostic and investigations | 5 (23)*** | 28 (25) | 0.1 (0.0, 0.1)*** | 0.4 (0.2, 0.6) | 5 (3, 7)** | 39 (18, 59) |
| Diagnostic imaging services | 15 (66)*** | 40 (35) | 0.3 (0.2, 0.4)*** | 0.9 (0.6, 1.3) | 28 (20, 36)** | 105 (58, 151) |
| Pathology services | 62 (277)*** | 83 (73) | 7.3 (6.2, 8.4)*** | 14.9 (11.4, 18.3) | 116 (100, 132)*** | 232 (189, 276) |
| Therapeutic procedures | 9 (39)*** | 30 (26) | 0.3 (0.1, 0.4)** | 1.3 (0.6, 2.1) | 21 (9, 33)* | 207 (50, 364) |
| Total medical services | 75 (339)** | 91 (80) | 22.6 (20.4, 24.8)*** | 42.1 (35.2, 49.0) | 1053 (954, 1151)*** | 2180 (1748, 2612) |
| Pharmaceuticals (no. unique medications) | 98 (443) | 99 (87) | 13.7 (13.1, 14.2)*** | 17.5 (15.7, 19.3) | 1821 (1687, 1955)*** | 2693 (2303, 3083) |
| Hospital admissions | 22 (97)*** | 40 (35) | 0.4 (0.3, 0.5)* | 1.2 (0.5, 2.0) | 2819 (1961, 3677)* | 5585 (3045, 8126) |
| Emergency department | 14 (59) | 18 (20) | 0.2 (0.1, 0.3) | 0.2 (0.1, 0.3) | 139 (97, 181) | 166 (61, 272) |
| Total health care utilisation costs | ‐ | ‐ | ‐ | ‐ | 5832b (4911, 6753)** | 10 624 (7728, 13 520) |
| Total resource use costs | ‐ | ‐ | 88 148c (86 587, 89 710) | 83 790 (79 131, 88 450) | ||
Note. See online supplement for further explanation of the costs. ACFI indicates Aged Care Funding Instrument.
US$62 700.
US$4442.
US$67 142.
P < .05.
P < .01.
P < .001.
Across all health care components, a lower proportion of participants with dementia accessed services in comparison to those without dementia (Table 4). The mean number of services accessed was also significantly lower for participants with dementia for all health care components except other attendances (nursing, optometry, etc.) and emergency presentations. Accordingly, total health care costs and costs of all individual health care components except emergency presentations were significantly lower for participants with dementia. Median total health care costs were also significantly lower for those with dementia in comparison to those without (dementia: $2947, no dementia: $5556, P < .0001).
Despite the higher residential care costs for people with dementia, lower health care utilisation meant that there was no significant difference in total resource use (residential care plus health care) costs by dementia status. The mean annual whole‐of‐system cost for those with dementia was about $88 000 (US$67 100; Table 4 and Table S2 in the Supporting Information).
The single largest component of total costs was for provision of residential care in both groups, representing 93% of all costs for people with dementia (Figure 1). Hospital admission costs accounted for the largest proportion of health care costs: 48% for those with dementia and 53% for those without dementia. Pharmaceuticals and general practitioner attendances costs accounted for 31% and 14% of health care costs, respectively, for participants with dementia. Other components of health care represented a relatively low proportion of health care costs (<10%) (See online supplement for further explanation of results).
Figure 1.
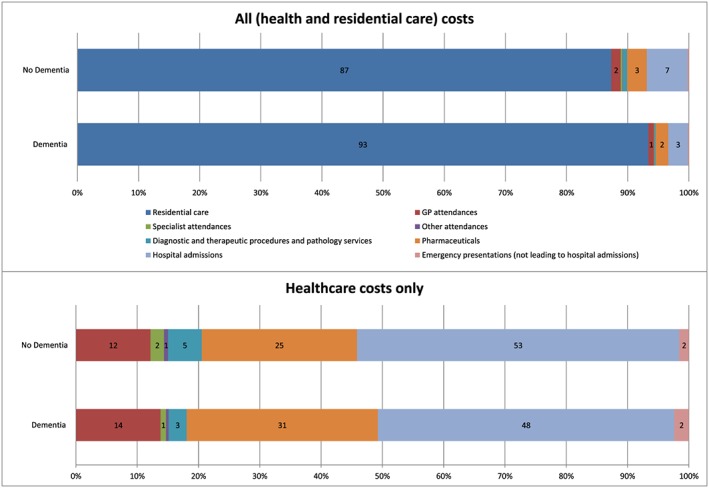
Components of resource use as proportions (mean) of all (health plus residential care) costs (top half) and healthcare costs (bottom half)
4. DISCUSSION
In this Australian study of individuals in long‐term residential aged care, the annual whole‐of‐system costs of those living with dementia was approximately AU$ 88 000 (US$ 67 100) per person from a broad health and residential care provision perspective. This estimate was derived by using individual level resource use data including both government and out of pocket costs of residential care plus out‐of‐hospital and in‐hospital all‐cause health care utilisation. This analysis provides, for the first time, a comprehensive estimate of the direct costs of providing health and residential care for this population in Australia using a predominantly bottom‐up approach.
The direct costs for a person living with dementia in a care setting in Australia have recently been estimated as $55 904 for the first year after diagnosis and $23 810 for subsequent years.14 These modelled estimates only included health care costs that were directly attributable to dementia and residential care costs from an out of pocket cost perspective.
Our costing, in contrast, provides an estimate capturing costs to both government and individuals, based on individual all‐cause resource use of people with dementia living long‐term in residential care. In the absence of a cost estimate from a societal perspective, such a comprehensive estimate is important for planning for both providers and policy makers and quantifies the financial impact of dementia in this population.
Previous estimates of direct costs of dementia for people living in institutionalised settings from a societal perspective, across a range of countries, range between AU$15 000 and 73 000 (in 2013 prices), with an average of $41 000.8, 14 While it is clear that some estimates are only for costs directly attributable to dementia, this is unclear for other estimates. In another review that reported all‐cause costs separately, the total costs of dementia for people living in residential care including informal care costs ranged from US$22 000 up to US$48 000 in 2006.9 Our costing of approximately AU$88 000 (US$ 67 100) per person in 2016 shows that the cost of care for people with dementia is substantial and potentially higher than previously estimated. True costs would be even higher if informal care and other indirect and intangible costs are taken into consideration.
In our estimate of whole‐of‐system costs, the highest proportion of costs are those incurred for the provision of residential care (93% for people with dementia). This proportion is similar to the estimate of 88% of direct health costs being due to residential care for all people living with dementia in a 2002 Australian estimate10 and in a more recent study in the UK (95%).28 It is also consistent with the range (85‐100%) reported for people living in residential care in an international review.8
The secondary aim of this analysis was to compare the costs between participants with dementia and those without. Lower health care costs for those living with dementia were driven by lower hospital admissions, emergency presentations, medical services, and pharmaceutical use. This has been observed previously in people with dementia in long‐term care29, 30 and in the last few years of life.31 These differences may be a function of the baseline differences between the groups; comorbidities were marginally lower and functional status was worse for those with dementia. Comorbidities such as diseases of the respiratory or circulatory system or congestive heart failure are associated with higher rates of hospitalisation in residents of care facilities32; thus, the higher rates of comorbidities in those without dementia in our study may partly explain the higher rate of hospital admissions. The differences in our study likely reflect differences between these populations in most residential care settings.
Hospital admissions represented a large proportion of direct health care costs (ie, excluding costs of residential care), being 48% for those with dementia. However, a low proportion of total admissions in this study were due to ambulatory‐care sensitive conditions (below the national performance target of 8.5%33), so it is considered that the majority of these were unavoidable.
Some of the facilities in this study provided specialised care for people with dementia. It has previously been suggested that in a managed care environment, secondary and tertiary prevention measures may improve care and therefore reduce the cost of caring for those with dementia.31 However, further exploration of the drivers for cost differences between these groups was considered beyond the scope of this analysis but warrants further exploration in future studies.
This study has a number of strengths. We collected comprehensive data on an older population living in residential care with a high prevalence of cognitive impairment that is largely similar to the residential aged care population in Australia (Table S1 in the Supporting Information). All resource use data and costing were based on individual data with linked health care utilisation. This predominately bottom‐up costing approach provides precision and is sensitive to differences within the population being studied. For the first time, residential care costs were estimated by using the ACFI assessment, so these are sensitive to the individual care needs of the population. However, this approach is not affected by facility‐level factors such as type of provider or size of facility. While the ACFI‐based care costs equate the funding provided for care for these individuals, it may not completely reflect the actual cost of care provided from the providers' perspective. Future costing studies should also address cost variations due to additional factors including the type and size of both care facilities and providers. Considering the rigours of collecting complex data in this population, this study is relatively large with a good cross section of care facilities across urban and rural locations across Australia.
We examined the costs of dementia as a broad perspective of health and social service provision. The costing methodology follows standard Australian guidelines20 and, as such, is robust in methodology. The costing approach is generally conservative. Data on public hospital utilisation and emergency presentations are from government administrative records. Private hospital utilisation is less comprehensively recorded in some jurisdictions and hence may be underestimated. However, these administrative records are considered to be more reliable than retrospective self‐report or records of the care facilities, particularly in this population.34
Additionally, there is some under estimate of out‐of‐hospital medical services and associated costs due to missing data. These services accounted for a small proportion (<2%) of total health and residential care costs (Figure 1). Accordingly, the differences by dementia status for these services need to be interpreted with caution.
The study participants were those living in residential care for 12 months or more. Hence, this costing provides a resource use and cost estimate reflective of the costs of ongoing care and is likely to provide a source for conservative estimates in comparison to all residents of aged care facilities.
Limitations of the study are primarily related to the observational nature of the study. The participating facilities were intentionally approached based on a high prevalence of residents living with dementia in their facilities and 82% of the facilities provided some level of dementia‐specific care. All consenting facilities were run by not‐for‐profit providers. Thus, generalisability of the study findings to both facilities that do not provide dementia‐specific care and to the for‐profit sector may be limited. However, approximately 70% of all permanent residents in care in Australia live in a not‐for profit facility.23 Both specialised dementia care facilities and not‐for‐profit providers may provide a higher quality of care for people living with dementia; thus, the estimate of the costs of residential and health care utilisation within this study may be conservative.35
5. CONCLUSION
In a sample of Australians living permanently in residential care, the annual cost of residential and health care for those living with dementia is approximately AU$88 000 per person (US$ 67 100). The costs of residential care were estimated as comprising 93% of the total whole‐of‐system cost for this population. The direct health care costs were driven mainly by the cost of hospital admissions (48% of health care costs), pharmaceuticals (31%), and attendances (14%). This analysis provides, for the first time, a comprehensive estimate of the cost of providing health and residential care for this population using individual service use data and a predominantly bottom‐up costing approach. The cost is significantly higher than that obtained with other perspectives or approaches, reflecting a significant financial burden of care for people with dementia.
FUNDING
This work was supported by funding provided by the National Health and Medical Research Council (NHMRC) Partnership Centre on Dealing with Cognitive and Related Functional Decline in Older People (CDPC) (grant number GNT9100000). The contents of the published materials are solely the responsibility of the Administering Institution, Flinders University, and the individual authors identified and do not reflect the views of the NHMRC or any other Funding Bodies or the Funding Partners. Tiffany Easton was supported by a CDPC PhD Scholarship and an Australian Government Research Training Programme Scholarship.
CONFLICT OF INTEREST
None declared.
Supporting information
Table S1. Comparison of Investigating Services Provided in the Residential Care Environment for Dementia (INSPIRED) study population individual and facility‐level characteristics with population estimates (Australian Institute of Health and Welfare [AIHW] National Aged Care Data Clearinghouse 2014/2015)
Table S2. Annual resource use and costs per person (2016 US$s) by dementia status
Gnanamanickam ES, Dyer SM, Milte R, et al. Direct health and residential care costs of people living with dementia in Australian residential aged care. Int J Geriatr Psychiatry. 2018;33:859–866. https://doi.org/10.1002/gps.4842
[Correction added on 19 March 2018, after first online publication: Figure 1 was replaced to represent the data in Table 4 and inconsistencies in reporting of some numbers were corrected. See online supplement for details.
REFERENCES
- 1. Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63, e62‐75. [DOI] [PubMed] [Google Scholar]
- 2. Organization for Economic Cooperation and Development . Health at a Glance 2011: OECD Indicators. OECD; 2011. [Google Scholar]
- 3. AIHW . Residential Aged Care and Home Care 2014–15 (web report). Canberra: AIHW; 2016. Cat. no. WEB 133. [Google Scholar]
- 4. Prince M, Comas‐Herrera A, Knapp M, Guerchet M, Karagiannidou M. World Alzheimer report 2016: improving healthcare for people living with dementia: coverage, quality and costs now and in the future. 2016.
- 5. Bynum JPW, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, Medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187‐194. [DOI] [PubMed] [Google Scholar]
- 6. Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. JAMA. 2012;307(2):165‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sköldunger A, Fastbom J, Wimo A, Fratiglioni L, Johnell K. The impact of dementia on drug costs in older people: results from the SNAC study. BMC Neurol. 2016;16(1):28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schaller S, Mauskopf J, Kriza C, Wahlster P, Kolominsky‐Rabas PL. The main cost drivers in dementia: a systematic review. Int J Geriatr Psychiatry. 2015;30(2):111‐129. [DOI] [PubMed] [Google Scholar]
- 9. Quentin W, Riedel‐Heller S, Luppa M, Rudolph A, König HH. Cost‐of‐illness studies of dementia: a systematic review focusing on stage dependency of costs. Acta Psychiatr Scand. 2010;121(4):243‐259. [DOI] [PubMed] [Google Scholar]
- 10. Access Economics . The Dementia Epidemic: Economic Impact and Positive Solutions for Australia: Prepared for Alzheimer's Australia. Alzheimer's Australia; 2003. [Google Scholar]
- 11. Wimo A, Jonsson L, Winblad B. An estimate of the worldwide prevalence and direct costs of dementia in 2003. Dement Geriatr Cogn Disord. 2006;21(3):175‐181. [DOI] [PubMed] [Google Scholar]
- 12. Jonsson L, Wimo A. The cost of dementia in Europe: a review of the evidence, and methodological considerations. Pharmacoeconomics. 2009;27: 391+ [DOI] [PubMed] [Google Scholar]
- 13. Wimo A, Winblad B, Jonsson L. The worldwide societal costs of dementia: estimates for 2009. Alzheimers Dement. 2010;6(2):98‐103. [DOI] [PubMed] [Google Scholar]
- 14. Brown L, Hansnata E, Anh La H. Economic Cost of Dementia In Australia 2016–2056. Alzheimer's Australia: Canberra; 2017. [Google Scholar]
- 15. Brouwer W, Rutten F, Koopmanschap M. Costing in economic evaluations In: Drummond MF, McGuire A, eds. Economic Evaluation in Health Care: Merging Theory with Practice. New York: Oxford University Press; 2001. [Google Scholar]
- 16. Lang L, Clifford A, Wei L, et al. Prevalence and determinants of undetected dementia in the community: a systematic literature review and a meta‐analysis. BMJ Open. 2017;7(2): [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lithgow S, Jackson GA, Browne D. Estimating the prevalence of dementia: cognitive screening in Glasgow nursing homes. Int J Geriatr Psychiatry. 2012;27(8):785‐791. [DOI] [PubMed] [Google Scholar]
- 18. Jorm AF, Mackinnon AJ, Henderson AS, et al. The Psychogeriatric Assessment Scales: a multidimensional alternative to categorical diagnoses of dementia and depression in the elderly. Psychol Med. 1995;25(3):447‐460. [DOI] [PubMed] [Google Scholar]
- 19. AIHW . Health Expenditure Australia 2014–15. AIHW; 2016. [Google Scholar]
- 20. Department of Health . Manual of resource items and their associated unit costs: for use in submissions to the Pharmaceutical Benefits Advisory Committee involving economic analyses. 2016; http://www.pbs.gov.au/info/industry/useful-resources/manual. Accessed March 27, 2017.
- 21. Australian Taxation Office . Foreign currency exchange rates for financial year 2016. 2016; https://www.ato.gov.au/tax-professionals/tp/financial-year-ending-30-june-2016/. Accessed March 15, 2017.
- 22. Department of Health . Aged Care Funding Instrument (ACFI): User Guide. Canberra; 2016. [Google Scholar]
- 23. Australian Government Aged Care Financing Authority . Fourth Report on the Funding and Financing of the Aged Care Sector. 2016. [Google Scholar]
- 24. Department of Health . Medicare benefits schedule. 2017; http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Home. Accessed June 26, 2017.
- 25. Australian Consortium for Classification Development . AR‐DRG. 2016; https://www.accd.net.au/ArDrg.aspx. Accessed March 03, 2017.
- 26. Independent Hospital Pricing Authority . Australian Public Hospitals Cost Report 2013–14 Round 18 2016. [Google Scholar]
- 27. Department of Health . Pharmaceutical benefits scheme. 2017; http://www.pbs.gov.au/pbs/home. Accessed June 27, 2017.
- 28. Romeo R, Knapp M, Salverda S, Orrell M, Fossey J, Ballard C. The cost of care homes for people with dementia in England: a modelling approach. Int J Geriatr Psychiatry. 2016; n/a‐n/a [DOI] [PubMed] [Google Scholar]
- 29. Becker M, Andel R, Boaz T, Howell T. The association of individual and facility characteristics with psychiatric hospitalization among nursing home residents. Int J Geriatr Psychiatry. 2009;24(3):261‐268. [DOI] [PubMed] [Google Scholar]
- 30. Gimm GW, Kitsantas P. Falls, depression, and other hospitalization risk factors for adults in residential care facilities. Int J Aging Hum Dev. 2016;83(1):44‐62. [DOI] [PubMed] [Google Scholar]
- 31. McCormick WC, Hardy J, Kukull WA, et al. Healthcare utilization and costs in managed care patients with Alzheimer's disease during the last few years of life. J Am Geriatr Soc. 2001;49(9):1156‐1160. [DOI] [PubMed] [Google Scholar]
- 32. Grabowski DC, Stewart KA, Broderick SM, Coots LA. Predictors of nursing home hospitalization: a review of the literature. Med Care Res Rev. 2008;65(1):3‐39. [DOI] [PubMed] [Google Scholar]
- 33. Council of Australian Governments . National Health Care Agreement 2012. Canberra; 2012. [Google Scholar]
- 34. Bhandari A, Wagner T. Self‐reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63(2):217‐235. [DOI] [PubMed] [Google Scholar]
- 35. Dwyer R, Stoelwinder J, Gabbe B, Lowthian J. Unplanned transfer to emergency departments for frail elderly residents of aged care facilities: a review of patient and organizational factors. J Am Med Dir Assoc. 2015;16(7):551‐562. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Comparison of Investigating Services Provided in the Residential Care Environment for Dementia (INSPIRED) study population individual and facility‐level characteristics with population estimates (Australian Institute of Health and Welfare [AIHW] National Aged Care Data Clearinghouse 2014/2015)
Table S2. Annual resource use and costs per person (2016 US$s) by dementia status


