Primary Biliary Cholangitis (PBC) is a chronic autoimmune liver disease characterized by immune-mediated damage to biliary epithelial cells resulting in inflammation, progressive fibrosis, cirrhosis, and liver failure (1). While its precise etiopathogenesis remains unclear, the disease is likely to develop in a genetically susceptible host after exposure to an as yet, undefined environmental trigger (Figure 1). The genetic contribution to PBC risk is highlighted by several lines of evidence that demonstrate a high concordance of disease in monozygotic twins (2), an increased prevalence in first-degree relatives (FDRs) of affected probands, a sibling relative risk (RR) of 10.5 (3), and a high prevalence of disease specific anti-mitochondrial antibodies (AMA) in FDRs of affected relatives compared to population controls (4). Furthermore, large-scale genome wide surveys (GWAS) have identified several single nucleotide polymorphisms (SNP) associated with PBC, though the majority of these SNPs are also associated with other autoimmune diseases.
Figure 1.
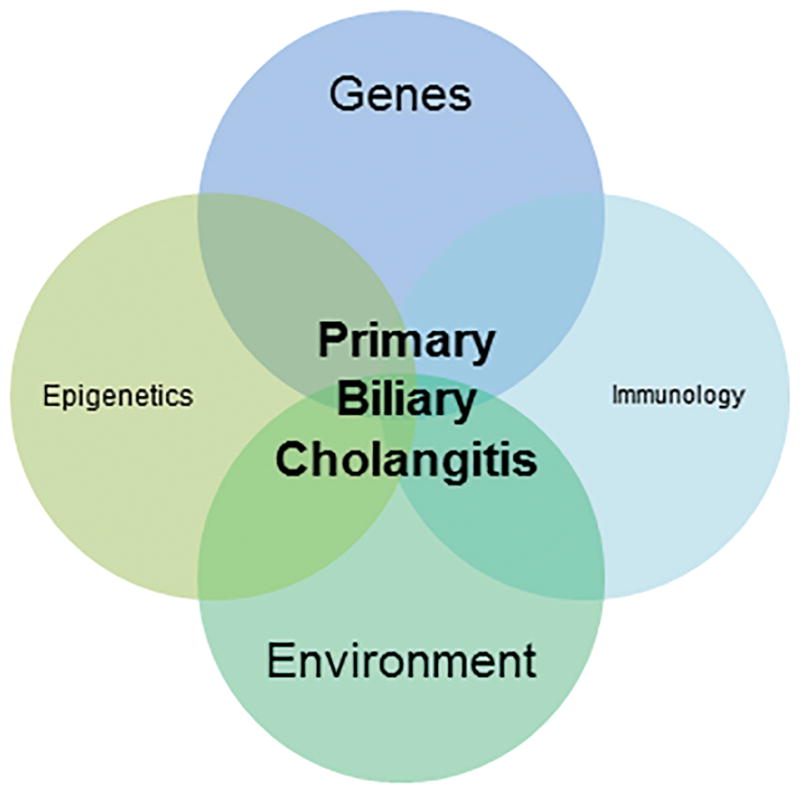
Venn Diagram demonstrating the interaction between various biologic processes including genetics, epigenome, environment and immunologic system in contributing to disease development.
In the current issue of HEPATOLOGY, Ornolfsson et al. use a unique Icelandic database to define the familial risk of PBC beyond FDRs. Applying population-level and otherwise unprecedented genealogical data on all living Icelanders and most of their ancestors since the island’s settlement, the authors report the RR of PBC and the average kinship coefficient (KC) in first- through fifth-degree relatives of PBC patients compared to age, sex, and number of known relative matched controls. A 9.13-fold (95% CI 4.17–16.76) increased risk of PBC in FDRs was demonstrated, with a lower, but still significantly increased risk also noted among second- and third-degree relatives with RR of 3.61 (95% CI 1.48–8.92), and 2.59 (95% CI 1.35–4.67), respectively. Among fourth- and fifth-degree relatives, the increased risk of PBC trended towards significance with a RR of 1.66 (95% CI 1.00–3.02) and 1.42 (95% CI 0.99–2.20), respectively. The KC, defined as the probability that two randomly selected autosomal alleles from two individuals are inherited from the same ancestor, was used as a measure of relatedness of PBC patients compared to the general population. Using this metric, PBC patients were shown to be more genetically related that population controls, even after step-wise exclusion of relatives within one to six meiotic distances. The authors rightfully conclude that their data expand on previous reports by describing familial risk of disease well beyond FDRs. Furthermore, they suggest that these findings emphasize the importance of genetic risk in the pathogenesis of PBC and support future investment in understanding the genetic underpinnings of this disease.
Do these data demonstrate that genetic susceptibility is acting alone to cause disease? Not necessarily. As with most autoimmune diseases, PBC is complex, and while genetics are important, it is highly likely that individual alleles are not deterministic, but rather act by modifying risk through their effect on disease-specific biologic processes in the context of environmental exposures. One important limitation of this study is the paucity of data on the shared environment among relatives. The authors report a high RR of PBC in FDRs as well as in more distant relatives, however the potential effect of environmental exposures on reported risk is not described, which admittedly is a challenging task. We all know that relatives share genes and often environmental exposures. Several epidemiologic studies have demonstrated consistent associations between environmental agents such as cigarette smoking and urinary tract infections (UTI) and the development of PBC. Studies from the United States and United Kingdom demonstrated an increased risk of PBC in those with a history of smoking; and furthermore, the French group demonstrated higher levels of exposure to cigarette smoke including from possible second-hand sources as being associated with PBC (5) (6). A history of prior UTI or recurrent UTIs has also repeatedly been associated with disease; and interestingly, Escherichia coli, the most common culprit pathogen, was a strong inducer of PDC-E2 specific AMA and PBC associated histologic changes in a mouse model (7), suggesting that E. coli exposure may be a relevant trigger in a genetically susceptible host. It remains unconfirmed whether molecular mimicry serves as the primary mechanism by which such environmental exposures act as cross-reactive epitopes to break immunologic self-tolerance. The complexity of heritability of PBC is further emphasized by studies in FDRs of patients. Our group reported a high prevalence of disease-specific AMA in FDRs of affected probands, yet longitudinal follow up of these subjects demonstrated a low risk (4%) of developing PBC after more than eight years of follow-up in this expected high risk cohort (8). This suggests that while genetics may be important in conferring risk, different environmental exposures or other as yet unknown risk factors even among FDRs are likely requisite for overt disease to develop. Given that Iceland is a relatively small and geographically remote region with two-thirds of the population living in and around the 106-square mile capital city, it seems possible that shared environmental exposures could affect the reported risk of disease, even beyond the nuclear family. An extension of this study including genetic data demonstrating the shared PBC-associated risk loci among affected relatives would be of great interest given the well-established effort and data of genome sequencing of the Icelandic population by de CODE (www.decode.com).
Another relevant consideration is that the familial clustering of PBC reported by the authors may not be limited to PBC specifically, but may reflect a familial predisposition to autoimmunity, in general. Importantly, nearly one-third of PBC patients are also affected by another autoimmune disease, and in keeping with this observation, the vast majority of genetic risk loci implicated in PBC have also been associated with other autoimmune diseases. This shared association among diverse autoimmune diseases suggests the presumed pleiotropic effect of reported genetic variants (i.e., SNPs, etc) and emphasizes that, at least among common variants detected by genome wide surveys, there are likely few truly PBC-specific genetic associations.
In the current landscape, it is estimated that only about 15% of the heritability of PBC has been explained, in part because in addition to common genetic variation identified through GWAS, highly penetrant rare variants with strong biologic effect, epigenetic modifications, gene-gene, and gene-environment interactions likely also play an important role (9). As the authors suggest, further investigation into the genetic basis of disease is certainly warranted. However, moving forward, understanding the functional consequences of identified genetic variation needs to be prioritized if progress is to be made in elucidating the pathogenesis of this enigmatic disease. Recently, it has been suggested that while GWAS may readily identify variants that influence gene regulation, these may not necessarily be involved in disease specific processes, but instead may have a peripheral role through action on regulatory networks that modulate a smaller number of core rare variants (10). Thus, while further efforts aimed at dissecting the genetic contribution to PBC are warranted, these should aim to provide insight about functionally relevant regulatory pathways and clinically important phenotypes.
In summary, the study by Ornolfsson et al. utilizes a highly unique population based cohort to demonstrate an increased risk of PBC in relatives beyond the traditional nuclear family and FDRs. While these findings highlight the importance of genetic susceptibility to disease, the precise causal variants, likely important environmental triggers, and relevance of the interaction between these variables in disease pathogenesis, remains largely unclear. Future work in characterizing genetic variants of functional relevance to PBC and important environmental triggers are certainly needed to better elucidate this complex disease and improve outcomes for patients.
Acknowledgments
Grant Support: Supported by NIH grant RO1 DK 080670.
References
- 1.Hirschfield GM, Gershwin ME. The immunobiology and pathophysiology of primary biliary cirrhosis. Annu Rev Pathol. 2013;8:303–330. doi: 10.1146/annurev-pathol-020712-164014. [DOI] [PubMed] [Google Scholar]
- 2.Selmi C, Mayo MJ, Bach N, Ishibashi H, Invernizzi P, Gish RG, et al. Primary biliary cirrhosis in monozygotic and dizygotic twins: genetics, epigenetics, and environment. Gastroenterology. 2004;127:485–492. doi: 10.1053/j.gastro.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Jones DE, Watt FE, Metcalf JV, Bassendine MF, James OF. Familial primary biliary cirrhosis reassessed: a geographically-based population study. J Hepatol. 1999;30:402–407. doi: 10.1016/s0168-8278(99)80097-x. [DOI] [PubMed] [Google Scholar]
- 4.Lazaridis KN, Juran BD, Boe GM, Slusser JP, de Andrade M, Homburger HA, et al. Increased prevalence of antimitochondrial antibodies in first-degree relatives of patients with primary biliary cirrhosis. Hepatology. 2007;46:785–792. doi: 10.1002/hep.21749. [DOI] [PubMed] [Google Scholar]
- 5.Parikh-Patel A, Gold EB, Worman H, Krivy KE, Gershwin ME. Risk factors for primary biliary cirrhosis in a cohort of patients from the united states. Hepatology. 2001;33:16–21. doi: 10.1053/jhep.2001.21165. [DOI] [PubMed] [Google Scholar]
- 6.Corpechot C, Chretien Y, Chazouilleres O, Poupon R. Demographic, lifestyle, medical and familial factors associated with primary biliary cirrhosis. J Hepatol. 2010;53:162–169. doi: 10.1016/j.jhep.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 7.Wang JJ, Yang GX, Zhang WC, Lu L, Tsuneyama K, Kronenberg M, et al. Escherichia coli infection induces autoimmune cholangitis and anti-mitochondrial antibodies in non-obese diabetic (NOD). B6 (Idd10/Idd18) mice. Clin Exp Immunol. 2014;175:192–201. doi: 10.1111/cei.12224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gulamhusein AF, Juran BD, Atkinson EJ, McCauley B, Schlicht E, Lazaridis KN. Low incidence of primary biliary cirrhosis (PBC) in the first-degree relatives of PBC probands after 8 years of follow-up. Liver Int. 2016;36:1378–1382. doi: 10.1111/liv.13143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu JZ, Almarri MA, Gaffney DJ, Mells GF, Jostins L, Cordell HJ, et al. Dense fine-mapping study identifies new susceptibility loci for primary biliary cirrhosis. Nat Genet. 2012;44:1137–1141. doi: 10.1038/ng.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liaskou E, Hirschfield GM. Genetic association studies and the risk factors for developing the ‘immuno-bile-logic’ disease PBC. Hepatology. 2017 doi: 10.1002/hep.29603. [DOI] [PubMed] [Google Scholar]


