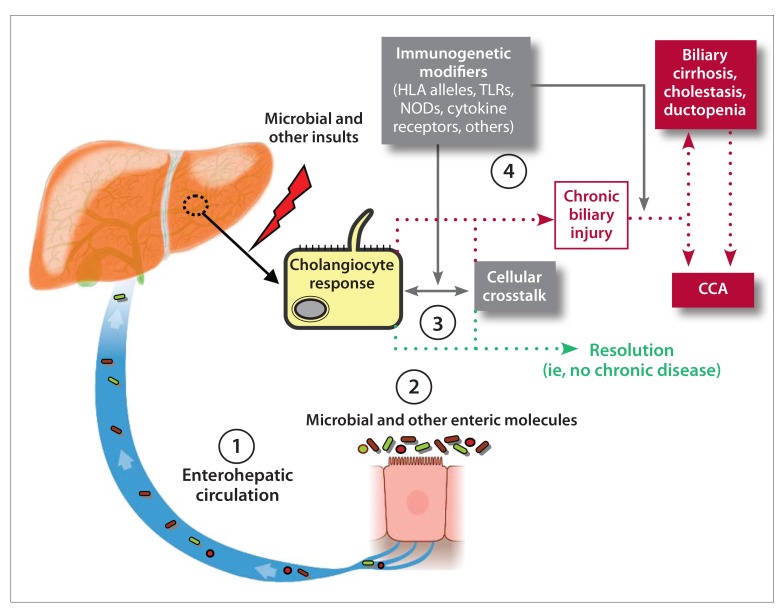
Figure.
A conceptual model of the etiopathogenesis and natural history of PSC. Biliary epithelial cells (ie, cholangiocytes) exist in an environment with multiple potential etiologic mediators of hepatobiliary injury. Approximately 95% of bile acids are reabsorbed in the terminal ileum and, together with other intestinal molecules, are transported back to the liver via the enterohepatic circulation. Portal blood flows into hepatic sinusoids, wherein hepatocytes may take up and modify these molecules and secrete them into bile, which is synthesized by hepatocytes and delivered into canaliculi by means of specialized membrane transporters. Canalicular bile drains into the biliary tree and is modified by cholangiocytes as it percolates through the biliary tree. Cholangiocytes recognize (eg, through cell surface receptors) and react to various molecules and may release chemokines/cytokines, growth factors, and morphogens, initiating both autocrine and paracrine signaling cascades. With respect to the source of hepatobiliary injury, it remains uncertain whether there is (1) increased exposure to microbial molecules (eg, through the enterohepatic circulation, potentially facilitated by compromised intestinal barrier function), (2) alteration to the repertoire of microbial and other intestinal molecules (eg, due to microbial dysbiosis, xenobiotics), and/or (3) an aberrant or exaggerated cholangiocyte (or another hepatic cell) response to these molecules (eg, increased induction of cholangiocyte senescence and the senescence-associated secretory phenotype). In addition, host immunogenetics (4) likely modulate the development and/or impact of any of these variables and thus play a role in determining whether hepatobiliary injury resolves or if it persists and results in chronic disease (ie, PSC). These variables may also determine whether PSC progresses to its associated major clinical endpoints, including CCA and cirrhosis. Further investigation of the cellular, molecular, and microbial interactions and signaling represented in this figure is underway and expected to advance understanding of the etiopathogenesis of PSC.
CCA, cholangiocarcinoma; HLA, human leukocyte antigen; NOD, nucleotide-binding oligomerization domain receptor; PSC, primary sclerosing cholangitis; TLR, toll-like receptor.