Abstract
Context
Steroid 5α-reductase inhibitors are used to treat benign prostatic hyperplasia and androgenic alopecia, but the role of 5α-dihydrotestosterone (DHT) in mediating testosterone’s effects on muscle, sexual function, erythropoiesis, and other androgen-dependent processes remains poorly understood.
Objective
To determine whether testosterone’s effects on muscle mass, strength, sexual function, hematocrit level, prostate volume, sebum production, and lipid levels are attenuated when its conversion to DHT is blocked by dutasteride (an inhibitor of 5α-reductase type 1 and 2).
Design, Setting, and Patients
The 5α-Reductase Trial was a randomized controlled trial of healthy men aged 18 to 50 years comparing placebo plus testosterone enthanate with dutasteride plus testosterone enanthate from May 2005 through June 2010.
Interventions
Eight treatment groups received 50, 125, 300, or 600 mg/wk of testosterone enanthate for 20 weeks plus placebo (4 groups) or 2.5 mg/d of dutasteride (4 groups).
Main Outcome Measures
The primary outcome was change in fat-free mass; secondary outcomes: changes in fat mass, muscle strength, sexual function, prostate volume, sebum production, and hematocrit and lipid levels.
Results
A total of 139 men were randomized; 102 completed the 20-week intervention. Men assigned to dutasteride were similar at baseline to those assigned to placebo. The mean fat-free mass gained by the dutasteride groups was 0.6 kg (95% CI, −0.1 to 1.2 kg) when receiving 50 mg/wk of testosterone enanthate, 2.6 kg (95% CI, 0.9 to 4.3 kg) for 125 mg/wk, 5.8 kg (95% CI, 4.8 to 6.9 kg) for 300 mg/wk, and 7.1 kg (95% CI, 6.0 to 8.2 kg) for 600 mg/wk. The mean fat-free mass gained by the placebo groups was 0.8 kg (95% CI, −0.1 to 1.7 kg) when receiving 50 mg/wk of testosterone enanthate, 3.5 kg (95% CI, 2.1 to 4.8 kg) for 125 mg/wk, 5.7 kg (95% CI, 4.8 to 6.5 kg) for 300 mg/wk, and 8.1 kg (95% CI, 6.7 to 9.5 kg) for 600 mg/wk. The dose-adjusted differences between the dutasteride and placebo groups for fat-free mass were not significant (P = .18). Changes in fat mass, muscle strength, sexual function, prostate volume, sebum production, and hematocrit and lipid levels did not differ between groups.
Conclusion
Changes in fat-free mass in response to graded testosterone doses did not differ in men in whom DHT was suppressed by dutasteride from those treated with placebo, indicating that conversion of testosterone to DHT is not essential for mediating its anabolic effects on muscle.
Trial Registration
clinicaltrials.gov Identifier: NCT00493987
5α-DIHYDROTESTOSTERONE (DHT) is a potent metabolite of testosterone; its role in post-embryonic life remains poorly understood. At least 2 isoenzymes of steroid 5α-reductase convert testosterone to DHT in humans.1–3 In marsupials and possibly in humans, DHT also can be produced from other substrates via 1 or more alternate pathways.3–5 Studies of the kindred with steroid 5α-reductase 2 mutations,6,7 and mice with genetic or pharmacological disruption of steroid 5α-reductase enzymes,8,9 suggest that DHT serves an important role in the formation of prostate and phallus.
An improved understanding of the role of steroid 5α-reductases has important clinical implications. Pharmacological inhibitors of steroid 5α-reductases are used to treat benign prostatic hyperplasia10,11 and androgenic alopecia,12 disorders of middle-aged and older men, who are at risk of reduced muscle mass and sexual dysfunction. Similarly, nonsteroidal selective androgen receptor modulators (SARMs) currently in development do not undergo 5α-reduction. Therefore, the safety of 5α-reductase inhibitors and nonsteroidal SARMs is predicated upon the supposition that 5α-reduction is not essential for mediating androgen’s effects on muscle mass and strength and on sexual function. Sexual dysfunction has been reported as an adverse event in clinical trials of 5α-reductase inhibitors in men with benign prostatic hyperplasia, who have high background rates of sexual dysfunction. However, it has been debated whether sexual dysfunction in older men receiving 5α-reductase inhibitors is causally related to these drugs and whether DHT is required for optimal erectile function.13,14 Similarly, the role of DHT in mediating androgenic effects on sebum production, bone markers, and levels of hematocrit, hemoglobin, and lipids in men remains unclear.
The primary objective of this study was to determine whether 5α-reduction of testosterone to DHT is obligatory for mediating its effects on fat-free mass. Secondary objectives were to determine whether 5-α reduction of testosterone is necessary for the maintenance of androgen effects on sexual function, hematocrit, sebum production, bone markers, and lipid levels in men. Accordingly, we determined the responsiveness of these androgen-dependent outcomes in healthy men, in whom endogenous testosterone production had been suppressed by administration of a gonadotropin-releasing hormone agonist, to graded doses of testosterone in the absence and presence of dutasteride, a potent dual inhibitor of type 1 and type 2 5α-reductase isoenzymes.
METHODS
Study Design
The 5α-Reductase Trial was a parallelgroup, double-blind, randomized placebo-controlled trial. The first participant was enrolled in May 2005, the trial was registered in June 2007, and the last participant completed the trial in June 2010. The study was approved by the institutional review board of Boston University and all participants provided written informed consent. A data and safety monitoring board reviewed the data every 6 months.
Participants
A structured medical history, physical examination, blood counts and chemistries, and levels of testosterone, luteinizing hormone, follicle-stimulating hormone, and prostate-specific antigen (PSA) were obtained to determine eligibility. Self-reported race and ethnicity were recorded. The participants were healthy men, aged 18 to 50 years, with normal testosterone levels (300-1200 ng/dL; to convert to nmol/L, multiply by 0.0347).
We excluded men who had androgen deficiency, prostate cancer, lower urinary tract symptom score greater than 20, body weight greater than 135 kg, uncontrolled hypertension, hematocrit level greater than 51%, PSA level greater than 4 ng/mL (to convert to μg/L, multiply by 1.0), aspartate aminotransferase or alanine aminotransferase greater than 1.5 times the upper limit of normal, creatinine level greater than 2 mg/dL (to convert to μmol/L, multiply by 88.4), or men receiving glucocorticoids, growth hormone, androgens, or 5α-reductase inhibitors. The participants were paid $1000 if they completed the study or a prorated amount based on their participation time.
Interventions
Because administration of a 5α-reductase inhibitor raises testosterone levels,15–17 which could render the placebo and dutasteride groups unbalanced with respect to testosterone levels, we suppressed endogenous testosterone by administering a long-acting gonadotropin-releasing hormone agonist, and created different levels of circulating testosterone concentrations by administration of graded doses of testosterone enanthate. Based on dose-response studies in healthy men,18,19 we selected testosterone doses that would be expected to generate varying testosterone concentrations spanning the entire physiological range for men and extending well into the sub-physiological as well as the supraphysiological range. Accordingly, participants received monthly injections of 7.5 mg of leuprolide acetate (Lupron depot; TAP Pharmaceuticals) starting on the day of randomization. A randomization table was used to allocate individuals to 1 of 8 study groups (placebo plus 50, 125, 300, or 600 mg/wk of testosterone enanthate intramuscularly for 20 weeks or 2.5 mg/d of dutasteride plus 50, 125, 300, or 600 mg/wk of testosterone enanthate intramuscularly for 20 weeks). Because a 0.5-mg/d dose of dutasteride suppresses circulating and intraprostatic DHT by more than 94%,20–23 we used 2.5 mg/d of dutasteride, reasoning that this dose would assuredly suppress circulating and intratissue DHT. Study staff and participants were unaware of testosterone dose and whether they received dutasteride or placebo.
Outcomes
The primary outcome was change in fat-free mass from baseline measured by dual-energy x-ray absorptiometry. The selection of fat-free mass as the primary outcome was guided by our primary hypothesis, which was related to the role of 5α-reductase in mediating the anabolic effects of testosterone on muscle mass. Additionally, among various androgen-dependent processes, the dose-response relationships of testosterone are the most robust with fat-free mass. Finally, the issue of whether 5α-reduction of testosterone to DHT is obligatory for mediating its anabolic effects on the muscle has relevance to the safety of 5α-reductase inhibitors and nonsteroidal SARMs.
Secondary outcomes included fat mass, leg-press and chest-press strength, sexual function, sebum production, and prostate volumes, which were assessed at baseline and at week 20. Blood counts and chemistries, PSA level, presence or absence of acne, and adverse events were monitored.
Body composition was measured using dual-energy x-ray absorptiometry (Hologic QDR 4500A),24 which was calibrated using a soft-tissue phantom. Leg-press and chest-press strength were measured by the 1-repetition-maximum method using Keiser machines.25,26 The participants underwent 5 to 10 minutes of warm-up followed by progressive lifts leading up to the 1-repetition maximum. Strength was reassessed within 2 to 7 days; if the measurements were within 5%, the better of the 2 measurements was recorded.25,26 Sexual function was assessed using the International Index of Erectile Function.27 Additionally, we used the Male Sexual Health Questionnaire for a more comprehensive assessment of sexual desire28 than is provided by the International Index of Erectile Function.
Prostate volume was measured using 1.5-Tesla magnetic resonance imaging (Philips Medical Systems). The mixed-fast-spin echo-pulse sequence (slice thickness: 5 mm; interslice distance: 2 mm) was used to generate parametric T1 and T2 maps. Prostate glands were segmented using a dual-space clustering algorithm that interrogates each voxel to determine whether the voxel is contained within the user-predefined quantitative imaging space and a predefined anatomic space.29 Sebum production was measured using sebu tapes applied to the forehead, nose, and back for 12 hours.30 Acne was assessed using the Palatzi scale.31
Hormone Assays
Testosterone and DHT were measured using liquid chromatography tandem mass spectrometry32,33 with sensitivities of 2 and 5 ng/dL, respectively. The interassay coefficient of variation for the testosterone assay was 7.7% at 241 ng/dL of testosterone, 4.4% at 532 ng/dL of testosterone, and 3.3% at 1016 ng/dL of testosterone. Free testosterone and free DHT were calculated.34 Sex-hormone binding globulin and luteinizing hormone were measured using immunofluormetric assays with sensitivities of 2.5 nmol/L and 0.1 U/L, respectively.26,35
Statistical Analyses
Univariate analyses were performed to examine the distribution of variables. Within each group (4 placebo groups and 4 dutasteride groups), the dose effects were estimated using 1-way analysis of variance. Estimates of differences in outcomes between groups were obtained from multiple linear regression models controlling for testosterone enanthate dose. Dose-response curves in participants assigned to placebo vs dutasteride were compared using statistical interaction terms and associated significance tests.
To assess potential bias in the use of parametric methods to test differences, sensitivity analyses were conducted using nonparametric equivalents. Within groups, Kruskal-Wallis rank sum tests were used to assess dose relationships. Models considering both testosterone enanthate dose and group assignment were replicated using multiple regression, replacing outcomes with their global rank transformations.
The associations between changes in testosterone concentrations and outcomes were assessed using generalized additive models with tensor product smoothing. An offset square root transformation of change in testosterone was used to provide a coherent range of values for plotting.
Because this was not an efficacy trial, and our intent was to test a specific hypothesis under idealized conditions of the 5α-reductase blockade, the primary analysis included men who were randomized and had postrandomization assessment of the primary outcome during week 20. A secondary, full intention-to-treat analysis used multiple imputation by chained equations to assess the sensitivity for inclusion of participants with missing outcomes data. All statistical tests were 2-sided with type I error probability set at an α level of equal to .05. Because analyses were specified a priori, the results were not adjusted for multiple comparisons. Estimation and inference were performed using SAS version 9.3 (SAS Institute Inc) and R version 2.14.0 (R Foundation for Statistical Computing).
Based on dose-response studies in men,18,19 we anticipated that in placebo groups, administration of 50, 125, 300, and 600 mg/wk of testosterone enanthate would be associated with fat-free mass change of 1, 2, 4, and 8 kg, respectively, and a 1.5-kg within-dose SD of change in fat-free mass. With type I error fixed at .05, 52 men each completing 20 weeks of intervention in the placebo and dutasteride groups provided 90% power to detect a 25% difference in the mean effect of testosterone between the study groups, using 2-way analysis of variance. Sample size was therefore set at 120 men, anticipating a 15% drop-out rate, but was revised later to 139 because of the higher observed drop-out rate.
RESULTS
Of the 3792 men who underwent telephone screening, 189 met eligibility criteria, 139 were randomized, and 102 (54 in the placebo groups and 48 in the dutasteride groups) completed the 20-week intervention (FIGURE 1). Randomized participants had a mean (SD) age of 37.6 (8.7) years, body mass index (calculated as weight in kilograms divided by height in meters squared) of 26.3 (4.0), and fat-free mass of 62.7 (8.3) kg. Participants displayed similar baseline characteristics (TABLE).
Figure 1.
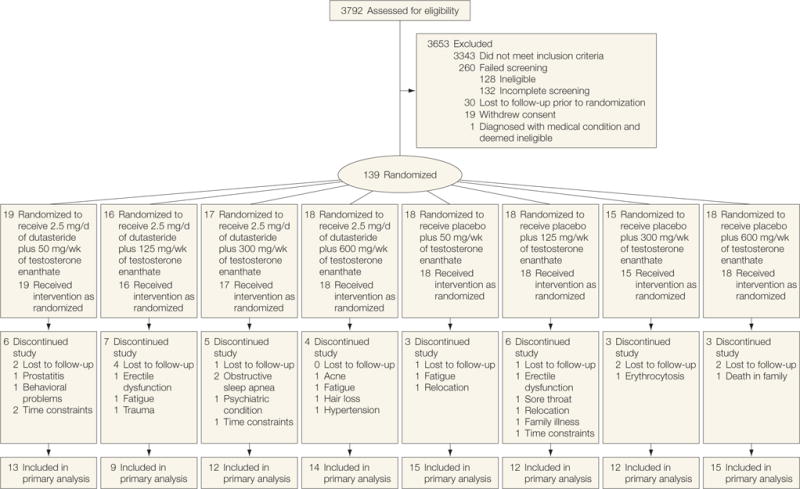
Flow of Participants Through the Trial
Table.
Baseline Characteristics of the Participants by Randomized Assignment (N = 102)a
| 2.5 mg/d of Dutasteride (n = 48) | Placebo (n = 54) | |||||||
|---|---|---|---|---|---|---|---|---|
| Dosage of Testosterone Enanthate, mg/wk | ||||||||
| 50 (n = 13) | 125 (n = 9) | 300 (n = 12) | 600 (n = 14) | 50 (n = 15) | 125 (n = 12) | 300 (n = 12) | 600 (n = 15) | |
| Demographics | ||||||||
| Age, y | 41 (9) | 40 (7) | 35(8) | 35 (9) | 39 (9) | 34 (8) | 37 (10) | 40 (8) |
| Height, cm | 174 (6) | 176 (7) | 175 (6) | 178 (7) | 177 (4) | 178 (9) | 177 (8) | 178 (6) |
| Weight, kg | 80 (10) | 84 (11) | 77 (14) | 86 (16) | 82 (13) | 84 (14) | 82 (12) | 82 (12) |
| Measures of body composition and muscle performance | ||||||||
| Fat-free mass, kg | 62 (7) | 63 (10) | 59 (9) | 66 (9) | 62 (7) | 64 (8) | 61 (7) | 63 (9) |
| Lean body mass, kg | 60 (7) | 60 (9) | 57 (9) | 63 (9) | 59 (7) | 61 (8) | 59 (7) | 60 (9) |
| Fat mass, kg | 16 (5) | 19 (7) | 16 (6) | 18 (10) | 19 (9) | 18 (8) | 19 (9) | 18 (6) |
| Leg-press strength, N | 2787 (482) | 3005 (834) | 2830 (648) | 3006 (731) | 2771 (499) | 2964 (498) | 2865 (543) | 2995 (789) |
| Leg-peak power, W | 1713 (340) | 1904 (458) | 1858 (516) | 2069 (592) | 1902 (448) | 2084 (520) | 2007 (488) | 1895 (441) |
| Chest-press strength, N | 784 (163) | 759 (228) | 713 (210) | 817 (272) | 711 (249) | 763 (142) | 734 (205) | 735 (249) |
| Baseline blood levels | ||||||||
| Total testosterone, ng/dL | 770 (275) | 842 (399) | 590 (198) | 676 (221) | 697 (320) | 701 (268) | 667 (175) | 776 (255) |
| Free testosterone, ng/dL | 16.8 (11.4) | 16.0 (9.0) | 11.9 (4.5) | 12.5 (4.6) | 12.1 (4.8) | 12.7 (5.6) | 12.8 (4.5) | 13.2 (5.1) |
| Total 5α-dihydrotestosterone, ng/dL | 50 (22) | 51 (13) | 49 (15) | 54 (23) | 59 (27) | 57 (22) | 54 (19) | 62 (27) |
| Free 5α-dihydrotestosterone, pg/mL | 4.7 (1.9) | 4.6 (2.1) | 4.7 (1.8) | 4.5 (2.6) | 4.5 (1.3) | 4.6 (1.3) | 5.4 (2.9) | 4.7 (1.5) |
| Luteinizing hormone, U/L | 3.2 (1.4) | 4.2 (3.8) | 3.5 (3.1) | 2.7 (1.1) | 3.8 (1.5) | 3.6 (1.2) | 3.4 (1.3) | 3.5 (1.1) |
| Prostate volume, cm3 | 20.3 (4.0) | 23.7 (3.2) | 21.4 (1.9) | 22.3 (3.4) | 22.2 (4.8) | 20.9 (3.7) | 23.7 (6.7) | 23.4 (3.2) |
| Prostate-specific antigen, ng/mL | 0.59 (0.24) | 0.60 (0.33) | 0.81 (0.20) | 0.75 (0.38) | 0.85 (0.40) | 0.42 (0.09) | 0.60 (0.27) | 0.77 (0.45) |
| Osteocalcin, ng/mL | 18.9 (5.0) | 18.3(4.9) | 20.6 (5.8) | 22.7 (6.7) | 26.5 (8.7) | 24.2 (7.5) | 19.2 (8.7) | 20.5(7.4) |
| N-telopeptide, nmol bone collagen equivalent/L | 11.1 (3.1) | 13.8 (5.0) | 13.2 (2.8) | 13.1 (2.5) | 14.5 (5.6) | 14.9 (7.5) | 12.7 (3.2) | 12.1 (5.2) |
| Hemoglobin, g/dL | 14.8 (1.0) | 15.0 (0.5) | 14.2 (1.4) | 15.0 (0.8) | 14.8 (0.7) | 14.2 (1.0) | 15.2 (0.9) | 14.9 (1.0) |
| Hematocrit, % | 43.4 (3.0) | 43.4 (1.7) | 41.6 (4.1) | 43.7 (2.0) | 43.3 (1.7) | 41.4 (2.4) | 44.0 (2.4) | 43.6 (3.0) |
| Cholesterol, mg/dL | ||||||||
| Total | 192 (24) | 176 (30) | 176 (37) | 196 (42) | 183 (28) | 177 (40) | 160 (32) | 188 (26) |
| Low-density lipoprotein | 121 (19) | 112 (30) | 108 (34) | 120 (37) | 105 (27) | 104 (36) | 93 (23) | 112 (28) |
| High-density lipoprotein | 51 (10) | 45 (10) | 47 (13) | 56 (18) | 55 (17) | 55 (14) | 51 (20) | 55 (15) |
| Triglycerides, mg/dL | 100 (49) | 98 (32) | 105 (56) | 98 (44) | 115 (58) | 85 (41) | 102 (58) | 102 (37) |
| Sexual function | ||||||||
| International Index of Erectile Function | ||||||||
| Total | 57 (10) | 53 (13) | 55 (10) | 57 (17) | 58 (12) | 55 (12) | 54 (9) | 58 (8) |
| Sexual desire | 7.8 (1.5) | 7.7 (1.5) | 7.5 (1.9) | 7.7 (2.1) | 8.1 (2.0) | 7.3 (1.3) | 7.8 (1.5) | 7.8 (1.3) |
| Erectile function | 23.2 (6.0) | 21.6 (5.7) | 23.5 (5.8) | 23.8 (8.0) | 24.1 (5.7) | 24.4 (6.1) | 23.1 (5.3) | 26.0 (4.7) |
| Orgasmic function | 8.7 (1.4) | 7.9 (2.5) | 8.6 (1.3) | 8.2 (3.0) | 8.3 (1.6) | 8.2 (1.7) | 7.4 (2.2) | 8.3 (1.6) |
| Intercourse satisfaction | 9.5 (3.6) | 8.8 (3.5) | 8.5 (4.1) | 10.2 (3.6) | 10.2 (3.3) | 8.9 (3.2) | 8.8 (3.2) | 9.4 (2.8) |
| Overall satisfaction | 7.6 (1.2) | 6.7 (2.5) | 6.8 (1.3) | 6.9 (2.9) | 7.6 (2.0) | 6.4 (2.0) | 6.3 (2.1) | 6.7 (2.4) |
| Male Sexual Health Questionnaire | ||||||||
| Total | 64 (8) | 64 (13) | 63 (7) | 63 (16) | 65 (9) | 65 (7) | 64 (8) | 66 (5) |
| Ejaculation | 30 (3) | 29 (5) | 31 (2) | 29 (7) | 30 (4) | 30 (2) | 30 (3) | 30 (2) |
| Erection | 12 (3) | 12 (2) | 13 (2) | 12 (3) | 13 (2) | 13 (2) | 12 (2) | 13 (2) |
| Satisfaction | 22 (4) | 23 (6) | 20 (6) | 22 (7) | 23 (5) | 23 (5) | 21 (5) | 22 (4) |
| Sebum forehead score | 3.6 (1.2) | 3.6 (0.9) | 4.2 (1.1) | 4.2 (0.9) | 3.7 (1.2) | 4.2 (0.9) | 3.8 (1.5) | 4.4 (0.7) |
SI conversion factors: To convert free 5α-dihydrotestosterone to pmol/L, multiply by 3.44; hemoglobin to g/L, multiply by 10; high-density, low-density, and total cholesterol to mmol/L, multiply by 0.0259; total 5α-dihydrotestosterone to nmol/L, multiply by 0.0344; total or free testosterone to nmol/L, multiply by 0.0347; triglycerides to mmol/L, multiply by 0.113.
Values are expressed as mean (SD).
Hormone Levels
Levels of total and free testosterone increased with testosterone dose in all groups and did not differ significantly between the groups (eFigure 1 at http://www.jama.com). Among participants who received dutasteride plus testosterone enanthate, the mean testosterone level was 519 ng/dL (95% CI, 378-660 ng/dL) for 50 mg/wk, 895 ng/dL (95% CI, 616-1173 ng/dL) for 125 mg/wk, 1706 ng/dL (95% CI, 13412071 ng/dL) for 300 mg/wk, and 3898 ng/dL (95% CI, 3089-4708 ng/dL) for 600 mg/wk. Among participants who received placebo plus testosterone enanthate, the mean testosterone level was 385 ng/dL (95% CI, 261-508 ng/dL) for 50 mg/wk, 822 ng/dL (95% CI, 658-986 ng/dL) for 125 mg/wk, 1702 ng/dL (95% CI, 1201-2203 ng/dL) for 300 mg/wk, and 3578 ng/dL (95% CI, 2876-4279 ng/dL) for 600 mg/wk. Levels of DHT were higher with higher testosterone doses among participants assigned to placebo, but were uniformly suppressed in all testosterone enanthate dose groups assigned to dutasteride (eFigure 1 at http://www.jama.com). Thus, the study intervention was effective in creating 8 groups that had similar testosterone levels, but which differed in DHT levels. Luteinizing hormone levels were suppressed in the placebo and dutasteride groups.
Fat-Free Mass
Fat-free mass and lean body mass increased in a dose-dependent manner in the placebo and dutasteride groups (FIGURE 2). The changes in fat-free mass were related to testosterone dose and changes in testosterone concentrations in the placebo and dutasteride groups but did not differ between groups; the dose-adjusted mean difference (placebo minus dutasteride) in fat-free mass was 0.50 kg (95% CI, −0.22 to 1.22 kg; P =.18). There was no significant interaction between testosterone dose and randomization to dutasteride or placebo, indicating a lack of evidence that the relationship of testosterone dose to change in fat-free mass differed between the dutasteride and placebo groups. The model-based smoothed regression lines, obtained by generalized additive models, describing the relationship between changes in testosterone concentrations and changes in fat-free mass and lean body mass were similar in the placebo and dutasteride groups. Changes in fat mass were negatively related to testosterone dose and concentrations, but the relationship between change in fat mass and dose did not differ significantly between the placebo and dutasteride groups (P =.41; Figure 2).
Figure 2.
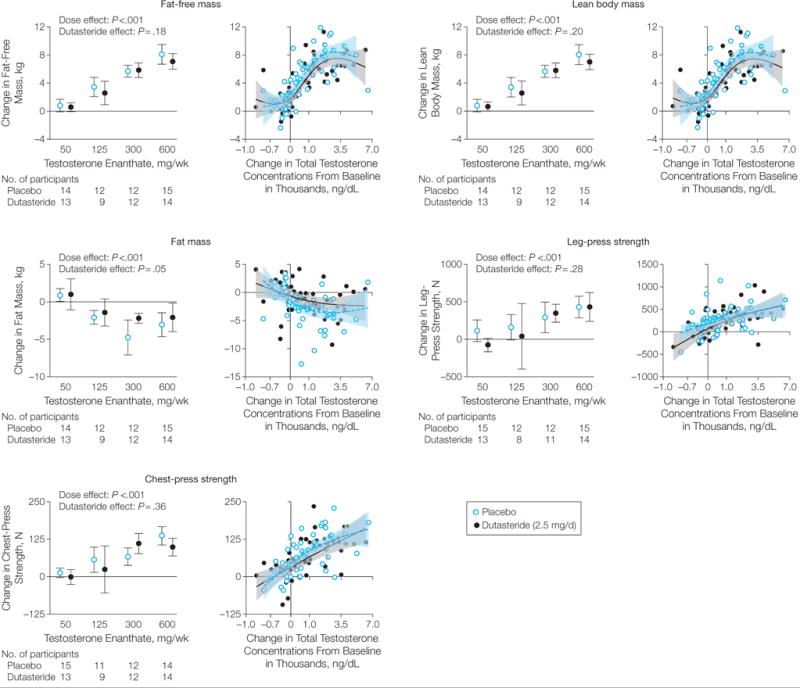
Body Composition and Muscle Strength Measures
In the graphs on the left, data markers indicate means and the error bars indicate 95% confidence intervals. In the graphs on the right (change in testosterone levels), the horizontal axis scales were shifted (offset) by 1000 ng/dL, and a square root transformation was then applied. Semiparametric smoothing was obtained using generalized additive models. Shaded regions indicate 95% confidence intervals.
Muscle Strength
Leg-press and chest-press strength increased dependently by dose in the placebo and dutasteride groups. Increases in leg-press and chest-press strength were greater with larger doses and higher concentrations of testosterone. These relationships did not differ between the placebo and dutasteride groups (Figure 2).
Sexual Function
The International Index of Erectile Function composite scores, the Male Sexual Health Questionnaire composite scores, and the domain scores were not significantly related to either the testosterone dose or concentrations of testosterone while receiving treatment (eFigure 2 at http://www.jama.com). Changes in the International Index of Erectile Function and Male Sexual Health Questionnaire composite scores and erectile, orgasmic, ejaculatory, intercourse, or overall satisfaction scores did not differ significantly between the dutasteride and placebo groups.
Prostate Volumes and PSA Level
Changes in prostate volume and PSA level were not significantly related to either testosterone dose or concentration, and did not differ significantly between the placebo and dutasteride groups (eFigure 2). The dose-adjusted mean difference in change in PSA level between participants assigned to placebo and participants assigned to dutasteride was 0.13 ng/mL (95% CI, −0.05 to 0.31 ng/mL; P = .15) and the corresponding difference in changes in prostate volume was 0.91 cm3 (−0.44 to 2.25 cm3; P=.19).
Sebum Production and Acne
Sebum production in the forehead region, but not on the nose or back, was related to testosterone dose, and did not differ between the placebo and dutasteride groups (eFigure 2). Twenty-five men in the dutasteride groups and 25 in the placebo groups experienced acne (eTable 1 at http://www.jama.com). The acne scores did not differ between groups.
Laboratory Tests
Levels of hemoglobin and hematocrit increased dose dependently in the placebo and dutasteride groups; changes in levels of hemoglobin and hematocrit were significantly related to changes in testosterone concentrations but did not differ significantly between the groups (eTable 2). Changes in total cholesterol and high-density lipoprotein cholesterol were negatively related to testosterone dose but did not differ significantly between the groups. Serum NTx (collagen-type I N-telopeptides) and osteocalcin levels did not change in the placebo and dutasteride groups.
Adverse Events
The overall frequency of adverse events, including the frequency of sexual dysfunction, acne, hot flashes, and breast tenderness was similar in the placebo and dutasteride groups (eTable 1 at http://www.jama.com).
Sensitivity Analyses
Sensitivity analyses using multiple imputation confirmed the findings of the main analyses described above, again supporting the significant relationship between testosterone dose and changes in fat-free mass, lean body mass, legpress and chest-press strength, fat mass, and levels of hemoglobin and hematocrit but there were no significant differences in the change in these outcomes between the dutasteride and placebo groups (eTable 3 and eFigures 3-5). Changes in sexual function scores, prostate volume, and PSA level in relation to testosterone dose also did not differ between the dutasteride and placebo groups using multiple imputation (eFigure 5). Analyses of rank-transformed outcomes likewise revealed similar results.
COMMENT
Several models have been invoked to explain the role of DHT in men. A widely held view is that conversion to DHT is obligatory for mediating testosterone’s effects in some tissues with high 5α-reductase activity, such as prostate and skin, but not in others, such as skeletal muscle and bone. It is possible that conversion of testosterone to DHT is not obligatory, but that it amplifies the effects of testosterone in tissues with high 5α-reductase activity such as the prostate and skin, but not in tissues with low 5α-reductase activity such as skeletal muscle and bone. A third possibility is that 5α-reduction of testosterone is not obligatory for mediating its effects in any tissue in men, but that testosterone and DHT can both exert androgenic effects in all androgen-sensitive tissues, and their relative effects in any tissue are contingent upon their relative concentrations and potency.
Our data, when viewed together with published literature on the effects of 5α-reductase inhibitors in patients with benign prostatic hyperplasia, are the most consistent with the second model in which DHT amplifies the effects of testosterone in tissues with high 5α-reductase activity. The changes in lean body mass, fat mass, muscle strength, several domains of sexual function, hematocrit level, and levels of total and high-density lipoprotein cholesterol in response to graded doses of testosterone enanthate in men assigned to dutasteride were not significantly different from those assigned to placebo. Even prostate volume, PSA level, sebum production, and acne scores (markers of androgenic activity in tissues with high 5α-reductase activity) were not affected by dutasteride administration in the range of testosterone concentrations achieved in these men.
Furthermore, the relationship of testosterone concentrations with these outcomes did not differ between the dutasteride and placebo groups despite substantial differences in DHT concentrations. Thus, the inhibition of testosterone’s conversion to DHT by dutasteride had no significant effect on the ability of testosterone to exert its effects on muscle mass and strength, sexual function, erythropoiesis, plasma lipid levels, prostate volume, and sebum production. Instead, over the range of testosterone concentrations that were achieved (and which spanned the entire physiological male range and extended well into the subphysiological and supraphysiological range for men), testosterone was able to subserve all androgen-dependent functions that were studied herein, including maintenance of prostate volumes, PSA levels, and sebum production.
The net androgen effect in any tissue can be viewed as a function of the prevalent intratissue testosterone and DHT concentrations and their relative androgenic potencies (eFigure 6). In tissues with low steroid 5α-reductase activity such as muscle and bone, intratissue DHT concentration is very low relative to testosterone and can be discounted, and the androgen effect attributed largely to testosterone. In tissues with high 5α-reuctase activity such as the prostate, intratissue DHT concentrations are higher than those of testosterone.22,23,36,37 Administration of 0.5 mg/d of dutasteride suppresses nearly completely intraprostatic DHT formation (approximately 94%)22,23; therefore, we assume that intraprostatic DHT concentrations in men who received 2.5 mg/d of dutasteride were suppressed to very low levels. Even under these conditions of suppressed circulating and intraprostatic DHT concentrations induced by a high-dose dutasteride regimen, prostate volumes and PSA levels were maintained by testosterone doses administered in this trial.
How can we reconcile these findings with those from trials in which dutasteride has been reported to decrease prostate volume and PSA in men with benign prostatic hyperplasia?10,11 The suppression of prostate volume by dutasteride in older men with benign prostatic hyperplasia, when viewed together with the findings from our trial, suggests that DHT formation is important for amplifying testosterone’s effect in this tissue at concentrations lower than those achieved in our trial. Indeed, our model predicts that administration of a 5α-reductase inhibitor in men who have low testosterone levels below the activation threshold of the prostate should attenuate androgen effects in this tissue. This argument is supported by the finding that in older men with benign prostatic hyperplasia, the largest reduction in prostate volume with dutasteride is observed in men with low serum testosterone levels.38 However, as circulating testosterone concentrations are increased from physiological to supraphysiological, testosterone alone can maintain prostate volumes even when 5α-reductase activity is suppressed effectively.
Why then did the steroid 5α-reductase system evolve for androgens? Forty-six XY males with steroid 5α-reductase deficiency exhibited ambiguous or female external genitalia at birth and poor prostate development, but underwent normal muscle and bone development during pubertal transition.6,7,39 The phenotype of these patients suggests that steroid 5α-reductase plays an essential role in the development of prostate and phallus by providing local amplification of an androgenic signal without systemic hyperandrogenemia during critical periods of sexual differentiation, illustrating nature’s extraordinary ingenuity in creating mechanisms for tissue-selective amplification during development. We speculate that in adult men, in whom this tissue-specific amplification is not essential because the circulating testosterone concentrations are substantially higher than those in the fetus, testosterone and DHT can interchangeably subserve many androgenic functions. When circulating testosterone concentrations are low, intraprostatic DHT formation may become important in maintaining prostate growth, thus buffering the effects of decreasing testosterone levels, which has been suggested by Marks et al.36
Our data are consistent with studies that have reported no effects of 5α-reductase inhibitors on muscle or bone mass.40–42 Inferences from these trials are limited by the fact that administration of 5α-reductase inhibitors increases testosterone levels,15–17 rendering it difficult to ascribe the outcomes to differences in DHT levels alone. In our trial, inhibition of endogenous testosterone by administration of a gonadotropin-releasing hormone agonist eliminated this problem. Additionally, the high-dose dutasteride regimen effectively inhibited both steroid 5α-reductase isoenzymes.
Our study had greater than 90% power to detect a 25% difference in outcomes between the placebo and dutasteride groups. We observed no meaningful numerical difference between the placebo and dutasteride groups, especially for the primary outcome, and the relationship between testosterone concentrations and outcomes did not differ between study groups despite substantially different DHT concentrations. Thus, these dataprovide evidence in favor of no difference. We did not measure intratissue DHT, but assume based on published data22,23 that the high dose of dutasteride effectively suppressed intraprostatic DHT. Because semen analyses were not performed, we cannot exclude an essential role for DHT in spermatogenesis.
The dutasteride and placebo groups did not differ in any domain of sexual function. In a rat model, testosterone’s effect on erectile response to electrical field stimulation was blocked by finasteride.13 Healthy men treated with dutasteride experience modestly lower erectile function scores than those treated with placebo.42 Another study found no significant effects of finasteride on sleep-related erections.43 Sexual dysfunction has been reported in some trials of 5α-reductase inhibitors but not in others.14
Our model predicts that there may be an interaction between testosterone concentrations and administration of 5α-reductase inhibitors such that in men with low testosterone, inhibition of testosterone’s conversion to DHT may impair erectile function. Consistent with this model, men with benign prostatic hyperplasia who were receiving dutasteride and who had low testosterone concentrations were more likely to report sexual dysfunction than those with normal testosterone concentrations.38 Although young men in our trial and in a previous trial42 who received dutasteride reported satisfactory sexual intercourse, older men with low testosterone concentrations (the likely recipients of these drugs) may be at risk for developing erectile dysfunction when treated with 5α-reductase inhibitors.
Although head-to-head comparisons of testosterone and DHT have not been conducted, randomized trials of DHT gel in older men have reported changes in lean body mass and in the levels of hematocrit and lipids similar to those observed in testosterone trials.44–46 Similarly, 7α-methyl 19-nortestosterone, which does not undergo 5α-reduction, maintains sexual function in hypogonadal men.47 These findings support the proposal that testosterone and DHT can interchangeably subserve androgen-dependent functions investigated in this trial.
The finding that 5α-reduction of testosterone to DHT is not obligatory for mediating its effects on outcomes that were studied in this trial has implications for therapeutic applications of androgens and 5α-reductase inhibitors. These findings bode well for the safety of 5α-reductase inhibitors with respect to their effects on muscle. Combined administration of testosterone plus a 5α-reductase inhibitor and the use of SARMs that do not undergo 5α-reduction have been proposed as strategies for mitigating concerns about androgen’s effects on the prostate.48 While our data suggest that SARMs that do not undergo 5α-reduction can exert anabolic effects on the muscle, they also indicate that such a strategy may not necessarily be effective in sparing the prostate, depending upon androgen dose. The prostate safety of such SARMs will need careful scrutiny. Our data also predict that efficacy of 5α-reductase inhibitors may be limited in men with normal or high testosterone concentrations; therefore, measurement of testosterone levels might be useful in identifying men less likely to respond to 5α-reductase inhibitors.
Supplementary Material
Acknowledgments
Dr S. Bhasin reported board membership for Novartis, working as a consultant to GlaxoSmithKline, having grants pending with Solvay Pharmaceuticals, Merck & Co, and Ligand Pharmaceuticals Inc, receiving reimbursement for travel expenses from GlaxoSmithKline, Novartis, Lilly and Co, and Ligand Pharmaceuticals, and receiving compensation for serving as the chairfor 2 Endocrine Society expert panels. No other author reported disclosures.
Funding/Support: This study was supported by grant 1RO1HD043348 from the National Institute of Child Health and Human Development. Additional support was provided by Boston University Clinical and Translational Science Institute grant 1UL1RR025771, by the Boston Claude D. Pepper Older Americans Independence Center, and by grant 5P30AG031679 from the National Institute on Aging. GlaxoSmithKline Inc provided dutasteride and placebo and ENDO Pharmaceuticals provided testosterone enanthate.
Role of the Sponsors: Thesponsors had no role in the design and conductof thestudy; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Independent Statistical Analyses: Dr Travison performed the statistical analyses of the data with the assistance of Ms Davda.
Footnotes
Author Contributions: Dr Travison had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: S. Bhasin, Storer, Basaria.
Acquisition of data: S. Bhasin, Storer, Lakshman, Mazer, Knapp, Hanka, Mohammed, Daou, Miciek, Ulloor, Zhang, Brooks, Orwoll, Hede-Brierley, Eder, Elmi, G. Bhasin, Collins, Basaria.
Analysis and interpretation of data: S. Bhasin, Travison, Lakshman, Kaushik, Ngyuen, Davda, Jara, Aakil, Anderson, Hanka, Mohammed, Singh, Basaria.
Drafting of the manuscript: S. Bhasin, Travison, Lakshman, Kaushik, Anderson, Miciek, Ulloor, Brooks, Orwoll, Elmi, Basaria.
Critical revision of the manuscript for important intellectual content: S. Bhasin, Travison, Storer, Mazer, Ngyuen, Davda, Jara, Aakil, Knapp, Hanka, Mohammed, Daou, Zhang, Hede-Brierley, G. Bhasin, Collins, Basaria.
Statistical analysis: S. Bhasin, Travison, Lakshman, Kaushik, Ngyuen, Davda.
Obtained funding: S. Bhasin.
Administrative, technical, or material support: S. Bhasin, Storer, Lakshman, Jara, Anderson, Knapp, Hanka, Mohammed, Daou, Ulloor, Zhang, Hede-Brierley, Elmi, G. Bhasin, Collins, Singh, Basaria.
Study supervision: S. Bhasin, Storer, Eder, Collins, Basaria.
Conflict of Interest Disclosures: The authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Data and Safety Monitoring Board: Steven Grinspoon, MD, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts (chair), and Peter J. Snyder, MD, University of Pennsylvania, Philadelphia.
Online-Only Material: eTables 1 through 3 and eFigures 1 through 6 are available at http://www.jama.com.
Additional Contributions: We thank the staff of the General Clinical Research Unit of Boston University’s Clinical and Translational Science Institute for their help with these studies, and thestudy participants for their commitment and generosity.
References
- 1.Wilson JD, Griffin JE, Russell DW. Steroid 5 alpha-reductase 2 deficiency. Endocr Rev. 1993;14(5):577–593. doi: 10.1210/edrv-14-5-577. [DOI] [PubMed] [Google Scholar]
- 2.Jenkins EP, Andersson S, Imperato-McGinley J, Wilson JD, Russell DW. Genetic and pharmacological evidence for more than one human steroid 5 alpha-reductase. J Clin Invest. 1992;89(1):293–300. doi: 10.1172/JCI115574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersson S, Russell DW. Structural and biochemical properties of cloned and expressed human and rat steroid 5 alpha-reductases. Proc Natl Acad Sci U S A. 1990;87(10):3640–3644. doi: 10.1073/pnas.87.10.3640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw G, Fenelon J, Sichlau M, et al. Role of the alternate pathway of dihydrotestosterone formation in virilization of the Wolffian ducts of the tammar wallaby, Macropus eugenii. Endocrinology. 2006;147(5):2368–2373. doi: 10.1210/en.2005-1251. [DOI] [PubMed] [Google Scholar]
- 5.Wilson JD, Renfree MB, Auchus RJ, et al. Formation of 5 alpha-reduced androgens in the testes and urogenital tract of the grey short-tailed opossum, Monodelphis domestica. Reprod Fertil Dev. 2009;21(5):649–654. doi: 10.1071/RD08253. [DOI] [PubMed] [Google Scholar]
- 6.Imperato-McGinley J, Guerrero L, Gautier T, Peterson RE. Steroid 5 alpha-reductase deficiency in man. Science. 1974;186(4170):1213–1215. doi: 10.1126/science.186.4170.1213. [DOI] [PubMed] [Google Scholar]
- 7.Walsh PC, Madden JD, Harrod MJ, et al. Familial incomplete male pseudohermaphroditism, type 2. N Engl J Med. 1974;291(18):944–949. doi: 10.1056/NEJM197410312911806. [DOI] [PubMed] [Google Scholar]
- 8.Imperato-McGinley J, Binienda Z, Arthur A, et al. The development of a male pseudohermaphroditic rat using an inhibitor of the enzyme 5 alpha-reductase. Endocrinology. 1985;116(2):807–812. doi: 10.1210/endo-116-2-807. [DOI] [PubMed] [Google Scholar]
- 9.Mahendroo MS, Cala KM, Hess DL, Russell DW. Unexpected virilization in male mice lacking steroid 5 alpha-reductase enzymes. Endocrinology. 2001;142(11):4652–4662. doi: 10.1210/endo.142.11.8510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gormley GJ, Stoner E, Bruskewitz RC, et al. The Finasteride Study Group The effect of finasteride in men with benign prostatic hyperplasia. N Engl J Med. 1992;327(17):1185–1191. doi: 10.1056/NEJM199210223271701. [DOI] [PubMed] [Google Scholar]
- 11.Roehrborn CG, Boyle P, Nickel JC, et al. ARIA3001 ARIA3002 and ARIA3003 Study Investigators Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology. 2002;60(3):434–441. doi: 10.1016/s0090-4295(02)01905-2. [DOI] [PubMed] [Google Scholar]
- 12.Diani AR, Mulholland MJ, Shull KL, et al. Hair growth effects of oral administration of finasteride, a steroid 5 alpha-reductase inhibitor, alone and in combination with topical minoxidil in the balding stumptail macaque. J Clin Endocrinol Metab. 1992;74(2):345–350. doi: 10.1210/jcem.74.2.1309834. [DOI] [PubMed] [Google Scholar]
- 13.Lugg JA, Rajfer J, González-Cadavid NF. Dihydrotestosterone is the active androgen in the maintenance of nitric oxide-mediated penile erection in the rat. Endocrinology. 1995;136(4):1495–1501. doi: 10.1210/endo.136.4.7534702. [DOI] [PubMed] [Google Scholar]
- 14.Canguven O, Burnett AL. The effect of 5 alpha-reductase inhibitors on erectile function. J Androl. 2008;29(5):514–523. doi: 10.2164/jandrol.108.005025. [DOI] [PubMed] [Google Scholar]
- 15.Amory JK, Watts NB, Easley KA, et al. Exogenous testosterone or testosterone with finasteride increases bone mineral density in older men with low serum testosterone. J Clin Endocrinol Metab. 2004;89(2):503–510. doi: 10.1210/jc.2003-031110. [DOI] [PubMed] [Google Scholar]
- 16.Page ST, Amory JK, Bowman FD, et al. Exogenous testosterone (T) alone or with finasteride increases physical performance, grip strength, and lean body mass in older men with low serum T. J Clin Endocrinol Metab. 2005;90(3):1502–1510. doi: 10.1210/jc.2004-1933. [DOI] [PubMed] [Google Scholar]
- 17.Wilton L, Pearce G, Edet E, et al. The safety of finasteride used in benign prostatic hypertrophy. Br J Urol. 1996;78(3):379–384. doi: 10.1046/j.1464-410x.1996.00091.x. [DOI] [PubMed] [Google Scholar]
- 18.Bhasin S, Woodhouse L, Casaburi R, et al. Testosterone dose-response relationships in healthy young men. Am J Physiol Endocrinol Metab. 2001;281(6):E1172–E1181. doi: 10.1152/ajpendo.2001.281.6.E1172. [DOI] [PubMed] [Google Scholar]
- 19.Bhasin S, Woodhouse L, Casaburi R, et al. Older men are as responsive as young men to the anabolic effects of graded doses of testosterone on the skeletal muscle. J Clin Endocrinol Metab. 2005;90(2):678–688. doi: 10.1210/jc.2004-1184. [DOI] [PubMed] [Google Scholar]
- 20.Clark RV, Hermann DJ, Cunningham GR, et al. Marked suppression of dihydrotestosterone in men with benign prostatic hyperplasia by dutasteride, a dual 5 alpha-reductase inhibitor. J Clin Endocrinol Metab. 2004;89(5):2179–2184. doi: 10.1210/jc.2003-030330. [DOI] [PubMed] [Google Scholar]
- 21.Andriole GL, Bostwick DG, Brawley OW, et al. REDUCE Study Group Effect of dutasteride on the risk of prostate cancer. N Engl J Med. 2010;362(13):1192–1202. doi: 10.1056/NEJMoa0908127. [DOI] [PubMed] [Google Scholar]
- 22.Rittmaster R, Hahn RG, Ray P, et al. Effect of dutasteride on intraprostatic androgen levels in men with benign prostatic hyperplasia or prostate cancer. Urology. 2008;72(4):808–812. doi: 10.1016/j.urology.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 23.Wurzel R, Ray P, Major-Walker K, et al. The effect of dutasteride on intraprostatic dihydrotestosterone concentrations in men with benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 2007;10(2):149–154. doi: 10.1038/sj.pcan.4500931. [DOI] [PubMed] [Google Scholar]
- 24.Kim J, Wang Z, Heymsfield SB, et al. Total-body skeletal muscle mass. Am J Clin Nutr. 2002;76(2):378–383. doi: 10.1093/ajcn/76.2.378. [DOI] [PubMed] [Google Scholar]
- 25.Storer TW, Magliano L, Woodhouse L, et al. Testosterone dose-dependently increases maximal voluntary strength and leg power, but does not affect fatigability or specific tension. J Clin Endocrinol Metab. 2003;88(4):1478–1485. doi: 10.1210/jc.2002-021231. [DOI] [PubMed] [Google Scholar]
- 26.Basaria S, Coviello AD, Travison TG, et al. Adverse events associated with testosterone administration. N Engl J Med. 2010;363(2):109–122. doi: 10.1056/NEJMoa1000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosen RC, Riley A, Wagner G, et al. The International Index of Erectile Function (IIEF) Urology. 1997;49(6):822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 28.Rosen RC, Catania J, Pollack L, et al. Male Sexual Health Questionnaire (MSHQ) Urology. 2004;64(4):777–782. doi: 10.1016/j.urology.2004.04.056. [DOI] [PubMed] [Google Scholar]
- 29.Farraher SW, Jara H, Chang KJ, et al. Liver and spleen volumetry with quantitative MR imaging and dualspace clustering segmentation. Radiology. 2005;237(1):322–328. doi: 10.1148/radiol.2371041416. [DOI] [PubMed] [Google Scholar]
- 30.Pierard GE, Pierard-Franchimont C. The sebutape technique for monitoring androgen dependent disorders. Eur J Med. 1992;1(2):109–112. [PubMed] [Google Scholar]
- 31.Palatsi R, Hirvensalo E, Liukko P, et al. Serum total and unbound testosterone and sex hormone binding globulin (SHBG) in female acne patients treated with two different oral contraceptives. Acta Derm Venereol. 1984;64(6):517–523. [PubMed] [Google Scholar]
- 32.Bhasin S, Pencina M, Jasuja GK, et al. Reference ranges for testosterone in men generated using liquid chromatography tandem mass spectrometry in a community-based sample of healthy nonobese young men in the Framingham Heart Study and applied to three geographically distinct cohorts. J Clin Endocrinol Metab. 2011;96(8):2430–2439. doi: 10.1210/jc.2010-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shiraishi S, Lee PWN, Leung A, et al. Simultaneous measurement of serum testosterone and dihydrotestosterone by liquid chromatography-tandem mass spectrometry. Clin Chem. 2008;54(11):1855–1863. doi: 10.1373/clinchem.2008.103846. [DOI] [PubMed] [Google Scholar]
- 34.Mazer NA. A novel spreadsheet method for calculating the free serum concentrations of testosterone, dihydrotestosterone, estradiol, estrone and cortisol. Steroids. 2009;74(6):512–519. doi: 10.1016/j.steroids.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 35.Bhasin S, Storer TW, Berman N, et al. The effects of supraphysiologic doses of testosterone on muscle size and strength in normal men. N Engl J Med. 1996;335(1):1–7. doi: 10.1056/NEJM199607043350101. [DOI] [PubMed] [Google Scholar]
- 36.Marks LS, Mazer NA, Mostaghel E, et al. Effect of testosterone replacement therapy on prostate tissue in men with late-onset hypogonadism: a randomized controlled trial. JAMA. 2006;296(19):2351–2361. doi: 10.1001/jama.296.19.2351. [DOI] [PubMed] [Google Scholar]
- 37.Bartsch W, Krieg M, Voigt KD. Quantification of endogenous testosterone, 5 alpha-dihydrotestosterone and 5 alpha-androstane-3 alpha, 17 beta-diol in subcellular fractions of the prostate, bulbocavernosus/levator ani muscle, skeletal muscle and heart muscle of the rat. J Steroid Biochem. 1980;13(3):259–264. doi: 10.1016/0022-4731(80)90003-5. [DOI] [PubMed] [Google Scholar]
- 38.Marberger M, Roehrborn CG, Marks LS, et al. Relationship among serum testosterone, sexual function, and response to treatment in men receiving dutasteride for benign prostatic hyperplasia. J Clin Endocrinol Metab. 2006;91(4):1323–1328. doi: 10.1210/jc.2005-1947. [DOI] [PubMed] [Google Scholar]
- 39.Sobel V, Schwartz B, Zhu YS, et al. Bone mineral density in the complete androgen insensitivity and 5 alpha-reductase-2 deficiency syndromes. J Clin Endocrinol Metab. 2006;91(8):3017–3023. doi: 10.1210/jc.2005-2809. [DOI] [PubMed] [Google Scholar]
- 40.Borst SE, Conover CF, Carter CS, et al. Anabolic effects of testosterone are preserved during inhibition of 5alpha-reductase. Am J Physiol Endocrinol Metab. 2007;293(2):E507–E514. doi: 10.1152/ajpendo.00130.2007. [DOI] [PubMed] [Google Scholar]
- 41.Matsumoto AM, Tenover L, McClung M, et al. Pless Study Group The long-term effect of specific type II 5 alpha-reductase inhibition with finasteride on bone mineral density in men. J Urol. 2002;167(5):2105–2108. [PubMed] [Google Scholar]
- 42.Amory JK, Anawalt BD, Matsumoto AM, et al. The effect of 5 alpha-reductase inhibition with dutasteride and finasteride on bone mineral density, serum lipoproteins, hemoglobin, prostate specific antigen and sexual function in healthy young men. J Urol. 2008;179(6):2333–2338. doi: 10.1016/j.juro.2008.01.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cunningham GR, Hirshkowitz M. Inhibition of steroid 5 alpha-reductase with finasteride. J Clin Endocrinol Metab. 1995;80(6):1934–1940. doi: 10.1210/jcem.80.6.7775644. [DOI] [PubMed] [Google Scholar]
- 44.Ly LP, Jimenez M, Zhuang TN, et al. A doubleblind, placebo-controlled, randomized clinical trial of transdermal dihydrotestosterone gel on muscular strength, mobility, and quality of life in older men with partial androgen deficiency. J Clin Endocrinol Metab. 2001;86(9):4078–4088. doi: 10.1210/jcem.86.9.7821. [DOI] [PubMed] [Google Scholar]
- 45.Idan A, Griffiths KA, Harwood DT, et al. Longterm effects of dihydrotestosterone treatment on prostate growth in healthy, middle-aged men without prostate disease. Ann Intern Med. 2010;153(10):621–632. doi: 10.7326/0003-4819-153-10-201011160-00004. [DOI] [PubMed] [Google Scholar]
- 46.Kunelius P, Lukkarinen O, Hannuksela ML, et al. The effects of transdermal dihydrotestosterone in the aging male. J Clin Endocrinol Metab. 2002;87(4):1467–1472. doi: 10.1210/jcem.87.4.8138. [DOI] [PubMed] [Google Scholar]
- 47.Anderson RA, Martin CW, Kung AW, et al. 7 Alpha-methyl-19-nortestosterone maintains sexual behavior and mood in hypogonadal men. J Clin Endocrinol Metab. 1999;84(10):3556–3562. doi: 10.1210/jcem.84.10.6028. [DOI] [PubMed] [Google Scholar]
- 48.Bhasin S, Calof OM, Storer TW, et al. Drug insight: testosterone and selective androgen receptor modulators as anabolic therapiesfor chronic illness and aging. Nat Clin Pract Endocrinol Metab. 2006;2(3):146–159. doi: 10.1038/ncpendmet0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


