Abstract
Recognizing the high prevalence of human immunodeficiency virus (HIV)-positive women and girls who are either at risk for or suffer from intimate partner violence (IPV) and the overlapping challenges posed by both public health issues, the White House established an Interagency Federal Working Group to address the intersection of both public health issues in 2012. We conducted this systematic review in response to the Working Group’s charge to identify and describe interventions that address both IPV and HIV among women. We identified 14 studies that met our inclusion criteria, including seven studies (nine unique intervention arms) that significantly affected at least one outcome related to IPV and HIV. In this article, we examine the characteristics of these studies including core components, intervention populations, and effectiveness data. We highlight opportunities to improve the effectiveness of existing interventions, guide future research about IPV and HIV, and inform prevention programmatic delivery. This knowledge will improve the lives of populations at risk, reduce gender-related health disparities, and ultimately reduce the societal burden of both public health issues.
Keywords: HIV, Intimate partner violence, Women, Prevention, Systematic review
Introduction
Women who have experienced intimate partner violence (IPV) are at increased risk of getting and transmitting human immunodeficiency virus (HIV). Likewise, women who are HIV-positive are at increased risk for experiencing IPV. The coexisting and mutually reinforcing relationship between HIV and IPV that makes each one worse than it would be without the other is referred to as “syndemic” [1]—HIV exacerbates the risk of IPV and IPV compounds the risk of HIV in a woman [1, 2]. This syndemic is particularly devastating to women as they are affected by biological, psychological, and behavioral conditions that place them at disproportionate risk for IPV and HIV [2–5]. This negative interaction poses a devastating threat to the quality of life of women and results in a large overall burden to society [2, 5, 6]. It is important to address these issues separately, but the frequent co-occurrence of HIV and IPV creates a need to address both issues simultaneously through prevention programs. The goal of this systematic review is to synthesize the published literature, including core components, regarding primary prevention interventions that address both IPV and HIV among women (“dual-focused interventions”) and identify information to guide future research, program development, and technical assistance efforts.
In a 2013 study of more than 80 countries, the World Health Organization (WHO) estimated the lifetime IPV prevalence among ever-partnered women was highest in low- to middle-income regions, like Southeast Asia (37.7%) and Africa (36.6%) and lowest in the high income regions, such as Europe (25.4%) and the Western Pacific (24.6%) [7]. The most recent report (2010–2012) from the National Intimate Partner and Sexual Violence Survey (NISVS) estimated that 37.3% (approximately 45 million) of women in the US have experienced any contact sexual violence, physical violence and/or stalking victimization by an intimate partner in their lifetime, and 6.6% (almost 8 million) experienced these forms of violence in the year prior to the survey [8].
HIV is also a major public health concern. Worldwide, there are approximately 36.7 million people living with HIV, and 17.8 million are women, constituting 51% of all adults living with HIV [9, 10]. The research shows that low-and middle-income countries have the highest IPV and HIV prevalence rates [7, 11] and that most of those living with HIV reside in sub-Saharan Africa (70%) [11]. In the US, there are an estimated 1.1 million adults and adolescents living with HIV, and women account for 23% of them according to the Centers for Disease Control and Prevention (CDC) [11]. Of these women, 12% are undiagnosed [11].
IPV/HIV Co-occurrence Among Women
The association between IPV and HIV has been studied broadly both in the US and international settings. Gender inequalities and social norms have been shown to be key drivers of both IPV and HIV, and they mediate the relation between abuse and HIV transmission as they give power to men over women and reduce women’s ability to negotiate health threats [12, 13]. Research shows that women who experience IPV are more likely to report engaging in risky sexual behaviors such as condomless sex and having multiple sex partners; contracting a sexually transmitted infection (STI); having an unwanted pregnancy or unsafe abortion; and infertility [3, 4, 14–17]. A woman may also be at increased risk for HIV if she is unable to engage in safer sex behaviors (i.e., negotiate condom use), have control over her sexuality, or is forced to have sex with an HIV-positive partner [3, 4, 18, 19]. Data show that women who report a history of IPV in their lifetimes are two times as likely to have gotten an HIV test as women who do not report a history of IPV, which suggests increased perceived risk of contracting HIV among women who have experienced IPV [20]. In addition, Maher et al. found no relationship between refusal to be tested for HIV and having experienced IPV though there is little research on this association [21]. Since experiencing IPV and fears of partner notification have not shown to be reasons for declining an HIV test, there may be opportunities for appropriate referrals from providers (i.e., IPV prevention service providers) among this at-risk population [21].
Research shows that among HIV-positive women in the US, 55% have experienced IPV at some point in their lifetime [22]. This rate is much higher than the overall national rate among women (37.2%) reported in NISVS, which is a nationally representative sample of women 18 years and older in the US [8]. Several studies show that women who are HIV-positive may experience IPV following disclosure of their HIV-positive serostatus to their partners [23–25]. Furthermore, IPV can occur more frequently and be more severe among HIV-positive women compared to those who are not HIV-positive due to increased susceptibility to risk factors for IPV, especially upon initial disclosure of HIV-positive status [26].
Prevention Efforts
Primary prevention of IPV has largely focused on preventing first-time perpetration [27]. Although both men and women report experiencing IPV, the majority of prevention efforts have focused on male-perpetrated IPV against women [27]. While prevention strategies that target perpetrators are critical for primary prevention of IPV, interventions are also needed to understand and effectively address risk and protective factors associated with intimate partner violence victimization. A number of approaches that may be promising for preventing IPV victimization among women tend to focus on empowering and supporting girls and women [28]. These approaches include policies and programs that seek to improve economic security for girls and strengthen educational, employment, and community engagement opportunities, e.g., microfinance to offer savings and loans opportunities to raise the financial status of women and their families [29]. However, microfinance has only been found to be effective through randomized controlled trials outside the US for preventing IPV in women. The Jewellery Education for Women Empowering Their Lives (JEWEL) study, a pilot study in Baltimore, Maryland, showed significant reductions in receiving drugs or money for sex, the median number of sex trade partners per month, the amount of money spent on drugs daily, and daily crack use among women in the study. However, it did not include a comparison group [30]. In addition, while IPV prevention interventions have concentrated on primary prevention, or preventing the first experience of IPV, IPV victimization has also been addressed through secondary and tertiary interventions that mitigate the adverse consequences associated with IPV victimization and prevent future occurrences across diverse populations [12, 27]. These interventions which have been shown to lessen harms for women who have experienced IPV include victim-centered services (i.e., domestic violence shelters) and evidence-based psychological interventions (e.g., trauma-focused cognitive behavioral therapy) conducted by clinicians to help address depression, fear, trauma, and anxiety associated with IPV [31]. These interventions have been shown to reduce the short- and long-term negative effects of victimization.
Compared to IPV, primary prevention efforts for HIV have a more established evidence base, many of which are behavioral interventions that aim to reduce risk related to sexual behavior and drug use. CDC’s HIV Prevention Research Synthesis (PRS) Project utilizes a set of criteria to systematically identify evidence-based behavioral interventions (EBIs) for HIV prevention [32]. These interventions are designated as ‘best-evidence’ or ‘good-evidence’ based on a specific set of criteria [33]. The EBIs target a wide range of populations in the US and are customized to their individualized needs (i.e., low-income, Hispanic/Latina women, black/African American women, sex workers, recently incarcerated, drug users/women in drug treatment, child sexual abuse survivors, and high risk heterosexual women and their social network). They address multiple risk and protective factors such as life stability and employment, relationship communication, pregnancy, psychosocial risk factors, adolescent truancy, and IPV [32].
Core Components
As a result of the high co-occurrence and the shared risk factors of IPV and HIV, we identified a need to assess the core components of dual-focused interventions and determine the efficacy of each strategy [34–37]. To determine the core components of IPV and HIV interventions, we performed a content analysis of selected sentinel studies looking for similarities and differences. We had multiple reviewers analyze each study and then synthesized our lists of components. The authors identified and focused on 23 intervention core components after reviewing the literature (Table 1). This list of core components would form the basis of our subsequent reviews. Our analysis revealed that IPV prevention strategies consistently include common intervention components, such as an increase in awareness and knowledge regarding: assessing danger, effects of trauma, empowerment, power and control, safety planning skills, and social support (Table 1) [38–40]. Among the HIV field, we found that the strong evidence base in HIV prevention indicates more specific intervention components that are essential in positive behavior change. Other core elements for women may include: attitude (e.g., towards safe sex, condom use); correct condom use (skills); culturally/linguistically appropriate materials and information; decision-making (skills); empowerment (e.g., knowing a woman’s sexual rights); gender norms/roles or masculinity/femininity; goal setting; knowledge/information; motivation/intention; negotiation about safer sex/condom use (skills); normative influence (i.e., changing peer/social norms); other skills (e.g., communication, disclosure, stress); personal risk/vulnerability; personalized risk reduction plan; protecting family/significant others; self-efficacy; social support; and women’s sexuality (having a positive view).
Table 1.
Core components identify through the IPV and HIV Literature
| Prevention focus | Core component |
|---|---|
| IPV prevention | Assessing danger Awareness Effects of trauma (e.g., PTSD, anxiety) Power and control Safety planning (skills) |
| HIV prevention | Attitude (e.g., towards safe sex, condom use) Correct condom use (skills) Culturally/linguistically appropriate materials and information Decision-making (skills) Gender norms/roles or masculinity/femininity Goal setting Motivation/intention Negotiation about safer sex/condom use (skills) Normative influence (e.g., changing peer/social norms) Other skills (e.g., communication, disclosure, stress) Personal risk/vulnerability Personalized risk reduction plan Protecting family/significant others Self-efficacy Women’s sexuality (having a positive view) |
| IPV and HIV Prevention | Knowledge/information Empowerment (e.g., knowing a woman’s sexual rights) Social support |
As previously stated, research has clearly shown the co-occurrence between IPV and HIV and the impact on women. Due to the frequency of co-occurrence, enacting prevention efforts for IPV and HIV simultaneously will provide the most public health value. Understanding the core components of IPV/HIV prevention efforts will inform the development, implementation, and evaluation of future research, program implementation, and technical assistance efforts.
A Federal Mandate to Address Violence against Women and HIV Prevention and Care
Acknowledging the syndemic of IPV and HIV in the lives of women and girls, former President Obama issued a memorandum establishing a Working Group on the Intersection of HIV and AIDS, Violence Against Women and Girls, and Gender-Related Health Disparities in 2012 [41]. The Working Group was tasked with coordinating federal agency efforts to address issues involving the intersection of HIV prevention and care and violence against women and girls [42]. The Federal Working Group developed five objectives with related recommended action steps for each participating agency that focus on improving health and wellness: addressing violence and trauma among HIV-positive women in care; addressing contributing factors for violence among HIV-positive women and girls; increasing education, prevention, and outreach efforts for IPV and HIV; and developing interventions that are effective and ensuring support for research that explores the co-occurrence of HIV and violence against women [42, 43]. These recommendations are included in the National HIV/AIDS Strategy: Updated to 2020, which was released in 2015 [44].
CDC conducted the current systematic review as part of the Working Group’s recommended action steps for each participating agency. Given the shared risk and protective factors associated with IPV victimization and HIV and the devastating health and social consequences that they pose to women, the identification and dissemination of dual-focused interventions through this systematic review can potentially reduce the prevalence and incidence of IPV and HIV and therefore improve the lives of vulnerable women.
Methods
Data Sources
Our systematic search was conducted by a specialist from the CDC Public Health Library Information Center (PHLIC). The CDC PHLIC specialist used keyword and indexing terms in the following domains: (1) intimate partner violence/or domestic violence/or battered women; (2) HIV/AIDS; and (3) prevention/intervention. The following electronic databases were searched during January 2016: EMBASE, Medline, PsycINFO, Sociological Abstracts, and the Cochrane Library for articles published prior to January 1, 2016.
Study Selection
Intervention studies were included in the review if they: (1) addressed IPV and HIV prevention; (2) enrolled an adult sample of heterosexual women (≥ 18 years old) or an adult sample stratified by gender; (3) were a randomized controlled trial (RCT) or rigorous quasi-experimental design (with a comparison group); (4) included IPV (i.e., experiencing physical, sexual, and psychological violence) or HIV (e.g., condomless sex and multiple sexual partners) outcome data; (5) were written in English; and (6) were published in a peer-reviewed journal any time prior to January 1, 2016. We limited our focus to adult women 18 years or older because of the previously discussed heightened vulnerability that this population faces. Studies were excluded if they focused exclusively on childhood sexual violence, adolescents, couples (without gender stratification), or only sampled men.
Data Abstraction
The data abstraction form was created by the authors based on the identified list of core components referent above and pilot tested among all authors using a single study. The authors agreed on 95% of initial codes and discussed the 5% of cases where codes diverged. Revisions were made to this form based on the pilot testing to ensure consistency and reliability across data abstraction questions. Once the form was finalized, two of the authors reviewed each study and coded according to the form. The authors then met to compare their codes and resolve coding discrepancies in order to determine final codes. The following variables were coded on the data abstraction form: study characteristics (study location and study date); participant characteristics (e.g., intervention focus, target population, race/ethnicity, age); baseline behaviors (alcohol and other drug use [cocaine, heroin, injection drug], STI and HIV status); design characteristics (e.g., whether they conducted formative research, had an ethnic-matched deliverer or gender-matched deliverer, etc.); intervention core component(s), intervention delivery (e.g., intervention setting, unit of delivery, intervention deliverer); study methodology quality (e.g., unit of assignment, unit of analysis, power analysis, intent-to-treat); and behavioral/biological outcomes (e.g., sexual, physical, and psychological violence by an intimate partner; condomless sex, incident STI/HIV). Our approach of screening and coding studies separately based on program characteristics and outcome data is aligned with the process for systematic reviews recommended by the Task Force on Community Preventive Services (CPSTF) [45]. Screening program characteristics and outcome data independently, as recommended by CPSTF, prohibits one from making causal linkages between program characteristics and outcome data.
Intervention Component Coding
A significant element of this review focused on capturing the core components described in the interventions included in each study (Table 1) using the previously discussed synthesized list of core components. Data coding for core components was based on intervention descriptions. If the study did not mention a component, it was coded ‘no’ for that component. If the study did include a component, it was coded ‘yes.’
Outcome Coding
Primary and secondary outcomes for interventions were also coded. The primary outcomes for IPV victimization included: sexual, physical, and psychological violence; IPV in general or composite (the specific forms of IPV were not provided or the authors combined at least two forms of violence—sexual, physical, and psychological). The primary outcomes for HIV included: condom use (vaginal and/or anal); number of sex partners; and incident STI/HIV (both medically determined and self-reported). The authors determined these outcomes were primary because they are direct mechanisms of HIV transmission (sex without a condom, multiple partners, etc.). All other outcomes were considered secondary because they are moderators and mediators between exposure and outcomes. Secondary outcomes included HIV knowledge, acceptability of physical violence by a man, communication with partner, self-efficacy, and depression.
Results
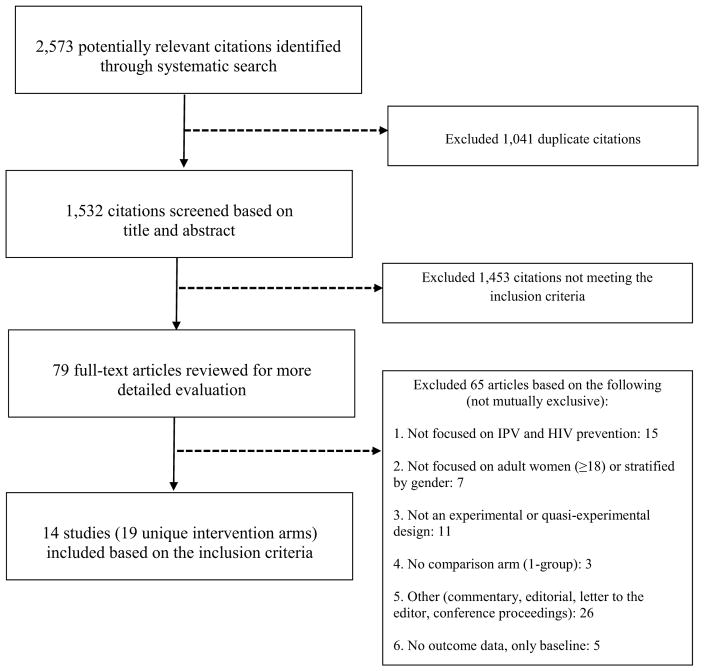
There were a total of 2573 potentially relevant citations identified using systematic search criteria, and 1041 duplicate citations were removed. This resulted in 1532 titles and/or abstracts that were independently screened by all authors (Fig. 1). A total of 1453 citations were excluded because they did not meet the inclusion criteria, which resulted in 79 full-text articles that were reviewed for further detail. Ultimately, 14 studies (19 unique intervention arms) met the six inclusion criterion and are included in this systematic review (Fig. 1). Out of the 14 studies, there were five studies that included two unique intervention arms [47, 48, 50, 51, 59]. The remaining nine studies only had one intervention arm [46, 49, 52–58]. In total, we reviewed the characteristics of 19 intervention arms.
Fig. 1.
Intimate partner violence and HIV systematic review flow chart
Overview of Studies
The 14 studies (19 unique intervention arms) included in this review incorporated both IPV and HIV prevention strategies in the intervention arms [13, 46–59]. In six of the 14 studies, the intervention was adapted from a previous risk reduction behavioral intervention, and five of these interventions had previously been included in CDC’s Compendium of Evidence-Based HIV Prevention Interventions [47, 51, 52, 57, 58]. In addition, three studies [48, 50, 53] were not adapted from previous interventions but are also included as risk-reduction evidence-based HIV behavioral interventions [60].
The 14 studies took place between 1994 (initial recruitment year) and 2012. Four were implemented in the US [48, 49, 52, 59] and ten were implemented internationally (Table 2) [13, 46, 47, 50, 51, 53, 54, 56–58]. The four studies that took place in the US were primarily in urban locations such as New York City, Miami, and Portland, Oregon. Of the ten international studies, eight were conducted in Sub-Saharan Africa, specifically Uganda and South Africa. Other international locations included Mumbai, India and Mongolia, East & Central Asia (Table 2). None of the studies reported cost or cost-effectiveness data.
Table 2.
Study characteristics for interventions that address intimate partner violence and HIV among women
| First author (year) | Intervention name(s) | Intervention focus | Study location | Study dates |
|---|---|---|---|---|
| Abramsky (2014) | SASA! activist kit for preventing violence against women and HIV | To encourage a critical examination and discussion of power imbalances, violence, and increased HIV vulnerability for women through a community mobilization intervention to change community norms, behaviors, and attitudes | Kampala, Uganda | 2007–2012 |
| Carlsona (2012) | HIV sexual risk reduction (HIV-SSR) intervention & HIV sexual risk reduction plus motivational interviewing (HIV-SSR + MI) intervention | To decrease the risk for women who exchange sex and use alcohol through an HIV/STI risk reduction intervention | Mongolia, East & Central Asia | 2007–2009 |
| Ehrhardta (2002) | Project FIO (the Future Is Ours) 4 sessions & project FIO (the Future Is Ours) 8 sessions | To examine the effectiveness of a gender- specific program of heterosexual women attending a family planning clinic | Brooklyn, New York | 1994–1996 (recruitment dates) |
| Gilbert (2006) | Relapse prevention and relationship safety (RPRS) intervention | To test the feasibility, safety, and preliminary effects of an intervention for women on methadone | New York City, New York | 2003–2004 |
| Kima (2009) | IMAGE (intervention with microfinance for AIDS and gender equity) & microfinance-only intervention | To examine the effectiveness of a microfinance and training intervention on gender inequalities, IPV, HIV/AIDS, and poverty | Limpopo Province, South Africa | 2001–2005 |
| Minnisa (2015) | Women’s Health CoOp and Men’s Health CoOp (MHC/WHC) & Couples Health CoOp (CHC) | To examine the effectiveness of a couples and gender-specific intervention on women’s report of relationship power, violence, and communication | Khayelitsha, South Africa | 2010–2012 (recruitment dates) |
| Peragallo (2012) | SEPA (Salud/Health, Educación/Education, Promoción/Promotion, y/and Autocuidado/Self-care) | To examine an HIV risk reduction intervention that is culturally-specific for Hispanic women | Miami-Dade and Broward counties, Florida | 2008–2010 |
| Pronyk (2006) | IMAGE (intervention with microfinance for AIDS and gender equity) | To examine the effectiveness of a microfinance and training intervention on gender inequalities, IPV, HIV/AIDS, and poverty | Limpopo Province, South Africa | 2001–2005 |
| Saggurti (2014) | RHANI (reducing HIV among non-infected) wives intervention | To examine marital conflict and IPV among married women in India | Mumbai, India | 2010–2011 |
| Sikkema (2010) | POWA (people opposing women abuse) HIV prevention interventionb |
To test the feasibility of incorporating HIV prevention with services being received by abused women | Johannesburg, South Africa | 2003–2004 |
| Wagman (2015) | The SHARE project (safe homes & respect for everyone) | To reduce physical and sexual IPV and HIV incidence using a community-based mobilization and a brief intervention | Rakai, Uganda | 2005–2006 |
| Wechsberg (2011) | Women’s Health CoOp (WHC)—Pretoria | To examine the effectiveness of an intervention that focuses on HIV, substance abuse, and gender-based violence among sex and non-sex workers | Pretoria, South Africa | 2003–2008 |
| Wechsberg (2013) | Women’s Health CoOp (WHC)—Cape Town | To examine the effectiveness of an intervention that focuses on HIV, substance abuse, and gender-based violence | Cape Town, South Africa | 2008–2012 |
| Weira (2009) | The Portland Women’s Health Study—HIV risk reduction & The Portland Women’s Health Study—HIV/IPV (intimate partner violence) Risk Reduction | To decrease the risk for HIV and IPV or HIV among women with criminal justice involvement | Portland, Oregon | 2001–2004 |
These studies had two intervention arms
Authors created a name for the intervention; no intervention was provided in the article
Study Participant and Intervention Characteristics
Although all of the interventions included IPV and HIV components, the specific intention of the interventions varied. Intentions of interventions fell into three themes: prevention efforts (primary, secondary, tertiary) to decrease the behavioral risk of HIV among women who had experienced or were at risk for experiencing IPV (physically, sexually, and/or psychologically; four interventions); prevention efforts directed towards women at-risk for HIV who may have also been at risk for IPV due to circumstantial vulnerabilities (e.g., sex workers, women involved with the criminal justice system, women who use alcohol or other substances; seven interventions); and prevention focusing on ameliorating conditions (e.g., poverty, power imbalances, harmful gender/cultural norms, etc.) that make women vulnerable to both IPV and HIV (7 interventions; Table 2). These themes were not mutually exclusive as there was overlap among studies—studies incorporated elements of more than one of these themes. For example, some studies that focused on preventing HIV and IPV also focused on ameliorating social conditions [59]. Given the previously identified shared components between HIV and IPV, the efforts may have been mutually reinforcing, i.e., prevention efforts directed towards IPV prevention may have also yielded benefits for HIV prevention.
Among the study participants, the mean age across the studies was 32 years. Among the US studies (75%) that reported poverty, half (51%) of the women were living below the poverty level (or < $1000/month). Four studies reported HIV-positive status, which ranged from 13% of women to 52% of study participants [13, 56–58]. The majority of studies (12 studies; 88%) reported using a theory and/or framework to guide the intervention. The ones most frequently reported included: social cognitive theory (29%), empowerment theory (29%), and feminist theory (21%). Half of the studies reported using culturally appropriate materials, and two studies (14%) used gender-appropriate materials. Moreover, four studies (27%) reported using an ethnically matched deliverer, and six studies (43%) reported using a gender-matched deliverer. Nine studies (64%) conducted formative research, three studies (21%) formed a community advisory board, and only one study (7%) was trauma-focused (data not shown).
Intervention Delivery, Intensity, and Study Methodology
Intervention delivery, intensity, and study methodology are presented in Table 3. Baseline sample sizes ranged from 34 to 6702 participants. The majority of the interventions were delivered in a group setting (12 studies; 86%) compared to one-on-one delivery (6 studies; 43%; not mutually exclusive). Eight interventions (57%) were delivered in a public area or the community; three interventions (21%) were delivered at a clinic (family planning clinic, drop-in clinic, and HIV treatment clinic); two interventions (14%) were delivered at a participant’s residence, and three interventions (21%) were delivered at a domestic violence shelter, a film show, and soap opera groups. Additionally, the interventions were delivered by different types of personnel including research staff, health care providers, field workers, counselors, police officers, and community workers. The most frequent deliverer was a facilitator (four studies; 29%) or a peer (three studies; 21%).
Table 3.
Intervention characteristics for interventions that address intimate partner violence and HIV among women
| First author (Year) | Study design | Sample Size at Baseline | Unit of delivery (number of women) | Intervention setting | Deliverer(s) | No. of sessions/Duration | Time span |
|---|---|---|---|---|---|---|---|
| Abramsky (2014) | RCT | 717 | Individual & group (8 communities) | Public area/community, residential, & film shows and soap opera groups | Community activist, community leader, traditional marriage counselor, police officer, institutional leader | NRb | 2.8 years |
| Carlsona (2012) | RCT | 166 | Group [6–8] | NR | Facilitator | 6/90 min | 4 weeks |
| Ehrhardta (2002) | RCT | 360 | Group (NR) | Family planning clinic | Facilitator | 4/120 min | 4 weeks |
| Gilbert (2006) | RCT | 34 | Individual & group (NR) | NR | Facilitator | 12/120 min (1 session NR) | 6 weeks |
| Kima (2009) | RCT | 1409 | Group [5] | Public area/community | Peer, trainer & field worker | NR | NR |
| Minnisa (2015) | RCT | 255 | Group [ 4–6] | Public area/community | Peer | 2/180 min | 2 weeks |
| Peragallo (2012) | RCT | 548 | Group (NR) | Community site | Facilitator | 5/120 min | NR |
| Pronyk (2006) | RCT | 843 | Group [5] | Public area/community | Health care provider, trainer, field worker, natural leader | NR | NR |
| Saggurti (2014) | RCT | 220 | Individual & Group (NR) | Public area/community & residential | Counselor | 6/NR | 6–9 weeks |
| Sikkema (2010) | Self-selected | 93 | Group [10] | Domestic violence shelters and drop-in clinics | Counselor & research staff | 6/90 min | 2–6 weeks |
| Wagman (2015) | RCT | 6702 | Individual and group (NR) | Public area/community & HIV treatment clinic | Community volunteer, community counseling Aide, HIV + women | NR | 4 years and 7 months |
| Wechsberg (2011) | RCT | 583 | Individual | NR | Interventionist | 2/50 min | Within 2 weeks |
| Wechsberg (2013) | RCT | 720 | Group [4–6] | Public area/Community | Peer | 2/60 min | Within 2 weeks |
| Weira (2009) | RCT | 530 | Individual | NR | Community health specialist | up to 12/NR | 3 months |
These studies had two intervention arms
NR = not reported
The number of intervention sessions ranged from two to 12 (average was six sessions) with an average duration of 1.6 h per session and an average of 7.6 total intervention hours (Table 3). The time span of the interventions ranged from 1 day to over 4 years, and the follow-up time periods ranged from 2 weeks to approximately 34 months post-intervention (Table 3). In addition, control groups received a wide variety of programming: some control groups received combined IPV and HIV-related content; some included only HIV-related content (including standard of care testing and counseling services); others offered general health and wellness information, knowledge, and skills training, referrals to agencies, and presentations about local community services). None of the control groups received information only related to IPV and not HIV. In almost one-third of the studies (5 studies; 36%), the control participants were waitlisted and did not receive anything until the intervention was complete. The range of control sessions was one to three (average was 2.1 sessions), and the control sessions lasted between 1 and 2 h with an average of 4.4 h.
Almost all of the studies (13; 93%) used random assignment and one study allowed participants to self-select (Table 3) [56]. Eight studies (53%) reported information on random assignment (e.g., using a random-numbers table or computer program) and allocation concealment (concealing which participants are allocated to each group). Moreover, all of the studies used intent-to-treat analysis (analyzing participants as originally assigned regardless of their intervention exposure).
IPV and HIV Intervention Core Content
Examining intervention core content was an integral part of this review (Table 4). More than two-thirds (68%) of the interventions provided knowledge/information on topics related to IPV and/or HIV and AIDS (e.g., distributing a pamphlet describing safe sex behaviors; eight interventions), taught skills for negotiation about safer sex/condom use (six interventions), and offered other HIV-related skill building (e.g., communication, disclosure, and stress reduction). Only one intervention (5%) included information on the effects of trauma (PTSD/anxiety). Many interventions incorporated discussion (n = 12; 63%) or role-playing (n = 10; 53%) when delivering intervention content (data not shown).
Table 4.
Core components for interventions that address intimate partner violence and HIV among women
| Core component | Number (%) of interventionsa |
|---|---|
| Knowledge/informationa | 13 [68] |
| Negotiation about safer sex/condom use (skills)b | 13 [68] |
| Other HIV-related skills (e.g., communication, disclosure, stress)b | 13 [68] |
| Culturally/linguistically appropriate materials and informationb | 12 [63] |
| Empowerment (e.g., knowing a woman’s sexual rights)a | 10 [53] |
| Gender norms/roles or masculinity/femininityb | 10 [53] |
| Correct condom use (skills)b | 9 [47] |
| Power and controlc | 8 [42] |
| Substance use (drugs and alcohol)b | 8 [42] |
| Awarenessc | 7 [37] |
| Goal settingb | 7 [37] |
| Personal risk/vulnerabilityb | 7 [37] |
| Normative influence (e.g., changing peer/social norms)b | 6 [32] |
| Decision-making (skills)b | 5 [26] |
| Motivation/intentionb | 5 [26] |
| Personalized risk reduction planb | 5 [26] |
| Attitude (e.g., towards safer sex, condom use)b | 4 [21] |
| Microfinance/economicsb | 4 [21] |
| Social supporta | 4 [21] |
| Safety planning (skills)c | 3 [16] |
| Women’s sexuality (having a positive view)b | 3 [16] |
| Assessing dangerc | 2 [11] |
| Motivational interviewingb | 2 [11] |
| Protecting family/significant othersb | 2 [11] |
| Self-efficacyb | 2 [11] |
| Effects of trauma (PTSD/anxiety)c | 1 [5] |
14 studies; 19 unique interventions (5 studies had two unique
IPV and HIV prevention
HIV prevention
IPV prevention
Outcomes
The studies that we reviewed ranged from a total of two to eight primary IPV/HIV outcomes. The study by Weir and colleagues [59] analyzed two intervention arms together and compared them to the comparison arm. One study did not report outcome data by intervention versus comparison groups (the authors analyzed the intervention and comparison groups separately); [47] and thus, we did not include in the outcomes table. Although the intervention addressed both violence and HIV risk, two studies did not measure IPV outcomes [48, 56] and three studies did not measure HIV-related outcomes (e.g., condomless sex, condom use, number of sex partners, incident STI/HIV) [46, 51, 53]. In addition, two studies reported either incident STI [52] or HIV [13] and both used biological measures (Table 5).
Table 5.
Primary outcomesa for interventions that address intimate partner violence and HIV among women
| First author (year) | Intervention name(s) | Statistically significant (positive; recall period) Effect size (follow-up time period) |
Non-significant (recall period) Effect size (follow-up time period) |
Mixed resultse (recall period) Effect size (follow-up time period) |
|---|---|---|---|---|
| Abramsky (2014) | SASA! activist kit for preventing violence against Women and HIV |
Sexual violence (past year) aRR = 0.76, 95% CI = 0.33–1.72, P value NR (2.8 years) Physical violence (past year) aRR = 0.48, 95% CI = 0.16–1.39, P value NR (2.8 years) |
||
| Ehrhardtb (2002) | Project FIO (the Future Is Ours) 4 sessions | Condomless sex occasions (past three months) B = −0.40, P = 0.20 (1 month) 6 and 12 month data NR Condom use (past three months) 1, 6, and 12 month data NR |
No condomless sex occasionsf or decrease in condomless sex (past three months) OR = 1.74, 95% CI = 0.99, 3.04, P = 0.05 (1 month) 6 month data NR OR = 1.22, 95% CI = 0.72, 2.08, P = 0.46 (12 months) |
|
| Project FIO (the future is ours) 8 sessions | Condom use (past three months) 1, 6, and 12 month data NR |
No condomless sex occasionsf or decrease in condomless sex (past three months) OR = 1.93, 95% CI = 1.07, 3.48, P = 0.03 (1 month) 6 month data NR OR = 1.56, 95% CI = 0.94, 2.90, P = 0.08 (12 months) |
||
| Gilbert (2006) | Relapse prevention and relationship safety (RPRS) intervention | Psychological violence (severe; past six months) OR = 6.07, 95% CI = 1.22–30.16, P = 0.03 (3 months) |
Sexual violence (minor; past six months) OR = 0.87, 95% CI = 0.15–4.92, P = 0.87 (3 months) Physical violence (severe; past six months) OR = 7.08, 95% CI = 0.82–61.18, P = 0.07 (3 months) Condomless sex (past 90 days) OR = 1.50, 95% CI = 0.44–5.13, P = 0.29 (3 months) Ccondom use (past 90 days) OR = 0.69, 95% CI = 0.10–4.85, P = 0.71 (3 months) Number of sex acts (past 90 days) OR = 2.77, 95% CI = 0.78–9.86, P = 0.09 (3 months) Severe injurious (past six months) OR = 0.66, 95% CI = 0.10–4.36, P = 0.67 (3 months) Severe (physical, sexual, injurious violence; past six months) OR = 1.36, 95% CI = 0.42–4.40, P = 0.33 (3 months) |
|
| Kimb (2009) | IMAGE (Intervention with Microfinance for AIDS and Gender Equity) Microfinance-only intervention | Physical &/or sexual violence (past year)aRR = 0.51, 95% CI = 0.28–0.93, P value NR (24 months) | Psychological violence (past year) aRR = 0.84, 95% CI = 0.38–1.87, P value NR (24 months) condom use (at last sex)aRR = 1.83, 95% CI = 0.94–3.57, P value NR (24 months) aRR = 1.18, 95% CI = 0.77–1.80, P value NR (24 months) Condom use (at last sex) aRR = 1.17, 95% CI = 0.32–4.29, P value NR (24 months) Physical &/or sexual violence (past year) aRR = 0.86, 95% CI = 0.22–3.36, P value NR (24 months) |
|
| Minnisb (2015) | Women’s Health CoOp and Men’s Health CoOp (MHC/WHC) | No victimization experienced (past three months) a OR = 3.05, 95% CI = 1.55–6.00, P = 0.001 (6 months) |
Woman’s influence/control in relationship (past three months) aOR = 0.53, 95% CI = −0.40 to 1.46, P = 0.263 (6 months) |
|
| Couples Health CoOp (CHC) | Woman’s influence/control in relationship (past three months) aOR = 0.92, 95% CI = 0.02–1.83, P = 0.045 (6 months) |
No victimization experienced (past three months) aOR = 1.17, 95% CI = 0.64–2.12, P = 0.614 (6 months) |
||
| Peragallo (2012) | SEPA (Salud/Health, Educación/Education, Promoción/Promotion, y/and Autocuidado/Self-care) | IPV in general (not reported) OR = 0.93, 95% CI NR, P = 0.74 (3 months) OR = 1.14, 95% CI NR, P = 0.54 (6 months) OR = 1.45, 95% CI NR, P = 0.08 (12 months) STI incidence (chlamydia infection) No test for chlamydia at 3 months OR not defined for groups of zero for 6 months OR = 0.37, 95% CI NR, P = 0.37 (12 months) |
Condom use (all time periods) OR = 1.32, 95% CI NR, P = 0.23 (3 months) OR = 0.98, 95% CI NR, P = 0.98 (6 months) OR = 1.77, 95% CI NR, P = 0.01 (12 months) |
|
| Pronyk (2006) | IMAGE (intervention with microfinance for AIDS and gender equity) | Physical or sexual violence (past year) aRR = 0.45, 95% CI = 0.23–0.91, P value NR (24 months) |
Psychological violence (past year) aRR = 0.80, 95% CI = 0.35–1.83, P value NR (24 months) |
|
| Saggurti (2014) & Raj (2013)g | RHANI (Reducing HIV among Non-Infected) Wives Intervention | Condomless sex (past 90 days) aRR = 0.83, 95% CI = 0.75–0.93, P = 0.001 (4.5 months post-baseline) Condom use (at last sex) aOR = 2.42, 95% CI = 1.002–5.70, P = 0.049 (4.5 months post-baseline) Condom use (past 90 days) aOR = 2.76, 95% CI = 1.15–6.60, P = 0.023 (4.5 months post-baseline) |
Sexual coercion (past 90 days) aRR = 0.2, 90% CI = 0.05–0.9, P = 0.082 (4.5 months post-baseline) Physical or sexual violence (past 90 days) aRR = 0.7, 90% CI = 0.2–1.8, P = 0.548 (4.5 months post-baseline) |
|
| Wagman (2015) | The SHARE project (safe homes & respect for everyone) | Psychological violence (past year) aPRR = 1.02, 95% CI = 0.92–1.14, P value NR (16 months post-baseline) aPRR = 0.91, 95% CI = 0.79–1.04, P value NR (35 months post-baseline) Condom use (past year) aPRR = 1.12, 95% CI = 0.52–1.33, P value NR (16 months post-baseline) aPRR = 1.01, 95% CI = 0.84–1.21, P value NR (35 months post-baseline) Number of sex partners (past year) aPRR = 1.00, 95% CI = 0.98–1.01, P value NR (16 months post-baseline) aPRR = 0.98, 95% CI = 0.97–1.00, P value NR (35 months post-baseline) |
Sexual violence (past year) aPRR = 1.12, 95% CI = 0.98–1.31, P value NR (16 months post-baseline) aPRR = 0.80, 95% CI = 0.67–0.97, P value NR (35 months post-baseline) Physical violence (past year) aPRR = 0.97, 95% CI = 0.85–1.11, P value NR (16 months post-baseline) aPRR = 0.79, 95% CI = 0.67–0.92, P value NR (35 months post-baseline) HIV incidence IRR = 0.75, 95% CI = 0.49–1.13, P value NR (16 months post-baseline) IRR = 0.64, 95% CI = 0.42–0.97, P value NR (35 months post-baseline) |
|
| Wechsberg (2011) | Women’s Health CoOp (WHC)—Pretoria—sex workers | Physical violence (past90 days) 4% vs. 11%, P= 0.05(6 months; mainpartner) |
Physical violence (past 90 days) 5% vs. 5%, P value NR (6 months; client) Sexual violence (past 90 days) 7% vs. 14%, P value = 0.08 (6 months;main partner) 5% vs. 5%, P value NR (6 months; client) Condom use (at last sex) 52% vs. 43%, P value NR (6 months;main partner) 100% vs. 99%, P value NR (6 months;client) |
|
| Women’s Health CoOp (WHC)—Pretoria—non-sex workers | Sexual violence (past 90 days) 5% vs. 11%, P = 0.02 (6 months) Condom use (at last sex) 52% vs. 31%, P = 0.004 (6 months) |
Physical violence (past 90 days) 5% vs. 7%, P <0.05 (6 months) |
||
| Wechsberg (2013) | Women’s Health CoOp (WHC)—Cape Town | No physical or partner violence aOR = 1.1, 95% CI = 0.8–1.6, P value = 0.657 (6 months) aOR = 1.1, 95% CI = 0.8–1.6, P value = 0.632 (12 months) Condom use (main partner; past six months) aOR = 1.1, 95% CI = 0.7–1.7, P value = 0.715 (6 months) aOR = 1.5, 95% CI = 0.9–2.3, P value = 0.072 (12 months) Condom use (casual partner; past six months) aOR = 0.6, 95% CI = 0.3–1.3, P value = 0.172 (6 months) aOR = 0.8, 95% CI = 4.1–1.6, P value = 0.519 (12 months) & No casual partners (past month) aOR = 1.1, 95% CI = 0.7–1.7, P value = 0.701 (6 months) aOR = 0.9, 95% CI = 0.6–1.6, P value = 0.533 (12 months) |
||
| Weirb,c,h (2009) | The Portland Women’s Health Study—HIV risk reduction | Any condomless sex (past 30 days) OR = 0.55, 95% CI = 0.32–0.96, P < 0.05 (3 months) OR = 0.54, 95% CI = 0.29–0.97, P < 0.05 (6 months) OR = 0.46, 95% CI = 0.26–0.81, P < 0.05 (9 months) |
Episodes of condomless sex (past 30 days) OR = 0.65, 95% CI = 0.42–1.01, P = 0.052 (3 months) OR = 0.58, 95% CI = 0.36–0.92, P < 0.05 (6 months) OR = 0.62, 95% CI = 0.39–1.00, P < 0.05 (9 months) |
|
| The Portland Women’s Health Study—HIV/IPV (intimate partner violence) Risk Reduction | Combined IPV (physical, coercion, or injury; past three months) OR = 0.91, 95% CI = 0.38–2.20, P value NR (3 months) OR = 0.89, 95% CI = 0.34–2.30, P value NR (6 months) OR = 0.86, 95% CI = 0.33–2.22, P value NR (9 months) |
Category: OR odds ratio, RR risk ratio, PRR prevalence rate ratio, IRR incidence rate ratio, a adjusted, NR not reported;
Primary outcomes: sexual violence, physical violence, psychological violence, condomless sex, condom use, number of sex partners, incident STI;
These studies had two intervention arms;
Two intervention arms were combined for condomless sex;
Authors created a name for the intervention; no intervention was provided in the article;
Mixed results: if the outcome had a positive statistically significant effect at one time point and a non-significant effect at another time point;
Condomless sex occasions = a count variable;
Rai et al. (2013) includes HIV outcomes;
Only the HIV/IPV intervention was compared with the control group for IPV
Our results show that overall, seven studies (54%) reported having at least one statistically significant effect on a primary IPV (sexual, physical, and psychological) or HIV-related outcome (condomless sex and condom use) [49–51, 53, 57, 59] and one study (7.7%) [58] did not have a statistically significant effect on a primary IPV or HIV-related outcome (Table 5). Twelve studies (92%) had at least one non-significant primary IPV or HIV outcome and four studies (31%) had mixed results (the specific IPV or HIV outcome had a positive statistically significant effect at one time point and a non-significant effect at another time point). Only one study (8%) had statistically significant effects on both a primary IPV and HIV outcome [57]. Several of the studies with significant findings incorporated microfinance and/or gender equity and a theory or framework related to empowerment, feminism, and/or power and gender. The secondary outcomes included: increased HIV knowledge, reduced perception of barriers to condom use, increased partner communication about sexual matters, reduced misconceptions about HIV, greater self-confidence, and reductions in depression and substance use (drugs and alcohol).
Discussion
This systematic review examined the published literature on dual-focused (IPV and HIV) victimization prevention interventions for women. We identified 14 studies, with 71% (ten studies) conducted internationally. Three themes emerged from reviewing the focus of the interventions: prevention efforts to decrease the risk of HIV among women who had experienced or at risk for experiencing IPV; prevention efforts directed towards women at-risk for HIV who also may be at risk for IPV; and prevention focused on ameliorating conditions (e.g., poverty) that make women vulnerable to both IPV and HIV. The overwhelming majority of interventions included content focused on providing IPV and/or HIV knowledge/information, teaching condom use and safer sex negotiation skills, and offering HIV-related skill building (Table 4). In addition, more than half of the studies found at least one statistically significant IPV or HIV primary outcome. Only one study found statistically significant outcomes for both an IPV and HIV primary outcome (sexual violence and condom use among non-sex workers; Table 5) [57]. The interventions that address both HIV and IPV in adult women included a wide variety of approaches, components, populations, and methods. Due to the disparate contexts of each study, it is difficult to make generalizations and comparisons between studies as well as establish causality between a specific intervention component and HIV/IPV outcomes. However, the identification of 14 dual-focused studies (19 unique interventions) is a significant step in understanding and addressing this intersection and provides useful information to guide future research and program development. Insight into the syndemic of IPV victimization and HIV will help practitioners develop and deliver primary, secondary, and tertiary prevention interventions. This systematic review gives us useful information to address this epidemic because by describing characteristics of existing interventions, we have an idea of what factors to consider when developing and implementing future interventions—i.e., intended purposes, target populations, theories of change, dose/response levels, and possible outcomes.
Our review of these studies and the existing evidence base of effective interventions suggests that efficacious interventions utilize multiple strategies with multi-pronged, multi-layered approaches (e.g., both individualized and group-oriented) to address the complex syndemic of IPV and HIV. Microfinance (providing loans to poor individuals to help generate income), for example, which has previously been proven efficacious for preventing IPV victimization, was included in the IMAGE intervention along with other more traditional health components [53]. The group that received the program with both microfinance and traditional health components was shown to have higher levels of economic well-being than matched control villages, which lends support to the hypothesis that combined approaches can achieve broader health and social benefits that are protective of both IPV and HIV. Similarly, the Women’s CoOp studies by Wechsberg et al. [58], which included relational, community and structural supports like offering women assistance with food, clothing, transportation, and child care were associated with positive outcomes with regard to both issues. Taken together, this information underscores the need for multi-sectoral, systems-level approaches to address this syndemic. Furthermore, many of the studies that yielded a significant effect on an IPV or HIV outcome incorporated empowerment theory, feminist theory, and/or theory of power and gender [49, 51, 54, 57, 58]. These theories addressed self-efficacy, assertiveness, and communication skills for the purpose of empowerment. Women in these studies may have been empowered by the skills that they developed through the trainings, and as a result, were able to take concrete actions to decrease their risk of IPV and HIV. This information supports the use of empowerment models in prevention programming.
Growing the evidence base of dual-focused interventions may entail further studying risk and protective factors for this syndemic and researching the dissemination, uptake, and possible adaptations of these identified interventions based on cultural context. Possible adaptations may include: applying an intervention that had been effective in one setting with one population to another setting or population; varying-response and exposure times; incorporating additional core components; and changing implementer types. An intervention that is effective in the US may also yield positive results if applied in an international setting. A model for this may be the Women’s Health CoOp mentioned above, which was originally developed in the US (North Carolina) and then adapted for international contexts including South Africa, Russia, and Asia [57, 58]. Interventions that were implemented in urban areas may also work if implemented in rural areas, e.g., Project FIO (the Future Is Ours) [48]. However, significant attention and consideration should be given to appropriate adaptations of these interventions across disparate cultural contexts. In addition, we suggest broadening the scope of evaluation of existing studies to test if interventions that yield outcomes for one of the public health issues (either IPV or HIV) also yield outcomes for the other public health issue, i.e. interventions that decrease physical IPV may also decrease risk of condomless sex. Finally, since a large number of studies were excluded from our review because they were not experimental or quasi-experimental, we identify a need for more rigorous evaluation of existing interventions in order to build up the evidence base of dual-focused interventions. By disseminating these interventions for implementation in varying contexts and rigorously evaluating their outcomes, we may gain more clarity as to the specific intervention content needed to prevent both issues.
In addition to programmatic adaptation and modification, it also may be helpful to vary the level of programmatic intervention. The interventions described in this systematic review were delivered to individuals and small groups. To achieve a broader population-level impact, additional interventions at the outer level of the social ecology (i.e., community and structural/policy approaches) are needed, especially since many of the IPV victimization strategies concern policy approaches [29]. These types of interventions could include: additional microenterprise services, (providing loans to poor individuals to help generate income) social norms campaigns, and gender equity policies [53]. By changing environments and conditions in which women live, there is potential to impact the shared underlying risk factors associated with HIV and IPV victimization and simultaneously prevent both of these issues.
It may also be advantageous to incorporate a dual-focused approach into extant surveillance systems and Notice of Funding Opportunities (NOFOs), formerly called Funding Opportunity Announcements (FOAs). According to Sharon Smith, PhD, the current NISVS instrument (2016–2017) includes a question about a woman’s HIV status which will allow researchers to further obtain information about prevalence of IPV and HIV among women (Sharon Smith zhp5@cdc.gov, September 21, 2017). National HIV Behavioral Surveillance (NHBS) may similarly incorporate IPV victimization questions to gain additional information. Among the CDC-supported EBIs (e.g., sister-to-sister and connect) [61, 62], there is opportunity to incorporate aspects of IPV prevention programming such as training women on communication skills and educating them about power dynamics in relationships [63]. Similarly, among NOFOs for IPV and sexual violence prevention, there may be latitude to address elements of HIV prevention programming like condom use and testing. These dual-focused interventions may include the identified shared components between IPV and HIV and also include feedback from women. This practice has been exemplified by Rountree and Mulraney [64] who interviewed a diverse group of IPV survivors who stated that HIV risk reduction needs to include free HIV testing, transportation, child care, housing, self-esteem, life skills, communication, negotiation skills, and educational and employment attainment [64]. Implementation of these dual-focused prevention efforts may inform intervention research, and in turn, this research will inform further prevention efforts. This cycle will provide for a practice-to-research and research-to-practice feedback loop.
In the current systematic review, none of the 14 studies included information related to cost associated with implementation or cost-effectiveness data. When public health funds and resources are scarce, it is critical to understand the utility of a dual-focused intervention. By addressing IPV and HIV together, we may jointly reduce costs associated with both. Future research may examine the costs and cost-effectiveness of dually addressing these health challenges.
Limitations
There are several limitations to this review. First, gray literature, non-peer-reviewed publications, and qualitative studies were not included. This review focused on studies that fit the inclusion criteria, which was further limited by the paucity of existing intervention-based studies examining both IPV and HIV prevention. Moreover, as an artifact of the inclusion criteria used for this review (i.e., control group), outer level programs of the social ecology (i.e., community and structural/policy approaches) may not have been included. The designs of the studies in this review (randomized controlled trial and quasi-experimental design) may not align well with community-level or policy-level interventions that are typically designed differently (i.e., regression discontinuity). Additionally, there may have been search terms related to components of dual-focused interventions that our search terms criteria or the Medical Subject Headings (MeSH®) terms did not capture and therefore their corresponding studies are not reflected in this review. Additionally, there was no MeSH® term for ‘violence’ [65]. We only reviewed the information reported in the published manuscripts and did not review the intervention manuals for each study, which may have provided more detailed information regarding core components. Due to publication bias, interventions that produced null findings and are therefore less likely to have been published may have been missed since this review only included the published literature. Nonetheless, this review adds much needed information to the scientific field by examining dual-focused interventions.
A major gap in the literature, and therefore opportunity for future research, stems from the lack of interventions targeted to disproportionate risk groups. As previously stated, only four studies reported the women’s HIV statuses [13, 56–58]. We identify a need to target HIV-positive women for such interventions; however it is also important to maintain confidentiality and cognizance of other ethical issues (e.g., informed consent) when collecting information about a woman’s HIV status. In addition, only three studies specifically targeted women who have experienced IPV [13, 49, 54, 56]. Given the co-occurrence between IPV and HIV, it is important for interventions to specifically target women who have suffered at the crossroads of both conditions. Although several studies included racial and ethnic minority women as well as low-income women, other marginalized groups were not included (e.g., transgender women). Also, only one study included female sex workers [57], which have been identified as at increased risk for HIV and IPV [66–68]. Future research on dual-focused interventions could potentially include targeted recruitment of these sub-groups (i.e., transgender women, sex workers) to achieve a representative sample. Related to this lacuna of targeted interventions is our inability to assess causality and directionality of the IPV/HIV relationship. Although research shows that women may experience IPV following disclosure of their HIV-positive status, we cannot prove that HIV was the only factor that resulted in the women experiencing IPV. There may have been other contributory factors to the IPV outcome such as alcoholism, substance abuse, mental health disorders, and generalized community violence. In addition, while this review discusses IPV occurring after HIV contraction, there is also evidence of IPV occurring prior to a woman becoming infected with HIV. Longitudinal studies are needed to further assess the causal and directional relationship between HIV and IPV [69].
Conclusion
IPV and HIV are not isolated phenomena but overlap and interact in ways that can cause serious emotional and physical health conditions among women. Though there is still much work to be done on intervention research and development, this review represents an important contribution to help the field in identifying interventions that address the intersection of IPV and HIV. Despite the limited number of studies contained in this review and the paucity of positive findings on outcomes for both issues, our synthesis of the evidence base of dual-focused interventions serves as a launching point for future research about intervention effectiveness. We believe that our recommendations for future research, particularly about more targeted approaches, will especially help grow the evidence base on IPV which, as stated earlier, is less developed than that of HIV. This heightened knowledge about the syndemic will help guide prevention programming efforts at the community-level for women at-risk for IPV and HIV, i.e. referring IPV victims to HIV prevention services and linking HIV-positive women to IPV prevention programs. These efforts could ultimately work to improve the quality of life for women who suffer at the crossroads of these two devastating public health issues and reduce the overall burden to society posed by both of them.
References
- 1.Wilson PA, Nanin J, Amesty S, Wallace S, Cherenack EM, Fullilove R. Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. J Urban Health. 2014;91(5):983–98. doi: 10.1007/s11524-014-9895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423–41. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 3.Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse. 2007;8(2):149–77. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- 4.El-Bassel N, Gilbert L, Wu E, et al. Intimate partner violence prevalence and HIV risks among women receiving care in emergency departments: implications for IPV and HIV screening. EMJ. 2007;24(4):255–9. doi: 10.1136/emj.2006.041541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. J Womens Health. 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schafer KR, Brant J, Gupta S, et al. Intimate partner violence: a predictor of worse HIV outcomes and engagement in care. AIDS Patient Care STDs. 2012;26(6):356–65. doi: 10.1089/apc.2011.0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: WHO; 2013. [Google Scholar]
- 8.Smith SG, Chen J, Basile KC, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010–2012 State Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 9.The Henry J. Kaiser Family Foundation. The global HIV/AIDS epidemic. 2016. [Google Scholar]
- 10.United Nations Women. Facts and Figures: HIV and AIDS. 2016. [Google Scholar]
- 11.The Joint United Nations Programme on HIV and AIDS (UNAIDS) [Accessed 20 July 2017];Global AIDS Update. http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf.
- 12.Campbell JC, Baty ML, Laughon K, Woods A. Health effects of partner violence: aiming toward prevention. In: Whitaker DJ, Lutzker JR, editors. Preventing partner violence: research and evidence-based intervention strategies. Washington, DC: American Psychological Association; 2009. [Google Scholar]
- 13.Wagman JA, Gray RH, Campbell JC, et al. Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: analysis of an intervention in an existing cluster randomised cohort. Lancet Glob Health. 2015;3(1):e23–33. doi: 10.1016/S2214-109X(14)70344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2015. HIV Surveillance Supplemental Report. 2017;21(2) [Google Scholar]
- 15.Allsworth JE, Anand M, Redding CA, Peipert JF. Physical and sexual violence and incident sexually transmitted infections. J Women’s Health. 2009;18(4):529–34. doi: 10.1089/jwh.2007.0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Adverse health conditions and health risk behaviors associated with intimate partner violence–United States, 2005. MMWR Morb Mortal Wkly Rep. 2008;57(5):113–7. [PubMed] [Google Scholar]
- 17.Mittal M, Senn TE, Carey MP. Intimate partner violence and condom use among women: does the information–motivation–behavioral skills model explain sexual risk behavior? AIDS Behav. 2012;16(4):1011–9. doi: 10.1007/s10461-011-9949-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000;50(4):459–78. doi: 10.1016/s0277-9536(99)00270-1. [DOI] [PubMed] [Google Scholar]
- 19.Moore AM, Frohwirth L, Miller E. Male reproductive control of women who have experienced intimate partner violence in the United States. Soc Sci Med. 2010;70(11):1737. doi: 10.1016/j.socscimed.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Brown MJ, Weitzen S, Lapane KL. Association between intimate partner violence and preventive screening among women. J Womens Health. 2013;22(11):947–52. doi: 10.1089/jwh.2012.4222. [DOI] [PubMed] [Google Scholar]
- 21.Maher JE, Peterson J, Hastings K, et al. Partner violence, partner notification, and women’s decisions to have an HIV test. JAIDS. 2000;25(3):276–82. doi: 10.1097/00126334-200011010-00012. [DOI] [PubMed] [Google Scholar]
- 22.Machtinger EL, Wilson TC, Haberer JE, Weiss DS. Psychological trauma and PTSD in HIV positive women: a meta-analysis. AIDS Behav. 2012;16(8):2091–100. doi: 10.1007/s10461-011-0127-4. [DOI] [PubMed] [Google Scholar]
- 23.Gielen AC, McDonnell KA, Burke JG, O’campo P. Women’s lives after an HIV-positive diagnosis: disclosure and violence. Matern Child Health J. 2000;4(2):111–20. doi: 10.1023/a:1009522321240. [DOI] [PubMed] [Google Scholar]
- 24.Mulrenan C, Colombini M, Howard N, Kikuvi J, Mayhew SH. Exploring risk of experiencing intimate partner violence after HIV infection: a qualitative study among women with HIV attending postnatal services in Swaziland. BMJ. 2015;5(5):e006907. doi: 10.1136/bmjopen-2014-006907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zierler S, Cunningham WE, Andersen R, et al. Violence victimization after HIV infection in a US probability sample of adult patients in primary care. Am J Public Health. 2000;90(2):208. doi: 10.2105/ajph.90.2.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O’Campo P. HIV/AIDS and intimate partner violence intersecting women’s health issues in the United States. Trauma Violence Abuse. 2007;8(2):178–98. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- 27.Whitaker DJ, Baker CK, Arias I. Interventions to prevent intimate partner violence. In: Doll L, editor. Handbook of Injury and Violence Prevention. New York: Springer; pp. 203–221. [Google Scholar]
- 28.Basile KC, DeGue S, Jones K, et al. STOP SV: A technical package to prevent sexual violence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 29.Hardee K, Gay J, Croce-Galis M, Peltz A. Strengthening the enabling environment for women and girls: what is the evidence in social and structural approaches in the HIV response? J Int AIDS Soc. 2014;17(1):18619. doi: 10.7448/IAS.17.1.18619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sherman SG, German D, Cheng Y, Marks M, Bailey-Kloche M. The evaluation of the JEWEL project: an innovative economic enhancement and HIV prevention intervention study targeting drug using women involved in prostitution. AIDS Care. 2006;18(1):1. doi: 10.1080/09540120500101625. [DOI] [PubMed] [Google Scholar]
- 31.National Registry of Evidence-based Programs and Practices (NREPP), Substance Abuse and Mental Health Services Administration. Trauma-Focused Cognitive Behavioral Therapy (TFCBT) intervention summary. [Accessed Aug 24 2015];Program reviewed in 2008. http://legacy.nreppadmin.net/ViewIntervention.aspx?id=135.
- 32.Centers for Disease Control and Prevention. HIV risk reduction: efficacy review: efficacy criteria. Atlanta, GA: Department of Health and Human Services; 2010. [Google Scholar]
- 33.Centers for Disease Control and Prevention. [Accessed Nov 15 2016];HIV/AIDS prevention research synthesis project. 2014b http://www.cdc.gov/hiv/dhap/prb/prs/index.html.
- 34.Breiding MJ, Black MC, Ryan GW. Chronic disease and health risk behaviors associated with intimate partner violence—18 US states/territories, 2005. Ann Epidemiol. 2008;18(7):538–44. doi: 10.1016/j.annepidem.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Kouyoumdjian FG, Findlay N, Schwandt M, Calzavara LM. A systematic review of the relationships between intimate partner violence and HIV/AIDS. PLoS ONE. 2013;8(11):25. doi: 10.1371/journal.pone.0081044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nasrullah M, Oraka E, Breiding MJ, Chavez PR. HIV testing and intimate partner violence among non-pregnant women in 15 US states/territories: findings from behavioral risk factor surveillance system survey data. AIDS Behav. 2013;17(7):2521–7. doi: 10.1007/s10461-013-0493-1. [DOI] [PubMed] [Google Scholar]
- 37.Sareen J, Pagura J, Grant B. Is intimate partner violence associated with HIV infection among women in the United States? Gen Hosp Psychiatr. 2009;31(3):274–8. doi: 10.1016/j.genhosppsych.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 38.Barner JR, Carney MM. Interventions for intimate partner violence: a historical review. J Fam Violence. 2011;26(3):235–44. [Google Scholar]
- 39.Campbell JC, Glass N. Safety planning, danger, and lethality assessment. In: Mitchell CE, editor. Health care response to domestic violence. Oxford: Oxford University Press; 2009. pp. 319–34. [Google Scholar]
- 40.Warshaw C, Sullivan CM, Rivera EA. A systematic review of trauma-focused interventions for domestic violence survivors. Chicago: National Center on Domestic Violence, Trauma & Mental Health; 2013. [Google Scholar]
- 41.Obama B. Presidential memorandum—Establishing a working group on the intersection of HIV/AIDS, violence against women and girls, and gender-related health disparities. [Google Scholar]
- 42.Interagency Federal Working Group. Addressing the Intersection of HIV/AIDS, Violence Against Women and Girls, & Gender-Related Health Disparities. [Google Scholar]
- 43.The White House. [Accessed 7 Nov 2016];FACT SHEET: The National HIV/AIDS Strategy: Updated to 2020. https://www.whitehouse.gov/sites/default/files/docs/national_hiv_aids_strategy_update_2020.pf.
- 44.The White House. National HIV/AIDS strategy for the United States: updated to 2020. [Google Scholar]
- 45.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services—methods. Am J Prev Med. 2000;18(1):35–43. doi: 10.1016/s0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 46.Abramsky T, Devries K, Kiss L, et al. Findings from the SASA! Study: a cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Med. 2014;12(1):122. doi: 10.1186/s12916-014-0122-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carlson CE, Chen J, Chang M, et al. Reducing intimate and paying partner violence against women who exchange sex in Mongolia: results from a randomized clinical trial. J Interpers Violence. 2012;27(10):1911–31. doi: 10.1177/0886260511431439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ehrhardt AA, Exner TM, Hoffman S, et al. A gender-specific HIV/STD risk reduction intervention for women in a health care setting: short-and long-term results of a randomized clinical trial. AIDS Care. 2002;14(2):147–61. doi: 10.1080/09540120220104677. [DOI] [PubMed] [Google Scholar]
- 49.Gilbert L, El-Bassel N, Manuel J, et al. An integrated relapse prevention and relationship safety intervention for women on methadone: testing short-term effects on intimate partner violence and substance use. Violence Vict. 2006;21(5):657–72. [PubMed] [Google Scholar]
- 50.Kim J, Ferrari G, Abramsky T, et al. Assessing the incremental effects of combining economic and health interventions: the IMAGE study in South Africa. Bull World Health Organ. 2009;87(11):824–32. doi: 10.2471/BLT.08.056580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Minnis AM, Doherty IA, Kline TL, et al. Relationship power, communication, and violence among couples: results of a cluster randomized HIV prevention study in a South African township. Int J Womens Health. 2015;7:517. doi: 10.2147/IJWH.S77398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peragallo N, Gonzalez-Guarda RM, McCabe BE, Cianelli R. The efficacy of an HIV risk reduction intervention for Hispanic women. AIDS Behav. 2012;16(5):1316–26. doi: 10.1007/s10461-011-0052-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pronyk PM, Hargreaves JR, Kim JC, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368(9551):1973–83. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 54.Saggurti N, Nair S, Silverman JG, et al. Impact of the RHANI Wives intervention on marital conflict and sexual coercion. Int J Gynaecol Obstet. 2014;126(1):18–22. doi: 10.1016/j.ijgo.2014.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Raj A, Saggurti N, Battala M, et al. Randomized controlled trial to test the RHANI Wives HIV intervention for women in India at risk for HIV from husbands. AIDS Behav. 2013;17(9):3066–80. doi: 10.1007/s10461-013-0586-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sikkema KJ, Neufeld SA, Hansen NB, et al. Integrating HIV prevention into services for abused women in South Africa. AIDS Behav. 2010;14(2):431–9. doi: 10.1007/s10461-009-9620-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wechsberg WM, Zule WA, Luseno WK, et al. Effectiveness of an adapted evidence-based woman-focused intervention for sex workers and non-sex workers: the Women’s Health CoOp in South Africa. J Drug Issues. 2011;41(2):233–52. [Google Scholar]
- 58.Wechsberg WM, Jewkes R, Novak SP, et al. A brief intervention for drug use, sexual risk behaviours and violence prevention with vulnerable women in South Africa: a randomised trial of the Women’s Health CoOp. BMJ. 2013;3(5):e002622. doi: 10.1136/bmjopen-2013-002622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Weir BW, O’Brien K, Bard RS, et al. Reducing HIV and partner violence risk among women with criminal justice system involvement: a randomized controlled trial of two motivational interviewing-based interventions. AIDS Behav. 2009;13(3):509–22. doi: 10.1007/s10461-008-9422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Centers for Disease Control and Prevention. [Accessed 15 Dec 2016];Complete Listing of Risk Reduction Evidence-based Behavioral Interventions. http://www.cdc.gov/hiv/research/interventionresearch/compendium/rr/complete.html.
- 61.Jemmott LS, Jemmott JB, III, O’Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. Am J Public Health. 2007;97(6):1034–40. doi: 10.2105/AJPH.2003.020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.El-Bassel N, Witte SS, Gilbert L, et al. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am J Public Health. 2003;93(6):963–9. doi: 10.2105/ajph.93.6.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Conroy AA, Tsai AC, Clark GM, et al. Relationship power and sexual violence among HIV-Positive women in Rural Uganda. AIDS Behav. 2016;20(9):2045–53. doi: 10.1007/s10461-016-1385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rountree MA, Mulraney M. HIV/AIDS risk reduction intervention for women who have experienced intimate partner violence. Clin Soc Work J. 2010;38(2):207–16. doi: 10.1007/s10615-008-0183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fogel CI, Crandell JL, Neevel AM, et al. Efficacy of an adapted HIV and sexually transmitted infection prevention intervention for incarcerated women: a randomized controlled trial. Am J Public Health. 2015;105(4):802–9. doi: 10.2105/AJPH.2014.302105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Romero-Daza N, Weeks M, Singer M. Conceptualizing the impact of indirect violence on HIV risk among women involved in street-level prostitution. Aggress Violent Behav. 2005;10(2):153–70. [Google Scholar]
- 67.Seth P, DiClemente JR, Lovvorn AE. State of the evidence: intimate partner violence and HIV/STI risk among adolescents. Curr HIV Res. 2013;11(7):528–35. doi: 10.2174/1570162x12666140129103122. [DOI] [PubMed] [Google Scholar]
- 68.Strathdee SA, Lozada R, Martinez G, et al. Social and structural factors associated with HIV infection among female sex workers who inject drugs in the Mexico-US border region. PloS ONE. 2011;6(4):e19048. doi: 10.1371/journal.pone.0019048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hatcher AM, Woollett N, Pallitto CC, et al. Bidirectional links between HIV and intimate partner violence in pregnancy: implications for prevention of mother-to-child transmission. J Int AIDS Soc. 2014;17:19233. doi: 10.7448/IAS.17.1.19233. [DOI] [PMC free article] [PubMed] [Google Scholar]