Abstract
Filipinos are one of the fastest growing Asian ethnic groups in the United States, yet little is known about how to specifically address the varying health needs of the Filipino community with diabetes and heart disease. This is a problem because rates of potentially preventable hospitalizations (PPH) are high for Filipinos with these conditions. A PPH is a hospitalization that could potentially have been avoided with better access to quality primary care. Patients over 21 years of age with heart disease or diabetes and who were hospitalized at the Queen's Medical Center with a PPH were recruited to complete a face-to-face interview eliciting the patients' perspectives on key factors leading to this hospitalization (n=102). This study focused on a subset of Filipino patients (n=21). Two independent coders reviewed interviews to identify factors leading to their PPH. A majority of the Filipino respondents identified social vulnerabilities as the most common factor that led to their hospitalization, including financial challenges, limited social support, and life instability. Many respondents also noted challenges with the healthcare system as precipitating their hospitalization, including poor communication/coordination, management plan issues, and bad experience with their healthcare providers. Cultural and language barriers were also identified by Filipino patients as challenges leading to their hospitalizations. These findings emphasize the importance of considering patients' perspectives of the barriers they face inside and outside of healthcare facilities.
Keywords: Filipino health; diabetes mellitus; heart failure; preventable hospitalizations; patient perspectives, qualitative research
Introduction
Filipinos, currently comprising 14% of the population in Hawai‘i, are one of the fastest growing Asian ethnic groups in the United States.1 Despite their growing number, there are very few widescale initiatives that specifically address the varying health needs of the Filipino community.2 The few studies comparing Filipinos with other ethnic groups in Hawai‘i have found disparities in health-related outcomes, such as lack of routine access to preventable health care.3 Additionally, over 1 in 10 Filipino adults have been diagnosed with diabetes (10%) and over a third have been diagnosed with hypertension (37%), which is higher than many other racial/ethnic groups in Hawai‘i.4–6
Because of these factors, Filipinos have high rates of potentially preventable hospitalizations, which are defined as admissions for chronic conditions, such as diabetes or heart failure, that could have been avoided with better access to high quality outpatient care.7 Between 2007 and 2012, an estimated $353 million was spent in Hawai‘i for potentially preventable hospitalizations for heart disease and diabetes, with approximately $8,400 spent for each hospitalization for a Filipino patient.8 Not only are the hospitalizations for heart disease and diabetes expensive and burdensome to patients, they can lead to patients being at greater risk for hospital-associated adverse events such as excess mortality observed in patient with diabetes admitted for foot problems 9,10
A prior study examined pathways to preventable hospitalizations for patients hospitalized for heart disease and/or diabetes in a large hospital in Hawai‘i.11 This study identified six underlying factors for preventable hospitalizations: (1) social factors; (2) knowledge; (3) practical problems; (4) avoidance/denial; (5) health care system; (6) behavioral health. Adapting the pathway model developed from the prior study for Filipino patients specifically could help us understand relevant pathways to preventable hospitalizations and identify potential intervention points for this community.11 Thus, the goal of this study was to identify the various pathways to diabetes and/or heart disease-related preventable hospitalizations specifically among Filipino patients in Hawai‘i.
Methods
Patients eligible for inclusion in the study were those 21 years and older who self-reported Filipino ethnicity and were admitted to The Queen's Medical Center from June 2013 to February 2016 for either heart failure and/or diabetes-related potentially preventable hospitalization, as defined by the Agency for Health Care Research and Quality Metrics.12 As we identified patients during their hospital stay, we were therefore unable to use discharge diagnoses to identify this study cohort. Instead, we used the principal “working” diagnosis to identify potentially eligible subjects.13
Patients unable to effectively communicate in English, unwilling to participate, admitted in the Intensive Care Unit, clinically unstable, pregnant, suffering with memory loss, non-Hawai‘i resident, or resided in a nursing home, hospice, prison, or other similar institution were excluded from the study.
Data Collection
After obtaining informed consent, participants completed a face-to-face interview in which they were asked both closed- and open-ended questions to assess factors related to their hospitalization. Relevant questions are available from the authors upon request. Interview questions were developed using relevant items from other studies, including validated measures. Open- ended questions were specifically designed to allow for patient perspectives around factors relevant to preventable hospitalizations for heart failure and diabetes based on existing literature. Interviews were pilot tested and refined before administration. The survey included the Rapid Estimate of Adult Literacy in Medicine (REALM), a screening instrument used to determine a patient's reading level.14
The majority of the interviews were completed by a trained Native Hawaiian female research nurse. Patients were encouraged to elaborate on stories and themes. Responses were recorded using an iPad. The open-ended questions took approximately 20 minutes for each patient. Field notes were taken by the interviewer during and immediately after the interview. Patients received a $20 drug store gift card incentive.
Demographic information (eg, age, gender, ethnicity) and relevant clinical information (eg, same hospital readmission, have been told by a doctor or other health professional if they have diabetes or heart disease) were obtained from the patients' medical record. The medical record review was used to gather data to validate and supplement the survey data.
Qualitative Analyses
Two researchers (TS and JM) independently reviewed audio recordings and field notes for the 21 Filipino patients and identified themes and details about the patients' stories regarding pathways to hospitalizations. The researchers then met to discuss the themes for each patient. After recorded interviews of all 21 patients were reviewed, they re-examined the consensus coding documents to ensure congruence with the final study factors and pathways. This final consensus coding was used for analyses. Quantitative data concerning demographic information was linked to the qualitative analysis.15,16 The research protocol was approved by the University of Hawai‘i Cooperative Institutional Review Board (CHS 21136).
Results
In the full study, 102 patients participated and 21 self-identified as Filipino. Of the 21 Filipino participants, 62% were aged 21–64, 71% were male, and 60% of those who reported income had family income less than $40,000 (Table 1). Seventy-one percent of the participants were born in the US, and 91% preferred to speak in English. Participants reported good access to care: 100% were insured and 91% had a usual source of care. Approximately one quarter (24%) of the hospitalizations were diabetes related, 33% were heart disease related, and 43% were both diabetes and heart disease related. The majority of the participants (63%) had a prior hospitalization for the same issue.
Table 1.
Patient Characteristics for the Filipino Participants (n=21) and the Total Sample (N=102).
| Filipino (%) | Non-Filipino (%) | |
| Age Group | ||
| Working Age (18–64) | 62 | 75 |
| Older (65+) | 38 | 25 |
| Education | ||
| Less than High School | 29 | 21 |
| High School Grad | 71 | 74 |
| College Grad | 0 | 5 |
| REALM | ||
| Low Health Literacy | 57 | 48 |
| Female | 29 | 33 |
| Yearly Income* | ||
| Less than $20,000 | 10 | 56 |
| Between $20,000–$40,000 | 50 | 32 |
| More than $40,000 | 40 | 12 |
| Insured | 100 | 88 |
| Has Usual Care | 91 | 86 |
| Prefer to Speak English | 91 | 89 |
| Admitted for: | ||
| Diabetes | 24 | 38 |
| Heart Disease | 33 | 27 |
| Both | 43 | 35 |
| Previously Hospitalized for this Issue | 63 | 66 |
Income was missing for 11 Filipinos and 23 Non-Filipinos
Pathways
Following a framework developed from the full sample, three types of factors were identified based on the qualitative data analysis: underlying, precipitating, and immediate factors. Factors were not mutually exclusive—patients could report one or more factors in each step of the pathway. Immediate factors were defined as the reason for admission and were clinical in nature. Precipitating factors were generally behavioral in nature and were the reason why the immediate factors arose. These included not taking medication as prescribed, not exercising, and not eating well. The underlying factors tended to be related to demographics (eg, low income) and mental health issues that led to the precipitating factors. An example of a pathway might be: a patient whose income is below the poverty level (underlying factor) may not take their medication (precipitating factor) because they cannot afford it and may end up in the hospital because of dangerously high blood sugar levels (immediate factor). These pathways are discussed in more detail elsewhere.11
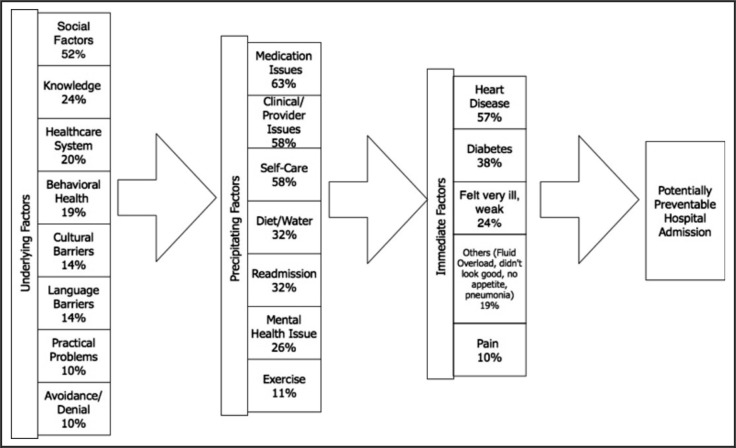
Healthcare system issues, behavioral health, and social challenges emerged as important themes in patient stories (Figure 1). Additional underlying factors included language and cultural barriers. Figure 1 shows the distribution of underlying, precipitating, and immediate factors resulting in potentially preventable hospitalizations for the 21 Filipino patients. For 57% of patients, immediate reasons for their hospitalizations included acute issues related to cardiovascular symptoms, such as shortness of breath and fluid overload. Fluid overload occurs when there is excessive water in the body resulting in swelling of the legs or arms and is a common reason for hospitalization in heart disease.17
Figure 1.
The Distribution of Underlying, Pprecipitating, and Immediate Factors Resulting Potentially Preventable Hospitalizations from the Filipino Patient Stories (n=21).
Approximately 63% of patients reported medication issues as a precipitating reason for their PPH (Figure 1). Other precipitating factors reported by patients were issues with clinics/providers (58%); challenges with self-care (58%); issues following diet or water intake restrictions (32%); readmission focused challenges (32%), such as inability to follow discharge instructions; a mental health/behavioral health issue (26%); and/or challenges with exercising (11%).
Social Factors
The most common underlying factor for Filipino patients was social vulnerability, reported by 52% of the participants (Figure 1). The emergence of social vulnerability as one of the recurrent factors in Filipino patient narratives was supported by the demographic data: 29% had no high school diploma, 57% had low health literacy, 60% reported household income of less than $40,000 annually, and 9% preferred to speak in their native language (Table 1).
Patients mentioned some examples of social factors that contributed to problems in managing their chronic conditions, including financial issues, limited social support, and life instability. For example, Patient A, who was hospitalized with diabetes, said, “I can shop, don't always buy what's good to me. Food expensive, little money.” Patient B stated, “I was shut down so many times I needed help. I would ask for money from people, so I could go to the doctor's office. It's rather disheartening and I feel embarrassed at time for feeling so.” Six patients also said that they delayed or did not get their needed medical care because they worried about the cost.
Participants with social support mentioned that they heavily relied on their family to help them manage their chronic conditions. For example, Patient C with diabetes said, “I don't remember to take my medications ‘til the pain starts. I need my daughter to remind me to take my medications.” Patient D stated, “Because my heart condition, I get tired a lot. I need help with organizing my day. Sometimes I need help to get up and use the walker, but there's no one at home to help.” Patient E also mentioned, “Sometimes my brother helps me go to the doctor, pick up prescription, and go to the grocery stores.” Patient F noted the critical importance of social support in health and described how he felt like a burden and inconvenience to his family.
In many cases, patients who described these social factors noted they were aware of what they should do to manage their chronic conditions; however, due to their social or financial challenges, they were unable to implement their management plan. For instance, Patient G said that people around him did drugs and he did not feel he had a sense of control in his environment. Because of that, he wanted to get his own place where he thinks he can get better: “If I keep going on that place I don't think I'll get better.”
Healthcare System Related Issues
One fifth (20%) of patients reported healthcare system-related issues as precipitating factors for their preventable hospitalizations (Figure 1). One issue identified was insufficient interaction with providers. Patient B stated that “[The clinic] want to get you quick [out] as soon as possible.”
Two patients complained about the hospital or clinic not meeting their health needs due to poor communication between patient and providers. Patient H said, “Sometimes the doctors ask questions but don't tell me what's going on. I went into the hospital, but no one was explaining stuff to me.” Patient J echoed Patient H's frustration about their doctors not articulating the seriousness of their condition. Patient J noted, “If they [had] done that, I could have listened…They need to explain what's happening to the patient and why it's happening to the patient and how things can change or responding depending on the circumstances.”
Patient Q said, “Sometimes my vision blurry. I cannot see words—I forget to tell my doctor, most of the time. They talked about my leg wound. Not much about other stuff. The diabetes but never my eyes. I understand more than I can read.”
Several of the participants mentioned the challenge of following their management plan created by the doctors, as exemplified by Patient E who said: “I have a hard time, frustrating time with managing my health. If you give me too many things to do. I can't do it and I quit. I rather do something small that I can manage then try manage me and all of it (time/schedule). It drives me crazy and I just quit doing anything for me. I want time to enjoy myself and do the things I want to do than have my health dictate my time. I easily get frustrated especially when I feel out of control. There are times when my health is out of control and it's hard to follow directions when I'm not feeling good.”
Four individuals echoed the thoughts of this participant with diabetes, who doesn't check his blood sugar level daily “because it usually ends up the same.” Twelve individuals reported not taking medications, as exemplified by Patient A: “Sometimes I don't want to take medication I have in my home. Sometimes I feel weak and tired. I don't feel good taking the medication.”
Some patients described notably bad experiences with the healthcare system. Patient B who was homeless and had heart failure stated: “Because I'm homeless, I feel as if I am an outcast. Sometimes the way I'm treated because of the way I look.” In addition, the patient believed that “[the state] have nothing they can do. State don't want to help you. They help other people, beside us… That's the truth.” Some avoided going to the doctor like Patient H with heart failure: “I usually never ask for help. Why? Because I don't want to feel stupid, inadequate perhaps shame about not knowing anything. If I need help for my health I usually just stay home. I can take care of myself.” One patient even mentioned that “the only way you can get your medication if you see your doctor. If you can't see your doctor, you go to the emergency… because you have no choice. What choice do I have?”
Cultural Barriers
Cultural barriers also emerged from patient stories as important factors affecting potentially preventable hospitalizations in Filipino patients, with 14% of respondents mentioning this factor (Figure 1). Two patients reported that establishing trust with their doctors and providers understanding their culture were important to them. Patient I said, “For me I learn different especially local ways. It's important for me to have face-to-face interaction. Trust to be established, I need to look in your eyes. You need to come from/or have information I can learn more about what I need to do. Doesn't make sense to me to learn somethings over, it has to be a shared experience.” Patient J said, “It boils down to relationship. It's all relationship. If you're going to get a doctor that looks down up you, or not understand our culture then eventually it's going to break up… It is important. Where you grew up? Who's your parents? Who you related? That's part of Hawai‘i. That's part of our culture.”
Language Barrier
Another factor was the language barrier. Fourteen percent of the respondents reported the language barrier as an issue (Figure 1). Patient A, who had recently migrated to Hawai‘i, described how English-language barriers affected how he handled his conditions. He mentioned that he brings a cousin with him to his doctor visits to help fill out forms and translate. Patient G with diabetes and heart failure, who was born in the Philippines, had a hard time understanding his doctor. The patient said, “Sometimes my doctor talks too fast and uses words I don't understand. But I don't ask questions I let him talk I don't like to bother.”
Knowledge
Twenty-four percent of the respondents identified lack of knowledge about their conditions as an underlying factor (Figure 1). A few individuals, like Patient K with diabetes, didn't know they had a chronic disease. Five individuals had the disease for years but lacked specific information about how to care and manage their conditions. Patient L said, “My doctor and I discussed about no salt. I didn't think little salt will hurt. I don't [know] what food I can't eat … I didn't know if it's safe to take my water pills with my medications together. I don't know if I should take it together.” Seven individuals (33%) echoed the thought of this respondent, Patient H with heart disease said, “I didn't think [my condition] was that bad.”
Behavioral Health
Overall, 19% of respondents reported behavioral health issues, including active substance abuse, depression and stress (Figure 1). Four patients felt that these issues had contributed to their hospitalizations. Patient M, who had several chronic health conditions including depression, used meth to escape from reality and feel numb. Patient B had used meth “to forget the pain and hunger” and said, “everyone is doing it.” Due to their challenging lifestyle, it was then hard for them to manage their condition. Patient R said, “I am homeless, no place to live. Very stressful. No really able to trust people. I am depressed about my situation. I have nothing.”
Self-Care/Practical Problems
Practical problems not caused by social or mental health issues also created challenges for patients. These included forgetting to take their medications and being too busy to manage their health. Practical problems were reported by 10% of participants (Figure 1). Patient L with a heart disease who was sent to the hospital because of difficulty breathing said, “Sometimes I forget to take my water pills because I only take it once not like my other medications.” Patient N said, “I don't know where to start” referring to the overwhelming management plan recommended by the doctor.
Denial/Avoidance
Denial or avoidance of the problem was reported by 10% of respondents (Figure 1). Denial or avoidance includes patients who believed they were healthy or did not want to deal with their chronic conditions. Patient O mentioned, “As long as I feel good when I go out [of the hospital], I think I'm okay.” Patient P with both chronic conditions had said, “I am ‘hard head’ I know what I need to do… eat right, take my medication, etc.”
Discussion
This study included a convenience sample of Filipino patients who had PPH. In-depth interviews of 21 Filipino patients with diabetes and heart failure enabled us to identify their PPH pathways. Their stories also provided insight into patient perspectives regarding the primary factors that led to their PPH for chronic condition(s).8,18 By definition “preventable” assumes that, if certain factors are addressed, the hospitalization could potentially have been avoided. Traditionally, these factors have been linked to hospital-focused factors (e.g. more patient education, better discharge planning) and areas where patients can improve themselves (e.g. better adherence, more responsibility/self-efficacy). In reality, the situation is much more complex.
From their own stories, PPH pathways of Filipinos in Hawai‘i were primarily associated with social vulnerabilities, healthcare system related issues, and cultural/language barriers. Social vulnerabilities, such as financial challenges, limited social support, and life instability were the most common underlying factors for Filipinos. This can be true for poor patients regardless of their race or ethnicity and was also the most common underlying factor in the overall sample of patients hospitalized with a preventable condition.19 An emergent theme notably common to the Filipino patients was their discussion about the support or involvement of family members in their care, which is a key Filipino cultural value.20 Many of the patients' families act as a motivating factor, and patients rely on their family for managing their health. This tendency can be found in other cultures especially for first-generation immigrants.21 For example, Patient C with diabetes needed the help of her daughter to remind her to take her medication. Some even expressed that they felt that they are a heavy burden to their family. This may be an important area to focus interventions.
We also identified healthcare system-related issues that may have contributed to respondents' hospitalizations, including insufficient interaction with their doctors, poor communication/coordination, management plan issues, and bad experiences. For instance, Patient S with diabetes said that she wished her doctor had articulated the seriousness of her condition better.
Some of the recent immigrants and the elderly reported the English language was a barrier to seeking healthcare services. For example, four patients mentioned that their physicians talked too fast or used medical terms that were difficult for them to understand. Additionally, patients reported that they don't want to ask questions because they “don't want to cause any trouble” to avoid embarrassment and avoid questioning authority. Moreover, language barriers may be an even greater barrier for Filipinos who were excluded from the study based on language issues.
Two patients reported avoidance or denial as an underlying factor. This may be due to Filipino's strong belief in fatalism or known in Filipino as bahala na. If the patient perceives his or her condition is hopeless or “out of their hands,” the patient would not fully engage and invest in managing their condition. Another Filipino cultural belief that may influence their behavior related to their condition was pakikisama or being very respectful and polite to people in authority. For instance, Filipinos may avoid asking for clarification even though they do not understand what is being told to them. As patient J noted, “I'm not the person to ask.” These tendencies should be kept in mind when treating Filipino patients, especially in regard to their understanding of their management plan.22, 23
Several limitations of this study should be mentioned. First, our sample was small and came from only one hospital in Hawai‘i, limiting generalizability. In addition, our participants may have responded to the open and closed ended questions in a manner that was socially acceptable. For instance, they may have been less likely to report substance abuse or share social challenges. Moreover, studies have shown that the interviewer's ethnicity, nationality, culture, religion, color of their skin, age, and gender can influence participant's responsiveness.24 Another limitation was the study population was limited to patients who spoke English. Pathways of non-English speaking Filipino patients may be different from those identified in this study.
Understanding the patient's perspectives is critical to the prevention of future hospitalizations. Patient perspectives can help healthcare providers develop management plans that are suitable, acceptable, and realistic for the patients.25 Increasing patients' involvement in their care could empower them by improving their knowledge of their health and giving them a sense of ownership of their health.26
Acknowledgement
The authors thank Malia Young and May Vawer for assistance with recruiting and interviewing patients and Michelle Quensell for helping to code data. This study was funded in part by the NIH National Institute on Minority Health and Health Disparities (NIMHD) grants P20 MD000173 and U54MD007584.
Biography
Jhon Michael Malabed
Jhon Michael Malabed is a junior at the University of Hawai‘i at Manoa and currently working toward his BS in Biology with a minor in Ilokano Language and Culture. In 2017, he worked as a summer research intern with the John A. Burns School of Medicine's Department of Native Hawaiian Health under the mentorship of Dr. Deborah Taira of the Daniel K. Inouye College of Pharmacy with additional assistance from Dr. Tetine Sentell and Dr. Kathryn Braun of University of Hawaii Manoa's Public Health Studies and Dr. Todd Seto of Queen's Medical Center. He presented his research project at the 2017 Hawai‘i Health Workforce Summit and won first-place for their health disparities poster competition. He is currently completing another research project with Infractructure Development Networks for Biomedical Research Excellence (INBRE) program, based at the John A. Burns School of Medicine and funded by the National Institutes of Health.
His winning manuscript is entitled, “Pathways to Preventable Hospitalization for Filipino Patients with Diabetes and heart Disease in Hawai‘i.” Filipinos are one of the fastest growing Asian ethnic groups in the United States, yet little is known about how to specifically address the varying health needs of the Filipino community with diabetes and heart disease. This is a problem because rates of potentially preventable hospitalizations (PPH) are high for Filipinos with these conditions. A PPH is a hospitalization that could potentially have been avoided with better access to quality primary care. The goal of this study was to investigate the factors and barriers that led to preventable hospitalizations among Filipino patients with heart disease and diabetes. From the patient's own stories, potentially preventable hospitalization pathways of Filipinos in Hawai‘i were primarily associated with social vulnerabilities, healthcare system related issues, and cultural/language barriers. They identified these challenges leading to their hospitalization. The findings emphasize the importance of considering the patient's perspectives in the prevention of future hospitalizations. Patient perspectives can help healthcare providers develop management plans that are suitable, acceptable, and realistic for the patients.
Conflict of Interest
None of the authors had conflicts of interest to report.
References
- 1.US Census Bureau, author. 2010 census shows Asians are fastest-growing race group. [December 2, 2017]. https://www.census.gov/newsroom/releases/archives/2010_census/cb12-cn22.html.
- 2.Chalmers ML, Housemann RA, Wiggs I, Newcomb-Hagood L, Malone B, Brownson RC. Process evaluation of a monitoring log system for community coalition activities: five-year results and lessons learned. Am J Health Promot. 2003;7(3):190–196. doi: 10.4278/0890-1171-17.3.190. [DOI] [PubMed] [Google Scholar]
- 3.Moy E, Mau MK, Raetzman S, Barrett M, Miyamura JB, Cheves KH, Andrews R. Ethnic differences in potentially preventable hospitalizations among Asian Americans, Native Hawaiians, and other Pacific Islanders: implications for reducing health care disparities. Ethn Dis. 2013;23(1):6–11. [PubMed] [Google Scholar]
- 4.Hawai‘i State Department of Health, author. The Hawai‘i behavioral risk factor surveillance system: 2015 results. [July 9, 2017]. https://health.hawaii.gov/brfss/files/2016/07/brfss15_results.pdf.
- 5.Hawai‘i State Department of Health, author. Hawai‘i health data warehouse, indicator-based information system for public health. [February 19, 2018]. http://ibis.hhdw.org/ibisph-view/query/result/brfss/DXDiabetes/DXDiabetesCrude11_.html.
- 6.Bayog ML, Waters CM. Cardiometabolic risks, lifestyle health behaviors and heart disease in Filipino Americans. Eur J Cardiovasc Nurs. 2017;16(6):522–529. doi: 10.1177/1474515117697886. [DOI] [PubMed] [Google Scholar]
- 7.Moy E, Chang E, Barrett M Centers for Disease Control and Prevention, author. Potentially preventable hospitalizations—United States, 2001–2009. MMWR Surveill Summ. 2013;62(Suppl 3):139–143. [PubMed] [Google Scholar]
- 8.Sentell TL, Ahn HJ, Miyamura J, Juarez DT. Cost Burden of Potentially Preventable Hospitalizations for Cardiovascular Disease and Diabetes for Asian Americans, Pacific Islanders, and Whites in Hawai‘i. Journal of Health Care for the Poor and Underserved. 2015;26(20):63–82. doi: 10.1353/hpu.2015.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303(21):2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nirantharakumar K, Saeed M, Wilson I, Marshall T, Coleman JJ. In-hospital mortality and length of stay in patients with diabetes having foot disease. J Diabetes Complications. 2013;27(5):454–458. doi: 10.1016/j.jdiacomp.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Sentell TL, Seto TB, Young MM, et al. Pathways to potentially preventable hospitalizations for diabetes and heart failure: a qualitative analysis of patient perspectives. BMC Health Serv Res. 2016;16:300. doi: 10.1186/s12913-016-1511-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agency for Health Research and Quality (AHRQ), author Prevention quality indicators overview: AHRQ Quality Indicators. Bethesda: 2011. [November 18, 2017]. http://www.qualityindicators.ahrq.gov/modules/pqi_overview.aspx. [Google Scholar]
- 13.Jiang HJ, Andreaws R, Styer D, Friedman B. Racial/ethnic disparities in potentially preventable readmissions: The case of diabetes. Am J Public Health. 2005;95(9):1561–1567. doi: 10.2105/AJPH.2004.044222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, Crouch MA. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 15.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42(4):1758–1772. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith J, Firth J. Qualitative data analysis: the framework approach. Nurse Res. 2011;18(2):52–62. doi: 10.7748/nr2011.01.18.2.52.c8284. [DOI] [PubMed] [Google Scholar]
- 17.Pellicori P, Kaur K, Clark AL. Fluid Management in Patients with Chronic Heart Failure. Cardiac Failure Review. 2015;1(2):90–95. doi: 10.15420/cfr.2015.1.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quensell ML, Taira DA, Seto TB, Braun KL, Sentell TL. “I Need my Own Place to get Better”: Patient Perspectives on the Role of Housing in Potentially Preventable Hospitalizations. Journal of Health Care for the Poor and Underserved. 2017;28(2):784–797. doi: 10.1353/hpu.2017.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.King GL, McNeely MJ, Thorpe LE, et al. Understanding and Addressing Unique Needs of Diabetes in Asian Americans, Native Hawaiians, and Pacific Islanders. Diabetes Care. 2012;35(5):1181–1188. doi: 10.2337/dc12-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agbayani-Siewert P. Filipino American culture and family: Guidelines for practitioners. Families in Society. 1994;75(7):429. [Google Scholar]
- 21.Sentell TL, Shen C, Landsittel D, Mays MH, Southerland J, King MH, Taira DA. Racial/Ethnic Differences in Those Accompanying Medicare Patients to the Doctor: Insights from the 2013 Medicare Current Beneficiary's Survey. Journal of immigrant and minority health. 2017:1–8. doi: 10.1007/s10903-017-0582-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujii D. The neuropsychology of Asian Americans. New York: Psychology Press; 2015. [Google Scholar]
- 23.McDermott JF, Andrade NN. People and cultures of Hawaii: The evolution of culture and ethnicity. University of Hawai‘i Press; 2011. [Google Scholar]
- 24.Fryer CS, Passmore SR, Maietta RC, Petruzzelli J, Casper E, Brown NA, Quinn SC. The symbolic value and limitations of racial concordance in minority research engagement. Qualitative health research. 2016;26(6):830–841. doi: 10.1177/1049732315575708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yagil D, Biron M, Pat D, Mizrahi-Reuveni M, Zoller L. Accurate diagnosis of patients' distress levels: The effect of family physicians' ability to take the patient's perspective. Patient Educ Couns. 2015 doi: 10.1016/j.pec.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 26.Gagnon MP, Desmartis M, Gagnon J, St-Pierre M, Gauvin FP, Rhainds M, Lepage-Savary D, Coulombe M, Dipankui MT, Légaré F. Introducing the patient's perspective in hospital health technology assessment (HTA): the views of HTA producers, hospital managers and patients. Health Expect. 2014;17(6):888–900. doi: 10.1111/hex.12010. [DOI] [PMC free article] [PubMed] [Google Scholar]